Pancreatic diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pancreatic diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
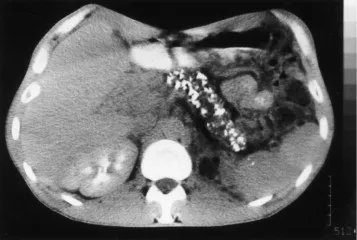
Pancreatic diseases US Medical PG Question 1: A 55-year-old man is brought to the emergency room by his roommate due to an abdominal pain that started 2 hours ago. His pain is dull, aching, and radiates to the back. He admits to binge drinking alcohol for the past 2 days. Past medical history is significant for multiple admissions to the hospital for similar abdominal pain events, hypertension, and hyperlipidemia. He takes chlorthalidone and atorvastatin. He admits to heavy alcohol consumption over the past 10 years. He has smoked a pack of cigarettes a day for the last 20 years. In the emergency department, his temperature is 38.9℃ (102.0℉), pulse rate is 100/min, and respiratory rate is 28/min. On physical examination, he looks generally unwell and diaphoretic. Auscultation of his heart and lungs reveals an elevated heart rate with a regular rhythm. His lungs are clear to auscultation bilaterally. His abdomen is tympanitic with generalized tenderness. Evaluation of lab values reveals a leukocyte count of 28,000/mm3 with 89% of neutrophils. His amylase level is 255 U/L. A CT scan of the abdomen shows the diffuse enlargement of the pancreas. Which pathological process is most likely occurring in this patient’s peripancreatic tissue?
- A. Fat necrosis (Correct Answer)
- B. Caseous necrosis
- C. Fibrinoid necrosis
- D. Coagulative necrosis
- E. Liquefactive necrosis
Pancreatic diseases Explanation: ***Fat necrosis***
- This patient presents with **acute pancreatitis**, characterized by severe epigastric pain radiating to the back, elevated amylase, and diffuse pancreatic enlargement on CT, all exacerbated by **binge drinking**.
- In acute pancreatitis, activated pancreatic enzymes, particularly **lipases**, leak into the peripancreatic fat, causing enzymatic breakdown of fat into fatty acids, which then combine with calcium to form **calcium soaps** (saponification), clinically recognizable as fat necrosis.
*Caseous necrosis*
- This type of necrosis is typically associated with **tuberculosis** and fungal infections, forming a cheesy, crumbly appearance.
- It involves a granulomatous inflammatory response and does not align with the enzyme-driven fat breakdown seen in pancreatitis.
*Fibrinoid necrosis*
- This is a vascular injury characterized by the deposition of **fibrin-like material** in arterial walls, often seen in immune-mediated vasculitis or severe hypertension.
- It is not a primary pathological process in the peripancreatic tissue during acute pancreatitis.
*Coagulative necrosis*
- This form of necrosis is characteristic of **ischemic injury** in most solid organs (e.g., heart, kidney) where the cellular architecture is preserved for some time.
- While pancreatic necrosis can occur, the specific breakdown of peripancreatic fat by lipases leads to fat necrosis, not coagulative necrosis of the fat itself.
*Liquefactive necrosis*
- This type of necrosis occurs in tissues rich in hydrolytic enzymes and low in structural proteins, such as the **brain after ischemia** or in **abscesses**.
- While pancreatic tissue undergoing severe necrosis can exhibit liquefaction, the specific process affecting the surrounding fat in pancreatitis is fat necrosis due to lipase activity.
Pancreatic diseases US Medical PG Question 2: A 70-year-old male visits his primary care physician because of progressive weight loss. He has a 20-year history of smoking 2 packs of cigarettes a day and was diagnosed with diabetes mellitus 6 years ago. After physical examination, the physician tells the patient he suspects adenocarcinoma at the head of the pancreas. Which of the following physical examination findings would support the diagnosis?
- A. Lymphadenopathy of the umbilicus
- B. Splenomegaly
- C. Acanthosis nigricans
- D. Palpable gallbladder (Correct Answer)
- E. Renal artery bruits
Pancreatic diseases Explanation: ***Palpable gallbladder***
- A palpable, non-tender gallbladder in the presence of **jaundice** (often caused by obstruction of the common bile duct) is known as **Courvoisier's sign**, which is highly suggestive of pancreatic head adenocarcinoma.
- The tumor in the head of the pancreas can compress the distal common bile duct, leading to bile stasis and gallbladder distension.
