Head and neck pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Head and neck pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Head and neck pathology US Medical PG Question 1: A 26-year-old woman presents to the medicine clinic with swelling around the right side of her chin and neck (Image A). She reports pain when moving her jaw and chewing. Her symptoms developed two days after receiving an uncomplicated tonsillectomy. She has been followed by a general medical physician since birth and has received all of her standard health maintenance procedures. Vital signs are stable with the exception of a temperature of 38.4 degrees Celcius. The area in question on the right side is exquisitely tender. The remainder of her exam is benign. What is the most likely diagnosis?
- A. Superior vena cava syndrome
- B. Mumps
- C. Acute bacterial parotitis (Correct Answer)
- D. Sjogren's syndrome
- E. Pleomorphic adenoma
Head and neck pathology Explanation: **Acute bacterial parotitis**
- The patient's presentation with **unilateral swelling** around the chin and neck, **pain with jaw movement and chewing**, fever, and **exquisite tenderness** in the area, particularly after a recent **tonsillectomy** (which can predispose to dehydration or salivary gland dysfunction), is highly characteristic of acute bacterial parotitis.
- The elevated temperature further supports an infectious etiology, and the **post-operative setting** increases the risk for this condition due to potential retrograde infection from the oral cavity.
*Superior vena cava syndrome*
- This syndrome typically presents with **facial and neck edema**, distended neck veins, and dyspnea, resulting from obstruction of the superior vena cava, usually by a mass.
- It does not typically cause localized, **exquisitely tender swelling** or pain with jaw movement, and a recent tonsillectomy is not a risk factor.
*Mumps*
- While mumps causes **parotid gland swelling**, it is a viral infection that usually presents with **bilateral parotitis**, although unilateral cases can occur.
- The patient's history of receiving **all standard health maintenance procedures** suggests she has likely been vaccinated against mumps, making it less probable, and the rapid onset post-tonsillectomy points more towards a bacterial process.
*Sjogren's syndrome*
- This is a **chronic autoimmune disease** primarily affecting the exocrine glands, leading to **dry eyes and dry mouth**, and can cause recurrent enlargement of the parotid glands.
- It would not explain the **acute, painful, and tender swelling with fever** in a patient with no prior history of autoimmune disease, nor would it typically follow a tonsillectomy.
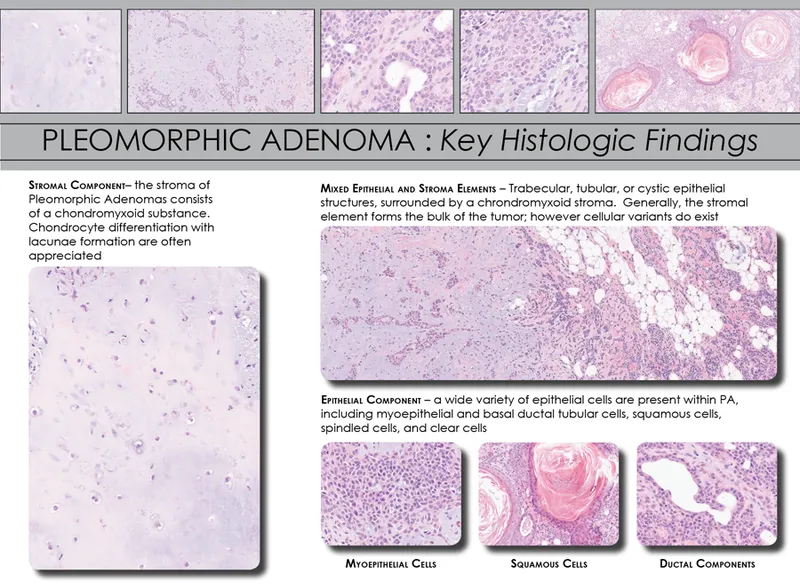
*Pleomorphic adenoma*
- This is a common **benign salivary gland tumor** that typically presents as a **slow-growing, painless mass** in the parotid gland.
