Kidney diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Kidney diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Kidney diseases US Medical PG Question 1: A 63-year-old man presents with a 2-month history of increasing sensation of fullness involving his left flank. The patient reports recent episodes of constant pain. The patient is hypertensive (145/90 mm Hg) and is currently on medications including losartan and hydrochlorothiazide. His past medical history is otherwise unremarkable. He is a 30-pack-year smoker. His temperature is 37.7°C (99.9°F); pulse, 76/min; and respiratory rate, 14/min. Palpation of the left flank shows a 10 x 10-cm mass. The patient's laboratory parameters are as follows:
Blood
Hemoglobin 19.5 g/dL
Leukocyte count 5,000/mm3
Platelet count 250,000/mm3
Urine
Blood 2+
Protein negative
RBC 45/hpf without dysmorphic features
Abdominal CT scan confirms the presence of a large solid mass originating in the left kidney. These findings are most consistent with which of the following conditions?
- A. Wilms tumor
- B. Transitional cell carcinoma
- C. Adenoma
- D. Renal cell carcinoma (Correct Answer)
- E. Angiomyolipoma
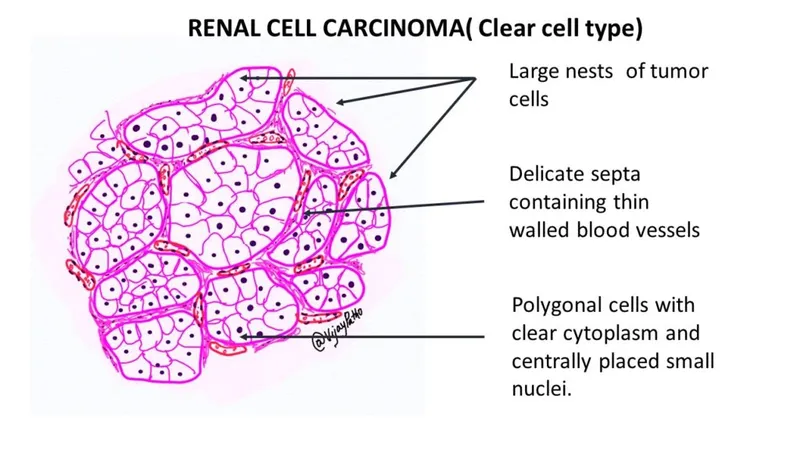
Kidney diseases Explanation: ***Renal cell carcinoma***
- The constellation of **flank pain**, a palpable **flank mass**, and **hematuria** is the classic triad of renal cell carcinoma.
- Additional findings like **hypertension**, **polycythemia** (high hemoglobin of 19.5 g/dL due to erythropoietin production by the tumor), and **smoker status** further support this diagnosis.
*Wilms tumor*
- This is primarily a **childhood tumor**, typically presenting before the age of 5, which is inconsistent with this 63-year-old patient.
- While it can present with a palpable mass and hematuria, the patient's age makes this diagnosis highly unlikely.
*Transitional cell carcinoma*
- This cancer usually arises in the **renal pelvis** or ureter and is strongly associated with smoking and painless gross hematuria.
- However, a large solid parenchymal mass as described by the CT scan points away from transitional cell carcinoma, which generally involves the collecting system.
*Adenoma*
- Renal adenomas are typically **small, benign tumors** that are often found incidentally and rarely cause symptoms like palpable masses or flank pain.
- They are not associated with paraneoplastic syndromes such as polycythemia or significant hypertension secondary to tumor activity.
*Angiomyolipoma*
- These are **benign tumors** composed of fat, smooth muscle, and blood vessels, often associated with **tuberous sclerosis**.
- While they can cause flank pain or hemorrhage, they typically appear as **fat-containing lesions** on imaging, and this patient's presentation with polycythemia and significant hypertension points to a malignant process.