*Lymphadenopathy of the umbilicus*
- **Umbilical lymphadenopathy**, specifically a **Sister Mary Joseph nodule**, indicates distant metastatic disease, often from intra-abdominal cancers like gastrointestinal or ovarian.
- While it points to an advanced malignancy, it is not a direct physical finding specific for initial suspicion of primary pancreatic head adenocarcinoma.
*Splenomegaly*
- **Splenomegaly** can be a feature of pancreatic cancer if there is splenic vein thrombosis due to tumor invasion, leading to **portal hypertension**.
- However, it is not a primary sign of pancreatic head adenocarcinoma and typically occurs in more advanced or specific cases.
*Acanthosis nigricans*
- **Acanthosis nigricans** is characterized by hyperpigmented, velvety plaques, often in skin folds, and can be a paraneoplastic syndrome associated with various malignancies, including pancreatic cancer.
- While possible, it is a less direct and less specific sign for pancreatic head adenocarcinoma compared to Courvoisier's sign.
*Renal artery bruits*
- **Renal artery bruits** indicate turbulent blood flow through the renal arteries, most commonly due to **renal artery stenosis**, which can cause hypertension.
- This finding is unrelated to pancreatic adenocarcinoma and would not support such a diagnosis.
Pancreatic diseases US Medical PG Question 3: A 51-year-old homeless man presents to the emergency department with severe abdominal pain and cramping for the past 3 hours. He endorses radiation to his back. He adds that he vomited multiple times. He admits having been hospitalized repeatedly for alcohol intoxication and abdominal pain. His temperature is 103.8° F (39.8° C), respiratory rate is 15/min, pulse is 107/min, and blood pressure is 100/80 mm Hg. He refuses a physical examination due to severe pain. Blood work reveals the following:
Serum:
Albumin: 3.2 gm/dL
Alkaline phosphatase: 150 U/L
Alanine aminotransferase: 76 U/L
Aspartate aminotransferase: 155 U/L
Gamma-glutamyl transpeptidase: 202 U/L
Lipase: 800 U/L
What is the most likely diagnosis of this patient?
- A. Duodenal peptic ulcer
- B. Choledocholithiasis
- C. Pancreatitis (Correct Answer)
- D. Cholecystitis
- E. Gallbladder cancer
Pancreatic diseases Explanation: ***Pancreatitis***
- The patient's history of **repeated alcohol intoxication** and abdominal pain, combined with **severe abdominal pain radiating to the back**, vomiting, and significantly elevated **lipase (800 U/L)**, are highly indicative of **acute pancreatitis**.
- The elevated **liver enzymes (ALT, AST, GGT)** and **alkaline phosphatase** can be associated with cholestasis or liver involvement often seen in alcohol-induced pancreatitis or can be elevated due to a gallstone lodged in the common bile duct, which is also a common cause of pancreatitis.
*Duodenal peptic ulcer*
- While duodenal ulcers cause severe abdominal pain, they typically present with **epigastric pain** that may be relieved by food, and often cause **melena or hematemesis** if bleeding.
- The extremely high **lipase level** and pain radiating to the back are not characteristic of an uncomplicated duodenal ulcer.
*Choledocholithiasis*
- **Choledocholithiasis** (gallstones in the common bile duct) can cause severe right upper quadrant or epigastric pain and elevated liver enzymes, but it doesn't typically present with an isolated, dramatically high **lipase** level without concomitant pancreatitis.
- The main symptom is **biliary colic**, often post-prandial, and usually involves jaundice or cholangitis if infected.
*Cholecystitis*
- **Cholecystitis** presents with **right upper quadrant pain**, often radiating to the shoulder, associated with fever and nausea, and is usually triggered by fatty meals.
- Although there might be some elevation in liver enzymes and amylase/lipase, the **markedly elevated lipase** and pain radiating to the back are more suggestive of pancreatitis.
*Gallbladder cancer*
- **Gallbladder cancer** typically presents with more insidious symptoms, such as chronic right upper quadrant pain, weight loss, jaundice, and anorexia.
- It would not usually present with an acute episode of **severe abdominal pain and drastically high lipase** in this manner.
