Bone and joint pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bone and joint pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
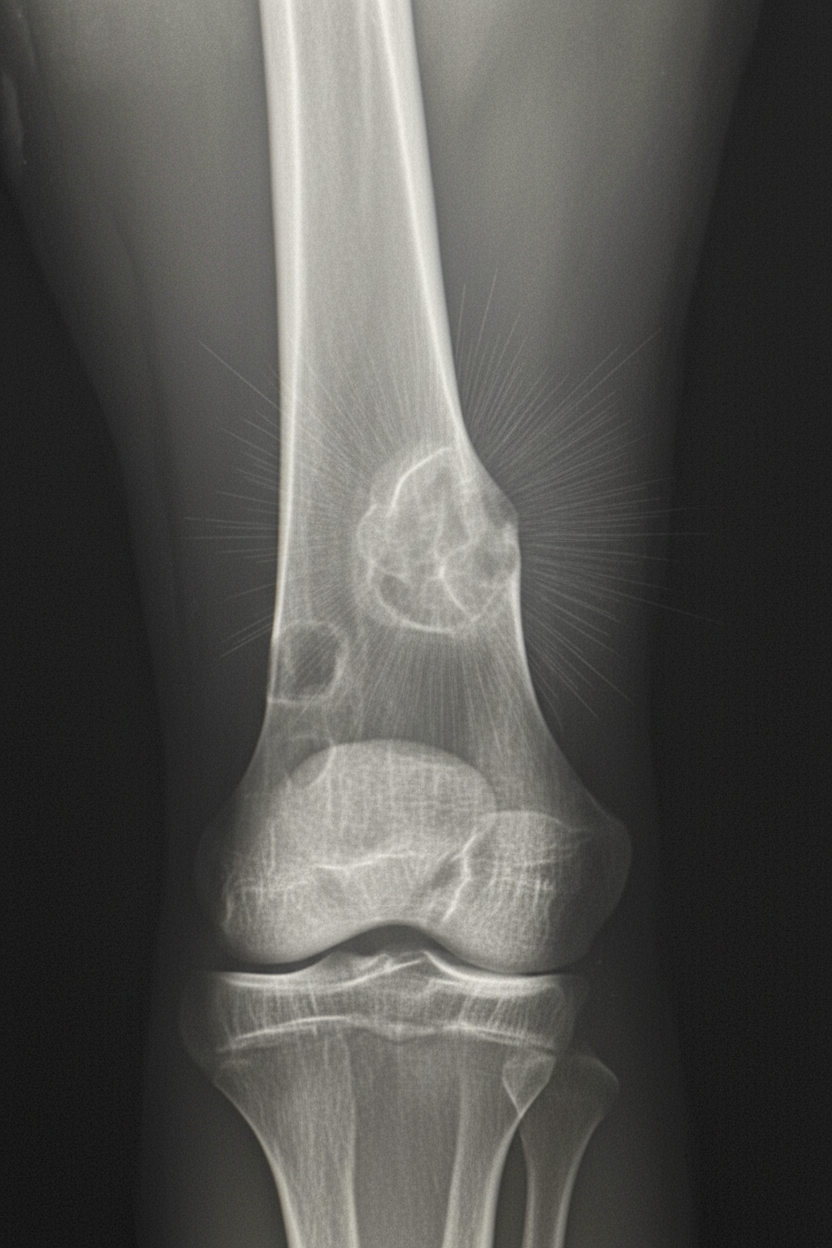
Bone and joint pathology US Medical PG Question 1: A 17-year-old boy is brought to the physician because of progressive right knee pain for the past 3 months. He reports that the pain is worse at night and while doing sports at school. He has not had any trauma to the knee or any previous problems with his joints. His vital signs are within normal limits. Examination of the right knee shows mild swelling and tenderness without warmth or erythema; the range of motion is limited. He walks with an antalgic gait. Laboratory studies show an alkaline phosphatase of 180 U/L and an erythrocyte sedimentation rate of 80 mm/h. An x-ray of the right knee is shown. Which of the following is the most likely diagnosis?
