Male reproductive pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Male reproductive pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Male reproductive pathology US Medical PG Question 1: A 68-year-old man with hypertension comes to the physician because of fatigue and difficulty initiating urination. He wakes up several times a night to urinate. He does not take any medications. His blood pressure is 166/82 mm Hg. Digital rectal examination shows a firm, non-tender, and uniformly enlarged prostate. Which of the following is the most appropriate pharmacotherapy?
- A. Finasteride
- B. α-Methyldopa
- C. Phenoxybenzamine
- D. Terazosin (Correct Answer)
- E. Tamsulosin
Male reproductive pathology Explanation: ***Terazosin***
- **Terazosin** is an alpha-1 blocker that relaxes the smooth muscles in the prostate and bladder neck, improving urine flow and relieving symptoms of **benign prostatic hyperplasia (BPH)**.
- It also has the added benefit of lowering blood pressure, making it suitable for this patient with both **BPH** and **hypertension**.
*Finasteride*
- **Finasteride** is a 5-alpha reductase inhibitor that reduces prostate volume by inhibiting the conversion of testosterone to **dihydrotestosterone (DHT)**.
- While effective for **BPH**, it takes longer to show benefits (6-12 months) and does not address the patient's **hypertension**.
*α-Methyldopa*
- **α-Methyldopa** is a centrally acting alpha-2 adrenergic agonist used to treat **hypertension**, particularly in pregnancy.
- It does not have a direct effect on prostate smooth muscle and would not alleviate the patient's urinary symptoms.
*Phenoxybenzamine*
- **Phenoxybenzamine** is a non-selective, irreversible alpha-adrenergic blocker primarily used for **pheochromocytoma** to control blood pressure.
- Its non-selective nature and side effect profile make it less suitable for chronic management of **BPH** and **hypertension** compared to selective alpha-1 blockers.
*Tamsulosin*
- **Tamsulosin** is a selective alpha-1A adrenergic blocker that specifically targets the prostate, rapidly improving **BPH** symptoms with less effect on blood pressure.
- While it effectively treats **BPH**, unlike terazosin, it does not offer the additional advantage of lowering the patient's elevated blood pressure.
Male reproductive pathology US Medical PG Question 2: A 3-year-old boy was brought in by his parents for undescended testes. The physical examination showed an absence of the left testis in the scrotum. Inguinal swelling was noted on the left side and was surgically corrected. Which of the following conditions will most likely occur in the later stages of his life?
- A. Epididymitis
- B. Testicular cancer (Correct Answer)
- C. Varicocele
- D. Torsion testis
- E. Spermatocele
Male reproductive pathology Explanation: ***Testicular cancer***
- Undescended testes (**cryptorchidism**) are a major risk factor for developing **testicular cancer**, even after surgical correction (**orchidopexy**).
- The risk is higher for both the undescended and the contralateral descended testicle, suggesting a potential underlying developmental abnormality.
*Epididymitis*
- **Epididymitis** is an inflammation of the **epididymis**, usually caused by bacterial infection, and is not a common long-term complication of surgically corrected undescended testes.
- While it can cause scrotal pain and swelling, it is not directly linked to the history of cryptorchidism in this context.
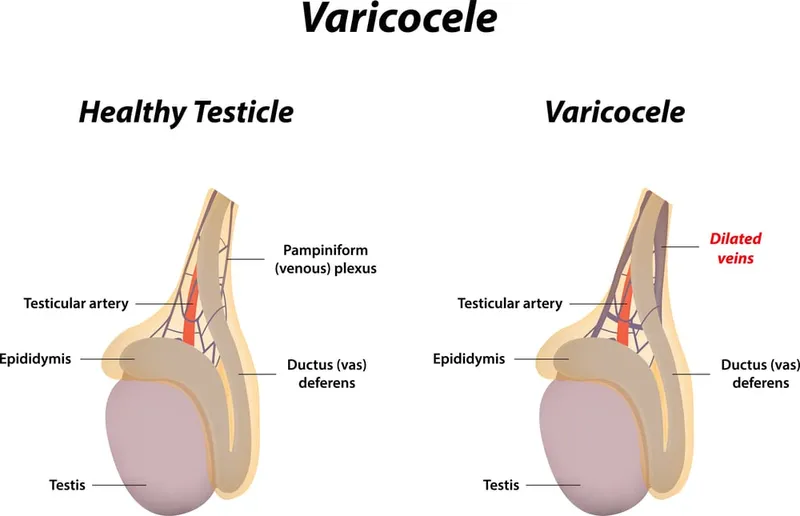
*Varicocele*
- A **varicocele** is an enlargement of veins within the **spermatic cord**, often compared to a "bag of worms," and is a common cause of **male infertility**.
