Endocrine pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Endocrine pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Endocrine pathology US Medical PG Question 1: A 37-year-old woman comes to the physician because of irregular menses and generalized fatigue for the past 4 months. Menses previously occurred at regular 25- to 29-day intervals and lasted for 5 days but now occur at 45- to 60-day intervals. She has no history of serious illness and takes no medications. She is 155 cm (5 ft 1 in) tall and weighs 89 kg (196 lb); BMI is 37 kg/m2. Her temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 146/100 mm Hg. Examination shows facial hair as well as comedones on the face and back. There are multiple ecchymotic patches on the trunk. Neurological examination shows weakness of the iliopsoas and biceps muscles bilaterally. Laboratory studies show:
Hemoglobin 13.1 g/dL
Leukocyte count 13,500/mm3
Platelet count 510,000/mm3
Serum
Na+ 145 mEq/L
K+ 3.3 mEq/L
Cl- 100 mEq/L
Glucose 188 mg/dL
Which of the following is the most likely diagnosis?
- A. Pheochromocytoma
- B. Cushing syndrome (Correct Answer)
- C. Primary hyperaldosteronism
- D. Polycystic ovarian syndrome
- E. Hypothyroidism
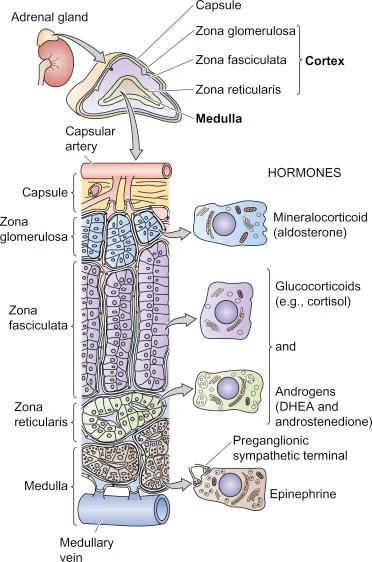
Endocrine pathology Explanation: ***Cushing syndrome***
- The constellation of **obesity**, **hypertension**, **irregular menses**, **hirsutism** (facial hair), **acne** (comedones), **easy bruising** (ecchymotic patches), **proximal muscle weakness** (iliopsoas and biceps), **leukocytosis**, **thrombocytosis**, **hypokalemia**, and **hyperglycemia** is highly characteristic of Cushing syndrome due to chronic glucocorticoid excess.
- The patient's **truncal obesity** (BMI 37 kg/m2) and the metabolic derangements further support this diagnosis.
*Pheochromocytoma*
- While pheochromocytoma can cause **hypertension** and **tachycardia**, it typically presents with **episodic symptoms** like palpitations, sweating, and headaches.
- It does not explain the other prominent features such as **hirsutism**, **menstrual irregularities**, **proximal muscle weakness**, or **easy bruising**.
*Primary hyperaldosteronism*
- This condition is characterized by **hypertension** and **hypokalemia**, often leading to fatigue.
- However, it does not account for the patient's **hirsutism**, **menstrual irregularities**, **obesity**, **easy bruising**, **muscle weakness**, **acne**, or **hyperglycemia**.
*Polycystic ovarian syndrome*
- PCOS causes **irregular menses**, **hirsutism**, **acne**, and **obesity**, which are present in this patient.
- However, it typically does not cause **hypertension**, **hypokalemia**, **easy bruising**, or **proximal muscle weakness**, making Cushing syndrome a more encompassing diagnosis.
*Hypothyroidism*
- Hypothyroidism can lead to **fatigue**, **menstrual irregularities**, and **weight gain**.
- However, it typically presents with **bradycardia**, **dry skin**, **constipation**, and **cold intolerance**, not **hypertension**, **hirsutism**, **acne**, **easy bruising**, or **proximal muscle weakness**.