- A. Chordoma
- B. Chondrosarcoma
- C. Osteosarcoma (Correct Answer)
- D. Osteochondroma
- E. Ewing sarcoma
Bone and joint pathology Explanation: ***Osteosarcoma***
- This diagnosis is supported by the **progressive knee pain** worsening at night and with activity, **elevated alkaline phosphatase** and **ESR**, and the X-ray findings typical of an osteosarcoma (e.g., **Codman's triangle**, **sunburst appearance**, or **periosteal elevation**).
- It commonly presents in adolescents, typically in the **metaphysis of long bones** (like the distal femur or proximal tibia), and the presence of mild swelling, tenderness, and limited range of motion align with a rapidly growing bone tumor.
*Chordoma*
- This is a rare, malignant tumor typically arising from notochord remnants, usually seen in the **sacrococcygeal region** or **skull base**, not the knee.
- It usually presents in older adults (30-60 years) and would not have the characteristic X-ray findings seen in this case.
*Chondrosarcoma*
- Characterized by the formation of **cartilage-producing tumors**, typically affecting older adults (40-70 years) and often the **pelvis and proximal long bones**, rather than the knee in an adolescent.
- While it causes pain and swelling, the radiographic features generally show **calcified cartilaginous matrix** (arc and ring pattern) rather than the aggressive periosteal reaction associated with osteosarcoma.
*Osteochondroma*
- This is a **benign cartilaginous tumor** that usually presents as a **painless, solitary mass** near a joint, only causing pain if it irritates surrounding structures or fractures.
- The X-ray image would show a **bony outgrowth covered by cartilage** pointing away from the joint, which is distinctly different from the lytic and blastic changes of an osteosarcoma, and it would not typically cause elevated inflammatory markers.
*Ewing sarcoma*
- While Ewing sarcoma can occur in the knee and presents with pain, swelling, and systemic symptoms, it typically has an **"onion-skin" periosteal reaction** on X-ray, which is distinct from the aggressive sunburst pattern or Codman's triangle seen in osteosarcoma.
- It is more commonly associated with a **diaphyseal location** in long bones and can sometimes show a large soft tissue mass.
Bone and joint pathology US Medical PG Question 2: A 62-year-old man comes to the physician because of a swollen and painful right knee for the last 3 days. He has no history of joint disease. His vital signs are within normal limits. Examination shows erythema and swelling of the right knee, with limited range of motion due to pain. Arthrocentesis of the right knee joint yields 7 mL of cloudy fluid with a leukocyte count of 29,000/mm3 (97% segmented neutrophils). Compensated polarized light microscopy of the aspirate is shown. Which of the following is the most likely underlying mechanism of this patient's knee pain?
- A. Immune complex-mediated cartilage destruction
- B. Calcium pyrophosphate deposition (Correct Answer)
- C. Bacterial infection of the joint
- D. Mechanical stress and trauma
- E. Monosodium urate deposition
Bone and joint pathology Explanation: ***Calcium pyrophosphate deposition***
- The **cloudy fluid** with a leukocyte count of **29,000/mm³** predominantly composed of **segmented neutrophils** indicates acute inflammation, characteristic of **pseudogout** (calcium pyrophosphate dihydrate crystal deposition disease).
- **Compensated polarized light microscopy** would reveal **weakly positive birefringent rhomboid-shaped crystals**, confirming CPPD deposition.
- The **age** of the patient (62 years), **acute monoarticular involvement of the knee**, and sudden onset support a diagnosis of **pseudogout**.
*Immune complex-mediated cartilage destruction*
- This mechanism is characteristic of **rheumatoid arthritis** or **systemic lupus erythematosus**, which present with **chronic polyarticular involvement** and systemic features.
- The acute monoarticular presentation and synovial fluid findings are inconsistent with an immune complex-mediated process.
*Bacterial infection of the joint*
- Septic arthritis typically presents with **synovial fluid WBC counts >50,000/mm³** (often >100,000), though some overlap exists.