- It would not explain the **acute onset, pain, tenderness, and fever** described in the patient, which are indicative of an inflammatory or infectious process.
Head and neck pathology US Medical PG Question 2: A 23-year-old woman presents with a painful lesion in her mouth. She denies tooth pain, bleeding from the gums, nausea, vomiting, diarrhea, or previous episodes similar to this in the past. She states that her last normal menstrual period was 12 days ago, and she has not been sexually active since starting medical school 2 years ago. On physical examination, the patient has good dentition with no signs of infection with the exception of a solitary ulcerated lesion on the oral mucosa. The nonvesicular lesion has a clean gray-white base and is surrounded by erythema. Which of the following is correct concerning the most likely etiology of the oral lesion in this patient?
- A. This lesion is non-contagious but will most likely recur. (Correct Answer)
- B. This lesion is associated with an autoimmune disease characterized by a sensitivity to gluten.
- C. This lesion may progress to squamous cell carcinoma.
- D. This lesion is due to a fungal infection and may mean you're immunocompromised.
- E. This lesion is highly contagious and is due to reactivation of a dormant virus.
Head and neck pathology Explanation: ***This lesion is non-contagious but will most likely recur.***
- The description of a **solitary, non-vesicular ulcerated lesion** with a **gray-white base** and surrounding **erythema** in the oral mucosa of a 23-year-old woman is highly characteristic of an **aphthous ulcer** (canker sore).
- Aphthous ulcers are **non-contagious** and are well-known for their **recurrent nature**, often appearing periodically throughout a person's life.
*This lesion is associated with an autoimmune disease characterized by a sensitivity to gluten.*
- While **celiac disease** (an autoimmune condition triggered by gluten) can be associated with recurrent aphthous ulcers, it is not the **most likely direct etiology** of the lesion itself, especially without other gastrointestinal symptoms or a history of celiac disease.
- The primary cause of aphthous ulcers in this context is typically unknown or related to minor trauma, stress, or nutritional deficiencies.
*This lesion may progress to squamous cell carcinoma.*
- Aphthous ulcers are **benign** and do not carry a risk of malignant transformation into **squamous cell carcinoma**.
- Risk factors for squamous cell carcinoma of the oral cavity include prolonged tobacco and alcohol use, and chronic irritation from ill-fitting dentures.
*This lesion is due to a fungal infection and may mean you're immunocompromised.*
- A fungal infection like **oral candidiasis** (thrush) typically presents as **white patches** that can be scraped off, often associated with immunocompromise or antibiotic use.
- The description of a well-demarcated ulcer with a gray-white base surrounded by erythema does not fit the typical presentation of a fungal infection.
*This lesion is highly contagious and is due to reactivation of a dormant virus.*
- Lesions caused by a dormant virus, such as **herpes simplex virus (HSV)**, typically present as **vesicles** that rupture to form ulcers, often appearing in clusters (cold sores).
- Aphthous ulcers are distinctly **non-viral** in origin and **not contagious**, differentiating them from herpetic lesions.
Head and neck pathology US Medical PG Question 3: An 11-year-old boy who recently emigrated from Nigeria is brought to the physician for evaluation of jaw swelling. He has no history of serious illness and takes no medications. Examination shows a 5-cm solid mass located above the right mandible and significant cervical lymphadenopathy. A biopsy specimen of the mass shows sheets of lymphocytes with interspersed tingible body macrophages. Serology for Epstein-Barr virus is positive. Which of the following chromosomal translocations is most likely present in cells obtained from the tissue mass?
- A. t(8;14) (Correct Answer)
- B. t(12;21)
- C. t(11;22)
- D. t(15;17)
- E. t(11;14)
Head and neck pathology Explanation: ***t(8;14)***
- The constellation of **jaw swelling** in a child from **Nigeria**, positive **Epstein-Barr virus (EBV)** serology, and a biopsy showing a **"starry sky"** pattern (sheets of lymphocytes with interspersed tingible body macrophages) is classic for **endemic Burkitt lymphoma**.
