Liver pathology (hepatitis, cirrhosis) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Liver pathology (hepatitis, cirrhosis). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 1: A 57-year-old man comes to the physician for a follow-up visit. Serum studies show:
AST 134 U/L
ALT 152 U/L
Hepatitis B surface antigen Positive
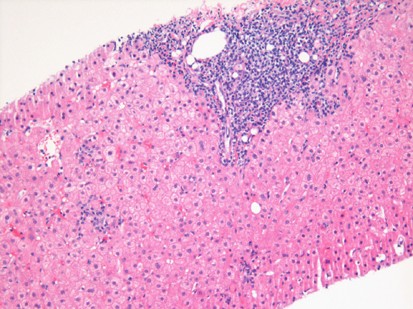
A photomicrograph of the microscopic findings of a liver biopsy is shown. These biopsy findings are most characteristic of which of the following types of inflammatory reactions?
- A. Malignant transformation
- B. Granulomatous inflammation
- C. Chronic inflammation (Correct Answer)
- D. Acute inflammation
- E. Ischemic necrosis
Liver pathology (hepatitis, cirrhosis) Explanation: ***Chronic inflammation***
- The combination of **elevated AST/ALT** and **positive Hepatitis B surface antigen** indicates persistent liver damage due to a chronic viral infection.
- Liver **biopsy findings** in such cases typically reveal **lymphocytic infiltrates**, fibrosis, and ongoing hepatocellular injury, which are hallmarks of chronic inflammation.
*Malignant transformation*
- While chronic viral hepatitis can lead to **hepatocellular carcinoma**, the question describes inflammatory findings, not **neoplastic changes** like cellular atypia or uncontrolled proliferation.
- **Malignant transformation** would present with disorganized architectural patterns and significant cellular pleomorphism.
*Granulomatous inflammation*
- **Granulomatous inflammation** is characterized by aggregates of activated macrophages (epithelioid cells), often with giant cells, which are not the primary feature described in chronic viral hepatitis.
- This type of inflammation is typically seen in diseases like **tuberculosis**, sarcoidosis, or fungal infections, not usually in viral hepatitis.
*Acute inflammation*
- **Acute inflammation** would present with a predominance of **neutrophils**, pronounced edema, and rapid onset of symptoms.
- The elevated liver enzymes and positive HBsAg suggest ongoing, long-term inflammation, which is characteristic of a chronic process.
*Ischemic necrosis*
- **Ischemic necrosis** is caused by a lack of blood supply, leading to cell death, and would typically present with **coagulative necrosis** of hepatocytes with minimal inflammatory infiltrate in the early stages.
- The clinical picture of chronic hepatitis B infection does not primarily involve an acute ischemic event affecting the liver.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 2: A 38-year-old woman comes to the physician because of a 3-month history of moderate abdominal pain that is unresponsive to medication. She has a history of two spontaneous abortions at 11 and 12 weeks' gestation. Ultrasound examination of the abdomen shows normal liver parenchyma, a dilated portal vein, and splenic enlargement. Upper endoscopy shows dilated submucosal veins in the lower esophagus. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased serum bilirubin levels
- B. Increased prothrombin time
- C. Thrombocytopenia (Correct Answer)
- D. Hepatic venous congestion
- E. Councilman bodies
Liver pathology (hepatitis, cirrhosis) Explanation: ***Thrombocytopenia***
- The patient's **recurrent spontaneous abortions** suggest **antiphospholipid syndrome (APS)**, a hypercoagulable state that predisposes to both arterial and venous thrombosis.
- APS likely caused **portal vein thrombosis**, leading to **prehepatic portal hypertension** (dilated portal vein, esophageal varices, and splenomegaly) with **normal liver parenchyma**.
- The **splenomegaly** causes **hypersplenism**, resulting in **thrombocytopenia** due to splenic sequestration and increased destruction of platelets.
- While APS can also cause immune-mediated thrombocytopenia directly, the primary mechanism here is hypersplenism secondary to portal hypertension.
*Increased serum bilirubin levels*
- Elevated bilirubin indicates **hepatocellular dysfunction** or **biliary obstruction**.
- The ultrasound shows **normal liver parenchyma**, making significant hepatocellular damage unlikely.
- Portal vein thrombosis without liver parenchymal disease does not typically cause hyperbilirubinemia.
*Increased prothrombin time*
- Prolonged PT reflects impaired **hepatic synthesis of coagulation factors** (II, VII, IX, X).
