Tubulointerstitial diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tubulointerstitial diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Tubulointerstitial diseases US Medical PG Question 1: An 8-year-old boy is brought to the physician by his parents because of fever for 3 days. During the period, he has had fatigue, severe burning with urination, and increased urination. The mother reports that his urine has red streaks and a “strange” odor. He has taken acetaminophen twice a day for the past two days with no improvement in his symptoms. He has had multiple ear infections in the past but has been healthy in the past year. His immunizations are up-to-date. He appears uncomfortable. His temperature is 39°C (102.2°F). Examination shows right-sided costovertebral angle tenderness. Laboratory studies show a leukocyte count of 16,000/cm3 and an erythrocyte sedimentation rate of 40 mm/hr. Urine dipstick shows leukocyte esterase and nitrites. Urinalysis shows:
Blood 2+
Protein 2+
WBC 24/hpf
RBC 50/hpf
RBC casts none
WBC casts numerous
Granular casts none
Urine cultures are sent to the laboratory. Damage to which of the following structures is the most likely cause of this patient's hematuria?
- A. Renal tubules
- B. Urethral epithelium
- C. Mucosa of the bladder
- D. Renal papilla
- E. Renal interstitium (Correct Answer)
Tubulointerstitial diseases Explanation: ***Renal interstitium***
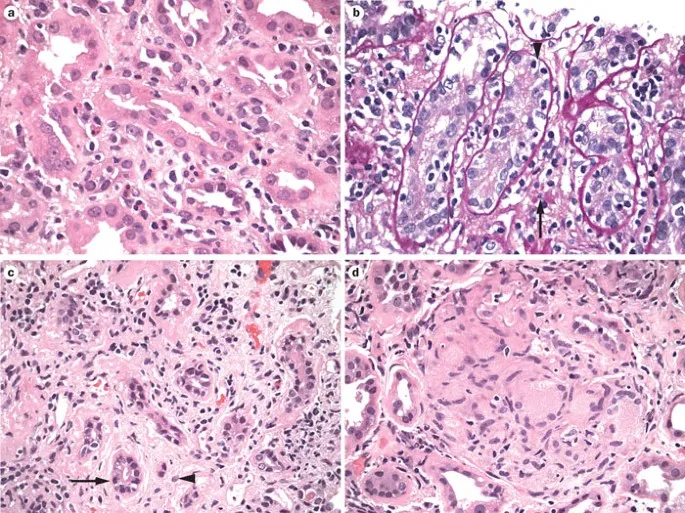
- This patient has **acute pyelonephritis**, indicated by fever, **costovertebral angle tenderness**, elevated inflammatory markers (WBC 16,000, ESR 40), positive leukocyte esterase and nitrites, and most importantly, **WBC casts** in the urine.
- Acute pyelonephritis is characterized by **bacterial infection of the renal parenchyma**, primarily affecting the **renal interstitium** (the tissue between tubules containing blood vessels, inflammatory cells, and connective tissue).
- The **hematuria** (RBC 50/hpf, Blood 2+) results from **inflammatory damage to interstitial capillaries** and disruption of the normal tissue architecture due to bacterial invasion and immune response.
- **WBC casts** form when WBCs from the inflamed interstitium enter the tubular lumen and aggregate with Tamm-Horsfall protein, confirming upper urinary tract (kidney) infection rather than simple cystitis.
*Renal papilla*
- **Papillary necrosis** can cause severe hematuria but typically occurs in specific settings: diabetes mellitus, sickle cell disease, chronic analgesic abuse (NSAIDs), or severe obstruction—none of which are present in this otherwise healthy child.
- While severe pyelonephritis can rarely lead to papillary necrosis, the clinical presentation here is consistent with **uncomplicated acute pyelonephritis** where interstitial inflammation is the primary pathology.
*Renal tubules*
- **Acute tubular necrosis (ATN)** presents with acute kidney injury, elevated creatinine, and **muddy brown granular casts**, which are not seen here.
- While tubular cells may be affected secondarily in pyelonephritis, the primary site of damage is the **interstitium**, not the tubules themselves.
*Urethral epithelium*
- **Urethritis** causes dysuria and urethral discharge but does not produce **fever**, **CVA tenderness**, or **WBC casts**, which indicate kidney involvement.
- Urethral inflammation would not explain the systemic inflammatory response or the casts originating from the kidney.