Kidney diseases US Medical PG Question 2: A 32-year-old woman comes to the physician because of flank pain, myalgia, and reddish discoloration of her urine for the past 2 days. One week ago, she had a fever and a sore throat and was prescribed antibiotics. She is otherwise healthy and has no history of serious illness. Her temperature is 37.9°C (100.2°F), pulse is 70/min, and blood pressure is 128/75 mm Hg. Physical examination shows a soft abdomen and no costovertebral angle tenderness. Examination of the mouth and pharynx shows no abnormalities. There is a faint maculopapular rash over the trunk and extremities. Serum creatinine is 2.4 mg/dL. Urinalysis shows:
Protein 2+
Blood 2+
RBC 20–30/hpf
WBC 12/hpf
Bacteria none
Which of the following is the most likely diagnosis?
- A. Thin basement membrane disease
- B. Allergic interstitial nephritis (Correct Answer)
- C. Crystal-induced acute kidney injury
- D. Poststreptococcal glomerulonephritis
- E. Pyelonephritis
Kidney diseases Explanation: ***Allergic interstitial nephritis***
- The development of **flank pain**, **myalgia**, **fever**, and a **maculopapular rash** following a recent antibiotic prescription, along with elevated creatinine and WBCs in urine, is highly suggestive of **allergic interstitial nephritis**.
- **Eosinophils** are often found in the urine, though not explicitly stated here, which further supports this diagnosis due to its association with drug hypersensitivity.
*Thin basement membrane disease*
- This condition typically presents with **isolated microscopic hematuria** and is often asymptomatic, not with acute onset of flank pain, rash, and significant renal dysfunction.
- Serum creatinine is usually normal, unlike the elevated level seen in this patient.
*Crystal-induced acute kidney injury*
- This type of AKI is characterized by the presence of **crystals in the urine** (e.g., uric acid, calcium oxalate), which are not mentioned in the urinalysis.
- While it can cause flank pain, it's typically seen in specific contexts like chemotherapy (tumor lysis syndrome) or **antifreeze ingestion**, which are not present here.
*Poststreptococcal glomerulonephritis*
- Although it can follow a pharyngeal infection, it typically presents with **cola-colored urine** (due to dysmorphic RBCs and casts), **edema**, and **hypertension**.
- The presence of a **rash** and the timing after antibiotic use make allergic interstitial nephritis a more likely diagnosis.
*Pyelonephritis*
- Characterized by **fever**, **flank pain**, and **costovertebral angle tenderness**, which is explicitly noted as absent in this patient.
- Urinalysis typically shows **leukocyturia** and sometimes **bacteriuria** with **nitrites**, but without significant bacteriuria, it is less likely.
Kidney diseases US Medical PG Question 3: A 32-year-old woman presents to the office with complaints of frothy urine and swelling in her body that started 6 days ago. She says that she first noticed the swelling in her face that gradually involved other parts of her body. On further questioning, she gives a history of rheumatoid arthritis for 2 years. She is taking Penicillamine and Methotrexate for the past 6 months. Vitals include: blood pressure 122/89 mm Hg, pulse rate 55/min, temperature 36.7°C (98.0°F), and a respiratory rate 14/min. On examination, there is generalized pitting edema along with some subcutaneous nodules on the dorsal aspect of the forearm.
Urinalysis
pH 6.6
Color light yellow
RBC none
WBC 1–2/HPF
Protein 4+
Cast fat globules
Glucose absent
Crystal none
Ketone absent
Nitrite absent
24 hours urine protein excretion 4.8 g
Basic metabolic panel
Sodium 141 mEq/L
Potassium 5.1 mEq/L
Chloride 101 mEq/L
Bicarbonate 22 mEq/L
Albumin 3.2 mg/dL
Urea nitrogen 17 mg/dL
Creatinine 1.3 mg/dL
Uric Acid 6.8 mg/ dL
Calcium 8.9 mg/ dL
Glucose 111 mg/dL
A renal biopsy is ordered which shows diffuse capillary and glomerular basement membrane thickening. Which of the following is the most likely cause for her impaired renal function?