- The **absence of fever** and presence of **crystal findings on polarized microscopy** distinguish pseudogout from bacterial infection.
- Septic arthritis would not show crystals on microscopy and would require immediate Gram stain and culture.
*Mechanical stress and trauma*
- While mechanical injury can cause joint effusion, the **high neutrophil count** and **acute inflammatory findings** indicate a crystal-induced or infectious arthropathy rather than traumatic injury.
- There is no history of **trauma** reported, and traumatic effusions typically have lower WBC counts with predominantly red blood cells.
*Monosodium urate deposition*
- This indicates **gout**, which presents with **strongly negative birefringent needle-shaped crystals** on polarized microscopy (not the weakly positive birefringent rhomboid crystals of pseudogout).
- Gout more commonly affects the **first metatarsophalangeal joint** and typically occurs in younger patients with hyperuricemia risk factors.
- The patient's age and knee involvement are more consistent with **pseudogout**.
Bone and joint pathology US Medical PG Question 3: A 15-year-old boy presents to the emergency department for evaluation of an ‘infected leg’. The patient states that his right shin is red, swollen, hot, and very painful. The body temperature is 39.5°C (103.2°F). The patient states there is no history of trauma but states he has a history of poorly managed sickle cell anemia. A magnetic resonance imaging (MRI) scan is performed and confirms a diagnosis of osteomyelitis. Which of the following is the most likely causative agent?
- A. S. aureus
- B. S. pyogenes
- C. N. gonorrhoeae
- D. Salmonella species (Correct Answer)
- E. H. influenzae
Bone and joint pathology Explanation: ***Salmonella species***
- **Salmonella** is the **most common cause of osteomyelitis in patients with sickle cell anemia**, accounting for a majority of cases in this population.
- Patients with sickle cell disease have **functional asplenia** (autosplenectomy), leading to impaired clearance of encapsulated organisms and increased susceptibility to Salmonella bacteremia.
- **Bone infarctions** in sickle cell disease create an avascular nidus that is prone to bacterial seeding, particularly by Salmonella species.
- The clinical presentation of fever, localized bone pain, and MRI confirmation of osteomyelitis in a patient with poorly managed sickle cell anemia is classic for Salmonella osteomyelitis.
*S. aureus*
- *S. aureus* is the most common cause of **osteomyelitis in the general population**, accounting for up to 80% of cases overall.
- While *S. aureus* can also cause osteomyelitis in sickle cell patients, it is **less common than Salmonella** in this specific population.
- Always consider *S. aureus* in osteomyelitis, but the sickle cell history makes Salmonella more likely.
*S. pyogenes*
- *S. pyogenes* (Group A Streptococcus) typically causes skin and soft tissue infections like **cellulitis**, **erysipelas**, and **necrotizing fasciitis**.
- While it can cause osteomyelitis, it is far less common than both *Salmonella* and *S. aureus* in this patient population.
*N. gonorrhoeae*
- *N. gonorrhoeae* can cause disseminated gonococcal infection, which may include **septic arthritis** and tenosynovitis, but osteomyelitis is rare.
- Gonococcal infection is usually associated with sexual activity and typically presents with symptoms of urethritis, cervicitis, or pelvic inflammatory disease, not isolated osteomyelitis.
*H. influenzae*
- Infections with *H. influenzae* type b were previously common in unvaccinated children but are now rare due to widespread **Hib vaccination**.
- While it can cause osteomyelitis, it is typically seen in younger children (under 5 years) and is not the most likely causative agent in this 15-year-old with sickle cell anemia.
Bone and joint pathology US Medical PG Question 4: A 4-year-old boy is brought to the pediatrician by his mother for a routine medical examination. His medical history is relevant for delayed gross motor milestones. The mother is concerned about a growth delay because both of his brothers were twice his size at this age. Physical examination reveals a well-groomed and healthy boy with a prominent forehead and short stature, in addition to shortened upper and lower extremities with a normal vertebral column. The patient’s vitals reveal: temperature 36.5°C (97.6°F); pulse 60/min; and respiratory rate 17/min and a normal intelligence quotient (IQ). A mutation in which of the following genes is the most likely cause underlying the patient’s condition?