*Mucosa of the bladder*
- **Cystitis** (bladder infection) causes dysuria, frequency, and urgency, but typically lacks **high fever** and **CVA tenderness**, which are hallmarks of kidney infection.
- While cystitis can cause hematuria, the presence of **WBC casts** definitively localizes the infection to the kidney (renal parenchyma/interstitium), not the bladder.
Tubulointerstitial diseases US Medical PG Question 2: A 62-year-old man presents to the emergency room with an acute myocardial infarction. Twenty-four hours after admission to the cardiac intensive care unit, he develops oliguria. Laboratory tests show that his serum BUN is 59 mg/dL and his serum creatinine is 6.2 mg/dL. Renal biopsy reveals necrosis of the proximal tubules and thick ascending limb of Henle's loop. Which of the following would you most likely observe on a microscopic examination of this patient's urine?
- A. White blood cell casts
- B. Broad waxy casts
- C. Fatty casts
- D. Hyaline casts
- E. Muddy brown casts (Correct Answer)
Tubulointerstitial diseases Explanation: ***Muddy brown casts***
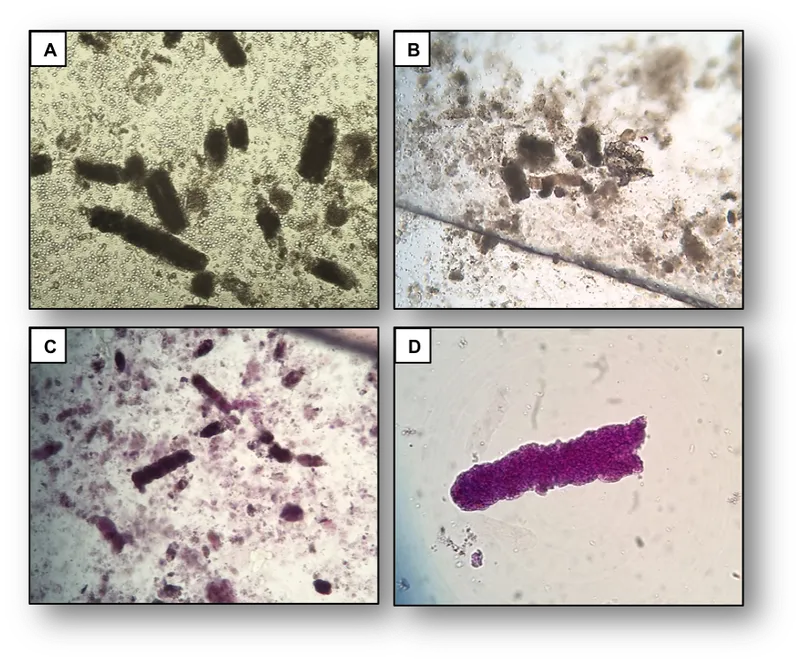
- The patient's presentation of **acute myocardial infarction** followed by **oliguria**, elevated **BUN** and **creatinine**, and necrosis of the **proximal tubules** and **thick ascending limb** of Henle's loop is characteristic of **acute tubular necrosis (ATN)**.
- **Muddy brown casts** composed of **granular material** and **renal tubular epithelial cells** are the classic finding in the urine sediment of patients with ATN.
*White blood cell casts*
- **White blood cell casts** are typically associated with **pyelonephritis** or **interstitial nephritis**, indicating renal inflammation or infection.
- While infection can exacerbate kidney injury, the primary pathology described here is **ischemic ATN**, not an infectious process.
*Broad waxy casts*
- **Broad waxy casts** indicate severe, **chronic kidney disease** with significant **tubular dilation** and **stasis**, often end-stage renal disease.
- The patient's clinical picture depicts **acute kidney injury**, not chronic kidney failure.
*Fatty casts*
- **Fatty casts** are characteristic of **nephrotic syndrome**, which involves significant proteinuria and hyperlipidemia.
- This patient's presentation does not describe the features of **nephrotic syndrome**, such as **massive proteinuria** or **edema**.
*Hyaline casts*
- **Hyaline casts** are composed of **Tamm-Horsfall protein** and can be found in healthy individuals, especially after exercise or dehydration.
- While they can be present in various kidney conditions, they are **non-specific** and not indicative of the specific **tubular epithelial cell injury** seen in ATN.