- With **normal liver parenchyma** on imaging, synthetic liver function should be preserved.
- Portal vein thrombosis alone does not impair hepatocyte function or coagulation factor synthesis.
*Hepatic venous congestion*
- This finding is characteristic of **Budd-Chiari syndrome** (hepatic vein thrombosis), which presents with hepatomegaly, ascites, and signs of hepatic outflow obstruction.
- The patient's findings (dilated **portal vein**, normal liver parenchyma) indicate **portal vein thrombosis** causing **prehepatic portal hypertension**, not posthepatic venous congestion.
*Councilman bodies*
- These are **eosinophilic apoptotic hepatocytes** seen in acute liver injury (viral hepatitis, yellow fever, toxic injury).
- **Normal liver parenchyma** on ultrasound excludes significant hepatocellular necrosis.
- This finding is unrelated to thrombotic disorders or portal hypertension.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 3: A 57-year-old man presents with fever and yellow discoloration of the skin for the past 4 days. He denies any recent weight loss or changes in urine or stool color. His past medical history is unremarkable. He admits to drinking about 130 g/day of alcohol and says he has been doing so for the past 25 years. His wife who is accompanying him during this visit adds that once her husband drank 15 cans of beer at a funeral. The patient also reports a 10-pack-year smoking history. His vital signs include: pulse 98/min, respiratory rate 13/min, temperature 38.2°C (100.8°F) and blood pressure 120/90 mm Hg. On physical examination, the patient appears jaundiced and is ill-appearing. Sclera is icteric. Abdominal examination reveals tenderness to palpation in the right upper quadrant with no rebound or guarding. Percussion reveals significant hepatomegaly extending 3 cm below the right costal margin. Laboratory studies are significant for the following:
Sodium 135 mEq/L
Potassium 3.5 mEq/L
ALT 240 U/L
AST 500 U/L
A liver biopsy is obtained but the results are pending. Which of the following would most likely be seen in this patient's biopsy?
- A. Steatosis alone
- B. Hürthle cells
- C. 'Florid' bile duct lesion
- D. Gaucher cells
- E. Mallory-Denk bodies (Correct Answer)
Liver pathology (hepatitis, cirrhosis) Explanation: ***Mallory-Denk bodies***
- The patient's history of heavy alcohol consumption, fever, **jaundice**, elevated AST and ALT with an **AST:ALT ratio > 2:1**, and hepatomegaly are highly indicative of **alcoholic hepatitis**.
- **Mallory-Denk bodies (MDBs)**, or alcoholic hyaline, are characteristic histological findings in alcoholic liver disease, representing damaged intermediate filaments within hepatocytes.
*Steatosis alone*
- While **steatosis (fatty liver)** is the earliest and most common response to alcohol, the presence of fever, jaundice, and marked transaminitis (especially the **AST:ALT ratio**) suggests a more severe, active inflammatory process like alcoholic hepatitis rather than isolated steatosis.
- **Simple steatosis** typically yields milder symptoms and less pronounced liver enzyme elevations.
*Hürthle cells*
- **Hürthle cells** are typically found in the **thyroid gland** and are associated with thyroid conditions like Hashimoto's thyroiditis or Hürthle cell carcinoma.
- They are not a feature of liver biopsies or alcoholic liver disease.
*'Florid' bile duct lesion*
- A **"florid" bile duct lesion** is characteristic of **primary biliary cholangitis (PBC)**, an autoimmune liver disease affecting small bile ducts.
- The patient's clinical presentation (heavy alcohol use, AST:ALT ratio > 2) does not align with PBC.
*Gaucher cells*
- **Gaucher cells** are **lipid-laden macrophages** found in individuals with **Gaucher disease**, a lysosomal storage disorder.
- They are typically seen in the bone marrow, spleen, and liver in the context of this specific genetic disorder, not alcoholic hepatitis.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 4: A 58-year-old man with a history of alcoholism is hospitalized with acute onset nausea and hematemesis. On admission, his vitals are as follows: blood pressure 110/70 mm Hg, heart rate 88/min, respiratory rate 16/min, and temperature 37.8℃ (100.0℉). Physical examination shows jaundice, palmar erythema, widespread spider angiomata, abdominal ascites, and visibly distended superficial epigastric veins. Abdominal ultrasound demonstrates portal vein obstruction caused by liver cirrhosis. Where in the liver would you find the earliest sign of fibrous deposition in this patient?