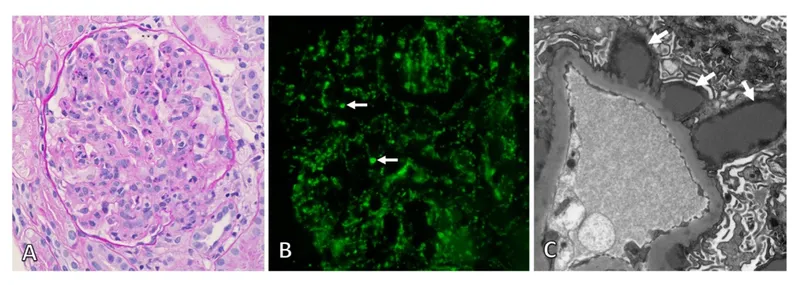
- A. Membranous nephropathy (Correct Answer)
- B. Diabetic glomerulonephropathy
- C. Minimal change disease
- D. Renal amyloidosis
- E. Lipoid nephrosis
Kidney diseases Explanation: **Membranous nephropathy**
- The patient's presentation with **nephrotic syndrome** (frothy urine, generalized edema, significant proteinuria > 3.5g/24h, hypoalbuminemia) and **renal biopsy findings of diffuse capillary and glomerular basement membrane thickening** are characteristic of membranous nephropathy.
- **Penicillamine**, which the patient is taking for rheumatoid arthritis, is a known cause of **secondary membranous nephropathy**.
*Diabetic glomerulonephropathy*
- While diabetes can cause nephrotic syndrome and renal impairment, there is **no history or evidence of diabetes** in this patient (fasting glucose 111 mg/dL is borderline but not diagnostic).
- Diabetic nephropathy typically shows **nodular glomerulosclerosis (Kimmelstiel-Wilson nodules) and mesangial expansion** on biopsy, not the diffuse GBM thickening described here.
- The patient's age and clinical presentation do not suggest longstanding diabetes.
*Minimal change disease*
- This condition typically presents with **abrupt onset of nephrotic syndrome**, primarily in children, and is characterized by a **normal renal biopsy on light microscopy** (hence "minimal change") with effacement of foot processes on electron microscopy.
- The patient's **diffuse capillary and glomerular basement membrane thickening** on biopsy contradicts minimal change disease.
*Renal amyloidosis*
- While amyloidosis can cause nephrotic syndrome and generalized edema, the **renal biopsy findings for amyloidosis would typically show Congo red-positive amyloid deposits**, which are not described here.
- Although rheumatoid arthritis can be a risk factor for secondary amyloidosis (AA amyloidosis), the description of diffuse capillary and glomerular basement membrane thickening is more specific to membranous nephropathy.
*Lipoid nephrosis*
- **Lipoid nephrosis** is an older term for **minimal change disease**.
- As explained above, minimal change disease is inconsistent with the **diffuse capillary and glomerular basement membrane thickening** observed on renal biopsy.
Kidney diseases US Medical PG Question 4: A 57-year-old man comes to the emergency department because of pain in the sides of his abdomen and blood-tinged urine since the previous night. Over the last 2 days, he has also had progressive malaise, myalgia, and a generalized itchy rash. He has a history of gastroesophageal reflux that did not respond to ranitidine but has improved since taking pantoprazole 2 months ago. He occasionally takes acetaminophen for back pain. His vital signs are within normal limits. Examination shows a generalized, diffuse maculopapular rash. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 13 g/dL
Leukocyte count 7,800/mm3
Serum
Na+ 140 mEq/L
Cl- 105 mEq/L
K+ 4.6 mEq/L
HCO3- 25 mEq/L
Glucose 102 mg/dL
Creatinine 4.1 mg/dL
Renal ultrasonography shows no abnormalities. Which of the following findings is most likely to be observed in this patient?