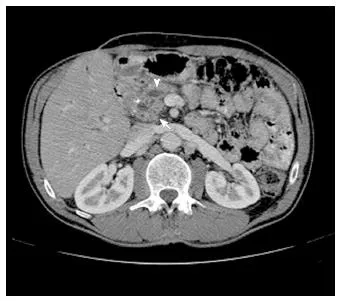
Pancreatic diseases US Medical PG Question 4: A 29-year-old woman presents with a 2-hour history of sudden onset of severe mid-epigastric pain. The pain radiates to the back, and is not relieved by over-the-counter antacids. The patient also complains of profuse vomiting. The patient’s medical history is negative for similar symptoms. She consumes 3–4 alcoholic drinks daily. The blood pressure is 80/40 mm Hg and the heart rate is 105/min. Examination of the lungs reveals bibasilar crackles. Abdominal examination reveals diffuse tenderness involving the entire abdomen, marked guarding, rigidity, and reduced bowel sounds. The chest X-ray is normal. However, the abdominal CT scan reveals peritoneal fluid collection and diffuse pancreatic enlargement. The laboratory findings include:
Aspartate aminotransferase 63 IU/L
Alkaline phosphatase 204 IU/L
Alanine aminotransferase 32 IU/L
Serum amylase 500 IU/L (Normal: 25-125 IU/L)
Serum lipase 1,140 IU/L (Normal: 0-160 IU/L)
Serum calcium 2 mmol/L
Which of the following cellular changes are most likely, based on the clinical and laboratory findings?
- A. Liquefactive necrosis
- B. Dry gangrene
- C. Caseous necrosis
- D. Coagulative necrosis
- E. Fat necrosis (Correct Answer)
Pancreatic diseases Explanation: ***Fat necrosis***
- The patient's presentation with severe epigastric pain radiating to the back, elevated serum amylase and lipase, **alcohol abuse**, and diffuse pancreatic enlargement indicates **acute pancreatitis**.
- **Fat necrosis** is a characteristic pathologic finding in acute pancreatitis, resulting from the release of activated pancreatic enzymes (like lipase) into the surrounding adipose tissue, causing **FFA (free fatty acid)** formation that complexes with calcium (saponification).
*Liquefactive necrosis*
- This type of necrosis is characterized by the complete digestion of dead cells, resulting in a **viscous liquid mass**.
- It is typically seen in **bacterial infections** or **cerebral infarcts**, not primarily in pancreatitis.
*Dry gangrene*
- **Dry gangrene** involves ischemic necrosis, usually affecting the extremities, where the tissue becomes **dry, shrunken, and black**.
- It is caused by **lack of blood supply** and does not fit the clinical picture of acute pancreatitis.
*Caseous necrosis*
- **Caseous necrosis** is a distinct form of coagulative necrosis, characterized by a **cheese-like appearance** of the necrotic tissue.
- It is most commonly associated with **tuberculosis** and certain fungal infections, not acute pancreatitis.
*Coagulative necrosis*
- **Coagulative necrosis** is characterized by the preservation of the cell shape and tissue architecture for several days after cell death, often due to **ischemia** (e.g., myocardial infarction).
- While pancreatic cells can undergo coagulative necrosis in severe ischemia, **fat necrosis** is specifically and prominently associated with the enzymatic destruction in acute pancreatitis.
Pancreatic diseases US Medical PG Question 5: A 53-year-old man comes to the physician because of fatigue, recurrent diarrhea, and an 8-kg (17.6-lb) weight loss over the past 6 months. He has a 4-month history of recurrent blistering rashes on different parts of his body that grow and develop into pruritic, crusty lesions before resolving spontaneously. Physical examination shows scaly lesions in different phases of healing with central, bronze-colored induration around the mouth, perineum, and lower extremities. Laboratory studies show:
Hemoglobin 10.1 mg/dL
Mean corpuscular volume 85 μm3
Mean corpuscular hemoglobin 30.0 pg/cell
Serum
Glucose 236 mg/dL
Abdominal ultrasonography shows a 3-cm, solid mass located in the upper abdomen. This patient's mass is most likely derived from which of the following types of cells?
- A. Gastrointestinal enterochromaffin cells
- B. Pancreatic β-cells
- C. Pancreatic δ-cells
- D. Pancreatic α-cells (Correct Answer)
- E. Gastric G-cells
Pancreatic diseases Explanation: ***Pancreatic α-cells***
- The patient's symptoms of **fatigue, recurrent diarrhea, weight loss, blistering rash (necrolytic migratory erythema)**, and **hyperglycemia** are classic features of a **glucagonoma**.