- A. Lumen of sinusoids
- B. Lumen of bile ducts
- C. Portal field
- D. Perisinusoidal space (Correct Answer)
- E. Interlobular connective tissue
Liver pathology (hepatitis, cirrhosis) Explanation: ***Perisinusoidal space***
- In cirrhosis, **hepatic stellate cells** (Ito cells) in the **perisinusoidal space** (space of Disse) are activated by liver injury.
- These activated cells transform into myofibroblast-like cells, leading to increased **collagen production** and fibrous deposition, initially in the space of Disse.
*Lumen of sinusoids*
- The lumen of the sinusoids is where blood from the portal vein and hepatic artery mixes and flows past hepatocytes.
- Fibrous deposition does not typically begin within the **lumen** itself; rather, it occurs in the surrounding tissue.
*Lumen of bile ducts*
- Bile ducts are involved in the transport of bile, and while certain cholangiopathies can cause fibrosis, the primary site of early fibrosis in **alcoholic cirrhosis** is not within the bile duct lumens.
- Fibrosis associated with bile ducts is usually seen in **biliary cirrhosis**, not directly in the lumen.
*Portal field*
- The portal field (or portal triad) contains the portal vein, hepatic artery, and bile duct. While fibrosis eventually extends to and connects portal fields, the **earliest microscopic changes** in alcoholic liver disease begin in the pericentral/perisinusoidal regions.
- Extensive fibrosis in the portal fields is characteristic of later stages of cirrhosis, forming **bridging fibrosis**.
*Interlobular connective tissue*
- Interlobular connective tissue provides structural support between liver lobules.
- While fibrosis can eventually infiltrate and replace this tissue, the **initial deposition** in alcoholic cirrhosis specifically targets the perisinusoidal space.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 5: A 58-year-old man with liver cirrhosis presents to his primary care physician complaining of increased abdominal girth and early satiety. He drinks 2–4 glasses of wine with dinner and recalls having had abnormal liver enzymes in the past. Vital signs include a temperature of 37.1°C (98.7°F), blood pressure of 110/70 mm Hg, and a pulse of 75/min. Physical examination reveals telangiectasias, mild splenomegaly, palpable firm liver, and shifting dullness. Liver function is shown:
Total bilirubin 3 mg/dL
Aspartate aminotransferase (AST) 150 U/L
Alanine aminotransferase (ALT) 70 U/L
Total albumin 2.5 g/dL
Abdominal ultrasonography confirms the presence of ascites. Diagnostic paracentesis is performed and its results are shown:
Polymorphonuclear cell count 10 cells/mm
Ascitic protein 1 g/dL
Which of the following best represents the mechanism of ascites in this patient?
- A. Peritoneal tuberculosis
- B. High sinusoidal pressure (Correct Answer)
- C. Pancreatic disease
- D. Serositis
- E. Peritoneal carcinomatosis
Liver pathology (hepatitis, cirrhosis) Explanation: ***High sinusoidal pressure***
- In **liver cirrhosis**, the fibrotic changes and regenerating nodules increase resistance to blood flow, leading to **portal hypertension** and increased pressure in the hepatic sinusoids.
- This elevated pressure drives fluid from the sinusoids into the abdominal cavity, forming **ascites**.
*Peritoneal tuberculosis*
- This condition typically presents with **ascitic fluid protein levels above 2.5 g/dL** and a significantly elevated **lymphocytic cell count** in the ascitic fluid.
- The patient's ascitic protein level is 1 g/dL, and the polymorphonuclear cell count is low, making this diagnosis less likely.
*Pancreatic disease*
- Pancreatic ascites results from a leaking **pancreatic duct or pseudocyst**, leading to ascitic fluid with very high **amylase levels** and often a high protein content.
- While the patient has alcohol use, the clinical presentation and paracentesis results point more strongly towards liver-related ascites rather than pancreatic.
*Serositis*
- **Serositis** involves inflammation of serous membranes, often seen in autoimmune diseases, and can cause ascites with a higher protein content and inflammatory cells.
- The patient's primary symptoms and signs are consistent with advanced liver disease, not systemic inflammatory serositis.
*Peritoneal carcinomatosis*
- **Peritoneal carcinomatosis** usually leads to ascites with a **high protein content** (>2.5 g/dL), sometimes with **malignant cells** present in the ascitic fluid cytology.