- A. Runt-related transcription factor 2
- B. Alpha-1 type I collagen
- C. Fibroblast growth factor receptor 3 (Correct Answer)
- D. Insulin-like growth factor 1 receptor
- E. Fibrillin-1
Bone and joint pathology Explanation: ***Fibroblast growth factor receptor 3***
- The constellation of **short stature**, prominent forehead, and **shortened upper and lower extremities** with a normal vertebral column in a child with normal intelligence is characteristic of **achondroplasia**.
- Achondroplasia is caused by a gain-of-function mutation in the **fibroblast growth factor receptor 3 (FGFR3)** gene, which inhibits chondrocyte proliferation and differentiation, leading to impaired endochondral ossification.
*Runt-related transcription factor 2*
- Mutations in **Runt-related transcription factor 2 (RUNX2)** are associated with **cleidocranial dysplasia**, a condition characterized by absent or hypoplastic clavicles, delayed closure of fontanelles, and dental abnormalities, which are not described in this patient.
- While it affects bone development, the specific features of achondroplasia, such as rhizomelic dwarfism and a prominent forehead, are not typical of RUNX2 mutations.
*Alpha-1 type I collagen*
- Mutations in **collagen genes**, particularly type I collagen (COL1A1, COL1A2), are linked to **osteogenesis imperfecta**, characterized by **fragile bones**, blue sclera, and hearing loss.
- The patient's presentation does not include these features, and the primary issue is disproportionate short stature due to impaired cartilage growth, not bone fragility.
*Insulin-like growth factor 1 receptor*
- Mutations in the **insulin-like growth factor 1 receptor (IGF1R)** can lead to **pre- and postnatal growth retardation** and microcephaly, often associated with developmental delay and feeding difficulties.
- While IGF1R mutations cause short stature, the specific skeletal dysmorphology (e.g., prominent forehead, shortened limbs) and normal intelligence are much more suggestive of achondroplasia.
*Fibrillin-1*
- Mutations in **fibrillin-1** are responsible for **Marfan syndrome**, which typically presents with **tall stature**, long limbs (dolichostenomelia), joint hypermobility, and cardiovascular abnormalities such as aortic root dilation.
- The patient's short stature and shortened limbs directly contradict the clinical picture of Marfan syndrome.
Bone and joint pathology US Medical PG Question 5: A 6-year-old boy with a history of multiple fractures is brought to his pediatrician by his mother, because she is concerned her child cannot hear her. On physical exam, kyphoscoliosis, poor dentition, bowing of long bones, and conductive hearing loss is noted. On genetic analysis, the patient has a COL1A1 gene mutation. The defect found in this patient is most likely associated with impaired formation of which of the following?
- A. Cartilage
- B. Vitreous body of the eye
- C. Lens
- D. Bone (Correct Answer)
- E. Sclera
Bone and joint pathology Explanation: ***Bone***
- This patient has **osteogenesis imperfecta (OI)** due to a **COL1A1 gene mutation** affecting **Type I collagen** synthesis.
- **Bone** is composed primarily of Type I collagen (~90% of the organic matrix), and its formation is **severely impaired** in OI.
- The major clinical manifestations all result from defective bone formation: **multiple fractures**, **kyphoscoliosis**, **bowing of long bones**, and poor bone mineralization.
- The **conductive hearing loss** results from abnormal ossicle development and otosclerosis-like changes in the temporal bone.
- **Poor dentition** is also related to defective Type I collagen in dentin (dentinogenesis imperfecta).
*Sclera*
- While the **sclera** does contain Type I collagen and appears **blue** in OI due to thinning (allowing choroidal vessels to show through), this is a clinical sign rather than the primary site of impaired formation.
- Blue sclera is a diagnostic feature but not the main pathology - it's a visible manifestation of the collagen defect, not the primary tissue with impaired formation.