- A **glucagonoma** is a tumor of the pancreatic α-cells that **secretes excessive glucagon**, leading to these characteristic signs and symptoms, supported by the presence of an **upper abdominal mass**.
*Gastrointestinal enterochromaffin cells*
- Tumors of gastrointestinal enterochromaffin cells (carcinoid tumors) typically produce **serotonin** and present with flushing, diarrhea, bronchospasm, and valvular heart disease, not the skin rash or hyperglycemia seen here.
- While carcinoid tumors can cause diarrhea, the additional symptoms of **necrolytic migratory erythema** and **diabetes** are not characteristic.
*Pancreatic β-cells*
- Tumors of pancreatic β-cells (**insulinomas**) produce excessive insulin, leading to **hypoglycemia**, not the hyperglycemia observed in this patient.
- Insulinomas cause symptoms like sweating, tremors, confusion, and palpitations, which are inconsistent with the patient's presentation.
*Pancreatic δ-cells*
- Pancreatic δ-cell tumors (**somatostatinomas**) secrete **somatostatin**, which can cause **diabetes mellitus**, steatorrhea, and gallstones.
- While diabetes is present, the characteristic **necrolytic migratory erythema** and severe diarrhea are less common with somatostatinomas.
*Gastric G-cells*
- Tumors of gastric G-cells (**gastrinomas**) secrete **gastrin**, leading to **Zollinger-Ellison syndrome**, characterized by severe peptic ulcers, abdominal pain, and chronic diarrhea.
- Gastrinomas do not typically cause **necrolytic migratory erythema** or significant hyperglycemia.
Pancreatic diseases US Medical PG Question 6: A 61-year-old woman presents to the urgent care unit with a 2-week history of abdominal pain after meals. The patient reports vomiting over the past few days. The past medical history is significant for osteoarthritis and systemic lupus erythematosus. She regularly drinks alcohol. She does not smoke cigarettes. The patient currently presents with vital signs within normal limits. On physical examination, the patient appears to be in moderate distress, but she is alert and oriented. The palpation of the abdomen elicits tenderness in the epigastric region. The CT of the abdomen shows no signs of an acute process. The laboratory results are listed below. Which of the following is the most likely diagnosis?
Na+ 139 mEq/L
K+ 4.4 mEq/L
Cl- 109 mmol/L
HCO3- 20 mmol/L
BUN 14 mg/dL
Cr 1.0 mg/dL
Glucose 101 mg/dL
Total cholesterol 187 mg/dL
LDL 110 mg/dL
HDL 52 mg/dL
TG 120 mg/dL
AST 65 IU/L
ALT 47 IU/L
GGT 27 IU/L
Amylase 512 U/L
Lipase 1,262 U/L
- A. Acute liver failure
- B. Acute pancreatitis (Correct Answer)
- C. Acute mesenteric ischemia
- D. Acute cholecystitis
- E. Gastric ulcer
Pancreatic diseases Explanation: **Acute pancreatitis**
- The patient presents with classic symptoms of **acute pancreatitis**, including **epigastric abdominal pain** that worsens after meals, and **vomiting**.
- Significantly elevated **amylase** (512 U/L) and **lipase** (1,262 U/L) levels (both more than three times the upper limit of normal) confirm the diagnosis. The patient's history of **alcohol consumption** is a major risk factor.
*Acute liver failure*
- Acute liver failure would typically present with significantly elevated **ALT and AST values**, often in the thousands, along with signs of **hepatic encephalopathy** or coagulopathy, none of which are present here.
- While the AST and ALT are mildly elevated, they are not indicative of acute liver failure, and the patient's other liver function tests (GGT, cholesterol panel) are relatively normal.
*Acute mesenteric ischemia*
- **Acute mesenteric ischemia** presents with severe, **disproportionate pain** to physical findings, often described as "pain out of proportion to examination." It is less commonly associated with elevated lipase and amylase.
- While patient has a history of systemic lupus erythematosus that could potentially increase the risk of thrombotic events, the absence of severe abdominal pain and the very high lipase levels make this less likely.
*Acute cholecystitis*
- **Acute cholecystitis** typically presents with right upper quadrant pain, fever, and leukocytosis, often precipitated by fatty meals. **Murphy's sign** is usually positive.