- **Burkitt lymphoma** is characterized by the **t(8;14) translocation**, which results in the constitutive activation of the **c-MYC oncogene** on chromosome 8 due to its proximity to the **immunoglobulin heavy chain locus** on chromosome 14.
*t(12;21)*
- This translocation is typically associated with **B-cell acute lymphoblastic leukemia (ALL)**, particularly in children.
- While ALL can present with bone pain or cytopenias, it does not typically manifest as a localized **jaw mass** with a "starry sky" histology.
*t(11;22)*
- This translocation is characteristic of **Ewing sarcoma**, a **bone tumor** that can affect the jaw.
- However, Ewing sarcoma would typically show small, round, blue cells on histology and would not be associated with **EBV infection** or the "starry sky" pattern.
*t(15;17)*
- This translocation is pathognomonic for **acute promyelocytic leukemia (APML)**, a subtype of acute myeloid leukemia.
- APML presents with signs of bone marrow failure and disseminated intravascular coagulation, not with a localized head and neck mass.
*t(11;14)*
- This translocation is primarily associated with **mantle cell lymphoma**, a type of non-Hodgkin lymphoma that typically affects older adults.
- Mantle cell lymphoma would have cyclin D1 overexpression, and usually does not present as a localized jaw mass in children, nor is it strongly linked to EBV in this clinical context.
Head and neck pathology US Medical PG Question 4: A 30-year-old boxer seeks evaluation by his physician after he noticed swelling at the angle of his jaw a few days ago. He recalls a recent boxing match when he was punched in his face. He says that his jaw is very painful. On examination, a firm mass is palpated, measuring 4 x 4 cm. An ultrasound was performed, which shows a thin, encapsulated, well-circumscribed, predominantly solid mass with occasional cystic areas. The mass is surgically excised, after which he develops a hoarse voice for a few days, but recovers within 1 week. The histopathologic evaluation of the surgical specimen reports a pseudocapsule with a hypocellular stromal component consisting of a myxoid background and cartilage arranged in clusters and a hypercellular epithelial component with cells arranged in sheets and trabeculae. From which of the following structures did the mass most likely arise?
- A. Salivary duct
- B. Thyroid
- C. Parotid gland (Correct Answer)
- D. Minor salivary gland
- E. Seventh cranial nerve
Head and neck pathology Explanation: ***Parotid gland***
- The location of the mass at the **angle of the jaw** is highly suggestive of the parotid gland, as the superficial lobe often extends into this region.
- The histopathological findings of a **pseudocapsule**, hypocellular stromal component with **myxoid background and cartilage**, and a hypercellular epithelial component are classic features of a **pleomorphic adenoma**, which is the most common tumor of the parotid gland.
- The temporary **hoarseness** after surgery suggests inadvertent injury to the **recurrent laryngeal nerve**, which can occur if the surgical dissection extends deeper into the neck near the carotid sheath. Note that the **facial nerve (CN VII)** runs through the parotid gland and is at risk during parotidectomy, but facial nerve injury typically causes facial weakness rather than voice changes.
*Salivary duct*
- While salivary ducts are present within salivary glands, a tumor arising directly from a salivary duct rather than the gland parenchyma would likely present with very different histological features, such as those of a **ductal papilloma** or **adenocarcinoma, salivary duct type**.
- The complex **stromal and epithelial components** with cartilage described are characteristic of a pleomorphic adenoma, which originates from both epithelial and mesenchymal elements of the gland, not solely the duct.
*Thyroid*
- The thyroid gland is located in the **anterior neck**, inferior to the laryngeal prominence (Adam's apple), not at the **angle of the jaw**.
- Tumors of the thyroid gland, such as papillary or follicular carcinoma, would have distinct histological features and would not typically present with the described myxoid and cartilaginous stromal components.
*Minor salivary gland*
- Minor salivary glands are numerous and widely distributed in the oral cavity and upper aerodigestive tract, but a mass of this size (4 x 4 cm) at the **angle of the jaw** specifically points to one of the major salivary glands.
