Skeletal muscle diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Skeletal muscle diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Skeletal muscle diseases US Medical PG Question 1: A 35-year-old woman presents for evaluation of symmetric proximal muscle weakness. The patient also presents with a blue-purple discoloration of the upper eyelids accompanied by rashes on the knuckles, as shown in the picture below. What is the most likely cause?
- A. Dermatomyositis (Correct Answer)
- B. Inclusion body myositis
- C. Duchenne muscular dystrophy
- D. Polymyositis
- E. Hypothyroidism
Skeletal muscle diseases Explanation: ***Dermatomyositis***
- This condition is characterized by **symmetric proximal muscle weakness** accompanied by distinctive skin manifestations, such as a **heliotrope rash** (blue-purple discoloration of the upper eyelids) and **Gottron's papules** (rashes on the knuckles).
- These classic features are almost pathognomonic for dermatomyositis, an **autoimmune inflammatory myopathy**.
*Inclusion body myositis*
- Inclusion body myositis typically presents with **asymmetric distal muscle weakness** and **atrophy**, a pattern different from the symmetric proximal weakness described.
- It primarily affects older individuals and does **not involve skin manifestations**.
*Duchenne muscular dystrophy*
- This is a **genetic disorder** primarily affecting young boys, presenting with progressive muscle weakness that is often noted in early childhood.
- It is characterized by **proximal muscle wasting** and does not present with the specific dermatological findings of heliotrope rash or Gottron's papules.
*Polymyositis*
- Polymyositis also presents with **symmetric proximal muscle weakness**, similar to dermatomyositis, but it **lacks the characteristic skin manifestations** described in the patient.
- The absence of the heliotrope rash and Gottron's papules helps differentiate it from dermatomyositis.
*Hypothyroidism*
- Hypothyroidism can cause **muscle weakness**, myalgia, and cramps, but these symptoms are usually insidious and accompanied by other systemic symptoms like **fatigue**, **weight gain**, and **cold intolerance**.
- It does **not cause the specific skin rashes** (heliotrope rash, Gottron's papules) seen in this patient.
Skeletal muscle diseases US Medical PG Question 2: A 32-year-old woman presents to the clinic with the complaint of excessive fatigue for the past few weeks. After returning home from the office, she feels too tired to climb up the stairs, comb her hair, or chew her food. She has occasionally experienced double vision. She denies any history of fever, cough, weight loss, night sweats, or snoring. Past history is unremarkable. Physical examination reveals: blood pressure 124/86 mm Hg, heart rate 85/min, respiratory rate 14/min, temperature 37.0°C (98.6°F), and body mass index (BMI) 22.6 kg/m2. On examination, the right upper eyelid is slightly drooping when compared to the left side. Her eye movements are normal. Flexion of the neck is mildly weak. Muscle strength is 5/5 in all 4 limbs. When she is asked to alternately flex and extend her shoulder continuously for 5 minutes, the power in the proximal upper limb muscles becomes 4/5. The muscle tone and deep tendon reflexes are normal. What is the most appropriate test to diagnose this condition?
- A. CT scan chest
- B. Plasmapheresis
- C. Tensilon test
- D. Single-fiber electromyography (Correct Answer)
- E. Presynaptic calcium channel antibodies
Skeletal muscle diseases Explanation: ***Single-fiber electromyography***
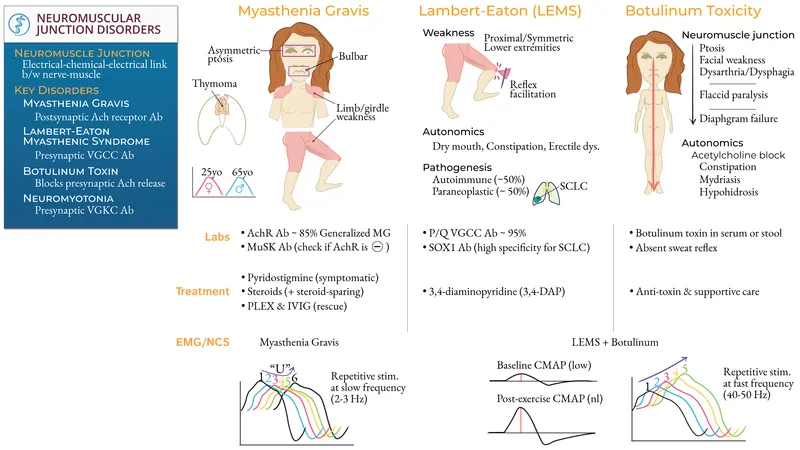
- This patient presents with symptoms highly suggestive of **myasthenia gravis**, including **fatigue**, **ptosis**, **diplopia**, and **fatigable weakness** of proximal muscles exacerbated by repetitive use.