*Cartilage*
- **Cartilage** is primarily composed of **Type II collagen**, not Type I collagen.
- Defects in Type II collagen cause **chondrodysplasias**, which present differently from this clinical picture.
*Vitreous body of the eye*
- The **vitreous body** is primarily composed of **Type II collagen** and hyaluronic acid.
- It is not primarily affected by Type I collagen defects.
*Lens*
- The **lens** relies primarily on **crystallin proteins** for its structure, not collagen.
- **Lens dislocation** (ectopia lentis) is associated with **Marfan syndrome** (defective fibrillin-1) and **homocystinuria**, not osteogenesis imperfecta.
Bone and joint pathology US Medical PG Question 6: A 67-year-old male presents with left hip pain. Examination reveals mild effusions in both knees, with crepitus in both patellofemoral joints. He states his hearing has worsened recently and that he feels like his hats don't fit anymore. Bone scan reveals diffuse uptake in the calvarium, right proximal femur, and left ilium. Which of the following laboratory abnormalities would be expected in this patient?
- A. Increased serum calcium
- B. Increased serum alkaline phosphatase (Correct Answer)
- C. Decreased serum alkaline phosphatase
- D. Increased serum parathyroid hormone
- E. Decreased serum parathyroid hormone
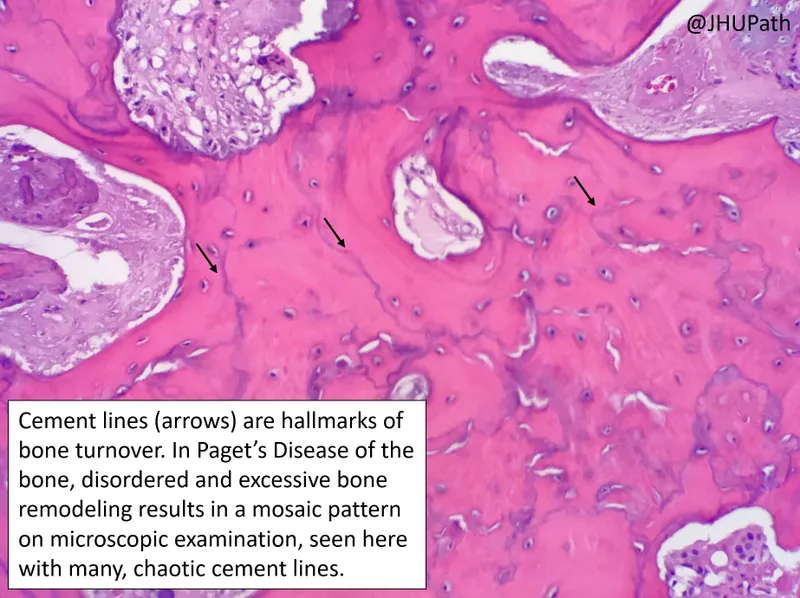
Bone and joint pathology Explanation: ***Increased serum alkaline phosphatase***
- The clinical picture (hip pain, worsened hearing, hats not fitting, diffuse bone uptake on scan) is highly suggestive of **Paget's disease of bone**.
- In Paget's disease, there is increased bone turnover with excessive osteoclastic activity followed by compensatory, disorganized osteoblastic activity, leading to a marked elevation in **serum alkaline phosphatase (ALP)**, a marker of osteoblastic activity.
*Increased serum calcium*
- While bone breakdown occurs in Paget's disease, hypercalcemia is uncommon; it usually only occurs in immobilized patients.
- The bone remodeling is typically balanced, with increased formation countering increased resorption.
*Decreased serum alkaline phosphatase*
- Paget's disease is characterized by significantly *increased* bone turnover and osteoblastic activity, leading to **elevated** rather than decreased serum alkaline phosphatase.
- A decreased ALP level would suggest conditions like hypophosphatasia, not Paget's disease.
*Increased serum parathyroid hormone*
- **Primary hyperparathyroidism** would lead to increased PTH, causing hypercalcemia and bone resorption, but the widespread, disorganized bone changes and localized uptake on a bone scan are more consistent with Paget's disease.