- While pleomorphic adenomas can arise in minor salivary glands (most commonly in the palate), their presentation as a large mass at the angle of the jaw is far less common than their occurrence in the parotid gland.
*Seventh cranial nerve*
- The seventh cranial nerve (facial nerve) passes through the parotid gland but does not itself give rise to tumors with the described histological features.
- Tumors involving the facial nerve are typically **schwannomas** or **neurofibromas**, which originate from Schwann cells and would show different microscopic characteristics such as Antoni A and B patterns, not the mixed epithelial-mesenchymal features of pleomorphic adenoma.
Head and neck pathology US Medical PG Question 5: A 63-year-old man presents to his primary care physician because he has been having headaches and hearing loss. In addition, he says that he has been having difficulty opening his jaw to eat and recurrent middle ear infections. Physical exam reveals enlarged neck lymph nodes and a mass in the nasopharynx. Biopsy of the mass reveals undifferentiated squamous epithelial cells. The organism that is most likely associated with this patient's disease is also associated with which of the following disorders?
- A. Kaposi sarcoma
- B. Hepatocellular carcinoma
- C. Adult T-cell lymphoma
- D. Burkitt lymphoma (Correct Answer)
- E. Vulvar carcinoma
Head and neck pathology Explanation: ***Burkitt lymphoma***
- The patient's symptoms (headaches, hearing loss, difficulty opening jaw, recurrent middle ear infections, nasopharyngeal mass, enlarged neck lymph nodes) and biopsy results (undifferentiated squamous epithelial cells) point to **nasopharyngeal carcinoma**.
- **Nasopharyngeal carcinoma** is strongly associated with the **Epstein-Barr virus (EBV)**. EBV is also a causative agent in **Burkitt lymphoma**.
*Kaposi sarcoma*
- **Kaposi sarcoma** is caused by **Human Herpesvirus 8 (HHV-8)**, not EBV.
- It typically presents as vascular skin lesions and can affect visceral organs, differing from the nasopharyngeal carcinoma described.
*Hepatocellular carcinoma*
- **Hepatocellular carcinoma** is primarily associated with **Hepatitis B virus (HBV)** and **Hepatitis C virus (HCV)** infection, as well as cirrhosis from other causes.
- There is no significant association between EBV and hepatocellular carcinoma.
*Adult T-cell lymphoma*
- **Adult T-cell lymphoma** is caused by the **Human T-lymphotropic virus type 1 (HTLV-1)**.
- This is a retrovirus distinct from EBV.
*Vulvar carcinoma*
- **Vulvar carcinoma** is most frequently associated with **Human Papillomavirus (HPV)** infection, especially high-risk strains like HPV 16 and 18.
- It is not typically linked to EBV.
Head and neck pathology US Medical PG Question 6: A 5-year-old boy is brought into your office by his mother. His father recently passed away, and his mother states she just lost her job. She has been unable to buy food regularly, and they have had to eat boiled and preserved vegetables. His mother denies that the boy has any prior medical conditions, but the patient states that his gums bleed when he brushes his teeth. On exam, the patient's vital signs are normal, but he appears malnourished. There is gum hypertrophy present on exam along with small, curled hairs over his head. CBC is significant for a Hgb of 9.5 g/dL with an MCV of 85. PT, aPTT, and bleeding time are all normal. What is the most likely cause?
- A. Vitamin C deficiency (Correct Answer)
- B. Vitamin K deficiency
- C. Vitamin B3 deficiency
- D. Vitamin B12 deficiency
- E. Iron deficiency
Head and neck pathology Explanation: ***Vitamin C deficiency***
- The patient's history of **malnutrition**, consumption of only **boiled and preserved vegetables** (which deplete vitamin C), **bleeding gums**, and **curled hairs** ("corkscrew hairs") are classic signs of scurvy, caused by vitamin C deficiency.