- It is not typically associated with a history of undescended testes, and its development is independent of whether the testis was surgically brought into the scrotum.
*Torsion testis*
- **Testicular torsion** is a surgical emergency involving the twisting of the **spermatic cord**, which cuts off the blood supply to the testicle.
- While it can occur in individuals with undescended testes, surgical correction does not significantly increase the lifetime risk beyond the general population, and it is a sudden event rather than a long-term consequence.
*Spermatocele*
- A **spermatocele** is a benign, sperm-containing cyst that develops in the **epididymis**, usually causing a painless lump above the testicle.
- These cysts are generally not a long-term complication of undescended testes or their surgical correction.
Male reproductive pathology US Medical PG Question 3: A 67-year-old man comes to the physician because of a 3-month history of difficulty initiating urination. He wakes up at least 3–4 times at night to urinate. Digital rectal examination shows a symmetrically enlarged, nontender prostate with a rubbery consistency. Laboratory studies show a prostate-specific antigen level of 2.1 ng/mL (N < 4). Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Lymphocytic infiltration of anterior prostatic lobe stroma
- B. Hyperplasia of lateral prostatic lobe tissue
- C. Infiltrating dysplasia of posterior prostatic lobe epithelium
- D. Infiltrating neoplasia of bladder urothelium
- E. Hypertrophy of middle prostatic lobe tissue (Correct Answer)
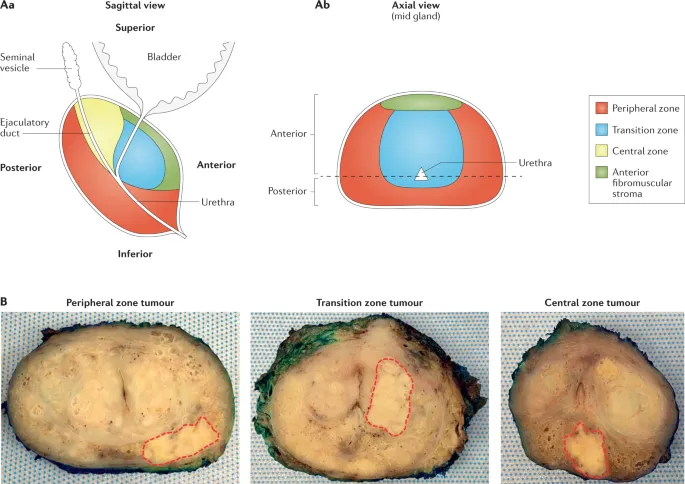
Male reproductive pathology Explanation: ***Hypertrophy of middle prostatic lobe tissue***
- This patient's symptoms of **difficulty initiating urination** and **nocturia** are classic for **benign prostatic hyperplasia (BPH)**.
- The **middle lobe** enlargement is particularly significant because it can **protrude into the bladder neck**, directly causing **urethral obstruction** and the obstructive voiding symptoms seen here.
- The digital rectal exam finding of a **symmetrically enlarged, nontender prostate** with a **rubbery consistency** is characteristic of BPH.
- The **normal PSA level** (2.1 ng/mL) supports a benign process.
*Lymphocytic infiltration of anterior prostatic lobe stroma*
- **Lymphocytic infiltration** of the prostate is consistent with **prostatitis**, which would typically present with **pain, fever, and dysuria**, not just obstructive symptoms.
- The **nontender prostate** on examination argues against prostatitis.
*Hyperplasia of lateral prostatic lobe tissue*
- While **lateral lobe hyperplasia** (transition zone) is the **most common finding in BPH**, this option is less specific to the obstructive symptoms described.
