Gallbladder and biliary tract disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gallbladder and biliary tract disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gallbladder and biliary tract disorders US Medical PG Question 1: A 65-year-old man presents to his primary care physician for fatigue. The patient states that he has not been sleeping well and requests sleep medication to help him with his fatigue. He recently changed his diet to try to increase his energy and has been on a vegetarian diet for the past several months. The patient has no significant past medical history. He smokes 1 pack of cigarettes per day and drinks 5 alcoholic beverages per day. The patient has lost 12 pounds since his last visit 1 month ago. Physical exam demonstrates a tired man. He appears thin, and his skin and sclera are icteric. Abdominal ultrasound is notable for a thin-walled and enlarged gallbladder. A urine sample is collected and is noted to be amber in color. Which of the following is the most likely diagnosis?
- A. Cholangiocarcinoma
- B. Pancreatic adenocarcinoma (Correct Answer)
- C. Gallbladder adenocarcinoma
- D. Iron deficiency anemia
- E. Autoimmune hemolytic anemia
Gallbladder and biliary tract disorders Explanation: ***Pancreatic adenocarcinoma***
- This patient presents with hallmark signs of **pancreatic adenocarcinoma**, including **painless jaundice** (icteric skin and sclera), **unexplained weight loss**, and risk factors such as **smoking** and **heavy alcohol use**.
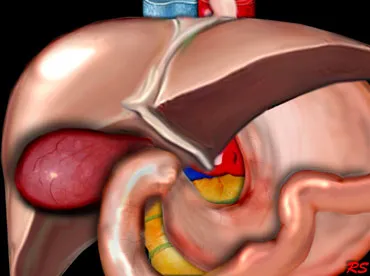
- The abdominal ultrasound finding of a **thin-walled and enlarged gallbladder** in the setting of jaundice is known as **Courvoisier's sign**, highly suggestive of a distal biliary obstruction, often caused by a pancreatic head tumor.
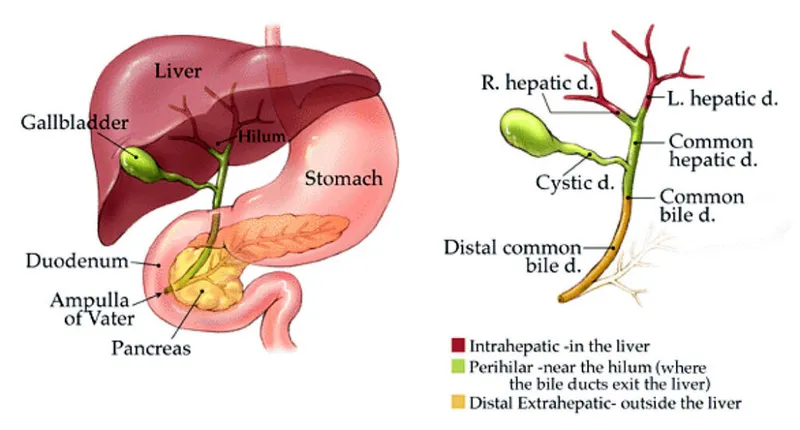
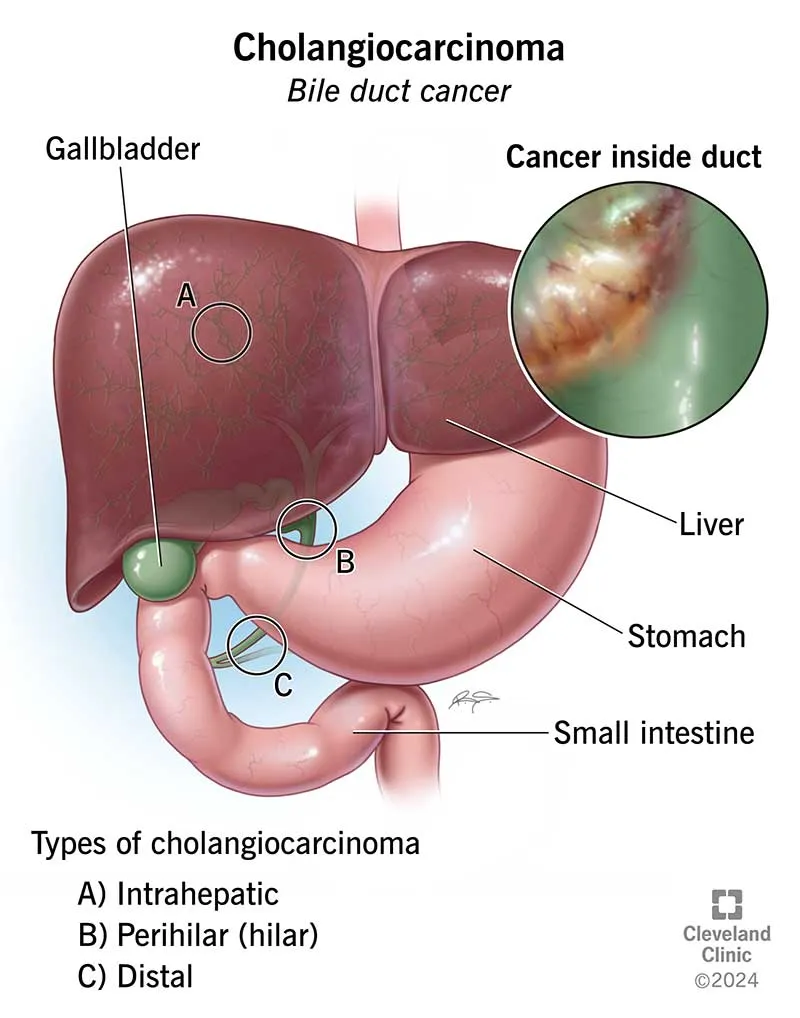
*Cholangiocarcinoma*
- While cholangiocarcinoma can cause **obstruction and jaundice**, it is less commonly associated with **Courvoisier's sign** (distended, palpable gallbladder) compared to pancreatic head tumors.
- Risk factors for cholangiocarcinoma often include **primary sclerosing cholangitis** or **liver fluke infections**, which are not mentioned here.