- **Single-fiber electromyography (SFEMG)** is the **most sensitive** electrodiagnostic test for myasthenia gravis, detecting impaired neuromuscular transmission with a sensitivity of **95-99%**.
- While **acetylcholine receptor (AChR) antibodies** are often the first-line test in clinical practice (85-90% sensitivity), SFEMG is superior when antibody tests are negative or when the highest diagnostic sensitivity is required, making it the most appropriate test overall.
*CT scan chest*
- A CT scan of the chest is used to look for a **thymoma**, which is associated with myasthenia gravis in 10-15% of cases, but it is not a diagnostic test for the condition itself.
- While important for prognostication and treatment planning (particularly in patients with confirmed MG), it does not confirm the diagnosis of myasthenia gravis.
*Plasmapheresis*
- **Plasmapheresis** is a treatment for myasthenia gravis, particularly in myasthenic crisis or during exacerbations, by removing anti-acetylcholine receptor antibodies.
- It is not a diagnostic test; diagnostic tests are performed to identify the condition before treatment initiation.
*Tensilon test*
- The **Tensilon (edrophonium) test** was historically used to diagnose myasthenia gravis by transiently improving muscle weakness upon administration of the anticholinesterase drug.
- However, due to potential side effects (e.g., **bradycardia, syncope**) and the availability of more sensitive and safer diagnostic methods like SFEMG and antibody testing, it is **less commonly used** as a primary diagnostic tool today.
*Presynaptic calcium channel antibodies*
- Presynaptic calcium channel antibodies (specifically **P/Q-type voltage-gated calcium channel antibodies**) are characteristic of **Lambert-Eaton myasthenic syndrome (LEMS)**, a disorder of the neuromuscular junction distinct from myasthenia gravis.
- LEMS typically presents with **proximal weakness that improves with exercise** (unlike MG where weakness worsens), autonomic dysfunction, and association with small cell lung cancer.
- This patient's symptoms (fatigable weakness worsening with activity, ptosis, diplopia) are more consistent with myasthenia gravis, which involves postsynaptic acetylcholine receptor antibodies.
Skeletal muscle diseases US Medical PG Question 3: A 10-year-old boy is brought to the physician because of recurring episodes of achy muscle pain in his legs. He has a history of poor school performance despite tutoring and has been held back two grades. He is at the 40th percentile for height and 30th percentile for weight. Examination shows ptosis, a high-arched palate, and muscle weakness in the face and hands; muscle strength of the quadriceps and hamstrings is normal. Sensation is intact. Percussion of the thenar eminence causes the thumb to abduct and then relax slowly. Which of the following is the most likely underlying cause?
- A. Defect of voltage-gated sodium channels of the sarcolemmal membrane
- B. CTG trinucleotide expansion in the DMPK gene (Correct Answer)
- C. Complete impairment of the dystrophin protein
- D. Apoptosis of lower motor neurons
- E. Humoral immune attack against the endomysial blood vessels
Skeletal muscle diseases Explanation: ***CTG trinucleotide expansion in the DMPK gene***
- The patient's symptoms, including **myotonia** (evidenced by the slow relaxation after percussion of the thenar eminence), muscle weakness (especially in the face and hands), ptosis, and intellectual disability, are classic features of **myotonic dystrophy type 1 (DM1)**.
- DM1 is caused by a **CTG trinucleotide repeat expansion** in the 3' untranslated region of the **_DMPK_ (dystrophia myotonica protein kinase) gene**.
*Defect of voltage-gated sodium channels of the sarcolemmal membrane*
- This description is characteristic of **nondystrophic myotonias**, such as **paramyotonia congenita** or **potassium-aggravated myotonia**.
- While these present with myotonia, they typically lack the systemic features of DM1, such as the intellectual disability, ptosis, and characteristic facial weakness.