- BPH typically involves both lateral and middle lobes, but **middle lobe** enlargement more directly causes **bladder outlet obstruction** by protruding into the bladder neck.
- Lateral lobe hyperplasia causes obstruction by compressing the prostatic urethra but is less likely to cause the severe obstructive symptoms without middle lobe involvement.
*Infiltrating dysplasia of posterior prostatic lobe epithelium*
- **Dysplasia** in the posterior lobe (peripheral zone) suggests a **premalignant condition** or **early prostate cancer**, which would more likely cause an **asymmetric, firm, or nodular prostate** on DRE.
- The **normal PSA** and **benign examination findings** do not suggest malignancy.
*Infiltrating neoplasia of bladder urothelium*
- **Bladder cancer** typically presents with **painless hematuria** as its primary symptom, which is not mentioned here.
- The **DRE findings** of prostatic enlargement point to prostatic, not bladder, pathology.
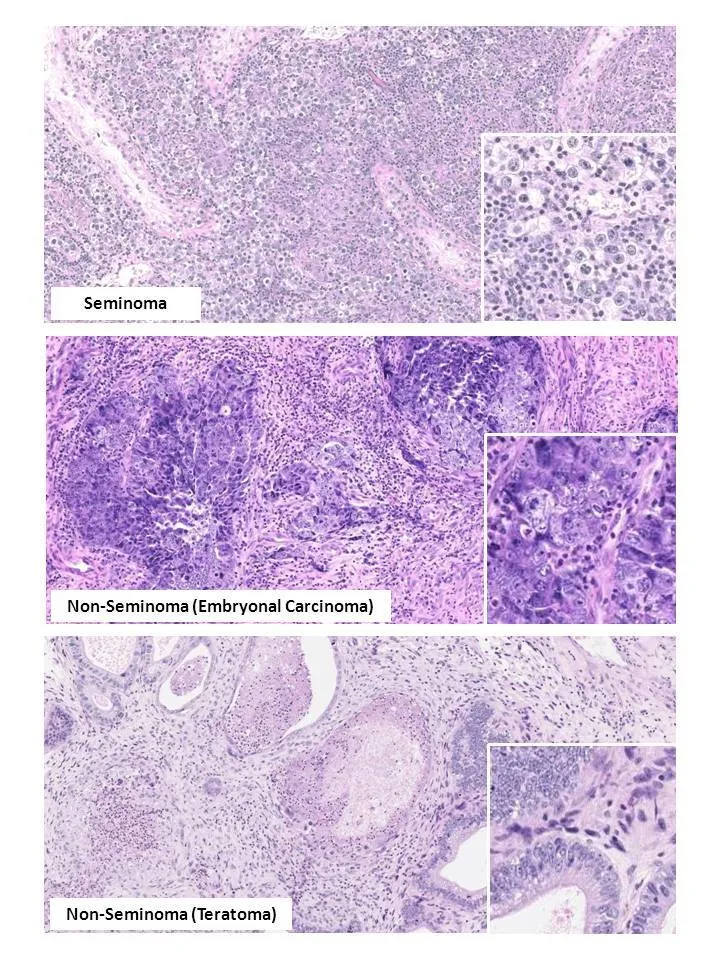
Male reproductive pathology US Medical PG Question 4: A 28-year-old man comes to the physician because of a 2-week history of testicular swelling and dull lower abdominal discomfort. Physical examination shows a firm, nontender left testicular nodule. Ultrasonography of the scrotum shows a well-defined hypoechoic lesion of the left testicle. Serum studies show an elevated β-hCG concentration and a normal α-fetoprotein concentration. The patient undergoes a radical inguinal orchiectomy. Histopathologic examination of the surgical specimen shows a mixed germ cell tumor with invasion of adjacent lymphatic vessels. Further evaluation is most likely to show malignant cells in which of the following lymph node regions?
- A. External iliac
- B. Deep inguinal
- C. Para-aortic (Correct Answer)
- D. Mediastinal
- E. Internal iliac
Male reproductive pathology Explanation: ***Para-aortic***
- Testicular lymphatic drainage primarily follows the **gonadal vessels** back to the para-aortic lymph nodes (also known as retroperitoneal lymph nodes).