*Gallbladder adenocarcinoma*
- Gallbladder adenocarcinoma often presents with **right upper quadrant pain**, **weight loss**, and sometimes **jaundice**, but the jaundice typically occurs later as the tumor invades the biliary tree.
- It is less likely to cause a **painless, distended gallbladder** (Courvoisier's sign) in the same way a pancreatic head mass would.
*Iron deficiency anemia*
- While fatigue can be a symptom of **iron deficiency anemia**, the striking features of **jaundice**, **weight loss**, and **Courvoisier's sign** point strongly away from this diagnosis as the primary cause of his symptoms.
- The dark urine in this context suggests **conjugated hyperbilirubinemia**, not typically seen in iron deficiency anemia.
*Autoimmune hemolytic anemia*
- **Autoimmune hemolytic anemia** can cause fatigue and **unconjugated hyperbilirubinemia**, leading to jaundice, but it would not explain the significant **weight loss**, **Courvoisier's sign**, or the amber (indicative of conjugated bilirubin) urine.
- The distended gallbladder points to an obstructive process rather than hemolytic jaundice.
Gallbladder and biliary tract disorders US Medical PG Question 2: A previously healthy 37-year-old woman, gravida 3, para 2, at 29 weeks' gestation comes to the physician because of colicky postprandial abdominal pain. Her vital signs are within normal limits. Physical examination shows a uterus consistent in size with a 29-week gestation. Ultrasonography of the abdomen shows multiple 5-mm hyperechoic masses within the gallbladder lumen. Which of the following processes is most likely involved in the pathogenesis of this patient's condition?
- A. Accelerated gallbladder emptying
- B. Increased secretion of bile acids
- C. Increased secretion of cholesterol (Correct Answer)
- D. Decreased caliber of bile duct
- E. Overproduction of bilirubin
Gallbladder and biliary tract disorders Explanation: ***Increased secretion of cholesterol***
- Pregnancy leads to increased **estrogen levels**, which elevate hepatic cholesterol secretion into bile.
- This increased cholesterol, combined with reduced gallbladder motility due to **progesterone**, promotes bile supersaturation and cholesterol stone formation.