Endocrine pathology US Medical PG Question 2: A 45-year-old woman comes to the physician because of fatigue, irregular menses, and recurrent respiratory infections for the past 6 months. Her blood pressure is 151/82 mm Hg. Physical examination shows a round face, thinning of the skin, and multiple bruises on her arms. Further studies confirm the diagnosis of an ACTH-secreting pituitary adenoma. This patient is at greatest risk for which of the following?
- A. Weight loss
- B. Eosinophilia
- C. Bitemporal hemianopsia
- D. Hypoglycemia
- E. Pathologic fracture (Correct Answer)
Endocrine pathology Explanation: ***Pathologic fracture***
- This patient has **Cushing's disease** due to an **ACTH-secreting pituitary adenoma**, leading to excess cortisol.
- **Excess cortisol** causes **osteoporosis** by increasing bone resorption and decreasing bone formation, significantly raising the risk of **pathologic fractures**.
- This is the **greatest risk** because **all patients** with chronic hypercortisolism develop bone loss, making fractures highly likely.
*Weight loss*
- Patients with Cushing's disease typically experience **weight gain**, particularly centrally (truncal obesity), due to **cortisol-induced fat redistribution**.
- **Fatigue** is common, but weight loss is not a characteristic feature of Cushing's syndrome.
*Eosinophilia*
- **Hypercortisolism** (Cushing's syndrome) usually causes **eosinopenia** (decreased eosinophil count) and **lymphopenia**, not eosinophilia.
- Cortisol has an anti-inflammatory and immunosuppressive effect, leading to a reduction in circulating eosinophils and lymphocytes.
*Bitemporal hemianopsia*
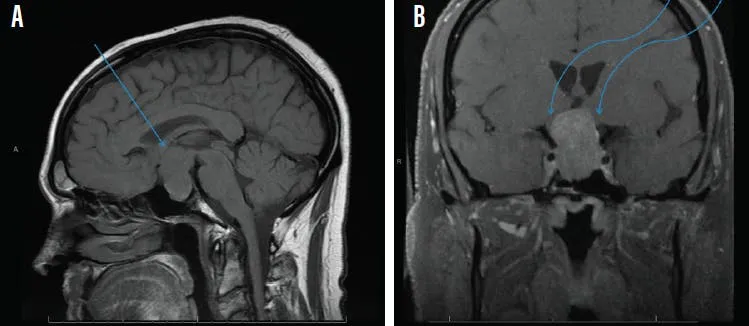
- While an **ACTH-secreting pituitary adenoma** is present, **bitemporal hemianopsia** occurs only when a pituitary tumor becomes a **macroadenoma** (>10mm) and compresses the **optic chiasm**.
- Most ACTH-secreting adenomas are **microadenomas** (<10mm) that cause symptoms through **hormonal excess**, not mass effect.
- The clinical picture here reflects **Cushing's syndrome** from hypercortisolism, which affects **all patients** regardless of tumor size, whereas visual field defects occur only with large tumors.
*Hypoglycemia*
- **Excess cortisol** **increases gluconeogenesis** and **insulin resistance**, leading to **hyperglycemia**, not hypoglycemia.
- This is a common metabolic complication of Cushing's syndrome, often progressing to **steroid-induced diabetes mellitus**.
Endocrine pathology US Medical PG Question 3: A 48-year-old woman presents to her primary care physician with complaints of persistent fatigue, dizziness, and weight loss for the past 3 months. She has a history of hypothyroidism and takes thyroxine replacement. Her blood pressure is 90/60 mm Hg in a supine position and 65/40 mm Hg while sitting, temperature is 36.8°C (98.2°F), and pulse is 75/min. On physical examination, there is a mild increase in thyroid size, with a rubbery consistency. Her skin shows diffuse hyperpigmentation, more pronounced in the oral mucosa and palmar creases. Which of the following best represent the etiology of this patient’s condition?