- A. Elevated levels of eosinophils in urine (Correct Answer)
- B. Mesangial IgA deposits on renal biopsy
- C. Urinary crystals on brightfield microscopy
- D. Crescent-shape extracapillary cell proliferation
- E. Papillary calcifications on CT imaging
Kidney diseases Explanation: ***Elevated levels of eosinophils in urine***
- This patient's symptoms of **fever, rash, eosinophilia (implied by high creatinine and drug history), and acute kidney injury** after starting pantoprazole strongly suggest **acute interstitial nephritis (AIN)**. **Eosinophiluria** is a hallmark of AIN.
- The history of recent initiation of **pantoprazole**, a proton pump inhibitor, is a significant clue as it is a common cause of drug-induced AIN.
*Mesangial IgA deposits on renal biopsy*
- **IgA nephropathy** typically presents with recurrent gross hematuria, often triggered by an upper respiratory infection.
- It would not explain the prominent **maculopapular rash**, malaise, and myalgia, which are more characteristic of a drug reaction.
*Urinary crystals on brightfield microscopy*
- **Urinary crystals** are associated with conditions like nephrolithiasis or certain drug toxicities, but not typically with this constellation of symptoms including a rash and systemic malaise.
- While the patient has flank pain and hematuria, the **acute kidney injury (creatinine 4.1 mg/dL)** and rash are inconsistent with simple crystaluria.
*Crescent-shape extracapillary cell proliferation*
- This finding is characteristic of **rapidly progressive glomerulonephritis (RPGN)**, which presents with severe acute renal failure and nephritic syndrome.
- While the patient has acute kidney injury, the prominent **rash, malaise, and eosinophilia** in the context of drug exposure point away from RPGN as the primary diagnosis.
*Papillary calcifications on CT imaging*
- **Papillary calcifications** or **nephrocalcinosis** indicate calcium deposition in the kidney parenchyma, often seen in chronic conditions like hyperparathyroidism or renal tubular acidosis.
- This imaging finding is not consistent with the acute presentation of systemic symptoms (rash, malaise) and acute kidney injury in this patient.
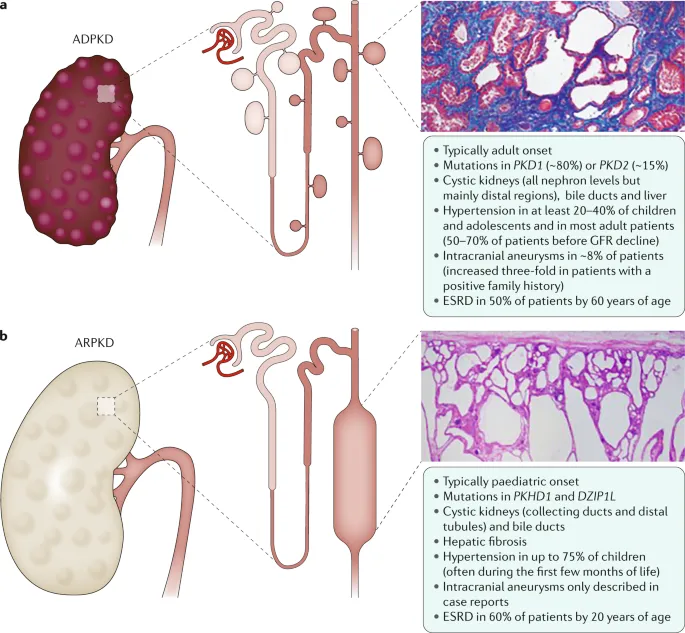
Kidney diseases US Medical PG Question 5: A female infant is born with a mutation in PKD1 on chromosome 16. An abdominal ultrasound performed shortly after birth would most likely reveal which of the following?