- While abdominal pain after meals and vomiting could occur, the pain is specifically epigastric, and there are no signs of inflammation (fever, WBC count not provided but general physical examination findings are not pointing to cholecystitis) and the remarkably elevated lipase and amylase are not features of cholecystitis.
*Gastric ulcer*
- A **gastric ulcer** typically causes **epigastric pain** that may be relieved by food (duodenal ulcer) or worsened by food (gastric ulcer), and can cause vomiting.
- However, the extremely high **amylase and lipase levels** are not characteristic of a gastric ulcer and point towards a pancreatic etiology.
Pancreatic diseases US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pancreatic diseases Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pancreatic diseases US Medical PG Question 8: A 62-year-old Caucasian man visits his primary care provider with recurrent episodes of moderate to severe abdominal pain, nausea, and anorexia for the past 2 years. Additional complaints include constipation, steatorrhea, weight loss, polyphagia, and polyuria. His personal history is relevant for a 2-year period of homelessness when the patient was 55 years old, cigarette smoking since the age of 20, alcohol abuse, and cocaine abuse for which is currently under the supervision of a psychiatry team. He has a pulse of 70/min, a respiratory rate of 16/min, a blood pressure of 130/70 mm Hg, and a body temperature of 36.4°C (97.5°F). His height is 178 cm (5 ft 10 in) and weight is 90 kg (198 lb). On physical examination, he is found to have telangiectasias over the anterior chest, mild epigastric tenderness, and a small nodular liver. Laboratory test results from his previous visit a month ago are shown below:
Fasting plasma glucose 160 mg/dL
HbA1c 8%
Serum triglycerides 145 mg/dL
Total cholesterol 250 mg/dL
Total bilirubin 0.8 mg/dL
Direct bilirubin 0.2 mg/dL
Amylase 180 IU/L
Lipase 50 IU/L
Stool negative for blood; low elastase
This patient’s condition is most likely secondary to which of the following conditions?
- A. Hypertriglyceridemia
- B. Alcohol abuse (Correct Answer)
- C. Cocaine abuse
- D. Hypercholesterolemia
- E. Obesity
Pancreatic diseases Explanation: ***Alcohol abuse***
- Chronic alcohol abuse is a major risk factor for **chronic pancreatitis**, which manifests with recurrent abdominal pain, steatorrhea, weight loss, and can lead to **diabetes mellitus** (polyphagia, polyuria, elevated fasting glucose and HbA1c).
- The elevated amylase, although not diagnostic for chronic pancreatitis on its own, along with low stool elastase (indicating **pancreatic exocrine insufficiency**), telangiectasias (suggesting liver disease often associated with alcohol), and a nodular liver (pointing to **cirrhosis**), strongly support chronic pancreatitis secondary to alcohol.
*Hypertriglyceridemia*
- While severe hypertriglyceridemia (typically >1000 mg/dL) can cause acute pancreatitis, the patient's triglyceride level (145 mg/dL) is not high enough to be the cause of his chronic pancreatic issues.
- Furthermore, chronic pancreatitis symptoms like steatorrhea and diabetes are better explained by long-term alcohol exposure.
*Cocaine abuse*
- Cocaine can cause **vasoconstriction** and ischemia, potentially leading to acute pancreatitis, but it is not a common cause of chronic pancreatitis with the constellation of symptoms observed here.
- The clinical picture strongly aligns with the chronic effects of alcohol on the pancreas and liver.
*Hypercholesterolemia*
- While hypercholesterolemia (total cholesterol 250 mg/dL) is a risk factor for cardiovascular disease, it is not directly implicated in causing pancreatitis or liver disease in the way described.
- It does not explain the recurrent abdominal pain, steatorrhea, or the development of diabetes and liver changes seen in this patient.
*Obesity*
- Obesity is a risk factor for various metabolic disorders, including type 2 diabetes and non-alcoholic fatty liver disease (NAFLD), but it is not a primary cause of chronic pancreatitis.
- The specific signs of liver damage (telangiectasias, nodular liver) and the pancreatic exocrine insufficiency point away from obesity as the primary etiology for this patient's condition.