- A. Prolonged corticosteroid therapy
- B. ↓ corticotropin-releasing hormone secretion from the hypothalamus
- C. Autoimmune destruction of the adrenal gland (Correct Answer)
- D. ↓ adrenocorticotropic hormone secretion from the pituitary gland
- E. ↑ iron absorption and deposition in the body
Endocrine pathology Explanation: ***Autoimmune destruction of the adrenal gland***
- The patient's symptoms, including **fatigue**, **dizziness**, **weight loss**, **hypotension**, and especially **diffuse hyperpigmentation of the skin and oral mucosa**, are classic signs of **primary adrenal insufficiency (Addison's disease)**.
- Given the history of **hypothyroidism** (another autoimmune disorder), **autoimmune destruction of the adrenal glands** is the most likely underlying cause.
*Prolonged corticosteroid therapy*
- **Prolonged corticosteroid therapy** can lead to **secondary adrenal insufficiency** by suppressing the **hypothalamic-pituitary-adrenal (HPA) axis**.
- However, this would typically cause **ACTH deficiency**, leading to **pale skin** rather than hyperpigmentation, as the melanocyte-stimulating hormone (MSH) levels would also be low.
*↓ corticotropin-releasing hormone secretion from the hypothalamus*
- Decreased **CRH secretion** would result in **secondary adrenal insufficiency**, characterized by **low ACTH** and subsequently low cortisol.
- This condition does not cause **hyperpigmentation** because MSH levels, which are co-secreted with ACTH from a common precursor (POMC), would also be low.
*↓ adrenocorticotropic hormone secretion from the pituitary gland*
- A reduction in **ACTH secretion** (secondary adrenal insufficiency) causes symptoms of **cortisol deficiency** but typically leads to **pallor** due to the lack of MSH stimulation.
- It does not cause the **hyperpigmentation** seen in this patient, which is a hallmark of primary adrenal insufficiency where high ACTH (and MSH) levels stimulate melanocytes.
*↑ iron absorption and deposition in the body*
- Increased **iron absorption and deposition** is characteristic of **hemochromatosis**, which can cause fatigue and skin bronzing, but not the specific hyperpigmentation patterns (oral mucosa, palmar creases) or the significant hypotension and weight loss seen here.
- Hemochromatosis primarily affects the liver, heart, and pancreas, and does not involve adrenal gland dysfunction in this manner.
Endocrine pathology US Medical PG Question 4: A 37-year-old female presents to her primary care physician with constipation and abdominal pain. She notes that the pain has been present for several days and is not related to food. She also reports increased urinary frequency without incontinence, as well as increased thirst. She takes no medications, but notes taking vitamin supplements daily. Her vital signs are: BP 130/72 mmHg, HR 82 bpm, T 97.0 degrees F, and RR 12 bpm. Lab studies reveal: Na 139, K 4.1, Cl 104, HCO3 25, Cr 0.9, and Ca 12.4. Further studies show an increased ionized calcium, decreased PTH, and normal phosphate. What is the most likely cause of this patient's symptoms?
- A. Vitamin overdose (Correct Answer)
- B. Vitamin deficiency
- C. Inherited disorder
- D. Plasma cell neoplasm
- E. Primary endocrine dysfunction
Endocrine pathology Explanation: ***Vitamin overdose***
- The patient's symptoms of **constipation**, **abdominal pain**, **increased urinary frequency**, and **thirst** are classic signs of **hypercalcemia**.
- The lab findings of **hypercalcemia (Ca 12.4)**, **increased ionized calcium**, **decreased PTH**, and increased phosphate, coupled with a history of daily vitamin supplements, strongly suggest **Vitamin D toxicity** from overdose, which leads to increased calcium absorption and bone resorption.
*Vitamin deficiency*
- Vitamin deficiencies typically do not cause **hypercalcemia**; in fact, severe **Vitamin D deficiency** can lead to **hypocalcemia** and **secondary hyperparathyroidism**.
- Symptoms associated with common vitamin deficiencies (e.g., scurvy, rickets) are not consistent with this patient's presentation.