- A. Microscopic cysts
- B. Normal kidneys (Correct Answer)
- C. Adrenal atrophy
- D. Horseshoe kidney
- E. Bilateral kidney enlargement
Kidney diseases Explanation: ***Normal kidneys***
- Autosomal dominant polycystic kidney disease (ADPKD), caused by a mutation in **PKD1 or PKD2**, typically presents with **cysts that develop later in life**, usually in adulthood.
- At birth, the kidneys of an infant with the ADPKD mutation are usually **structurally normal** and do not yet show macroscopic cyst formation on ultrasound.
*Microscopic cysts*
- While the genetic mutation is present, significant **macroscopic cyst formation** detectable by standard abdominal ultrasound does not typically occur at birth in ADPKD.
- The cysts develop and enlarge over decades, leading to symptoms later in adulthood.
*Adrenal atrophy*
- **Adrenal atrophy** is not a feature of polycystic kidney disease and is caused by other conditions like autoimmune diseases or prolonged corticosteroid use.
- The adrenal glands are distinct from the kidneys and are not directly affected by PKD1 mutations.
*Horseshoe kidney*
- **Horseshoe kidney** is a congenital anomaly where the kidneys are fused, usually at the lower poles, and is not associated with PKD1 mutations.
- This condition is a **developmental fusion defect** during embryogenesis.
*Bilateral kidney enlargement*
- Bilateral kidney enlargement due to multiple cysts is characteristic of **ADPKD in adulthood**, not at birth.
- Though ADPKD is a genetic condition, the **phenotypic expression (cyst growth)** progresses over time.
Kidney diseases US Medical PG Question 6: A 6-year-old boy is brought to the physician because of increasing swelling around his eyes for the past 3 days. During this period, he has had frothy light yellow urine. He had a sore throat 12 days ago. He appears tired. His temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 105/65 mm Hg. Examination shows periorbital edema and pitting edema of the lower extremities. Cardiopulmonary examination shows no abnormalities. Which of the following findings on urinalysis is most likely associated with this patient's condition?
- A. WBC casts
- B. Fatty casts (Correct Answer)
- C. Hyaline casts
- D. RBC casts
- E. Muddy brown casts
Kidney diseases Explanation: ***Fatty casts***
- The patient's symptoms of **periorbital edema**, **pitting edema of lower extremities**, and **frothy urine** are classic for **nephrotic syndrome**, characterized by massive **proteinuria** (>3.5 g/day), **hypoalbuminemia**, **hyperlipidemia**, and **edema**.
- **Fatty casts** (also called **oval fat bodies** when in tubular cells) are **pathognomonic for nephrotic syndrome** and result from hyperlipidemia and lipiduria associated with severe proteinuria.
- In a **6-year-old child**, the most common cause of nephrotic syndrome is **minimal change disease**.
*WBC casts*
- **WBC casts** indicate **renal parenchymal inflammation** or **infection**, such as **pyelonephritis**, **acute interstitial nephritis**, or **tubulointerstitial disease**.
- These are not characteristic findings in **nephrotic syndrome**, which primarily affects the **glomerular filtration barrier** leading to protein loss rather than inflammatory cell infiltration.
*Hyaline casts*
- **Hyaline casts** are composed of **Tamm-Horsfall protein** and can be found in **normal urine**, especially with **dehydration**, **exercise**, or **concentrated urine**.
- They are **non-specific** and do not indicate significant kidney pathology or nephrotic syndrome.
*RBC casts*
- **RBC casts** are characteristic of **glomerulonephritis** and **nephritic syndrome** (such as **post-streptococcal glomerulonephritis**), where patients present with **hematuria**, **hypertension**, **mild edema**, and **oliguria**.
- While this patient had a **sore throat 12 days ago** (typical timing for post-streptococcal disease), his clinical presentation is clearly **nephrotic** (massive edema, frothy urine, normal blood pressure) rather than **nephritic**, making RBC casts unlikely.
- The **frothy urine** indicates significant **proteinuria**, not hematuria.