- The low ascitic fluid protein and absence of other signs of malignancy make this an unlikely cause.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 6: A 33-year-old female comes to her primary care physician with complaints of fatigue and nausea. She has also noticed that her skin tone is darker than it used to be. On exam, the physician notes that the woman appears to be jaundiced and obtains liver enzymes which demonstrate an elevated AST and ALT. Further testing subsequently confirms the diagnosis of hepatitis B (HBV). The woman is extremely concerned about transmitting this disease to her loved ones and ask how HBV is transmitted. By which of the following routes can HBV be spread? (I) blood, (II) sexual contact, (III) maternal-fetal, and/or (IV) breast milk?
- A. II, III
- B. I, II, III, IV
- C. I, II, III (Correct Answer)
- D. I, III, IV
- E. I only
Liver pathology (hepatitis, cirrhosis) Explanation: ***I, II, III***
- **Hepatitis B virus (HBV)** is primarily transmitted through contact with infected **blood** or other bloody body fluids (e.g., semen, vaginal secretions), making routes I (blood) and II (sexual contact) major modes of transmission.
- **Maternal-fetal transmission** (route III) can occur during childbirth, especially if the mother has high viral loads, although *in utero* transmission is rare.
*II, III*
- This option is incorrect because it omits **blood transmission (I)**, which is a major route for HBV spread through shared needles, transfusions, or open wounds.
- While sexual and maternal-fetal transmissions are significant, they do not account for all primary modes of spread.
*I, II, III, IV*
- This option is incorrect because while routes I, II, and III are valid, **breast milk (IV)** is generally *not* considered a significant route for HBV transmission.
- Studies have shown a very low, if any, risk of HBV transmission through breast milk, and breastfeeding is typically safe for HBV-positive mothers, especially if the infant is vaccinated.
*I, III, IV*
- This option is incorrect because it includes **breast milk (IV)**, which is not a clinically significant route of transmission, and it excludes **sexual contact (II)**, a very common mode of HBV spread.
- Many HBV infections are acquired through unprotected sexual intercourse with an infected partner.
*I only*
- This option is incorrect as it severely underrepresents the various transmission routes of HBV, omitting **sexual contact (II)** and **maternal-fetal transmission (III)**.
- While blood transmission is critical, HBV is also frequently spread through other bodily fluids and from mother to child.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 7: A 25-year-old man presents to the office for a 3-day history of fever and fatigue. Upon further questioning, he says that he also had constant muscular pain, headaches, and fever during these days. He adds additional information by giving a history of regular unprotected sexual relationship with multiple partners. He is a non-smoker and drinks alcohol occasionally. The heart rate is 102/min, respiratory rate is 18/min, temperature is 38.0°C (100.4°F), and blood pressure is 120/80 mm Hg. On physical examination, he is icteric and hepatosplenomegaly is evident with diffuse muscular and abdominal tenderness particularly in the right upper quadrant. The serologic markers show the following pattern:
Anti-HAV IgM negative
HBsAg positive
Anti-HBs negative
IgM anti-HBc positive
Anti-HCV negative
Anti-HDV negative
What is the most likely diagnosis?
- A. Viral hepatitis D
- B. Viral hepatitis C
- C. Viral hepatitis A
- D. Viral hepatitis E
- E. Viral hepatitis B (Correct Answer)
Liver pathology (hepatitis, cirrhosis) Explanation: ***Viral hepatitis B***
- The combination of **HBsAg positive** and **IgM anti-HBc positive** indicates an **acute hepatitis B infection**.
- Symptoms like **fever**, **fatigue**, **muscular pain**, **icterus**, and **hepatosplenomegaly** are consistent with acute viral hepatitis.
*Viral hepatitis D*
- This is ruled out by the **negative Anti-HDV** marker, as hepatitis D requires co-infection with hepatitis B.
- While patients can be co-infected with HBV and HDV, the serology explicitly excludes HDV in this case.
*Viral hepatitis C*
- This is excluded by the **negative Anti-HCV** marker, which would be positive in hepatitis C infection.
- Though sexually transmitted, the serological markers point away from HCV.
*Viral hepatitis A*
- This is ruled out by the **negative Anti-HAV IgM** marker.
- Hepatitis A is typically transmitted via the **fecal-oral route**, which is less consistent with the patient's sexual history.
*Viral hepatitis E*
- While hepatitis E can cause acute hepatitis, it is typically diagnosed by **IgM anti-HEV** antibodies, which are not provided as positive here.