*Inherited disorder*
- While some **inherited disorders** (e.g., **Familial Hypocalciuric Hypercalcemia**) can cause hypercalcemia, the distinguishing feature is typically a **normal or mildly elevated PTH** and **low urinary calcium excretion**, which is not entirely aligned with the presented PTH and phosphate levels and the acute onset suggested by symptoms.
- The patient's history of **vitamin supplement** use provides a more direct and likely explanation for acute hypercalcemia.
*Plasma cell neoplasm*
- **Plasma cell neoplasms** like **multiple myeloma** can cause **hypercalcemia** due to increased bone resorption from osteoclast-activating factors.
- However, hypercalcemia from these conditions is often accompanied by other signs of malignancy such as **renal failure**, **anemia**, or **bone lesions**, which are not reported in this case, and the **decreased PTH** points away from malignancy-associated humorally mediated hypercalcemia.
*Primary endocrine dysfunction*
- **Primary hyperparathyroidism** is a common cause of **hypercalcemia**, but it is characterized by **elevated or inappropriately normal PTH levels** in the presence of hypercalcemia, which contradicts the **decreased PTH** found in this patient.
- Other endocrine causes of hypercalcemia, such as **thyrotoxicosis** or **adrenal insufficiency**, present with distinct clinical features not described here.
Endocrine pathology US Medical PG Question 5: A 53-year-old man comes to the physician because of fatigue, recurrent diarrhea, and an 8-kg (17.6-lb) weight loss over the past 6 months. He has a 4-month history of recurrent blistering rashes on different parts of his body that grow and develop into pruritic, crusty lesions before resolving spontaneously. Physical examination shows scaly lesions in different phases of healing with central, bronze-colored induration around the mouth, perineum, and lower extremities. Laboratory studies show:
Hemoglobin 10.1 mg/dL
Mean corpuscular volume 85 μm3
Mean corpuscular hemoglobin 30.0 pg/cell
Serum
Glucose 236 mg/dL
Abdominal ultrasonography shows a 3-cm, solid mass located in the upper abdomen. This patient's mass is most likely derived from which of the following types of cells?
- A. Gastrointestinal enterochromaffin cells
- B. Pancreatic β-cells
- C. Pancreatic δ-cells
- D. Pancreatic α-cells (Correct Answer)
- E. Gastric G-cells
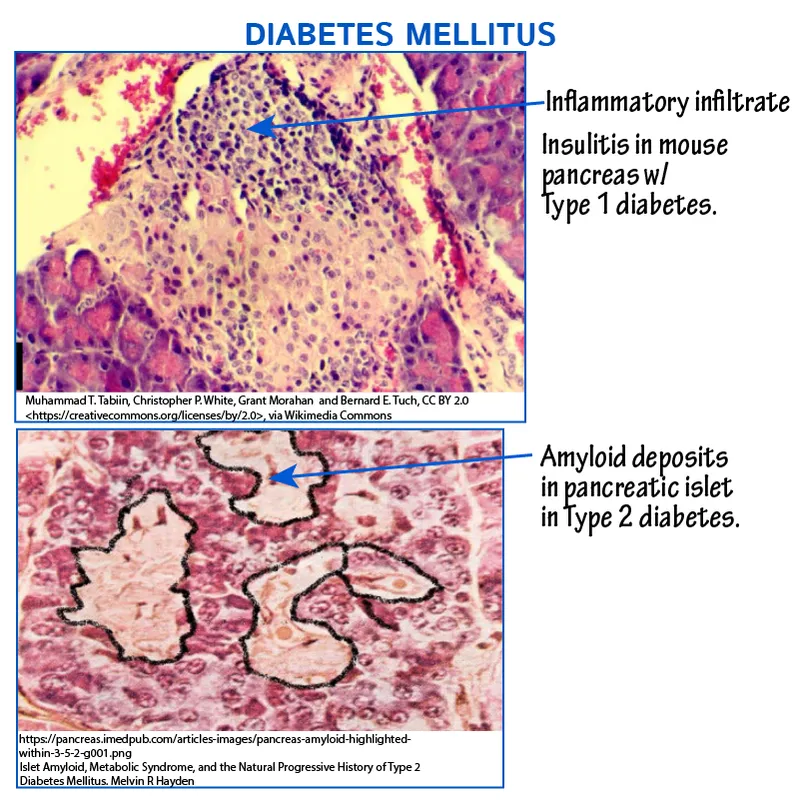
Endocrine pathology Explanation: ***Pancreatic α-cells***
- The patient's symptoms of **fatigue, recurrent diarrhea, weight loss, blistering rash (necrolytic migratory erythema)**, and **hyperglycemia** are classic features of a **glucagonoma**.