*Muddy brown casts*
- **Muddy brown casts** (granular casts with epithelial cell debris) are highly suggestive of **acute tubular necrosis (ATN)**, typically resulting from **ischemic** or **nephrotoxic injury**.
- This patient's presentation with **gradual onset edema** and **frothy urine** points to a **glomerular disorder** (nephrotic syndrome), not **acute tubular injury**.
Kidney diseases US Medical PG Question 7: A 34-year-old female presents to her primary care physician with complaints of fevers, nausea/vomiting, and severe left flank pain that has developed over the past several hours. She denies any prior episodes similar to her current presentation. Physical examination is significant for a body temperature of 39.1 C and costovertebral angle tenderness. A urinalysis and urine microscopy are ordered. Which of the following findings on kidney histology would be expected in this patient?
- A. Enlarged, hypercellular glomeruli with 'wire-looping' of capillaries
- B. Neutrophils filling the lumens of the renal tubules (Correct Answer)
- C. Scarring of the glomeruli
- D. Interstitial fibrosis and lymphocytic infiltrate
- E. Thickening of the capillaries and glomerular basement membrane
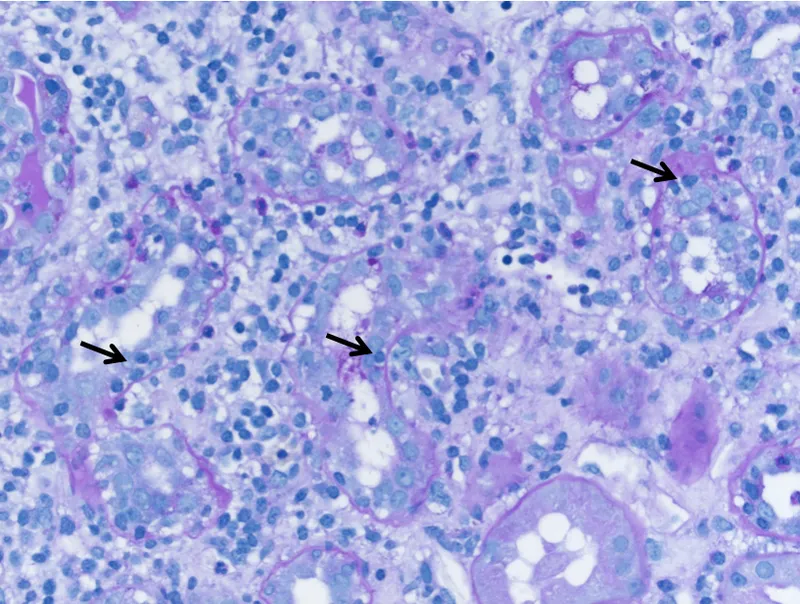
Kidney diseases Explanation: ***Neutrophils filling the lumens of the renal tubules***
- This patient's symptoms (fevers, nausea/vomiting, severe left flank pain, fever, and costovertebral angle tenderness) are highly suggestive of **acute pyelonephritis**, an infection of the kidney parenchyma.
- Histologically, acute pyelonephritis is characterized by an acute inflammatory infiltrate, primarily **neutrophils**, within the **renal tubules** and interstitial tissue, often forming **abscesses**.
*Enlarged, hypercellular glomeruli with 'wire-looping' of capillaries*
- This description is characteristic of **diffuse proliferative glomerulonephritis**, often associated with conditions like **systemic lupus erythematosus (SLE)**.
- The clinical presentation of sudden-onset severe flank pain and fever is not typical for glomerulonephritis, which usually presents with hematuria, proteinuria, and edema.
*Scarring of the glomeruli*
- **Glomerulosclerosis** (scarring of the glomeruli) is a feature of chronic kidney disease and various chronic glomerular disorders, not acute pyelonephritis.