*Complete impairment of the dystrophin protein*
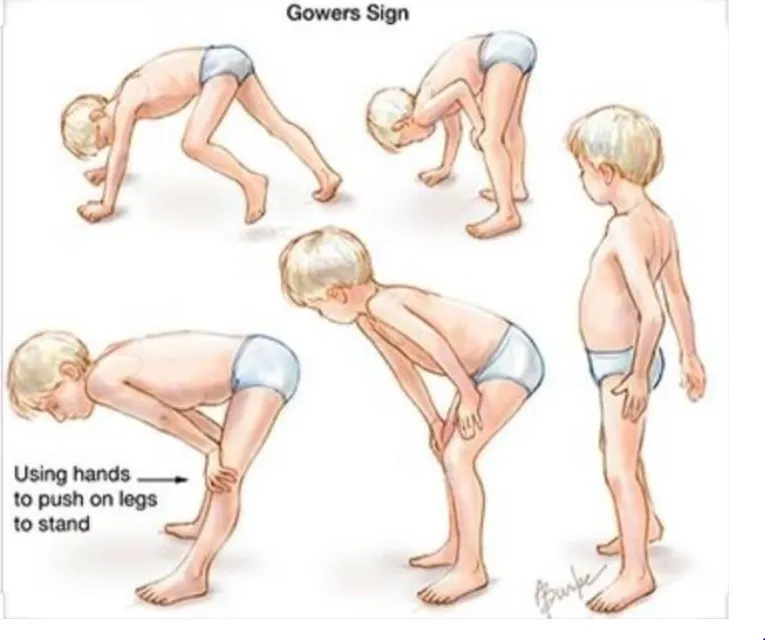
- **Complete impairment of dystrophin** is the underlying cause of **Duchenne muscular dystrophy (DMD)**.
- DMD presents with progressive **proximal muscle weakness**, Gowers' sign, and calf pseudohypertrophy, and typically manifests much earlier with significant motor developmental delays, which are not the primary complaints here.
*Apoptosis of lower motor neurons*
- **Apoptosis of lower motor neurons** is characteristic of conditions like **spinal muscular atrophy (SMA)**.
- SMA causes progressive weakness and atrophy but typically presents as a **flaccid paralysis** and does not involve myotonia, ptosis, or intellectual disability in the same manner as described.
*Humoral immune attack against the endomysial blood vessels*
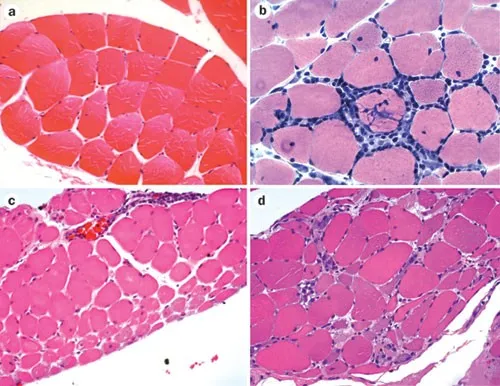
- A **humoral immune attack against endomysial blood vessels** is the hallmark of **dermatomyositis**, a type of inflammatory myopathy.
- Dermatomyositis presents with **proximal muscle weakness**, characteristic skin rashes (e.g., heliotrope rash, Gottron papules), and systemic inflammation, which are not described in this patient.
Skeletal muscle diseases US Medical PG Question 4: A 33-year-old woman comes to the clinic for a follow-up visit after recently starting high dose corticosteroids for a newly diagnosed autoimmune condition. She was first evaluated a month ago due to fatigue, muscle weakness, and a scaly rash on both hands. On examination, muscle strength was rated 2 out of 5 in the upper extremities. Creatine kinase-MB was elevated, and anti-Jo-1 antibodies were observed. A muscle biopsy later showed perimysial inflammation and treatment was initiated. Today, the patient says that her symptoms have not improved despite treatment with corticosteroids. It is agreed upon to initiate methotrexate with the hopes of achieving better symptom control. Which of the following is most often associated with this patient’s condition?
- A. Ovarian cancer
- B. Arthritis
- C. Lung cancer
- D. Raynaud's phenomenon
- E. Interstitial lung disease (Correct Answer)
Skeletal muscle diseases Explanation: ***Interstitial lung disease***
- The patient's condition, characterized by **fatigue**, **muscle weakness**, **scaly rash** (likely **Gottron's papules** or **heliotrope rash**), **elevated CK-MB**, and **anti-Jo-1 antibodies**, strongly suggests **dermatomyositis**, which is frequently associated with **interstitial lung disease (ILD)**.