- Transmission is usually **fecal-oral**, which is not the primary risk factor suggested by the patient's history.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 8: Two weeks after returning from vacation in Mexico, a 21-year-old man comes to the emergency department because of malaise, nausea, vomiting, fever, and abdominal pain. He has no history of serious illness and takes no medications. Physical examination shows scleral icterus and right upper quadrant tenderness. The liver is palpated 1.5 cm below the right costal margin. A biopsy specimen of this patient's liver would most likely show which of the following findings?
- A. Piecemeal necrosis and fatty changes
- B. Lymphocytic infiltration and progressive ductopenia
- C. Ballooning degeneration and bridging necrosis (Correct Answer)
- D. Ground glass hepatocytes and apoptotic bodies
- E. Dysplastic hepatocytes with intracellular bile
Liver pathology (hepatitis, cirrhosis) Explanation: ***Ballooning degeneration and bridging necrosis***
- The patient presents with symptoms and signs of **acute viral hepatitis**, characterized by malaise, nausea, vomiting, fever, abdominal pain, scleral icterus, and right upper quadrant tenderness following travel to an endemic area (Mexico). **Ballooning degeneration** of hepatocytes and **bridging necrosis** (necrosis extending between portal tracts and central veins) are classic histological features of severe acute viral hepatitis.
- These findings reflect the **cytopathic effect of the virus** and the host's immune response, leading to hepatocyte injury and extensive liver damage.
*Piecemeal necrosis and fatty changes*
- **Piecemeal necrosis** (also known as interface hepatitis) is characteristic of **chronic hepatitis**, where inflammation at the portal-parenchymal interface leads to destruction of periportal hepatocytes, not typical for acute resolving hepatitis.
- **Fatty changes** (steatosis) are commonly seen in conditions like **alcoholic liver disease** or **non-alcoholic fatty liver disease (NAFLD)**, and are not primary features of acute viral hepatitis.
*Lymphocytic infiltration and progressive ductopenia*
- **Lymphocytic infiltration** is a general feature of many forms of hepatitis, but **progressive ductopenia** (loss of bile ducts) is highly suggestive of **primary biliary cholangitis (PBC)**, an autoimmune condition, or **primary sclerosing cholangitis (PSC)**, which does not fit the acute presentation or travel history.
- These conditions are typically chronic and have different clinical manifestations.
*Ground glass hepatocytes and apoptotic bodies*
- **Ground-glass hepatocytes** are a hallmark feature of **chronic hepatitis B infection**, indicating the accumulation of HBsAg in the endoplasmic reticulum. This is not typical for acute viral hepatitis where the virus may still be replicating rapidly.
- While **apoptotic bodies** (Councilman bodies) can be seen in acute hepatitis, they are not the predominant or most specific finding to describe the widespread damage seen with ballooning degeneration and necrosis.
*Dysplastic hepatocytes with intracellular bile*
- **Dysplastic hepatocytes** are indicative of **precancerous changes** or **hepatocellular carcinoma (HCC)**, usually occurring in the context of chronic liver disease, not acute self-limiting hepatitis.
- While **intracellular bile** might be seen in cholestatic conditions, the combination of dysplastic hepatocytes points away from acute viral hepatitis.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 9: A 37-year-old man presents to an urgent care clinic with complaints of speech problems and yellowing of his eyes for a week. He admits to using illicit intravenous drugs. His vital signs include: blood pressure 110/60 mm Hg, pulse rate 78/min, and respiratory rate 22/min. On examination, the patient appears jaundiced, and his speech is slurred. His liver enzymes and viral markers are as follows:
Aspartate aminotransferase 6,700 IU/L
Alanine aminotransferase 5,000 IU/L
HBsAg Negative
Anti-HBs Negative
Anti-HCV Ab Positive
HCV RNA Positive
If this patient develops chronic hepatitis C infection, he is at risk of developing a secondary dermatological condition. A biopsy of this skin condition would most likely show which of the following findings?
- A. Intraepithelial cleavage with acantholysis
- B. Noncaseating granulomas
- C. Microabscesses with fibrin and neutrophils
- D. Crypt abscesses containing neutrophils
- E. Lymphocytic infiltrate at the dermal-epidermal junction (Correct Answer)
Liver pathology (hepatitis, cirrhosis) Explanation: ***Lymphocytic infiltrate at the dermal-epidermal junction***
- Chronic hepatitis C infection is strongly associated with **lichen planus**, a dermatological condition characterized histologically by a **lymphocytic infiltrate along the dermal-epidermal junction**, often described as a "sawtooth" pattern.