- A **glucagonoma** is a tumor of the pancreatic α-cells that **secretes excessive glucagon**, leading to these characteristic signs and symptoms, supported by the presence of an **upper abdominal mass**.
*Gastrointestinal enterochromaffin cells*
- Tumors of gastrointestinal enterochromaffin cells (carcinoid tumors) typically produce **serotonin** and present with flushing, diarrhea, bronchospasm, and valvular heart disease, not the skin rash or hyperglycemia seen here.
- While carcinoid tumors can cause diarrhea, the additional symptoms of **necrolytic migratory erythema** and **diabetes** are not characteristic.
*Pancreatic β-cells*
- Tumors of pancreatic β-cells (**insulinomas**) produce excessive insulin, leading to **hypoglycemia**, not the hyperglycemia observed in this patient.
- Insulinomas cause symptoms like sweating, tremors, confusion, and palpitations, which are inconsistent with the patient's presentation.
*Pancreatic δ-cells*
- Pancreatic δ-cell tumors (**somatostatinomas**) secrete **somatostatin**, which can cause **diabetes mellitus**, steatorrhea, and gallstones.
- While diabetes is present, the characteristic **necrolytic migratory erythema** and severe diarrhea are less common with somatostatinomas.
*Gastric G-cells*
- Tumors of gastric G-cells (**gastrinomas**) secrete **gastrin**, leading to **Zollinger-Ellison syndrome**, characterized by severe peptic ulcers, abdominal pain, and chronic diarrhea.
- Gastrinomas do not typically cause **necrolytic migratory erythema** or significant hyperglycemia.
Endocrine pathology US Medical PG Question 6: A 43-year-old man visits his physician’s office for a routine check-up. He tells his physician that he is otherwise healthy, except for persistent headaches that he gets every morning. Upon further questioning, he reveals that he has been changing glove sizes quite frequently over the past couple of years. His wedding ring doesn’t fit him anymore. He thought this was probably due to some extra weight that he has put on. Vital signs include: blood pressure 160/90 mm Hg, heart rate 82/min, and respiratory rate 21/min. His current physical appearance is cataloged in the image. His past medical history is significant for diabetes for which he has been receiving treatment for the past 2 years. Which of the following organs most likely has a structural abnormality that has resulted in this patient’s current presentation?
- A. Liver
- B. Pancreas
- C. Posterior pituitary gland
- D. Lungs
- E. Anterior pituitary gland (Correct Answer)
Endocrine pathology Explanation: ***Anterior pituitary gland***
- The patient's symptoms, including **persistent headaches**, **increasing glove and ring sizes**, and **physical appearance** suggestive of facial and acral growth, are classic signs of **acromegaly**.
- **Acromegaly** is most commonly caused by a **growth hormone-secreting adenoma** of the **anterior pituitary gland**, leading to excess growth hormone production.
*Liver*
- While the liver plays a role in metabolism and produces **insulin-like growth factor 1 (IGF-1)**, it is not the primary site of pathology in acromegaly.
- Liver abnormalities would typically present with symptoms such as jaundice, fatigue, or abdominal pain, which are not the patient's primary complaints.
*Pancreas*
- The pancreas is responsible for insulin production, and its dysfunction leads to **diabetes mellitus**. While the patient has diabetes, this is often a **secondary complication** of acromegaly due to insulin resistance, rather than the primary cause of the growth-related symptoms.