- This is the **most common site** for metastatic spread of testicular germ cell tumors.
*External iliac*
- The external iliac lymph nodes primarily drain structures in the pelvis and lower limbs, such as the bladder and vagina, not the testes.
- While they can be involved in advanced pelvic malignancies, they are not the primary drainage site for testicular cancer.
*Deep inguinal*
- The deep inguinal lymph nodes primarily drain the superficial inguinal lymph nodes, which receive lymphatic drainage from the penis, scrotum (superficial layers), and perineum.
- Testicular lymphatics bypass the inguinal nodes unless there is scrotal invasion or prior surgery involving the scrotum.
*Mediastinal*
- Mediastinal lymph nodes are involved in the lymphatic drainage of thoracic organs and can be affected in later stages of testicular cancer if there is widespread metastatic disease, particularly to the lungs.
- However, they are not the initial or primary site of lymphatic spread from testicular tumors.
*Internal iliac*
- The internal iliac lymph nodes primarily drain pelvic organs and the deep perineum.
- While they may be involved in some pelvic cancers, they are not the primary lymphatic drainage site for the testes.
Male reproductive pathology US Medical PG Question 5: A 16-year-old boy comes to the physician because of painless enlargement of his left testis for the past 2 weeks. The patient reports that the enlargement is worse in the evenings, especially after playing soccer. He has not had any trauma to the testes. There is no personal or family history of serious illness. Vital signs are within normal limits. Examination shows multiple cord-like structures above the left testes. The findings are more prominent while standing. The cord-like structures disappear in the supine position. The testes are normal on palpation. The patient is at greatest risk of developing which of the following complications?
- A. Testicular torsion
- B. Erectile dysfunction
- C. Testicular tumor
- D. Infertility (Correct Answer)
- E. Bowel strangulation
Male reproductive pathology Explanation: ***Infertility***
- The patient's presentation of a **painless left testicular enlargement** with **"bag of worms"** feeling that is more prominent when standing and disappears when supine is classic for a **varicocele**.
- Varicoceles increase scrotal temperature, which can impair spermatogenesis and lead to **reduced sperm count** and motility, thus increasing the risk of infertility.
*Testicular torsion*
- Testicular torsion typically presents with **sudden onset**, **severe testicular pain** and swelling, often associated with nausea and vomiting.
- The physical examination findings of a varicocele, specifically the **painless nature** and the **disappearance of swelling in the supine position**, rule out torsion.
*Erectile dysfunction*
- While hormonal imbalances can sometimes be associated with severe varicoceles due to Leydig cell dysfunction, **erectile dysfunction is not a direct or common complication** of varicocele in adolescents.
- Erectile dysfunction is more commonly related to psychological factors, vascular issues, or systemic diseases.
*Testicular tumor*
- Testicular tumors usually present as a **painless, firm mass** within the testis itself, which does not typically change with position.
- The description of **"cord-like structures above the testes"** that disappear in the supine position is inconsistent with a solid testicular mass.
*Bowel strangulation*
- Bowel strangulation involves compromised blood supply to a segment of the bowel, often within a hernia, leading to severe abdominal pain, nausea, and vomiting.
- The symptoms described are localized to the scrotum and are not indicative of an abdominal emergency like bowel strangulation or an incarcerated hernia.
Male reproductive pathology US Medical PG Question 6: A 25-year-old man presents to his primary care provider complaining of scrotal swelling. He is a college student and plays basketball with his friends regularly. Two days ago, he sustained an injury close to his thigh. He does not have any significant past medical history. Today, his vitals are normal. A focused scrotal examination reveals a firm painless lump on the right testicle which is irregular and small. Ultrasound of the scrotum reveals a vascular 0.6 x 0.5 cm testicular mass. A pelvic lymph node exam is negative. He undergoes a radical orchiectomy and subsequent histopathological examination reveals sheets of small cuboidal cells, multinucleated cells, and large eosinophilic cells with pleomorphic nuclei consistent with choriocarcinoma. Which of the following tumor marker is most likely elevated in this patient?