*Accelerated gallbladder emptying*
- Pregnancy hormones like **progesterone** actually lead to *decreased* gallbladder motility and delayed emptying, contributing to bile stasis.
- Accelerated emptying would reduce the likelihood of stone formation, as bile would not remain in the gallbladder long enough to supersaturate.
*Increased secretion of bile acids*
- While bile acids are crucial for fat digestion, their *increased* secretion would help solubilize cholesterol, thus *reducing* the risk of gallstone formation.
- The problem in cholesterol gallstone pathogenesis is often an imbalance *favoring* cholesterol over bile acids.
*Decreased caliber of bile duct*
- A decreased caliber of the bile duct is more characteristic of conditions like **cholangitis** or **choledocholithiasis** (stones in the common bile duct), which occur *after* stones have formed or due to other pathologies.
- It is not a primary factor in the *formation* of gallstones within the gallbladder.
*Overproduction of bilirubin*
- Overproduction of bilirubin, as seen in conditions like **hemolytic anemia**, primarily leads to the formation of **pigment gallstones** (black or brown stones).
- The hyperechoic masses in this patient, especially given the context of pregnancy, are more consistent with cholesterol gallstones.
Gallbladder and biliary tract disorders US Medical PG Question 3: A 42-year-old woman is brought to the emergency department because of intermittent sharp right upper quadrant abdominal pain and nausea for the past 10 hours. She has vomited 3 times. There is no associated fever, chills, diarrhea, or urinary symptoms. She has 2 children who both attend high school. She appears uncomfortable. She is 165 cm (5 ft 5 in) tall and weighs 86 kg (190 lb). Her BMI is 32 kg/m2. Her temperature is 37.0°C (98.6°F), pulse is 100/min, and blood pressure is 140/90 mm Hg. She has mild scleral icterus. On physical examination, her abdomen is soft and nondistended, with tenderness to palpation of the right upper quadrant without guarding or rebound. Bowel sounds are normal. Laboratory studies show the following:
Blood
Hemoglobin count 14 g/dL
Leukocyte count 9,000 mm3
Platelet count 160,000 mm3
Serum
Alkaline phosphatase 238 U/L
Aspartate aminotransferase 60 U/L
Bilirubin
Total 2.8 mg/dL
Direct 2.1 mg/dL
Which of the following is the most appropriate next step in diagnosis?
- A. Endoscopic retrograde cholangiopancreatography (ERCP)
- B. Supine and erect X-rays of the abdomen
- C. Computed tomography (CT) scan of the abdomen
- D. Hepatobiliary iminodiacetic acid (HIDA) scan of the biliary tract
- E. Transabdominal ultrasonography (Correct Answer)
Gallbladder and biliary tract disorders Explanation: ***Transabdominal ultrasonography***
- This is the **initial diagnostic test of choice** for suspected **gallstones** or other biliary pathology due to its non-invasive nature, accessibility, and high sensitivity for detecting stones.
- The patient's presentation with **RUQ pain**, nausea, vomiting, obesity, and mild **scleral icterus** with elevated **alkaline phosphatase** and **direct bilirubin** is highly suggestive of **choledocholithiasis** or **cholecystitis**.
*Endoscopic retrograde cholangiopancreatography (ERCP)*
- **ERCP** is a **therapeutic procedure** used to remove stones from the common bile duct, rather than a primary diagnostic tool.
- It is an **invasive procedure** with risks such as pancreatitis and is reserved for cases where obstruction is confirmed and needs intervention.
*Supine and erect X-rays of the abdomen*
- **Plain X-rays** are not effective for diagnosing gallstones as only about **10-20% of gallstones are radiopaque**.
- While they can rule out other causes of abdominal pain like bowel obstruction or perforation, they are **not the primary imaging modality** for biliary issues.
*Computed tomography (CT) scan of the abdomen*
- A **CT scan** is less sensitive than ultrasound for detecting gallstones and is associated with **radiation exposure**.
- It might be used if ultrasound findings are inconclusive or if there is concern for other intra-abdominal pathology, but it is **not the initial test of choice** for suspected cholelithiasis.