- A primary pancreatic structural abnormality would not explain the generalized growth of extremities and facial features.
*Posterior pituitary gland*
- The **posterior pituitary gland** primarily secretes **vasopressin (ADH)** and **oxytocin**.
- Structural abnormalities here would typically result in disorders like **diabetes insipidus** (due to ADH deficiency) or syndromes related to oxytocin, not the growth-related symptoms seen in this patient.
*Lungs*
- Lung abnormalities can lead to various respiratory symptoms, such as shortness of breath, cough, or chest pain.
- There is no direct link between a primary structural abnormality of the lungs and the systemic growth changes or persistent headaches described in this patient.
Endocrine pathology US Medical PG Question 7: A 55-year-old man presents to the emergency department because of an excruciating headache that started suddenly after he got home from work. He also reports having double vision. Specifically, in the last week he almost got into two car accidents with vehicles that "came out of nowhere" while he was trying to merge on the highway. Physical examination is notable for ptosis of the left eye, which is also inferiorly and laterally deviated. The patient is treated emergently and then started on a hormone replacement in order to avoid life-threatening post-treatment complications. The patient's current presentation was associated with a pathologic process that existed for several months prior to this event. Which of the following symptoms could this patient have experienced as part of that pre-existing pathology?
- A. Kidney stones
- B. Hyperkalemia
- C. Increased hat size (Correct Answer)
- D. Gastric ulcers
- E. Hypoglycemia
Endocrine pathology Explanation: ***Increased hat size***
- The emergent treatment and subsequent hormone replacement for a life-threatening post-treatment complication, along with double vision and an excruciating headache, suggests a diagnosis of **pituitary apoplexy**.
- Pituitary apoplexy is often due to an acute hemorrhage or infarction within a pre-existing pituitary adenoma. A large adenoma can cause symptoms like **increased hat size** due to the progressive growth of facial bones and skull, a hallmark of **acromegaly** if the adenoma secretes growth hormone.
*Kidney stones*
- While a pituitary adenoma secreting **ACTH** (Cushing's disease) can lead to **hypercalciuria** and kidney stones, this specific symptom is not as directly indicative of a pre-existing pathology that would explain the acute presentation and subsequent hormone replacement.
- Kidney stones are not a primary or direct symptom of a pituitary adenoma in the way that acromegaly-related changes are.
*Hyperkalemia*
- Hyperkalemia is typically associated with conditions like **adrenal insufficiency** or **renal failure**, not directly with the pre-existing pituitary pathology leading to apoplexy.
- Insufficiency of mineralocorticoids (e.g., in adrenal crisis, which can be a complication of pituitary apoplexy due to ACTH deficiency) causes **hyponatremia** and **hyperkalemia**, but this would be a consequence of the acute event and not a pre-existing symptom of the adenoma itself.
*Gastric ulcers*
- Although conditions like **Zollinger-Ellison syndrome** (due to a **gastrinoma**) involve ulcers, and **MEN1 syndrome** can include pituitary adenomas and gastrinomas, gastric ulcers are not a direct or common pre-existing symptom of a pituitary adenoma itself.
- Additionally, **Cushing's syndrome** (which can be caused by an ACTH-secreting pituitary adenoma) can be associated with an increased risk of peptic ulcers due to high cortisol levels, but it's not a primary or specific finding.
*Hypoglycemia*
- Hypoglycemia can occur with **adrenal insufficiency** or **growth hormone deficiency**, both of which can be consequences of pituitary dysfunction, particularly if the adenoma destroys normal pituitary tissue or after apoplexy.
- However, hypoglycemia is often an acute or late symptom of hormonal deficiencies, rather than a prominent pre-existing symptom of the growing adenoma prior to the acute event, especially compared to the chronic changes of acromegaly.
Endocrine pathology US Medical PG Question 8: A 52-year-old woman presents to her primary care physician with symptoms of heat intolerance, unintentional weight loss, feelings of anxiety, and excessive energy that hinder her from falling asleep at night. On physical exam, the patient is found to have mildly protuberant eyes bilaterally as well as discoloration and swelling of her shins. Which of the following lab results would most likely be present in this patient?