- A. Placental alkaline phosphatase
- B. Prostate-specific antigen
- C. Carcinoembryonic antigen
- D. Testosterone
- E. Beta-human chorionic gonadotropin (Correct Answer)
Male reproductive pathology Explanation: ***Beta-human chorionic gonadotropin***
- **Choriocarcinoma** is a rare and aggressive type of germ cell tumor that secretes **beta-human chorionic gonadotropin (β-hCG)**, which serves as a crucial tumor marker for diagnosis and monitoring.
- The presence of multinucleated cells and large eosinophilic cells (syncytiotrophoblasts) in the histopathology is characteristic of choriocarcinoma, and these cells are responsible for β-hCG production.
*Placental alkaline phosphatase*
- **Placental alkaline phosphatase (PLAP)** is primarily associated with **seminoma**, another type of testicular germ cell tumor, but is not typically elevated in choriocarcinoma.
- While PLAP can be detected in some non-seminomatous germ cell tumors, it is not the primary or most sensitive marker for choriocarcinoma.
*Prostate-specific antigen*
- **Prostate-specific antigen (PSA)** is a tumor marker used for the screening and monitoring of **prostate cancer** and is not associated with testicular germ cell tumors.
- Testicular pathology would not lead to an elevation of PSA.
*Carcinoembryonic antigen*
- **Carcinoembryonic antigen (CEA)** is a tumor marker commonly associated with **colorectal cancer**, as well as other adenocarcinomas such as those of the lung, breast, and pancreas, but not testicular cancers.
- Its elevation would not be expected in a patient with choriocarcinoma.
*Testosterone*
- **Testosterone** is the primary male sex hormone produced by the testicles and adrenal glands; its levels can be affected by testicular pathologies but it is **not a tumor marker** for choriocarcinoma.
- While some testicular tumors can lead to hormonal imbalances, testosterone itself does not serve as a diagnostic or monitoring marker for testicular choriocarcinoma.
Male reproductive pathology US Medical PG Question 7: A 62-year-old man seeks evaluation at an outpatient clinic for a single, red, crusty lesion on the shaft of his penis and a similar lesion on the middle finger of his left hand. He recently immigrated to the US from Africa. The lesions are painless and the physicians in his country treated him for syphilis and eczema, with no improvement. He lives with his 4th wife. He smokes 2 packs of cigarette per day and has been doing so for the last 30 years. He is not aware of any family members with malignancies or hereditary diseases. The physical examination is remarkable for an erythematous plaque, with areas of crusting, oozing, and irregular borders on the dorsal surface of the penile shaft and a similar lesion on his left middle finger (shown in the picture). The regional lymph nodes are not affected. A biopsy is obtained and the pathologic evaluation reveals cells with nuclear hyperchromasia, multinucleation, and increased mitotic figures within the epidermis. What is the most likely diagnosis?
- A. Bowen's disease (Correct Answer)
- B. Bowenoid papulosis
- C. Erythroplasia of Queyrat
- D. Lichen sclerosus
- E. Condyloma acuminata
Male reproductive pathology Explanation: ***Bowen's disease***
- The patient presents with **solitary, erythematous, crusty lesions on the penile shaft and finger**, which are characteristic of Bowen's disease, an in situ squamous cell carcinoma. The histological findings of **nuclear hyperchromasia, multinucleation, and increased mitotic figures within the epidermis** further confirm this diagnosis.
- The **lack of improvement with syphilis and eczema treatments** and the patient's **smoking history** (a risk factor for SCC) support this diagnosis over benign conditions.
*Bowenoid papulosis*
- This condition typically presents as **multiple, small, reddish-brown to violaceous papules**, often in the genital area of younger individuals.
- Unlike Bowen's disease, it is generally considered a **benign or low-grade intraepithelial neoplasia** with a lower risk of progression to invasive cancer.
*Erythroplasia of Queyrat*
- This is a form of **squamous cell carcinoma in situ** that specifically affects the **glans penis or prepuce**, presenting as a well-demarcated, velvety, erythematous patch.
- While histologically similar to Bowen's disease, the patient's lesion is on the **penile shaft and finger**, making Bowen's disease a more encompassing diagnosis for both sites.