Tubulointerstitial diseases US Medical PG Question 3: A 53-year-old woman presents to the emergency room with severe chest pain radiating to the back. She was diagnosed with acute aortic dissection. A few hours into the resuscitation, she was having oliguria. Laboratory findings show a serum creatinine level of 5.3 mg/dL. Which of the following casts are most likely to be seen on urinalysis?
- A. RBC casts
- B. Fatty casts
- C. Muddy brown casts (Correct Answer)
- D. Waxy casts
- E. Hyaline casts
Tubulointerstitial diseases Explanation: ***Muddy brown casts***
- **Acute tubular necrosis (ATN)**, likely caused by **renal hypoperfusion** in the context of an aortic dissection, is characterized by the presence of **muddy brown granular casts** in urinalysis. The significantly elevated **creatinine (5.3 mg/dL)** and **oliguria** support a diagnosis of acute kidney injury with ATN.
- These casts are pathognomonic for ATN and are formed from shed **epithelial cells** and debris accumulating in the renal tubules.
*RBC casts*
- **Red blood cell (RBC) casts** are indicative of **glomerulonephritis** or other causes of **glomerular injury**, which are not directly suggested by the presentation of aortic dissection and subsequent oliguria.
- While hematuria can occur in various renal conditions, the presence of **RBC casts** points to bleeding originating from the glomerulus, which is a different pathology than ATN.
*Fatty casts*
- **Fatty casts** are typically associated with **nephrotic syndrome**, a condition characterized by significant proteinuria, hypoalbuminemia, and edema.
- There is no clinical information to suggest nephrotic syndrome in this patient, whose acute renal failure is likely due to hypoperfusion.
*Waxy casts*
- **Waxy casts** are generally indicative of **chronic kidney disease** and highly advanced, severe tubular damage, representing a later stage of kidney injury.
- While the patient has acute kidney injury, the timeline and acute nature of the insult make muddy brown casts more likely than waxy casts.
*Hyaline casts*
- **Hyaline casts** are composed primarily of Tamm-Horsfall mucoprotein, a normal protein secreted by renal tubule cells.
- These casts can be seen in normal urine, especially after exercise or dehydration, and are not specific for any particular kidney pathology or acute kidney injury.
Tubulointerstitial diseases US Medical PG Question 4: A 33-year-old female presents with recent onset of painful urination, fever, and right flank pain. Urinary sediment analysis is positive for the presence of white blood cell casts and Gram-negative bacteria. She has not recently started any new medications. What is the most likely diagnosis in this patient?
- A. Appendicitis
- B. Cystitis
- C. Pyelonephritis (Correct Answer)
- D. Acute Interstitial Nephritis
- E. Pelvic Inflammatory Disease
Tubulointerstitial diseases Explanation: ***Pyelonephritis***
- The combination of **painful urination**, **fever**, **right flank pain**, and **white blood cell casts** in the urine is highly indicative of pyelonephritis, an infection of the renal parenchyma.
- **White blood cell casts** are pathognomonic for inflammation within the renal tubules and are a key differentiating feature that points to an upper urinary tract infection.
*Appendicitis*
- While appendicitis can cause **right-sided abdominal pain** and **fever**, it typically does not present with painful urination or urinary sediment abnormalities like white blood cell casts.
- The pain is usually localized to the **right lower quadrant** and often migrates, which is not characteristic of flank pain.
*Cystitis*
- Cystitis involves bladder inflammation and causes **painful urination**, **frequency**, and **urgency**, but typically does not cause **fever** or **flank pain**, and **white blood cell casts** are absent.
- It is an infection limited to the **lower urinary tract**, without renal parenchymal involvement.
*Acute Interstitial Nephritis*
- This condition is often associated with a **drug hypersensitivity reaction**, causing inflammation in the renal interstitium, but typically presents with **eosinophilia**, rash, and renal failure, not usually with white blood cell casts directly from infection.
- While it can cause renal dysfunction and sometimes fever, the presence of **Gram-negative bacteria** and **WBC casts** strongly points to an infection rather than an allergic reaction.
*Pelvic Inflammatory Disease*
- PID causes **lower abdominal pain**, **fever**, and sometimes painful urination if there's concurrent urethritis, but it is not associated with **flank pain** or **white blood cell casts** in the urine.
- It is an infection of the **female reproductive organs**, often caused by sexually transmitted organisms, and would typically present with cervical motion tenderness.