- Approximately 70% of patients with **anti-Jo-1 antibodies** develop **ILD**, which can manifest as chronic cough and dyspnea.
*Ovarian cancer*
- While dermatomyositis is associated with an **increased risk of malignancy**, particularly in older patients, **ovarian cancer** is not the *most common* or *most frequently associated* manifestation of the disease overall, especially given the patient's age (33).
- The risk of malignancy is higher in adults with dermatomyositis and polymyositis, with various cancers observed, but no single cancer type predominates as a universal association.
*Arthritis*
- **Arthritis** can occur in dermatomyositis and polymyositis, but it is typically **non-erosive** and **non-deforming**, affecting small and large joints.
- While a possible feature, it is less specific and less frequently highlighted as a major systemic complication compared to interstitial lung disease in the context of anti-Jo-1 antibodies.
*Lung cancer*
- Similar to ovarian cancer, **lung cancer** is a potential malignancy associated with dermatomyositis, especially in older patients and smokers.
- However, for a 33-year-old woman with anti-Jo-1 antibodies, **interstitial lung disease** is a more direct and prevalent associated complication than **lung cancer**.
*Raynaud's phenomenon*
- **Raynaud's phenomenon** (episodic digital ischemia) is observed in a subset of patients with dermatomyositis, often those with features of overlap syndromes.
- While present in some cases, it is not as highly prevalent or as clinically significant as **interstitial lung disease** in patients with anti-Jo-1 antibodies.
Skeletal muscle diseases US Medical PG Question 5: A 9-year-old boy is getting fitted for leg braces because he has become too weak to walk without them. He developed normally until age 3 but then he began to get tired more easily and fell a lot. Over time he started having trouble walking and would stand up by using the Gower maneuver. Despite this weakness, his neurologic development is normal for his age. On exam his calves appeared enlarged and he was sent for genetic testing. Sequence data showed that he had a mutation causing a shift in the reading frame, resulting in a severely truncated and non-functional protein. Which of the following types of mutations is most likely the cause of this patient's disorder?
- A. Splice site
- B. Missense
- C. Nonsense
- D. Frameshift (Correct Answer)
- E. Silent
Skeletal muscle diseases Explanation: ***Frameshift***
- A **frameshift mutation** is caused by the insertion or deletion of nucleotides not in multiples of three, leading to a shift in the reading frame of the mRNA. This results in altered codons downstream of the mutation, typically leading to a **premature stop codon** and a **severely truncated, non-functional protein**.
- The description of a mutation causing "a shift in the reading frame, resulting in a severely truncated and non-functional protein" is characteristic of a frameshift mutation, which is the most common type of mutation in **Duchenne muscular dystrophy** (DMD). The clinical picture (onset around age 3-5, progressive proximal weakness, Gower maneuver, calf pseudohypertrophy) is classic for DMD.
- In DMD, frameshift mutations in the dystrophin gene lead to complete loss of functional dystrophin protein, causing the severe progressive muscle weakness seen in this patient.
*Splice site*
- A **splice site mutation** affects the recognition sequences for intron-exon boundaries during mRNA splicing, potentially leading to exon skipping, intron retention, or use of cryptic splice sites. While splice site mutations can cause DMD (accounting for ~10% of cases), they are less common than frameshifts/deletions.
- The specific description of a "shift in the reading frame" points more directly to a frameshift mutation rather than a splicing defect.
*Missense*
- A **missense mutation** results in a single nucleotide substitution that changes one codon to specify a different amino acid. This produces a full-length protein with a single amino acid substitution.
- Missense mutations typically cause the milder **Becker muscular dystrophy** phenotype (with partially functional dystrophin), not the severe Duchenne phenotype described here. The description of a "severely truncated and non-functional protein" does not fit a missense mutation.
*Nonsense*
- A **nonsense mutation** introduces a premature stop codon directly by changing a codon that normally specifies an amino acid into a stop codon (UAG, UAA, or UGA). This results in a truncated protein.
- While nonsense mutations can cause DMD and do produce truncated proteins, the specific wording "shift in the reading frame" is more characteristic of a frameshift mutation. Nonsense mutations don't shift the reading frame—they directly create a stop signal.
*Silent*
- A **silent (synonymous) mutation** is a nucleotide substitution that does not change the amino acid sequence due to the degeneracy of the genetic code (multiple codons can specify the same amino acid).
- Silent mutations produce normal, full-length proteins and would not cause disease symptoms.