- A. Decreased serum TSH (Correct Answer)
- B. Increased anti-mitochondrial antibodies
- C. Decreased free T4
- D. Increased serum TSH
- E. Decreased anti-TSH receptor antibodies
Endocrine pathology Explanation: ***Decreased serum TSH***
- The patient's symptoms (heat intolerance, weight loss, anxiety, insomnia, protuberant eyes, pretibial myxedema) are classic for **hyperthyroidism**, specifically **Graves' disease**.
- In primary hyperthyroidism, the thyroid gland overproduces thyroid hormones (T3 and T4), which **negatively feedback** on the pituitary, leading to a decreased or **undetectable serum TSH**.
*Increased anti-mitochondrial antibodies*
- **Anti-mitochondrial antibodies (AMAs)** are the hallmark of **primary biliary cholangitis**, a chronic autoimmune liver disease.
- This condition presents with symptoms like **fatigue, pruritus, and jaundice**, which are not observed in this patient.
*Decreased free T4*
- A **decreased free T4** indicates **hypothyroidism**, where the thyroid gland produces insufficient thyroid hormones.
- This would present with symptoms opposite to those described, such as **cold intolerance, weight gain, fatigue, and bradycardia**.
*Decreased anti-TSH receptor antibodies*
- **Anti-TSH receptor antibodies (TRAb)** are characteristic of Graves' disease, and they are typically **stimulatory** (thyroid-stimulating immunoglobulins), meaning they mimic TSH and **increase** thyroid hormone production.
- A decrease in these antibodies would suggest a *reduction* in the autoimmune stimulation, which is inconsistent with the patient's active hyperthyroid state.
- In this patient with clear Graves' disease, these antibodies would be **elevated**, not decreased.
*Increased serum TSH*
- An **increased serum TSH** is indicative of **primary hypothyroidism**, where the pituitary gland attempts to stimulate an underactive thyroid.
- This would lead to symptoms of **fatigue, weight gain, cold intolerance, and bradycardia**, which contradict the patient's presentation.
Endocrine pathology US Medical PG Question 9: An otherwise healthy 47-year-old woman comes to the physician for the evaluation of a 4-month history of worsening fatigue and constipation. She has also noticed that her cheeks appear fuller and her voice has become hoarse. Her temperature is 36.3°C (97.3°F) and pulse is 59/min. Examination of the neck shows a painless, mildly enlarged thyroid gland. Her skin is dry and cool and her nails appear brittle. Serum studies show antibodies against thyroid peroxidase. A biopsy of the thyroid gland is most likely to show which of the following?
- A. Tall follicular cells, scalloped colloid, and vascular congestion
- B. Lymphocytic infiltration, Hürthle cells, and germinal centers (Correct Answer)
- C. Large, irregular nuclei, nuclear grooves, and Psammoma bodies
- D. Spindle cells, pleomorphic giant cells, and mitotic figures
- E. Multinucleated giant cells, macrophages, and degenerated follicular cells
Endocrine pathology Explanation: ***Lymphocytic infiltration, Hürthle cells, and germinal centers***
- The patient's symptoms (fatigue, constipation, fuller cheeks, hoarse voice, dry and cool skin, brittle nails, bradycardia, mildly enlarged thyroid gland) are classic for **hypothyroidism**. The presence of **anti-thyroid peroxidase antibodies** confirms an autoimmune etiology, specifically **Hashimoto's thyroiditis**.
- **Hashimoto's thyroiditis** is characterized pathologically by extensive **lymphocytic infiltration** of the thyroid parenchyma, the presence of **Hürthle cells** (metaplastic follicular cells with abundant eosinophilic cytoplasm), and the formation of **germinal centers** within the thyroid gland.
*Tall follicular cells, scalloped colloid, and vascular congestion*
- This description is characteristic of **Graves' disease**, an autoimmune cause of **hyperthyroidism**.