Tubulointerstitial diseases US Medical PG Question 5: Ten days after being discharged from the hospital, a 42-year-old man comes to the emergency department because of reduced urine output for 3 days. Physical examination is normal. Serum creatinine concentration is 2.9 mg/dL. Urinalysis shows brownish granular casts and 2+ proteinuria. Renal biopsy shows patchy necrosis of the proximal convoluted tubule with sloughing of tubular cells into the lumen and preservation of tubular basement membranes. Administration of which of the following drugs during this patient's hospitalization is most likely the cause of the observed decrease in renal function?
- A. Aspirin
- B. Acyclovir
- C. Omeprazole
- D. Captopril
- E. Gentamicin (Correct Answer)
Tubulointerstitial diseases Explanation: ***Gentamicin***
- The patient's presentation with **acute kidney injury** (reduced urine output, elevated creatinine) and characteristic urinalysis findings (**brownish granular casts**, proteinuria) points to **acute tubular necrosis (ATN)**.
- **Gentamicin** is an **aminoglycoside antibiotic** well-known for causing ATN, particularly with prolonged use or in susceptible patients. The biopsy findings of **patchy necrosis of the proximal convoluted tubule** and **sloughing of tubular cells** with preserved basement membranes are classic for ATN.
*Aspirin*
- **Aspirin**, especially at high doses or in sensitive individuals, can cause **analgesic nephropathy** (chronic interstitial nephritis) or, less commonly, acute interstitial nephritis.
- It does not typically cause ATN with the specific biopsy findings described, and its primary renal toxicity is often related to **prostaglandin inhibition**.
*Acyclovir*
- **Acyclovir** can cause acute kidney injury, but it primarily does so through **crystalluria** and **tubular obstruction**, leading to acute interstitial nephritis or acute kidney injury due to crystal deposition.
- The biopsy findings described (patchy tubular necrosis, sloughing cells) are not typical for acyclovir-induced nephrotoxicity.
*Omeprazole*
- **Omeprazole**, a proton pump inhibitor, is most commonly associated with **acute interstitial nephritis (AIN)**, an allergic reaction affecting the renal interstitium.
- AIN would typically present with eosinophiluria, white blood cell casts, and interstitial inflammation on biopsy, rather than primary tubular necrosis.
*Captopril*
- **Captopril**, an ACE inhibitor, can cause acute kidney injury, particularly in patients with **renal artery stenosis** or volume depletion, by altering glomerular hemodynamics.
- It typically does not cause direct tubular necrosis or the specific histological changes seen in ATN; rather, it primarily reduces **glomerular filtration pressure**.
Tubulointerstitial diseases US Medical PG Question 6: A 53-year-old woman presents with a severe headache, nausea, and vomiting for the past 48 hours. Vitals show a blood pressure of 220/134 mm Hg and a pulse of 88/min. Urinalysis shows a 2+ proteinuria and RBC casts. Which of the following renal lesions is most likely to be seen in this patient?
- A. Papillary necrosis
- B. Fibrinoid necrosis (Correct Answer)
- C. Acute tubular necrosis (ATN)
- D. Acute pyelonephritis
- E. Acute interstitial nephritis (AIN)
Tubulointerstitial diseases Explanation: ***Fibrinoid necrosis***
- The patient's presentation with **severe hypertension** (220/134 mm Hg), **proteinuria**, and **RBC casts** is highly suggestive of a **hypertensive crisis with malignant nephrosclerosis**.
- **Fibrinoid necrosis** refers to the accumulation of **fibrin-like material** in the walls of arterioles, a characteristic pathological finding in **malignant hypertension** leading to vascular damage in the kidney.