*Hepatobiliary iminodiacetic acid (HIDA) scan of the biliary tract*
- A **HIDA scan** is primarily used to diagnose **acute cholecystitis** (inflammation of the gallbladder) by assessing gallbladder emptying or obstruction of the cystic duct.
- While useful for acute cholecystitis, it is **not the first-line diagnostic test** for simply detecting gallstones or common bile duct stones, for which ultrasound is superior.
Gallbladder and biliary tract disorders US Medical PG Question 4: A 45-year-old woman comes to the emergency department complaining of abdominal pain for the past day. The pain is situated in the right upper quadrant, colicky, 8/10, and radiates to the tip of the right shoulder with no aggravating or relieving factors. The pain is associated with nausea but no vomiting. She tried to take over-the-counter antacids which relieved her pain to a certain extent, but not entirely. She does not smoke cigarettes or drink alcohol. She has no past medical illness. Her father died of pancreatic cancer at the age of 75, and her mother has diabetes controlled with medications. Temperature is 38°C (100.4°F), blood pressure is 125/89 mm Hg, pulse is 104/min, respiratory rate is 20/min, and BMI is 29 kg/m2. On abdominal examination, her abdomen is tender to shallow and deep palpation of the right upper quadrant.
Laboratory test
Complete blood count
Hemoglobin 13 g/dL
WBC 15,500/mm3
Platelets 145,000/mm3
Basic metabolic panel
Serum Na+ 137 mEq/L
Serum K+ 3.6 mEq/L
Serum Cl- 95 mEq/L
Serum HCO3- 25 mEq/L
BUN 10 mg/dL
Serum creatinine 0.8 mg/dL
Liver function test
Total bilirubin 1.3 mg/dL
AST 52 U/L
ALT 60 U/L
Ultrasonography of the abdomen shows normal findings. What is the best next step in management of this patient?
- A. Emergency cholecystectomy
- B. CT scan
- C. Reassurance and close follow up
- D. Cholescintigraphy (Correct Answer)
- E. Percutaneous cholecystostomy
Gallbladder and biliary tract disorders Explanation: ***Cholescintigraphy***
- The patient presents with **right upper quadrant pain**, fever, **leukocytosis**, and elevated liver enzymes, pointing towards **acute cholecystitis**. Despite a normal ultrasound, cholescintigraphy (HIDA scan) is the gold standard for diagnosing acute cholecystitis when imaging is equivocal.
- Cholescintigraphy can assess the **patency of the cystic duct**, which is often obstructed in acute cholecystitis, by observing whether the gallbladder fills with tracer.
*Emergency cholecystectomy*
- **Acute cholecystitis** usually requires cholecystectomy, but it's typically performed **after confirmation** of the diagnosis, often after a period of stabilization with antibiotics and fluids, not immediately as an emergency for this stable patient.
- There is no evidence of severe complications such as **gallbladder perforation** or gangrene that would necessitate immediate emergency surgery without further diagnostic confirmation.
*CT scan*
- A **CT scan** is not the primary imaging modality for acute cholecystitis as it is **less sensitive** than ultrasound or cholescintigraphy for detecting gallbladder inflammation and cystic duct obstruction.
- While CT can identify complications such as abscess formation or perforation, the initial diagnostic work-up should focus on confirming the inflammation of the gallbladder itself.
*Reassurance and close follow up*
- The patient's symptoms (severe **colicky pain**, fever, **leukocytosis**, elevated liver enzymes) indicate an **acute inflammatory process** requiring active medical management and diagnosis, not mere reassurance.
- Delaying appropriate diagnosis and treatment for acute cholecystitis can lead to severe complications like gallbladder perforation, sepsis, or cholangitis.
*Percutaneous cholecystostomy*
- **Percutaneous cholecystostomy** is generally reserved for patients with acute cholecystitis who are **too unstable for surgery**, or in cases where surgical risk is very high.
- The patient is hemodynamically stable and does not have contraindications for surgery, making a definitive surgical approach (after diagnosis) preferable over a temporizing measure.
Gallbladder and biliary tract disorders US Medical PG Question 5: An otherwise healthy 56-year-old woman comes to the physician because of a 3-year history of intermittent upper abdominal pain. She has had no nausea, vomiting, or change in weight. Physical examination shows no abnormalities. Laboratory studies are within normal limits. Abdominal ultrasonography shows a hyperechogenic rim-like calcification of the gallbladder wall. The finding in this patient's ultrasonography increases the risk of which of the following conditions?