- **Vitamin C** is essential for **collagen synthesis** and *antioxidant function*, and its deficiency leads to impaired wound healing, fragile capillaries, and anemia.
*Vitamin K deficiency*
- This deficiency primarily affects **blood clotting**, leading to increased PT/aPTT, but the patient's **PT, aPTT, and bleeding time are all normal**.
- While bleeding gums can occur, it's not typically associated with **curled hairs** or caused by a diet of boiled vegetables in this manner.
*Vitamin B3 deficiency*
- Also known as **niacin deficiency**, it causes pellagra, characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**.
- These symptoms are not present in the patient, and bleeding gums or curled hairs are not typical manifestations of niacin deficiency.
*Vitamin B12 deficiency*
- This deficiency usually results in **macrocytic anemia** (high MCV), **neurological symptoms**, and **glossitis** (sore, smooth tongue).
- The patient has a **normal MCV** (85) and none of the characteristic neurological or oral findings of B12 deficiency.
*Iron deficiency*
- Iron deficiency leads to **microcytic anemia** (low MCV) and symptoms like **fatigue**, **pallor**, and **pica**.
- The patient has **normocytic anemia** (MCV 85), and while anemia is present, the specific constellation of bleeding gums and curled hairs is not characteristic of iron deficiency.
Head and neck pathology US Medical PG Question 7: A 16-year-old boy is brought to the physician by his mother because of a 4-day history of painful lesions in his mouth. During the past year, he has twice had similar lesions that resolved without treatment after approximately 10 days. He has never had any genital or anal lesions. His mother reports that he has been very stressed over the past month because he is approaching his senior year at high school. He is otherwise healthy and takes no medications. He appears thin. His temperature is 37.6°C (99.7°F). A photograph of his oral cavity is shown. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Herpangina
- B. Oral leukoplakia
- C. Pemphigus vulgaris
- D. Aphthous stomatitis (Correct Answer)
- E. Oral thrush
Head and neck pathology Explanation: ***Aphthous stomatitis***
- This patient presents with **recurrent painful oral lesions** that resolve spontaneously, consistent with **aphthous stomatitis**, commonly known as **canker sores**. The lesions are often triggered by **stress**, as described in the patient's history.
- The absence of **genital or anal lesions** helps differentiate this from other conditions like Behçet's disease, and the photograph would likely show characteristic **shallow, circumscribed ulcers** with a reddish halo.
*Herpangina*
- Herpangina is typically caused by **coxsackievirus** and presents with **vesicles and ulcers** predominantly on the **posterior oropharynx** (soft palate, tonsillar pillars, uvula).
- It often accompanies **fever, sore throat, and dysphagia**, and is more common in younger children, differing from this patient's presentation.
*Oral leukoplakia*
- **Oral leukoplakia** is characterized by **white, adherent patches** on the oral mucosa that **cannot be scraped off**. It is typically **painless** and considered a **precancerous lesion**, often associated with chronic irritation like tobacco use.
- This differs significantly from the patient's **painful, recurrent ulcerative lesions**.
*Pemphigus vulgaris*
- **Pemphigus vulgaris** is a **severe autoimmune blistering disease** affecting the skin and mucous membranes. Oral lesions are often the **first manifestation**, presenting as **flaccid bullae** that rupture to form widespread, **painful erosions**.
- This condition is chronic, progressive, and usually requires treatment, unlike the patient's self-resolving, recurrent lesions.
*Oral thrush*
- **Oral thrush (candidiasis)** is caused by *Candida albicans* and presents as **creamy white patches** on the oral mucosa that **can be scraped off**, revealing erythematous, sometimes bleeding tissue underneath.
- It is typically seen in infants, immunocompromised individuals, or those on antibiotics, and the lesions are generally **not painful** unless severe, and they are not described as ulcers.