*Lichen sclerosus*
- This is a **chronic inflammatory skin condition** characterized by **atrophic, white, sclerotic plaques**, often on the genitals.
- It does not present with the **crusting, oozing, and irregular borders** described, nor the specific histological features of squamous cell carcinoma in situ.
*Condyloma acuminata*
- These are **genital warts caused by HPV**, appearing as soft, flesh-colored, verrucous papules or plaques.
- They typically lack the **crusting, oozing, and histological features of severe atypia and increased mitotic figures** seen in this patient's biopsy.
Male reproductive pathology US Medical PG Question 8: A 67-year-old man presents to his primary care physician complaining of frequent urination overnight. He states that for several years he has had trouble maintaining his urine stream along with the need for frequent urination, but the nighttime urination has only recently started. The patient also states that he has had 2 urinary tract infections in the last year, which he had never had previously. On exam, his temperature is 98.8°F (37.1°C), blood pressure is 124/68 mmHg, pulse is 58/min, and respirations are 13/min. On digital rectal exam, the prostate is enlarged but feels symmetric and smooth. Which of the following is a possible consequence of this condition?
- A. Increased serum creatinine (Correct Answer)
- B. Malignant transformation
- C. Increased serum AFP
- D. Increased serum hCG
- E. Increased serum ALP
Male reproductive pathology Explanation: ***Increased serum creatinine***
- Chronic **urinary retention** due to benign prostatic hyperplasia (BPH) can lead to **hydronephrosis** and **renal parenchymal damage**, impairing kidney function and increasing serum creatinine.
- The patient's symptoms of difficulty maintaining urine stream, frequent urination, and recurrent UTIs suggest BPH, which can progress to urinary obstruction and subsequent kidney dysfunction.
*Malignant transformation*
- **Benign prostatic hyperplasia (BPH)** is a non-malignant condition and does not directly undergo **malignant transformation** into prostate cancer.
- While both BPH and prostate cancer can coexist, BPH itself is not considered a premalignant lesion.
*Increased serum AFP*
- **Alpha-fetoprotein (AFP)** is a tumor marker primarily associated with **hepatocellular carcinoma** and **germ cell tumors** (e.g., testicular cancer).
- It is not associated with benign prostatic hyperplasia (BPH) or its complications.
*Increased serum hCG*
- **Human chorionic gonadotropin (hCG)** is a tumor marker most notably elevated in **choriocarcinoma** and some **germ cell tumors**.
- It has no association with benign prostatic hyperplasia (BPH) or urinary obstruction.
*Increased serum ALP*
- **Alkaline phosphatase (ALP)** can be elevated in conditions affecting the **liver** (e.g., cholestasis) or **bones** (e.g., Paget's disease, osteoblastic metastases).
- While significantly elevated ALP can indicate prostate cancer with **bone metastases**, it is not a direct consequence of uncomplicated benign prostatic hyperplasia (BPH).
Male reproductive pathology US Medical PG Question 9: A 68-year-old man comes to the physician for a routine health maintenance examination. Over the past six months, he has had an increase in the frequency of his bowel movements and occasional bloody stools. He has hypertension, coronary artery disease, and chronic obstructive pulmonary disease. He has smoked one pack of cigarettes daily for 40 years. His current medications include aspirin, lisinopril, and salmeterol. His temperature is 37°C (98.6°F), pulse is 75/min, and blood pressure is 128/75 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no murmurs, rubs, or gallops. The abdomen is soft with no organomegaly. Digital rectal examination shows a large internal hemorrhoid. Test of the stool for occult blood is positive. Which of the following is the most appropriate next step in the management of this patient?
- A. Capsule endoscopy
- B. Rubber band ligation
- C. Hemorrhoidectomy
- D. Barium enema
- E. Colonoscopy (Correct Answer)
Male reproductive pathology Explanation: ***Colonoscopy***
- This patient presents with **changes in bowel habits** (increased frequency) and **rectal bleeding** (bloody stools, positive fecal occult blood test), which are classic alarm symptoms for **colorectal cancer**.
- A **colonoscopy** is the most appropriate next step because it allows for direct visualization of the entire colon, biopsy of suspicious lesions, and removal of polyps, which is crucial for diagnosing or ruling out colorectal cancer and other colon pathologies.