- Increased PTH is not a direct consequence or feature of uncomplicated Paget's disease.
*Decreased serum parathyroid hormone*
- This would typically be seen in states of hypercalcemia not driven by PTH, or in conditions like primary hypoparathyroidism.
- There is no direct mechanism in Paget's disease that would cause decreased PTH levels.
Bone and joint pathology US Medical PG Question 7: A 23-year-old woman comes to the office because of a 2-day history of right knee pain. She says, "I can't run anymore because my knee hurts." The pain is localized "somewhere under the kneecap" and is achy, rated 5/10, but increases to 8/10 with prolonged sitting. She reports an occasional "popping" sound and sensation when she rises from a seated position. She has no history of trauma to the knee. She had a right clavicular fracture 2 years ago that was treated with a shoulder sling. She takes a daily multivitamin and has no known drug allergies. She does not smoke and drinks up to three glasses of wine weekly.
Vital signs: Temperature 37°C (98.6°F), pulse 65/min, respirations 15/min, blood pressure 108/62 mm Hg. Height 173 cm (5 ft 8 in), weight 54 kg (119 lb), BMI 18 kg/m².
Physical examination shows no acute distress. Pulmonary examination shows lungs clear to auscultation. Cardiac examination shows regular rate and rhythm with normal S1 and S2; no murmurs, rubs, or gallops. The abdomen is thin with no tenderness, guarding, masses, bruits, or hepatosplenomegaly. Extremities show no joint erythema, edema, or warmth; dorsalis pedis, radial, and femoral pulses are intact. Musculoskeletal examination shows diffuse tenderness to palpation over the right anterior knee, worse with full extension of the knee; no associated effusion or erythema; full, symmetric strength of quadriceps, hip abductors, and hip external rotators; crepitus with knee range of motion; and antalgic gait. Neurologic examination shows the patient is alert and oriented with cranial nerves grossly intact and no focal neurologic deficits.
Which of the following is the most appropriate next step in management?
- A. Physical therapy (Correct Answer)
- B. Pain control and rest
- C. Synovial fluid analysis
- D. Intraarticular steroid injection
- E. Arthroscopy of the knee
Bone and joint pathology Explanation: ***Physical therapy***
- This patient presents with symptoms highly suggestive of **patellofemoral pain syndrome (PFPS)**, including anterior knee pain, pain worse with prolonged sitting and activity, and crepitus. **Physical therapy** focusing on quadriceps strengthening, hip abductor strengthening, and core stability is the cornerstone of PFPS management.
- PFPS is often related to **biomechanical imbalances** and muscle weakness (e.g., weak vastus medialis obliquus or hip abductors), which can be effectively addressed through a structured physical therapy program.
*Pain control and rest*
- While **rest** can temporarily alleviate symptoms, it does not address the underlying biomechanical issues contributing to PFPS and can lead to **deconditioning**, potentially worsening the condition in the long term.
- **Pain control**, often with NSAIDs, can be used adjunctively, but it is not the primary or sole management strategy for PFPS as it also does not address the root cause.
*Synovial fluid analysis*
- **Synovial fluid analysis** is indicated for suspected inflammatory or infectious arthritis, which is not suggested by this patient's presentation of an atraumatic, "achy" pain without signs of inflammation (e.g., warmth, effusion, erythema).
- The patient's symptoms are more consistent with a **mechanical issue** rather than an intra-articular pathology requiring fluid analysis.
*Intraarticular steroid injection*
- **Intraarticular steroid injections** are generally not recommended for PFPS as the condition is typically not inflammatory within the joint space itself, but rather an issue of patellar tracking or soft tissue irritation.
- Steroid injections carry risks and provide only **temporary symptom relief** for inflammatory conditions, and their efficacy in PFPS is limited.
*Arthroscopy of the knee*
- **Arthroscopy** is an invasive surgical procedure and is typically reserved for cases where conservative management has failed, or when there is suspicion of a specific intra-articular lesion like a meniscal tear or loose body, which are not indicated here.