*Papillary necrosis*
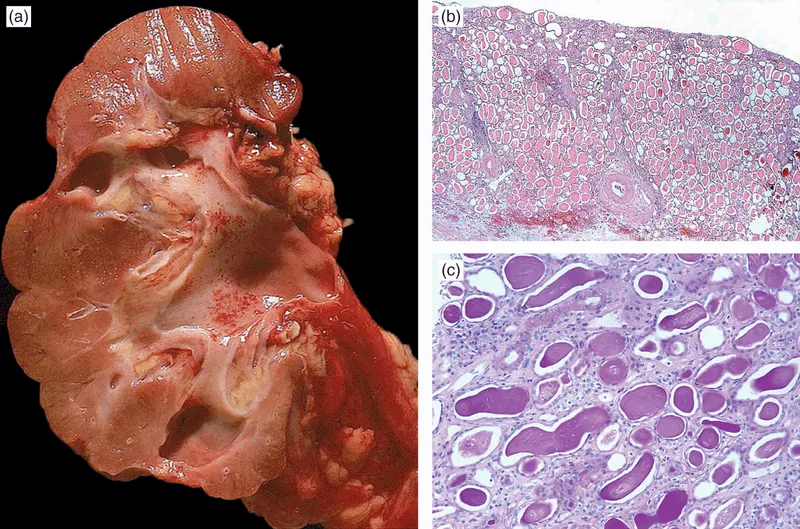
- This condition is typically associated with **analgesic nephropathy**, **diabetes mellitus**, and **urinary tract obstruction** or **sickle cell disease**.
- While it can cause renal dysfunction, it does not directly explain the acute severe hypertension and RBC casts unique to hypertensive emergencies.
*Acute tubular necrosis (ATN)*
- While ATN can cause **acute kidney injury**, it is usually characterized by **muddy brown casts** and is often precipitated by **ischemic** or **nephrotoxic insults**.
- The prominent hypertension and RBC casts point away from primary ATN in this context.
*Acute pyelonephritis*
- Acute pyelonephritis is an **infection of the kidney** characterized by **fever**, **flank pain**, and **pyuria** (white blood cells in urine), usually not severe hypertension and RBC casts.
- The main findings in this patient are related to vascular damage, not infection.
*Acute interstitial nephritis (AIN)*
- AIN is often caused by **drug reactions** or systemic diseases, presenting with **fever**, **rash**, **eosinophilia**, and **white blood cell casts**.
- The clinical picture of severe hypertension and RBC casts is not typical for AIN.
Tubulointerstitial diseases US Medical PG Question 7: A 56-year-old African-American man comes to the physician for intermittent episodes of dark urine and mild flank pain. The patient has had 3 episodes of frank reddish discoloration of his urine within 1 month. He has chronic headaches and back pain for which he has been taking aspirin and ibuprofen daily for 1 year. The patient has sickle cell trait. He has smoked a pack of cigarettes daily for 10 years. He appears well. His temperature is 37.4°C (99.3°F). His pulse is 66/min, and his blood pressure is 150/90 mm Hg. Physical exam shows mild, bilateral flank tenderness. Laboratory analysis shows a serum creatinine concentration of 2.4 mg/dL. Urine studies are shown below.
Urine
Blood 3+
Protein 2+
RBC > 10/hpf
WBC 3/hpf
Which of the following is the most likely underlying cause of this patient's hematuria?
- A. Direct nephrotoxic injury
- B. Purulent renal inflammation
- C. Renal reperfusion injury
- D. Chronic hemoglobin filtration
- E. Renal papillary ischemia (Correct Answer)
Tubulointerstitial diseases Explanation: ***Renal papillary ischemia***
- The patient's **sickle cell trait** predisposes him to episodes of renal papillary ischemia, which can lead to **papillary necrosis** and subsequent gross hematuria and flank pain.
- The use of **NSAIDs (aspirin and ibuprofen)** chronically can also contribute to renal papillary necrosis, exacerbating the risk in a patient with sickle cell trait.
*Direct nephrotoxic injury*
- While chronic NSAID use can cause **nephrotoxic injury**, it typically manifests as interstitial nephritis or acute kidney injury, not primarily recurrent gross hematuria.
- The level of proteinuria (2+) and absence of specific casts associated with direct toxic tubular injury make this less likely as the primary cause of hematuria.
*Purulent renal inflammation*
- This would typically present with symptoms of **urinary tract infection** (e.g., dysuria, fever), significant pyuria (WBCs > 10/hpf), and potentially bacterial casts, which are not seen here.
- The urinalysis shows only 3 WBCs/hpf, making a purulent infection unlikely.
*Renal reperfusion injury*
- This type of injury occurs after a period of **ischemia followed by restoration of blood flow**, often in the context of surgery, trauma, or organ transplantation.
- There is no history in the patient suggestive of an event that would lead to renal reperfusion injury.