Pancreatic diseases US Medical PG Question 9: A previously healthy 59-year-old man comes to the physician with a 6-month history of worsening headaches, difficulty chewing, and progressive hearing loss. Examination shows a mildly tender, 1-cm, hard swelling over the left maxilla. The remainder of the examination shows no abnormalities. Serum studies show a calcium concentration of 8.5 mg/dL, alkaline phosphatase activity of 112 U/L, and parathyroid hormone concentration of 310 pg/mL. Audiometry shows bilateral mixed conductive and sensorineural hearing loss. Which of the following processes is the most likely cause of this patient's condition?
- A. Defective synthesis of dynein
- B. Decreased activity of carbonic anhydrase II
- C. Decreased expression of menin protein
- D. Increased activity of nuclear factor-κB (Correct Answer)
- E. Defective synthesis of type I collagen
Pancreatic diseases Explanation: ***Increased activity of nuclear factor-κB***
- The patient's symptoms (worsening headaches, difficulty chewing, hearing loss, localized bony swelling) and laboratory findings (elevated alkaline phosphatase, normal calcium, elevated PTH) are highly suggestive of **Paget's disease of bone** (osteitis deformans).
- **Paget's disease** is characterized by focal areas of increased bone turnover, involving both excessive bone resorption by osteoclasts and disorganized bone formation by osteoblasts, often linked to increased **NF-κB activity** in osteoclasts.
*Defective synthesis of dynein*
- **Dynein defects** are associated with conditions like primary ciliary dyskinesia, which presents with chronic sinopulmonary infections and situs inversus.
- This condition does not explain the patient's bone remodeling issues or localized bony swelling.
*Decreased activity of carbonic anhydrase II*
- **Carbonic anhydrase II deficiency** causes osteopetrosis (marble bone disease), a condition characterized by abnormally dense bones due to impaired osteoclast function.
- This would typically lead to symptoms like bone fractures, cranial nerve compression, and pancytopenia, which are distinct from the presented case.
*Decreased expression of menin protein*
- **Menin protein deficiency**, due to mutations in the *MEN1* gene, is associated with Multiple Endocrine Neoplasia type 1 (MEN1), involving tumors of the parathyroid, pituitary, and pancreas.
- While the patient has elevated PTH, the primary features of bone remodeling and localized swelling point away from MEN1 as the primary diagnosis.
*Defective synthesis of type I collagen*
- **Defective type I collagen synthesis** is characteristic of osteogenesis imperfecta, leading to brittle bones, frequent fractures, and blue sclera.
- This is a generalized skeletal disorder with a genetic basis, typically presenting earlier in life, and does not align with the patient's localized bone overgrowth and increased osteoclast activity.
Pancreatic diseases US Medical PG Question 10: A 15-year-old Caucasian male is brought to his pediatrician by his parents, who note the development of a tremor in their child. Urine and serum analysis reveal elevated levels of copper. Which of the following clinical manifestations would the physician most expect to see in this patient?
- A. Kaiser-Fleischer rings (Correct Answer)
- B. Diabetes mellitus
- C. Hepatocytes that stain with Prussian blue
- D. Panacinar emphysema
- E. Increased serum ceruloplasmin
Pancreatic diseases Explanation: ***Kaiser-Fleischer rings***
- Elevated copper levels, tremor, and young age are classic signs of **Wilson's disease**, an autosomal recessive disorder leading to copper accumulation.
- **Kaiser-Fleischer rings** are greenish-brown deposits of copper in the cornea, a hallmark ocular manifestation of Wilson's disease.
*Diabetes mellitus*
- While copper dysregulation can affect various organs, **diabetes mellitus** is not a typical clinical manifestation of Wilson's disease.
- Pancreatic involvement leading to diabetes is more commonly associated with conditions like **hemochromatosis** (iron overload) or chronic pancreatitis.
*Hepatocytes that stain with Prussian blue*
- **Prussian blue stain** is used to detect **iron deposits**, not copper.
- In Wilson's disease, copper accumulates in hepatocytes, which would not stain positive with Prussian blue.
*Panacinar emphysema*
- **Panacinar emphysema** is primarily associated with **alpha-1 antitrypsin deficiency**, a genetic disorder affecting elastic tissue in the lungs.
- It has no direct association with copper metabolism or Wilson's disease.
*Increased serum ceruloplasmin*
- **Ceruloplasmin** is a copper-carrying protein, and in Wilson's disease, the **serum ceruloplasmin level is typically reduced**, not increased.
- This reduction is due to impaired copper incorporation into ceruloplasmin by the dysfunctional ATP7B protein.
More Pancreatic diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.