- This patient's symptoms are classic for PFPS, which is a **non-surgical condition** in the first line of management.
Bone and joint pathology US Medical PG Question 8: A 54-year-old female presents to her primary care physician with complaints of fatigue, constipation, and what the patient describes as "aching in her bones." Her medical history is significant for hypertension, well-controlled on lisinopril, and two prior kidney stones that both passed spontaneously without need for surgery. Vital signs are within normal limits, and physical exam is not significant for any notable findings. Preliminary lab work is ordered and reveals: calcium 11.6 mg/dL (normal range 8.5 - 10.9 mg/dL), phosphorus 2.1 mg/dL (normal range 2.4 - 4.1 mg/dL), and an elevated parathyroid hormone (PTH) level. Which of the following findings would most likely be expected on radiographic evaluation of this patient's hands?
- A. Osteoid matrix accumulation around bony trabeculae
- B. Joint space narrowing at the proximal and distal interphalangeal joints
- C. Subperiosteal cortical thinning (Correct Answer)
- D. Dense bone filling the medullary cavity of the phalanges and metacarpals
- E. Ulnar deviation of the metacarpophalangeal joints
Bone and joint pathology Explanation: ***Subperiosteal cortical thinning***
- The patient's symptoms (fatigue, constipation, bone pain) combined with **hypercalcemia**, **hypophosphatemia**, and **elevated PTH** are highly indicative of **primary hyperparathyroidism**.
- **Subperiosteal cortical resorption**, leading to cortical thinning, is a **classic radiographic finding** in hyperparathyroidism, often seen in the phalanges.
*Osteoid matrix accumulation around bony trabeculae*
- This description is more consistent with **osteomalacia** or **rickets**, where there is impaired mineralization of osteoid.
- While osteomalacia can cause bone pain and weakness, the lab findings of **hypercalcemia and hypophosphatemia** with **elevated PTH** are characteristic of hyperparathyroidism, not osteomalacia.
*Joint space narrowing at the proximal and distal interphalangeal joints*
- **Joint space narrowing** is a common radiographic feature of **osteoarthritis** or inflammatory arthropathies like **rheumatoid arthritis** or **psoriatic arthritis**.
- These conditions do not present with the specific metabolic abnormalities (hypercalcemia, hypophosphatemia, elevated PTH) described in the patient.
*Dense bone filling the medullary cavity of the phalanges and metacarpals*
- **Dense bone** (osteosclerosis) filling the medullary cavity, often described as a "bone within a bone" appearance, can be seen in conditions like **osteopetrosis** or **myelofibrosis**.
- This is not a typical finding in hyperparathyroidism, which is characterized by bone resorption rather than increased bone density.
*Ulnar deviation of the metacarpophalangeal joints*
- **Ulnar deviation** is a hallmark sign of advanced **rheumatoid arthritis**, indicating chronic inflammation and joint destruction.
- The patient's symptoms and lab findings are not consistent with an inflammatory arthropathy like rheumatoid arthritis.
Bone and joint pathology US Medical PG Question 9: A 38-year-old woman was brought to the emergency department after she experienced dizziness and shortness of breath while walking with her friend. She recently immigrated to the United States and is unable to report her previous medical history. Physical exam reveals pallor underneath her eyelids. Labs are obtained with the following results:
Hemoglobin: 8.4 g/dL
Platelet count: 62,000/mm^3
Mean corpuscular volume: 89 µm^3
Reticulocyte count: 0.1%
Lactate dehydrogenase: 175 U/L
Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Living in an old house
- B. Recent infection with a toxin producing gram-negative rod
- C. Vegan diet
- D. Chronic alcohol abuse
- E. Administration of a 50S ribosomal inhibitor (Correct Answer)
Bone and joint pathology Explanation: ***Administration of a 50S ribosomal inhibitor***
- The patient's symptoms (dizziness, shortness of breath, pallor) and lab results (anemia, thrombocytopenia, normal MCV, very low reticulocyte count) are highly suggestive of **aplastic anemia**.