- A. Gallbladder empyema
- B. Pyogenic liver abscess
- C. Gallbladder carcinoma (Correct Answer)
- D. Hepatocellular carcinoma
- E. Acute pancreatitis
Gallbladder and biliary tract disorders Explanation: ***Gallbladder carcinoma***
- The hyperechogenic rim-like calcification of the gallbladder wall described is characteristic of a **porcelain gallbladder**.
- A **porcelain gallbladder** significantly increases the risk of developing adenocarcinoma of the gallbladder, making regular surveillance or prophylactic cholecystectomy often recommended.
*Gallbladder empyema*
- **Gallbladder empyema** is characterized by the presence of pus within the gallbladder, usually due to severe acute cholecystitis with bacterial infection and obstruction.
- While it would present with pain, it's typically associated with **fever, leukocytosis**, and more acute, severe symptoms, not primarily a calcified wall.
*Pyogenic liver abscess*
- **Pyogenic liver abscess** is a collection of pus in the liver, often caused by bacterial infection spreading from the biliary tract or other abdominal infections.
- This condition would typically present with **fever, right upper quadrant pain, and abnormal liver function tests**, none of which are indicated by a calcified gallbladder wall.
*Hepatocellular carcinoma*
- **Hepatocellular carcinoma (HCC)** is a primary liver cancer, most commonly associated with chronic liver diseases like **hepatitis B, hepatitis C, or cirrhosis**.
- It is not directly linked to gallbladder calcification and would not be increased by the finding of a porcelain gallbladder.
*Acute pancreatitis*
- **Acute pancreatitis** is inflammation of the pancreas, often caused by gallstones or alcohol abuse, presenting with severe epigastric pain radiating to the back, nausea, and elevated lipase/amylase.
- While gallstones can cause pancreatitis, a calcified gallbladder wall itself does not directly increase the risk of acute pancreatitis compared to the general risk of gallstone disease.
Gallbladder and biliary tract disorders US Medical PG Question 6: A 41-year-old G3P3 woman presents with acute on chronic right upper quadrant abdominal pain. She says that her current symptoms acutely onset 8 hours ago after eating a large meal and have not improved. She describes the pain as severe, sharp and cramping in character, and localized to the right upper quadrant. She also describes feeling nauseous. The patient says she has had similar less severe episodes intermittently for the past 2 years, usually precipitated by the intake of fatty foods. She denies any history of fever or jaundice. Vital signs are stable. Physical examination is unremarkable, and laboratory findings show normal liver function tests and normal serum bilirubin and serum amylase levels. Ultrasonography of the abdomen reveals multiple stones in the gallbladder. The patient is managed symptomatically for this episode, and after a few months, undergoes elective cholecystectomy, which reveals multiple stones in her gallbladder as shown in the figure (see image). Which of the following best describes these gallstones?
- A. These are usually radiopaque on X-ray imaging.
- B. They are formed due to elevated uric acid in the blood.
- C. These are seen in patients with chronic hemolysis.
- D. They are formed due to the release of beta-glucuronidase from infecting bacteria.
- E. They are formed due to bile supersaturated with cholesterol. (Correct Answer)
Gallbladder and biliary tract disorders Explanation: ***They are formed due to bile supersaturated with cholesterol.***
- The patient's history of **postprandial right upper quadrant pain**, especially after fatty meals, and the ultrasound showing multiple gallstones, points to **cholesterol cholelithiasis**, which is caused by supersaturation of bile with cholesterol.
- **Cholesterol stones** are the most common type of gallstones, accounting for about 80% of cases in Western countries, and their formation is linked to factors like obesity, rapid weight loss, and certain medications.
*These are usually radiopaque on X-ray imaging.*
- **Cholesterol stones** are primarily composed of cholesterol, which is not radiopaque, making them **radiolucent** in about 80% of cases on plain X-rays.
- Their presence is typically detected by **ultrasonography**, which visualizes the stones regardless of their calcium content.