Head and neck pathology US Medical PG Question 8: A 53-year-old man is brought to the emergency department for confusion. He was in his usual state of health until about 3 hours ago when he tried to use his sandwich to turn off the TV. He also complained to his wife that he had a severe headache. Past medical history is notable for hypertension, which has been difficult to control on multiple medications. His temperature is 36.7°C (98°F), the pulse is 70/min, and the blood pressure is 206/132 mm Hg. On physical exam he is alert and oriented only to himself, repeating over and over that his head hurts. The physical exam is otherwise unremarkable and his neurologic exam is nonfocal. The noncontrast CT scan of the patient's head is shown and reveals an acute intraparenchymal hemorrhage in the basal ganglia. Which of the following diagnostic tests would be most helpful in determining the underlying cause of this patient's hemorrhage?
- A. Lumbar puncture
- B. Electroencephalogram (EEG)
- C. MRI of the brain
- D. CT angiography of the neck
- E. CT angiography of the brain (Correct Answer)
Head and neck pathology Explanation: ***CT angiography of the brain***
- Following identification of an **intracerebral hemorrhage** on noncontrast CT, **CT angiography (CTA) of the brain** is the most appropriate next diagnostic test to identify underlying vascular abnormalities such as **arteriovenous malformations (AVMs)**, **aneurysms**, **dural arteriovenous fistulas**, or **moyamoya disease**.
- While this patient has severe hypertension (a common cause of basal ganglia hemorrhage), CTA should still be performed to rule out secondary causes, particularly in patients under 70 years old or those with atypical features.
- CTA can be performed rapidly in the acute setting and has high sensitivity for detecting vascular lesions that may require specific treatment.
*MRI of the brain*
- MRI with specialized sequences (GRE, SWI, FLAIR) can provide detailed information about **chronic microhemorrhages**, **cerebral amyloid angiopathy**, **underlying tumors**, or **cavernomas**.
- However, MRI is typically performed **after CTA** in the workup of intracerebral hemorrhage, not as the immediate next step.
- MRI is less readily available in the acute setting and takes longer to perform than CTA.
*CT angiography of the neck*
- This test visualizes the **carotid and vertebral arteries** in the neck to detect **stenosis**, **dissection**, or **atherosclerotic disease**.
- It is not directly useful for identifying the cause of an **intraparenchymal hemorrhage** within the brain substance itself.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** and is primarily used for suspected **subarachnoid hemorrhage** (when CT is negative), **meningitis**, or **encephalitis**.
- It is **contraindicated** in patients with significant intraparenchymal hemorrhage due to risk of herniation from increased intracranial pressure.
*Electroencephalogram (EEG)*
- EEG measures **electrical activity in the brain** and is used to diagnose **seizure disorders** or evaluate altered mental status from metabolic or epileptic causes.
- While confusion can result from seizures, the primary pathology is the **intracerebral hemorrhage** identified on CT, which EEG cannot diagnose or characterize.
Head and neck pathology US Medical PG Question 9: A 20-year-old man presents with a painless neck mass that has gradually increased in size. The mass is anteromedial to the right sternocleidomastoid muscle and has been present for 3 years. The mass increased in size and became more tender following an upper respiratory infection. An ultrasound of the neck identifies a single, round cystic mass with uniform, low echogenicity, and no internal septations. A contrast-enhanced CT scan of the neck shows a homogeneous mass with low attenuation centrally and with smooth rim enhancement. Which of the following is the most likely diagnosis?
- A. First branchial cleft cyst
- B. Sternomastoid tumor
- C. Second branchial cleft cyst (Correct Answer)
- D. Ectopic thyroid tissue
- E. Cervical lymphadenopathy
Head and neck pathology Explanation: **Second branchial cleft cyst**
- The **location** (anteromedial to the sternocleidomastoid muscle), **painless** nature, and history of **gradual enlargement** becoming tender after an URI are classic presentations.
- **Imaging findings** (single, round cystic mass with uniform low echogenicity on ultrasound; homogeneous mass with low attenuation centrally and smooth rim enhancement on CT) are highly characteristic of an infected branchial cleft cyst.