- Patients with glomerular scarring typically present with signs of chronic kidney injury, such as persistent proteinuria and declining renal function, rather than acute infectious symptoms.
*Interstitial fibrosis and lymphocytic infiltrate*
- This is a hallmark of **chronic interstitial nephritis**, which can be caused by long-term drug use, autoimmune diseases, or chronic obstructive uropathy.
- While lymphocytes indicate inflammation, the presence of fibrosis suggests a chronic process, differing from the acute bacterial infection seen in pyelonephritis.
*Thickening of the capillaries and glomerular basement membrane*
- This finding is suggestive of various glomerular diseases, such as **membranous nephropathy** or **diabetic nephropathy**, where the glomerular basement membrane is significantly altered.
- Such conditions typically manifest with proteinuria and nephrotic or nephritic syndromes, not the acute infectious symptoms described.
Kidney diseases US Medical PG Question 8: A 35-year-old male with a history of hypertension presents with hematuria and abdominal discomfort. Ultrasound and CT scan reveal large, bilateral cysts in all regions of the kidney. What is the most likely diagnosis?
- A. Henoch-Schonlein purpura
- B. Diabetes mellitus
- C. Aortic stenosis
- D. Berger’s disease
- E. Polycystic kidney disease (Correct Answer)
Kidney diseases Explanation: ***Polycystic kidney disease***
- The presentation of **bilateral, large renal cysts** on imaging, along with **hematuria** and **hypertension** in a 35-year-old, is classic for **autosomal dominant polycystic kidney disease (ADPKD)**.
- ADPKD is a systemic disorder that can also cause cysts in other organs and is a leading cause of **end-stage renal disease**.
*Henoch-Schonlein purpura*
- This is a **small-vessel vasculitis** characterized by palpable purpura, arthritis, abdominal pain, and renal involvement (usually IgA nephropathy).
- It does not present with **large, bilateral renal cysts**.
*Diabetes mellitus*
- **Diabetic nephropathy** is a common complication causing progressive kidney damage and is a leading cause of kidney failure.
- However, it typically manifests as **proteinuria**, progressive decline in GFR, and eventually end-stage renal disease, not large renal cysts.
*Aortic stenosis*
- **Aortic stenosis** is a valvular heart disease impacting blood flow from the heart and is entirely unrelated to renal cysts or the described kidney pathology.
- While it can be associated with bleeding disorders (e.g., Heyde's syndrome), it does not directly cause **renal disease or cysts.**
*Berger’s disease*
- Also known as **IgA nephropathy**, Berger's disease is an immune-mediated glomerulonephritis, often presenting with recurrent **gross hematuria**, particularly after an upper respiratory infection.
- It involves inflammation of the glomeruli, not the development of **large renal cysts**.
Kidney diseases US Medical PG Question 9: A 36-year-old man comes to the physician for a 4-week history of swollen legs. He has difficulty putting on socks because of the swelling. Two years ago, he was diagnosed with sleep apnea. He takes no medications. He emigrated from Guatemala with his family when he was a child. He is 171 cm (5 ft 6 in) tall and weighs 115 kg (253 lb); BMI is 39 kg/m2. His pulse is 91/min and blood pressure is 135/82 mm Hg. Examination shows periorbital and bilateral lower extremity edema.
Serum
Albumin 3.1 g/dL
Total cholesterol 312 mg/dL
Urine
Blood negative
Protein +4
RBC 1-2/hpf
RBC cast negative
Fatty casts numerous
A renal biopsy is obtained. Which of the following is most likely to be seen under light microscopy of the patient's renal biopsy specimen?
- A. Diffuse thickening of glomerular capillaries
- B. Amyloid deposition in the mesangium
- C. Eosinophilic nodules within the glomeruli
- D. Fibrin crescents within the glomerular space
- E. Segmental sclerosis of the glomeruli (Correct Answer)
Kidney diseases Explanation: ***Segmental sclerosis of the glomeruli***
- The patient presents with **nephrotic syndrome** (edema, proteinuria, hypoalbuminemia, hypercholesterolemia) and **obesity** (BMI 39 kg/m2), which are strong risk factors for **focal segmental glomerulosclerosis (FSGS)**.