*They are formed due to elevated uric acid in the blood.*
- **Uric acid stones** are a type of **kidney stone**, primarily associated with conditions like gout and hyperuricemia, and are not involved in gallstone formation.
- Gallstones are mineral deposits that form in the gallbladder, primarily from **cholesterol** or **bilirubin**, not uric acid.
*These are seen in patients with chronic hemolysis.*
- **Chronic hemolysis** leads to an increased production of **unconjugated bilirubin**, which can precipitate as **pigment gallstones** (specifically black pigment stones) due to excess bilirubin in the bile.
- The patient's normal bilirubin levels rule out **hemolytic causes** for the gallstones in this case.
*They are formed due to the release of beta-glucuronidase from infecting bacteria.*
- The release of **beta-glucuronidase** from infecting bacteria (e.g., E. coli) in the biliary tract typically leads to the formation of **brown pigment stones**.
- These stones are often found in the bile ducts and are associated with **biliary infections** or stasis, which is not suggested by the patient's presentation or normal lab findings.
Gallbladder and biliary tract disorders US Medical PG Question 7: A 57-year-old man is brought to the emergency department because of a 2-day history of fever and right upper quadrant abdominal pain. Examination shows jaundice. Ultrasonography of the abdomen shows cholelithiasis and marked dilation of the biliary duct. An ERCP is performed and reveals pus with multiple brown concrements draining from the common bile duct. Which of the following is the most likely underlying cause of the patient's findings?
- A. Biliary stricture
- B. Pancreatic cancer
- C. Primary sclerosing cholangitis
- D. Mirizzi syndrome
- E. Choledocholithiasis (Correct Answer)
Gallbladder and biliary tract disorders Explanation: ***Choledocholithiasis***
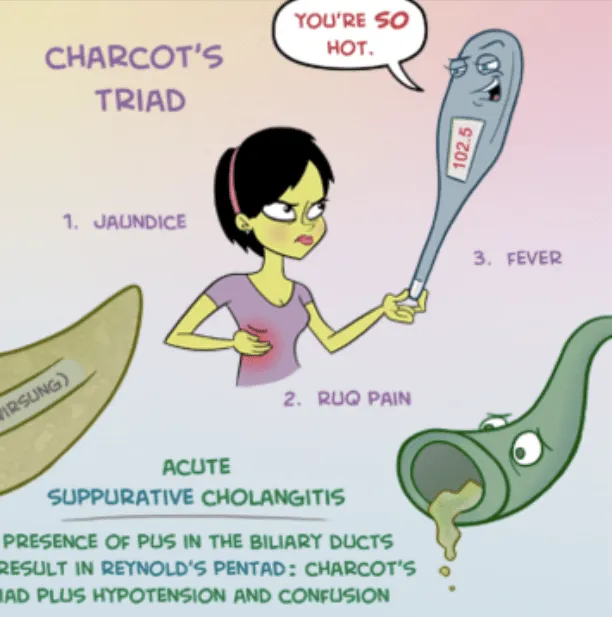
- The patient presents with **fever**, **right upper quadrant pain**, and **jaundice** (Charcot's triad), highly suggestive of **acute cholangitis**.
- The presence of **cholelithiasis** on ultrasound, **dilated common bile duct**, and **pus with multiple brown concrements** draining from the CBD during ERCP confirm **choledocholithiasis** (stones in the common bile duct) as the underlying cause of biliary obstruction and subsequent cholangitis.
- **Brown pigment stones** form within the bile duct itself due to bacterial infection and bile stasis, and their presence is pathognomonic for choledocholithiasis with secondary infection.
*Biliary stricture*
- While a biliary stricture can cause biliary dilation and potentially cholangitis, it typically doesn't present with **multiple brown concrements** draining during ERCP.
- The primary pathology would be ductal narrowing, not intraductal stones.
*Pancreatic cancer*
- Pancreatic cancer can cause biliary obstruction and jaundice, but typically presents with **painless jaundice** rather than the acute febrile presentation seen here.
- Ultrasound would more likely show a pancreatic mass rather than primarily cholelithiasis with intraductal stones.
*Primary sclerosing cholangitis*
- This condition involves chronic **inflammation and fibrosis** of bile ducts leading to multifocal strictures, but is not typically associated with **acute presentation** or **brown pigment stones**.