*First branchial cleft cyst*
- Typically presents with a mass located near the **external auditory canal** or **angle of the mandible**, often causing otorrhea or recurrent infections.
- The presented mass is in a different anatomical location, **anteromedial** to the sternocleidomastoid.
*Sternomastoid tumor*
- This condition usually presents as a **fibrotic mass** within the sternocleidomastoid muscle in **neonates or infants**, associated with **congenital muscular torticollis**.
- The patient's age (20 years old) and the **cystic nature** of the mass make this diagnosis unlikely.
*Ectopic thyroid tissue*
- While possible in the neck, ectopic thyroid tissue would typically present as a **solid mass** and would show **iodine uptake** on nuclear imaging, not a cystic appearance on ultrasound and CT.
- It is more commonly located in the **midline** of the neck (e.g., lingual thyroid) rather than anteromedial to the sternocleidomastoid.
*Cervical lymphadenopathy*
- Enlarged lymph nodes typically present with **multiple, often tender, solid masses** or a single mass with typical lymph node morphology (e.g., hilar fat, oval shape), especially after an infection.
- The **cystic nature** described by imaging, with uniform low echogenicity and rim enhancement, is not typical for uncomplicated lymphadenopathy.
Head and neck pathology US Medical PG Question 10: A 15-year-old girl comes to the physician because of a sore throat and subjective fevers for the past 2 weeks. She has been feeling lethargic and is unable to attend school. She has a history of multiple episodes of streptococcal pharyngitis treated with amoxicillin. She immigrated with her family to the United States from China 10 years ago. She appears thin. Her temperature is 37.8°C (100°F), pulse is 97/min, and blood pressure is 90/60 mm Hg. Examination shows pharyngeal erythema and enlarged tonsils with exudates and palatal petechiae. There is cervical lymphadenopathy. The spleen is palpated 2 cm below the left costal margin. Her hemoglobin concentration is 12 g/dL, leukocyte count is 14,100/mm3 with 54% lymphocytes (12% atypical lymphocytes), and platelet count is 280,000/mm3. A heterophile agglutination test is positive. The underlying cause of this patient's symptoms is most likely to increase the risk of which of the following conditions?
- A. Kaposi sarcoma
- B. Glomerulonephritis
- C. Pneumonia
- D. Nasopharyngeal carcinoma (Correct Answer)
- E. Necrotizing retinitis
Head and neck pathology Explanation: ***Nasopharyngeal carcinoma***
- The patient's symptoms (sore throat, fatigue, pharyngeal erythema, enlarged tonsils with exudates, palatal petechiae, cervical lymphadenopathy, splenomegaly, atypical lymphocytosis, and positive heterophile agglutination test) are classic for **infectious mononucleosis**, caused by the **Epstein-Barr virus (EBV)**.
- EBV infection is a significant risk factor for developing **nasopharyngeal carcinoma**, especially in individuals of Chinese descent, making this the most likely long-term complication.
*Kaposi sarcoma*
- **Kaposi sarcoma** is associated with **human herpesvirus 8 (HHV-8)**, not EBV.
- It is typically seen in immunocompromised individuals, such as those with HIV/AIDS, or in specific endemic regions.
*Glomerulonephritis*
- **Glomerulonephritis** can be a complication of **Streptococcus pyogenes infections** (post-streptococcal glomerulonephritis) or other autoimmune diseases, but it is not directly linked to EBV infection.
- The patient's history of streptococcal pharyngitis is relevant for this, but her current presentation points to EBV.
*Pneumonia*
- While pneumonia can occur as a secondary complication in severely ill patients with infectious mononucleosis, it is not a direct long-term increased risk associated with the underlying EBV infection itself.
- EBV primarily affects lymphoid tissues.
*Necrotizing retinitis*
- **Necrotizing retinitis** is most commonly associated with **cytomegalovirus (CMV)** infection, particularly in immunocompromised patients (e.g., HIV/AIDS).
- It is not a typical complication or long-term risk of EBV infection.
More Head and neck pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.