- The patient's symptoms and signs (e.g., bradycardia, dry skin, constipation) are consistent with **hypothyroidism**, not hyperthyroidism.
*Large, irregular nuclei, nuclear grooves, and Psammoma bodies*
- These are classic histological features of **papillary thyroid carcinoma**, the most common type of thyroid cancer.
- While thyroid nodules can occur in Hashimoto's, the overall clinical picture points strongly to a benign autoimmune inflammatory process, not malignancy.
*Spindle cells, pleomorphic giant cells, and mitotic figures*
- This describes **anaplastic thyroid carcinoma**, a highly aggressive and undifferentiated thyroid malignancy.
- Anaplastic carcinoma typically presents as a rapidly enlarging, painful neck mass in older individuals, which is not consistent with this patient's chronic, milder presentation.
*Multinucleated giant cells, macrophages, and degenerated follicular cells*
- This histological pattern is characteristic of **subacute granulomatous thyroiditis (de Quervain's thyroiditis)**.
- Subacute thyroiditis typically presents with painful thyroid enlargement and often follows a viral infection, which is not suggested by the patient's symptoms or antibody findings.
Endocrine pathology US Medical PG Question 10: A 36-year-old man is admitted to the hospital because of a 1-day history of epigastric pain and vomiting. He has had similar episodes of epigastric pain in the past. He drinks 8 oz of vodka daily. Five days after admission, the patient develops aspiration pneumonia and sepsis. Despite appropriate therapy, the patient dies. At autopsy, the pancreas appears gray, enlarged, and nodular. Microscopic examination of the pancreas shows localized deposits of calcium. This finding is most similar to an adaptive change that can occur in which of the following conditions?
- A. Primary hyperparathyroidism
- B. Sarcoidosis
- C. Multiple myeloma
- D. Congenital CMV infection
- E. Chronic kidney disease (Correct Answer)
Endocrine pathology Explanation: ***Chronic kidney disease***
- The pancreatic finding represents **dystrophic calcification** (calcium deposition in damaged tissue with normal serum calcium levels), a consequence of chronic pancreatitis.
- **Chronic kidney disease** is the most similar condition because it also involves pathologic calcification as an adaptive/pathologic change, though through a different mechanism called **metastatic calcification**.
- In CKD, **hyperphosphatemia** and secondary **hyperparathyroidism** elevate the serum calcium-phosphate product, leading to calcium deposition in **normal tissues** (blood vessels, kidneys, lungs, gastric mucosa).
- Both conditions demonstrate **pathologic calcification as a tissue response** to metabolic derangement, making CKD the best answer among the options provided.
*Primary hyperparathyroidism*
- Causes **hypercalcemia** and **hypophosphatemia** due to excess PTH secretion.
- Can lead to **metastatic calcification** in normal tissues, but is less commonly associated with widespread tissue calcification compared to CKD.
- The mineral imbalance pattern differs from CKD (high calcium, low phosphate vs. high phosphate, variable calcium).
*Sarcoidosis*
- Causes **hypercalcemia** due to increased 1,25-dihydroxyvitamin D production by activated macrophages in granulomas.
- Can result in **metastatic calcification**, particularly nephrocalcinosis.
- However, this is less common and less extensive than the calcification seen in CKD.
*Multiple myeloma*
- Produces **hypercalcemia** through osteolytic bone destruction and cytokine-mediated bone resorption.
- Can theoretically cause **metastatic calcification**, but this is not a typical or prominent feature of the disease.
- The hypercalcemia is usually addressed before significant tissue calcification occurs.
*Congenital CMV infection*
- Causes **dystrophic calcification** in damaged tissues, typically **periventricular intracranial calcifications**.
- While this involves the same type of calcification (dystrophic), CMV infection is not characterized by systemic or progressive calcification as an adaptive metabolic response.
- The calcifications are focal sequelae of viral tissue damage, not a widespread metabolic derangement.
More Endocrine pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.