- PSC often presents with chronic symptoms and is associated with inflammatory bowel disease.
*Mirizzi syndrome*
- Mirizzi syndrome involves an **impacted gallstone in the cystic duct or gallbladder neck** causing extrinsic compression of the common hepatic duct.
- While it can cause biliary obstruction, the key finding of **multiple brown concrements within the common bile duct** indicates primary intraductal stone disease rather than extrinsic compression from a single impacted stone.
Gallbladder and biliary tract disorders US Medical PG Question 8: A 45-year-old woman comes to the emergency department because of right upper abdominal pain and nausea that have become progressively worse since eating a large meal 8 hours ago. She has had intermittent pain similar to this before, but it has never lasted this long. She has a history of hypertension and type 2 diabetes mellitus. She does not smoke or drink alcohol. Current medications include metformin and enalapril. Her temperature is 38.5°C (101.3°F), pulse is 90/min, and blood pressure is 130/80 mm Hg. The abdomen is soft, and bowel sounds are normal. The patient has sudden inspiratory arrest during right upper quadrant palpation. Laboratory studies show a leukocyte count of 13,000/mm3. Serum alkaline phosphatase, total bilirubin, amylase, and aspartate aminotransferase levels are within the reference ranges. Imaging is most likely to show which of the following findings?
- A. Dilated common bile duct with intrahepatic biliary dilatation
- B. Enlargement of the pancreas with peripancreatic fluid
- C. Gallstone in the cystic duct (Correct Answer)
- D. Gas in the gallbladder wall
- E. Decreased echogenicity of the liver
Gallbladder and biliary tract disorders Explanation: ***Gallstone in the cystic duct***
- The patient's presentation with **right upper quadrant pain** after a fatty meal, **nausea**, **fever**, **leukocytosis**, and a positive **Murphy's sign** (inspiratory arrest during palpation) is highly suggestive of **acute cholecystitis**.
- **Acute cholecystitis** is most commonly caused by an obstructing gallstone in the **cystic duct**, leading to inflammation of the gallbladder.
*Dilated common bile duct with intrahepatic biliary dilatation*
- This finding suggests **choledocholithiasis** (gallstone in the common bile duct) or another obstruction of the common bile duct, which would typically cause **elevated bilirubin** and **alkaline phosphatase**.
- These laboratory values are **within normal limits** for this patient, making choledocholithiasis less likely.
*Enlargement of the pancreas with peripancreatic fluid*
- These findings are characteristic of **acute pancreatitis**, which would present with elevated **amylase** and **lipase**.
- The patient's **amylase level is normal**, ruling out acute pancreatitis as the primary diagnosis.
*Gas in the gallbladder wall*
- This indicates **emphysematous cholecystitis**, a severe form of acute cholecystitis typically seen in elderly or immunocompromised patients, often with diabetes.
- While the patient has diabetes, the overall clinical picture does not specifically point to this more advanced and rare complication, and it's not the *most likely* initial finding for typical acute cholecystitis.
*Decreased echogenicity of the liver*
- Decreased echogenicity of the liver is typically associated with conditions like **fatty liver disease** or **hepatitis**.
- While the patient has risk factors for fatty liver (type 2 diabetes), this finding does not explain her acute symptoms of right upper quadrant pain, fever, and Murphy's sign, which point towards gallbladder pathology.
Gallbladder and biliary tract disorders US Medical PG Question 9: A 66-year-old woman comes to the physician because of a 1-week history of pruritic blister formation. Physical examination shows multiple 1–3 cm bullae on the palms, soles, lower legs, and inguinal folds. Gentle rubbing of the skin does not result in sloughing of the epidermis. Immunofluorescence studies of a perilesional skin biopsy specimen are most likely to show deposition of antibodies in which of the following areas?
- A. In dermal papillae
- B. Between epidermal keratinocytes
- C. No staining
- D. In dermal vessel walls
- E. At the dermoepidermal junction (Correct Answer)
Gallbladder and biliary tract disorders Explanation: ***At the dermoepidermal junction***
- This presentation of **tense bullae** on flexural surfaces in an elderly patient, with a negative **Nikolsky's sign** (no epidermal sloughing with rubbing), is classic for **bullous pemphigoid**.