*Capsule endoscopy*
- **Capsule endoscopy** is primarily used to evaluate the **small bowel** for obscure GI bleeding, Crohn's disease, or small bowel tumors.
- It is **not effective** for evaluating the colon as it cannot be controlled to visualize the colonic lining thoroughly and cannot perform biopsies.
*Rubber band ligation*
- **Rubber band ligation** is a procedure used to treat **hemorrhoids**, particularly problematic internal hemorrhoids.
- While the patient has an internal hemorrhoid, his new onset of bowel changes and bloody stools warrants a more comprehensive evaluation to rule out other serious conditions like **colorectal cancer** before attributing symptoms solely to hemorrhoids, especially given his age and risk factors.
*Hemorrhoidectomy*
- **Hemorrhoidectomy** is a surgical procedure for treating severe or refractory hemorrhoids.
- Similar to rubber band ligation, performing a hemorrhoidectomy without a prior **colonoscopy** would be inappropriate given the patient's alarm symptoms, as it might delay the diagnosis of a more serious underlying condition.
*Barium enema*
- A **barium enema** is a radiological study that can identify large polyps or masses in the colon, but it has **lower sensitivity** than colonoscopy, especially for smaller lesions.
- It **does not allow for biopsy** of suspicious areas or removal of polyps, which limits its diagnostic and therapeutic utility compared to colonoscopy for these symptoms.
Male reproductive pathology US Medical PG Question 10: A 54-year-old woman comes to the physician because of an ulcer on her left ankle for 6 years. She has had multiple ulcers over her left lower extremity during this period that have subsided with wound care and dressing. She has type 2 diabetes mellitus and gastroesophageal reflux disease. Current medications include metformin, sitagliptin, and omeprazole. She appears anxious. She is 162 cm (5 ft 4 in) tall and weighs 89 kg (196 lb); BMI is 34 kg/m2. Vital signs are within normal limits. Examination shows a 7.5-cm (3-in) ulcer with elevated, indurated margins and a necrotic floor above the left medial malleolus. There are multiple dilated, tortuous veins along the left lower extremity. There is 2+ pretibial edema of the lower extremities bilaterally. The skin around the left ankle appears darker than the right and there are multiple excoriation marks. Cardiopulmonary examination shows no abnormalities. Which of the following is the most appropriate next step in management of this patient's current condition?
- A. Trendelenburg test
- B. Punch biopsy (Correct Answer)
- C. Digital subtraction angiography
- D. Perthes test
- E. CT scan of the left leg
Male reproductive pathology Explanation: ***Punch biopsy***
- A 6-year history of a non-healing **ulcer with elevated, indurated margins and a necrotic floor** is highly suspicious for **Marjolin's ulcer**, a type of squamous cell carcinoma arising in chronic wounds.
- A **punch biopsy** is the most appropriate next step to obtain a tissue diagnosis and confirm or rule out malignancy.
*Trendelenburg test*
- The Trendelenburg test assesses **venous valve competence** in superficial veins.
- While this patient has signs of **venous insufficiency** (dilated veins, edema, skin changes), the primary concern is the non-healing, suspicious ulcer, for which biopsy is more urgent.
*Digital subtraction angiography*
- Digital subtraction angiography is used to visualize **arterial blood flow** and diagnose peripheral artery disease.
- Although the patient has diabetes, there are no classic signs of significant arterial insufficiency (e.g., claudication, cold limb, diminished pulses), and the ulcer characteristics are more suggestive of malignancy or venous etiology.
*Perthes test*
- The Perthes test evaluates the **patency of deep veins** and the function of communicating veins by assessing changes in superficial venous distension after exercise with a tourniquet.
- Similar to the Trendelenburg test, it focuses on venous hemodynamics, which is secondary to the suspicion of malignancy in a chronic, non-healing ulcer.
*CT scan of the left leg*
- A CT scan can assess the **extent of soft tissue destruction or bone involvement** if malignancy is suspected or confirmed.
- However, it is not the initial diagnostic step for determining the nature of the ulcer itself; a **tissue biopsy** is required for definitive diagnosis.
More Male reproductive pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.