Skeletal muscle diseases US Medical PG Question 6: A 3-year-old boy presents to the office with his mother. She states that her son seems weak and unwilling to walk. He only learned how to walk recently after a very notable delay. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all verbal and social milestones but he has a great deal of trouble with gross and fine motor skills. Past medical history is noncontributory. He takes a multivitamin every day. The mother states that some boys on her side of the family have had similar symptoms and worries that her son might have the same condition. Today, the boy’s vital signs include: blood pressure 110/65 mm Hg, heart rate 90/min, respiratory rate 22/min, and temperature 37.0°C (98.6°F). On physical exam, the boy appears well developed and pleasant. He sits and listens and follows direction. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. He struggles to get up to a standing position after sitting on the floor. A genetic study is performed that reveals a significant deletion in the gene that codes for dystrophin. Which of the following is the most likely diagnosis?
- A. Limb-girdle muscular dystrophy
- B. Becker muscular dystrophy
- C. Myotonic muscular dystrophy
- D. Emery-Dreifuss muscular dystrophy
- E. Duchenne muscular dystrophy (Correct Answer)
Skeletal muscle diseases Explanation: ***Duchenne muscular dystrophy***
- The patient's presentation with **delayed walking**, **progressive muscle weakness** (manifesting as difficulty getting up from the floor, i.e., **Gowers' sign**), and the genetic finding of a **significant dystrophin gene deletion** are classic for Duchenne muscular dystrophy (DMD).
- DMD is caused by **out-of-frame deletions** or mutations that result in the **complete absence of functional dystrophin protein**, leading to severe, early-onset muscle weakness.
- DMD is an **X-linked recessive** condition, explaining the maternal family history of similar symptoms in boys, as only males are typically affected.
*Limb-girdle muscular dystrophy*
- This group of disorders also causes progressive muscle weakness, primarily affecting the **proximal muscles** of the shoulders and hips.
- However, these are caused by mutations in genes **other than dystrophin**, and the **specific dystrophin gene deletion** found in this patient points definitively to DMD rather than limb-girdle muscular dystrophy.
*Becker muscular dystrophy*
- Becker muscular dystrophy (BMD) is also caused by mutations in the **dystrophin gene**, but typically involves **in-frame deletions** that produce a **shortened but partially functional** dystrophin protein.
- The **significant deletion** described in this case, combined with the **severe, early-onset presentation** (weakness at age 3, delayed walking), indicates complete loss of dystrophin function characteristic of DMD, not the milder BMD which typically presents later (age 5-15) with slower progression.
*Myotonic muscular dystrophy*
- This condition is characterized by **myotonia** (delayed muscle relaxation) and a multisystemic presentation, often including **facial weakness**, **cataracts**, and cardiac conduction abnormalities.
- It is caused by a **trinucleotide repeat expansion**, not a dystrophin gene deletion, and none of the key features of myotonic dystrophy are described in this patient's presentation.
*Emery-Dreifuss muscular dystrophy*
- Emery-Dreifuss muscular dystrophy (EDMD) is characterized by a classic triad of **early contractures** (elbows, ankles, neck), **progressive muscle weakness** (especially in the humeroperoneal distribution), and **cardiac involvement** (e.g., conduction defects).
- While some forms of EDMD can involve genes related to the dystrophin-associated protein complex, the **dystrophin gene deletion** itself is specific to DMD/BMD, and this patient lacks the characteristic early contractures and cardiac findings of EDMD.
Skeletal muscle diseases US Medical PG Question 7: A 7-year-old boy is brought to the emergency department by his parents. He is complaining of left-sided knee pain which has progressively increased in severity over the past 2 days. It started when he was playing football with his brothers but he does not recall falling or getting any injury. Past medical history is significant for prolonged bleeding and easy bruising. His maternal uncle has similar problems. Physical exam reveals swollen and painful left knee. His laboratory investigations reveal:
Hemoglobin 11.8 g/dL
WBC count 7,000/mL
Platelets 250,000/mL
INR 0.9
aPTT 62 sec, fully corrected with a mixing study
Which of the following disorders have the same mode of inheritance as this patient’s disease?