- **Direct immunofluorescence** in bullous pemphigoid typically reveals linear deposits of **IgG** and/or **C3** at the **dermoepidermal junction (basement membrane zone)**.
*In dermal papillae*
- Deposition in dermal papillae is characteristic of **dermatitis herpetiformis**, which typically presents with intensely pruritic papules and vesicles, often on extensor surfaces.
- The morphology and distribution of lesions in this patient (large bullae on palms, soles, inguinal folds) are not consistent with dermatitis herpetiformis.
*Between epidermal keratinocytes*
- Deposition of autoantibodies (IgG) between epidermal keratinocytes is a hallmark of **pemphigus vulgaris**, resulting in suprabasal blistering and a positive **Nikolsky's sign**.
- This patient exhibits **tense bullae** and a **negative Nikolsky's sign**, which rules out pemphigus vulgaris.
*No staining*
- The presence of pruritic blister formation in an elderly patient strongly suggests an autoimmune bullous disease, for which direct immunofluorescence is a key diagnostic tool.
- A lack of staining would indicate a non-immunological cause of blistering or a different type of dermatological condition, which is unlikely given the clinical picture.
*In dermal vessel walls*
- Immune complex deposition in dermal vessel walls is characteristic of diseases like **leukocytoclastic vasculitis**, which presents with palpable purpura rather than tense bullae.
- The clinical presentation of pruritic bullae in this patient is inconsistent with a vasculitis.
Gallbladder and biliary tract disorders US Medical PG Question 10: A 7-year-old boy is brought to the emergency department by his parents. He is complaining of left-sided knee pain which has progressively increased in severity over the past 2 days. It started when he was playing football with his brothers but he does not recall falling or getting any injury. Past medical history is significant for prolonged bleeding and easy bruising. His maternal uncle has similar problems. Physical exam reveals swollen and painful left knee. His laboratory investigations reveal:
Hemoglobin 11.8 g/dL
WBC count 7,000/mL
Platelets 250,000/mL
INR 0.9
aPTT 62 sec, fully corrected with a mixing study
Which of the following disorders have the same mode of inheritance as this patient’s disease?
- A. Hereditary spherocytosis
- B. Alkaptonuria
- C. Duchenne muscular dystrophy (Correct Answer)
- D. Sickle cell disease
- E. Huntington's disease
Gallbladder and biliary tract disorders Explanation: ***Duchenne muscular dystrophy***
- The patient's presentation with **hemarthrosis** (knee pain and swelling without trauma), **prolonged bleeding**, and **easy bruising**, along with a **prolonged aPTT** that corrects with a mixing study, is highly suggestive of **hemophilia A or B**. Both conditions are **X-linked recessive disorders**, affecting males predominantly.
- **Duchenne muscular dystrophy** is also an **X-linked recessive disorder**, making its mode of inheritance identical to the suspected diagnosis of hemophilia in this patient.
*Hereditary spherocytosis*
- This condition is inherited in an **autosomal dominant** pattern, which is different from the mode of inheritance for hemophilia.
- It is characterized by **hemolytic anemia** due to a defect in red blood cell membrane proteins.
*Alkaptonuria*
- Alkaptonuria is an **autosomal recessive** disorder, caused by a deficiency of homogentisate 1,2-dioxygenase.
- It leads to the accumulation of **homogentisic acid**, causing **dark urine** when exposed to air, **ochronosis**, and **arthropathy**, distinct from the patient's bleeding disorder.
*Sickle cell disease*
- **Sickle cell disease** is an **autosomal recessive** disorder, characterized by abnormal hemoglobin leading to chronic hemolytic anemia and vaso-occlusive crises.
- While it can cause joint pain due to avascular necrosis or infarction, its inheritance pattern is different from the patient's condition.
*Huntington's disease*
- **Huntington's disease** is an **autosomal dominant** neurodegenerative disorder that manifests with progressive motor, cognitive, and psychiatric symptoms, typically in middle age.
- Its inheritance pattern and clinical presentation are distinct from the patient's bleeding disorder.
More Gallbladder and biliary tract disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.