- Aplastic anemia is often caused by exposure to toxins or medications; **chloramphenicol**, a 50S ribosomal inhibitor, is a classic cause of dose-independent, idiosyncratic aplastic anemia.
*Living in an old house*
- Living in an old house is associated with **lead poisoning**, which typically causes a **microcytic anemia** with **basophilic stippling**, not normocytic anemia with thrombocytopenia and low reticulocytes.
- Lead poisoning does not typically cause severe thrombocytopenia as seen in this patient.
*Recent infection with a toxin producing gram-negative rod*
- This scenario would suggest **hemolytic uremic syndrome (HUS)**, which presents with microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.
- The patient's **normal LDH** and **low reticulocyte count** argue against hemolysis as the primary cause of anemia.
*Vegan diet*
- A vegan diet can lead to **vitamin B12 deficiency**, which causes **macrocytic anemia**, often with pancytopenia.
- This patient has a **normal MCV (89 µm^3)**, ruling out macrocytic anemia.
*Chronic alcohol abuse*
- Chronic alcohol abuse can cause **folate deficiency** leading to **macrocytic anemia** and **thrombocytopenia**.
- The patient's **normal MCV** makes macrocytic anemia due to folate deficiency unlikely.
Bone and joint pathology US Medical PG Question 10: A previously healthy 59-year-old man comes to the physician with a 6-month history of worsening headaches, difficulty chewing, and progressive hearing loss. Examination shows a mildly tender, 1-cm, hard swelling over the left maxilla. The remainder of the examination shows no abnormalities. Serum studies show a calcium concentration of 8.5 mg/dL, alkaline phosphatase activity of 112 U/L, and parathyroid hormone concentration of 310 pg/mL. Audiometry shows bilateral mixed conductive and sensorineural hearing loss. Which of the following processes is the most likely cause of this patient's condition?
- A. Defective synthesis of dynein
- B. Decreased activity of carbonic anhydrase II
- C. Decreased expression of menin protein
- D. Increased activity of nuclear factor-κB (Correct Answer)
- E. Defective synthesis of type I collagen
Bone and joint pathology Explanation: ***Increased activity of nuclear factor-κB***
- The patient's symptoms (worsening headaches, difficulty chewing, hearing loss, localized bony swelling) and laboratory findings (elevated alkaline phosphatase, normal calcium, elevated PTH) are highly suggestive of **Paget's disease of bone** (osteitis deformans).
- **Paget's disease** is characterized by focal areas of increased bone turnover, involving both excessive bone resorption by osteoclasts and disorganized bone formation by osteoblasts, often linked to increased **NF-κB activity** in osteoclasts.
*Defective synthesis of dynein*
- **Dynein defects** are associated with conditions like primary ciliary dyskinesia, which presents with chronic sinopulmonary infections and situs inversus.
- This condition does not explain the patient's bone remodeling issues or localized bony swelling.
*Decreased activity of carbonic anhydrase II*
- **Carbonic anhydrase II deficiency** causes osteopetrosis (marble bone disease), a condition characterized by abnormally dense bones due to impaired osteoclast function.
- This would typically lead to symptoms like bone fractures, cranial nerve compression, and pancytopenia, which are distinct from the presented case.
*Decreased expression of menin protein*
- **Menin protein deficiency**, due to mutations in the *MEN1* gene, is associated with Multiple Endocrine Neoplasia type 1 (MEN1), involving tumors of the parathyroid, pituitary, and pancreas.
- While the patient has elevated PTH, the primary features of bone remodeling and localized swelling point away from MEN1 as the primary diagnosis.
*Defective synthesis of type I collagen*
- **Defective type I collagen synthesis** is characteristic of osteogenesis imperfecta, leading to brittle bones, frequent fractures, and blue sclera.
- This is a generalized skeletal disorder with a genetic basis, typically presenting earlier in life, and does not align with the patient's localized bone overgrowth and increased osteoclast activity.
More Bone and joint pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.