- The history of IV drug use, jaundiced eyes, elevated liver enzymes, and positive HCV RNA confirm a diagnosis of **acute hepatitis C**, which can progress to chronic infection and lead to extrahepatic manifestations like lichen planus.
*Intraepithelial cleavage with acantholysis*
- This finding is characteristic of **pemphigus vulgaris**, an autoimmune blistering disorder where antibodies target desmoglein 3, leading to loss of cohesion between keratinocytes.
- Pemphigus vulgaris is not typically associated with chronic hepatitis C infection.
*Noncaseating granulomas*
- **Noncaseating granulomas** are the hallmark histological feature of **sarcoidosis** and Crohn's disease.
- While sarcoidosis can have cutaneous manifestations, it is not directly linked to chronic hepatitis C in the way lichen planus is.
*Microabscesses with fibrin and neutrophils*
- This description aligns with findings in conditions such as **dermatitis herpetiformis** (neutrophilic infiltrates in dermal papillae) or acute neutrophilic dermatoses, but it is not the characteristic feature of skin conditions directly associated with chronic hepatitis C.
- Skin conditions like vasculitis can also show neutrophilic infiltrates, but the primary association with HCV and the provided options points away from this.
*Crypt abscesses containing neutrophils*
- **Crypt abscesses** are histological features typically found in the intestinal lining in conditions like **ulcerative colitis**, an inflammatory bowel disease.
- This finding is not relevant to dermatological conditions associated with chronic hepatitis C.
Liver pathology (hepatitis, cirrhosis) US Medical PG Question 10: A 59-year-old woman comes to the physician because of progressively worsening coordination and involuntary movements in her left hand for the past 6 months. Her husband also reports that she has been withdrawn and apathetic during this period. She is oriented to time, place, and person. Examination shows a bimanual, rhythmic, low-frequency tremor that is more prominent in the left hand. There is normal range of motion in the arms and legs; active movements are very slow. Muscle strength is normal, and there is increased resistance to passive flexion and extension in the limbs. She walks with a shuffling gait and takes small steps. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Proliferation of beta-adrenergic receptors from excessive circulating T4
- B. Neuronal degeneration due to α-synuclein protein misfolding (Correct Answer)
- C. Accumulation of neurotoxic metabolites secondary to hepatocyte damage
- D. Copper accumulation due to mutations in hepatocyte copper-transporting ATPase
- E. Cerebellar ischemia due to chronic hypertension
Liver pathology (hepatitis, cirrhosis) Explanation: ***Neuronal degeneration due to α-synuclein protein misfolding***
- This describes **Parkinson's disease (PD)**, characterized by the degeneration of dopaminergic neurons in the **substantia nigra** due to the accumulation of misfolded **α-synuclein** into Lewy bodies.
- The patient's symptoms—**bradykinesia (slow movements), resting tremor (rhythmic, low-frequency tremor), rigidity (increased resistance to passive movement), and shuffling gait**—are classic signs of PD. Apathy and withdrawal are common non-motor symptoms.
*Proliferation of beta-adrenergic receptors from excessive circulating T4*
- This describes symptoms of **hyperthyroidism**, which can cause a fine tremor, but not the **low-frequency resting tremor** and **rigidity** seen in this patient.
- Hyperthyroidism is also associated with weight loss, heat intolerance, and tachycardia, which are not mentioned.
*Accumulation of neurotoxic metabolites secondary to hepatocyte damage*
- This is characteristic of **hepatic encephalopathy**, which presents with altered mental status, asterixis (flapping tremor), and generalized slowness.
- However, the patient's specific motor symptoms like **rigidity, shuffling gait**, and a distinct **resting tremor** are not typical features of hepatic encephalopathy.
*Copper accumulation due to mutations in hepatocyte copper-transporting ATPase*
- This describes **Wilson's disease**, an inherited disorder of copper metabolism. It can cause neurological symptoms, including tremor, dystonia, and ataxia, along with liver disease.
- However, the patient's age (59 years) and the specific presentation of a **resting tremor, bradykinesia, and rigidity** are more consistent with Parkinson's disease than Wilson's, which typically presents in younger individuals.
*Cerebellar ischemia due to chronic hypertension*
- **Cerebellar ischemia** would lead to **ataxia, dysarthria, and intention tremor**, which is a tremor that worsens with voluntary movement, unlike the **resting tremor** observed in this patient.
- **Rigidity and bradykinesia** are not primary symptoms of cerebellar lesions.
More Liver pathology (hepatitis, cirrhosis) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.