- A. Hereditary spherocytosis
- B. Alkaptonuria
- C. Duchenne muscular dystrophy (Correct Answer)
- D. Sickle cell disease
- E. Huntington's disease
Skeletal muscle diseases Explanation: ***Duchenne muscular dystrophy***
- The patient's presentation with **hemarthrosis** (knee pain and swelling without trauma), **prolonged bleeding**, and **easy bruising**, along with a **prolonged aPTT** that corrects with a mixing study, is highly suggestive of **hemophilia A or B**. Both conditions are **X-linked recessive disorders**, affecting males predominantly.
- **Duchenne muscular dystrophy** is also an **X-linked recessive disorder**, making its mode of inheritance identical to the suspected diagnosis of hemophilia in this patient.
*Hereditary spherocytosis*
- This condition is inherited in an **autosomal dominant** pattern, which is different from the mode of inheritance for hemophilia.
- It is characterized by **hemolytic anemia** due to a defect in red blood cell membrane proteins.
*Alkaptonuria*
- Alkaptonuria is an **autosomal recessive** disorder, caused by a deficiency of homogentisate 1,2-dioxygenase.
- It leads to the accumulation of **homogentisic acid**, causing **dark urine** when exposed to air, **ochronosis**, and **arthropathy**, distinct from the patient's bleeding disorder.
*Sickle cell disease*
- **Sickle cell disease** is an **autosomal recessive** disorder, characterized by abnormal hemoglobin leading to chronic hemolytic anemia and vaso-occlusive crises.
- While it can cause joint pain due to avascular necrosis or infarction, its inheritance pattern is different from the patient's condition.
*Huntington's disease*
- **Huntington's disease** is an **autosomal dominant** neurodegenerative disorder that manifests with progressive motor, cognitive, and psychiatric symptoms, typically in middle age.
- Its inheritance pattern and clinical presentation are distinct from the patient's bleeding disorder.
Skeletal muscle diseases US Medical PG Question 8: A 15-year-old Caucasian male is brought to his pediatrician by his parents, who note the development of a tremor in their child. Urine and serum analysis reveal elevated levels of copper. Which of the following clinical manifestations would the physician most expect to see in this patient?
- A. Kaiser-Fleischer rings (Correct Answer)
- B. Diabetes mellitus
- C. Hepatocytes that stain with Prussian blue
- D. Panacinar emphysema
- E. Increased serum ceruloplasmin
Skeletal muscle diseases Explanation: ***Kaiser-Fleischer rings***
- Elevated copper levels, tremor, and young age are classic signs of **Wilson's disease**, an autosomal recessive disorder leading to copper accumulation.
- **Kaiser-Fleischer rings** are greenish-brown deposits of copper in the cornea, a hallmark ocular manifestation of Wilson's disease.
*Diabetes mellitus*
- While copper dysregulation can affect various organs, **diabetes mellitus** is not a typical clinical manifestation of Wilson's disease.
- Pancreatic involvement leading to diabetes is more commonly associated with conditions like **hemochromatosis** (iron overload) or chronic pancreatitis.
*Hepatocytes that stain with Prussian blue*
- **Prussian blue stain** is used to detect **iron deposits**, not copper.
- In Wilson's disease, copper accumulates in hepatocytes, which would not stain positive with Prussian blue.
*Panacinar emphysema*
- **Panacinar emphysema** is primarily associated with **alpha-1 antitrypsin deficiency**, a genetic disorder affecting elastic tissue in the lungs.
- It has no direct association with copper metabolism or Wilson's disease.
*Increased serum ceruloplasmin*
- **Ceruloplasmin** is a copper-carrying protein, and in Wilson's disease, the **serum ceruloplasmin level is typically reduced**, not increased.
- This reduction is due to impaired copper incorporation into ceruloplasmin by the dysfunctional ATP7B protein.
Skeletal muscle diseases US Medical PG Question 9: A 25-year-old woman presents to her primary care physician for her yearly physical exam. She has no past medical history and says that she does not currently have any health concerns. On physical exam, she is found to have hyperactive patellar reflexes but says that she has had this finding since she was a child. She asks her physician why this might be the case. Her physician explains that there are certain cells that are responsible for detecting muscle stretch and responding to restore the length of the muscle. Which of the following is most likely a characteristic of these structures?
- A. They inhibit the activity of alpha-motoneurons
- B. They activate inhibitory interneurons
- C. They are in parallel with extrafusal skeletal muscle fibers (Correct Answer)
- D. They are in series with extrafusal skeletal muscle fibers
- E. They are innervated by group Ib afferent neurons
Skeletal muscle diseases Explanation: ***They are in parallel with extrafusal skeletal muscle fibers***
- The structures described are **muscle spindles**, which are **stretch receptors** located within the muscle belly and arranged in parallel with **extrafusal muscle fibers**.