- **FSGS** is characterized by **segmental sclerosis** within some glomeruli, often affecting juxtamedullary glomeruli initially.
*Diffuse thickening of glomerular capillaries*
- **Diffuse thickening of glomerular capillaries** (due to subepithelial immune complex deposition causing SPIKES on silver stain) is characteristic of **membranous nephropathy**, which typically presents with nephrotic syndrome but is not directly linked to obesity in the way FSGS is.
- While membranous nephropathy could cause nephrotic syndrome, the association with **morbid obesity** makes FSGS a stronger consideration.
*Amyloid deposition in the mesangium*
- **Amyloid deposition** typically presents with nephrotic syndrome and is associated with chronic inflammatory conditions or plasma cell dyscrasias, not primarily with obesity or the specific presentation described.
- On light microscopy, amyloid appears as **acellular, eosinophilic congophilic deposits** in the mesangium and capillary walls, showing apple-green birefringence under polarized light, which is not suggested by the clinical picture.
*Eosinophilic nodules within the glomeruli*
- **Eosinophilic nodules within the glomeruli** (Kimmelstiel-Wilson lesions) are characteristic of **diabetic nephropathy**, which commonly causes nephrotic syndrome.
- While the patient is obese, there is no information about diabetes or hyperglycemia to suggest diabetic nephropathy as the primary cause.
*Fibrin crescents within the glomerular space*
- **Fibrin crescents within the glomerular space** are indicative of **rapidly progressive glomerulonephritis (RPGN)**, which typically presents as nephritic syndrome (hematuria, hypertension, azotemia) rather than pure nephrotic syndrome.
- The patient's urine microscopic findings show only 1-2 RBC/hpf and no RBC casts, making RPGN unlikely.
Kidney diseases US Medical PG Question 10: A 15-year-old Caucasian male is brought to his pediatrician by his parents, who note the development of a tremor in their child. Urine and serum analysis reveal elevated levels of copper. Which of the following clinical manifestations would the physician most expect to see in this patient?
- A. Kaiser-Fleischer rings (Correct Answer)
- B. Diabetes mellitus
- C. Hepatocytes that stain with Prussian blue
- D. Panacinar emphysema
- E. Increased serum ceruloplasmin
Kidney diseases Explanation: ***Kaiser-Fleischer rings***
- Elevated copper levels, tremor, and young age are classic signs of **Wilson's disease**, an autosomal recessive disorder leading to copper accumulation.
- **Kaiser-Fleischer rings** are greenish-brown deposits of copper in the cornea, a hallmark ocular manifestation of Wilson's disease.
*Diabetes mellitus*
- While copper dysregulation can affect various organs, **diabetes mellitus** is not a typical clinical manifestation of Wilson's disease.
- Pancreatic involvement leading to diabetes is more commonly associated with conditions like **hemochromatosis** (iron overload) or chronic pancreatitis.
*Hepatocytes that stain with Prussian blue*
- **Prussian blue stain** is used to detect **iron deposits**, not copper.
- In Wilson's disease, copper accumulates in hepatocytes, which would not stain positive with Prussian blue.
*Panacinar emphysema*
- **Panacinar emphysema** is primarily associated with **alpha-1 antitrypsin deficiency**, a genetic disorder affecting elastic tissue in the lungs.
- It has no direct association with copper metabolism or Wilson's disease.
*Increased serum ceruloplasmin*
- **Ceruloplasmin** is a copper-carrying protein, and in Wilson's disease, the **serum ceruloplasmin level is typically reduced**, not increased.
- This reduction is due to impaired copper incorporation into ceruloplasmin by the dysfunctional ATP7B protein.
More Kidney diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.