- This parallel arrangement allows them to detect changes in **muscle length** and the rate of change of length, initiating the **stretch reflex**.
*They inhibit the activity of alpha-motoneurons*
- Muscle spindles, primarily through their **Ia afferent fibers**, **excite** alpha-motoneurons, leading to muscle contraction and opposing the stretch.
- **Inhibition** of alpha-motoneurons is typically associated with structures like **Golgi tendon organs**, which respond to muscle tension.
*They activate inhibitory interneurons*
- While muscle spindles do excite **excitatory interneurons** that activate synergistic muscles, their primary action in the monosynaptic stretch reflex is direct excitation of **alpha-motoneurons**.
- **Inhibitory interneurons** are typically involved in mediating **reciprocal inhibition** of antagonistic muscles in response to muscle spindle activation.
*They are in series with extrafusal skeletal muscle fibers*
- Structures arranged in **series** with extrafusal muscle fibers are **Golgi tendon organs**, which are tension receptors.
- Muscle spindles are oriented **in parallel** to detect changes in muscle length.
*They are innervated by group Ib afferent neurons*
- Muscle spindles are primarily innervated by **group Ia (primary) afferent neurons** and **group II (secondary) afferent neurons**, which detect muscle length and rate of change of length.
- **Group Ib afferent neurons** innervate **Golgi tendon organs**, which are sensitive to muscle tension.
Skeletal muscle diseases US Medical PG Question 10: You are conducting a lab experiment on skeletal muscle tissue to examine force in different settings. The skeletal muscle tissue is hanging down from a hook. The experiment has 3 different phases. In the first phase, you compress the muscle tissue upwards, making it shorter. In the second phase, you attach a weight of 2.3 kg (5 lb) to its lower vertical end. In the third phase, you do not manipulate the muscle length at all. At the end of the study, you see that the tension is higher in the second phase than in the first one. What is the mechanism underlying this result?
- A. The tension in phase 1 is only active, while in phase 2 it is both active and passive.
- B. Shortening the muscle in phase 1 pulls the actin and myosin filaments apart.
- C. Lengthening of the muscle in phase 2 increases passive tension. (Correct Answer)
- D. There are more actin-myosin cross-bridges attached in phase 2 than in phase 1.
- E. Shortening of the muscle in phase 1 uses up ATP stores.
Skeletal muscle diseases Explanation: ***Lengthening of the muscle in phase 2 increases passive tension.***
- Attaching a weight of 2.3 kg (5 lb) in phase 2 **stretches** the muscle, increasing the **passive tension** generated by elastic components like **titin**.
- This added passive tension, combined with any active tension, results in a **higher total tension** compared to the shortened state in phase 1 where passive tension is minimal.
*The tension in phase 1 is only active, while in phase 2 it is both active and passive.*
- While passive tension is more significant in phase 2 due to stretching, the muscle in phase 1, even when compressed, can still generate some **active tension** if stimulated.
- The key difference contributing to higher tension in phase 2 is the additional **passive component** from stretching, not necessarily the exclusive presence of active tension in one phase.
*Shortening the muscle in phase 1 pulls the actin and myosin filaments apart.*
- Shortening the muscle too much, beyond its optimal resting length, leads to **overlap of actin filaments** and **crumpling of myosin filaments**, reducing the number of available cross-bridge binding sites.
- This **decreases active tension** rather than pulling filaments apart, which would require excessive stretching.
*There are more actin-myofibril cross-bridges attached in phase 2 than in phase 1.*
- Shortening the muscle in phase 1 beyond optimal length **reduces the number of cross-bridges** that can form due to actin filament overlap.
- While lengthening in phase 2 might bring the muscle closer to an **optimal length** for cross-bridge formation (increasing active tension), the primary reason for the higher tension in phase 2 as described is the increase in **passive tension** from stretching, rather than solely increased active cross-bridge formation.
*Shortening of the muscle in phase 1 uses up ATP stores.*
- Muscle contraction, whether shortening or lengthening, requires **ATP hydrolysis** for cross-bridge cycling.
- The act of shortening itself doesn't uniquely "use up" ATP stores more significantly than other contractile actions to explain the observed tension difference; ATP is continuously consumed and regenerated during muscle activity.
More Skeletal muscle diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.