*Chronic hemoglobin filtration*
- While sickle cell trait involves abnormal hemoglobin, **chronic hemoglobin filtration** itself does not typically cause the discreet episodes of gross hematuria and flank pain described.
- Hemoglobinuria without red blood cells in the urine is characteristic of chronic intravascular hemolysis, which is not indicated by the RBCs > 10/hpf.
Tubulointerstitial diseases US Medical PG Question 8: A 71-year-old, hospitalized man develops abnormal laboratory studies 4 days after starting treatment for exacerbation of congestive heart failure. He also has a history of osteoarthritis and benign prostatic hyperplasia. He recently completed a course of amikacin for bacterial prostatitis. Before hospitalization, his medications included simvastatin and ibuprofen. Blood pressure is 111/76 mm Hg. Serum studies show a creatinine of 2.3 mg/dL (previously normal) and a BUN of 48 mg/dL. Urinalysis shows a urine osmolality of 600 mOsm/kg and urine sodium of 10 mEq/L. Which of the following is the most likely explanation for this patient's renal insufficiency?
- A. Volume depletion (Correct Answer)
- B. Antibiotic use
- C. Glomerulonephritis
- D. Urinary tract infection
- E. Bladder outlet obstruction
Tubulointerstitial diseases Explanation: ***Volume depletion***
- The patient's presentation with **elevated BUN** and **creatinine**, along with **high urine osmolality** (600 mOsm/kg) and **low urine sodium** (10 mEq/L), are classic signs of **prerenal azotemia**, indicating effective circulating volume depletion.
- The patient has **congestive heart failure exacerbation**, which is often treated with **diuretics**, and a history of **ibuprofen** use, both of which can contribute to volume depletion and impaired renal perfusion.
*Antibiotic use*
- While **amikacin** is nephrotoxic, the urinalysis findings (**high urine osmolality**, **low urine sodium**) are not typical of established acute kidney injury (e.g., acute tubular necrosis) caused by aminoglycosides, which generally cause an inability to concentrate urine and higher urine sodium due to tubular damage.
- The timing of the renal insufficiency, occurring 4 days after starting CHF treatment and after completing amikacin, points away from amikacin as the primary, immediate cause.
*Glomerulonephritis*
- **Glomerulonephritis** typically presents with active urine sediment (e.g., **red blood cell casts**, **proteinuria**), which is not mentioned here.
- The urine osmolality and sodium values are not characteristic of glomerulonephritis, which is a cause of intrinsic renal disease.
*Urinary tract infection*
- A **urinary tract infection (UTI)** primarily causes symptoms like dysuria, frequency, and urgency, and can lead to pyelonephritis with fever and flank pain.
- While UTIs can worsen renal function, they do not directly explain the specific laboratory findings of **prerenal azotemia**.
*Bladder outlet obstruction*
- **Bladder outlet obstruction** (due to **benign prostatic hyperplasia** in this patient) causes **postrenal azotemia**, which would typically manifest with **bilateral hydronephrosis** on imaging and often leads to an inability to concentrate urine effectively over time, with less dramatic changes in urine sodium initially.
- The given urine osmolality and sodium values are very suggestive of prerenal causes, not obstruction.
Tubulointerstitial diseases US Medical PG Question 9: A 53-year-old woman presents to her physician for evaluation of sudden onset respiratory distress for the past few hours. The past medical history includes a myocardial infarction 2 years ago. The vital signs include a blood pressure 70/40 mm Hg, pulse 92/min, respiratory rate 28/min, and SpO2 92% on room air. The physical examination reveals bilateral basal crepitations on auscultation. The echocardiogram reveals an ejection fraction of 34%. She is admitted to the medical floor and started on furosemide. The urine output in 24 hours is 400 mL. The blood urea nitrogen is 45 mg/dL and the serum creatinine is 1.85 mg/dL. The fractional excretion of sodium is 2.4%. Urinalysis revealed muddy brown granular casts. Which of the following is the most likely cause of the abnormal urinalysis?
- A. Acute interstitial nephritis
- B. Acute tubular necrosis (Correct Answer)
- C. Acute pyelonephritis
- D. Chronic kidney disease
- E. Acute glomerulonephritis
Tubulointerstitial diseases Explanation: ***Acute tubular necrosis***
- The presence of **muddy brown granular casts** on urinalysis is pathognomonic for **acute tubular necrosis (ATN)**, indicating damage to the renal tubules.
- The patient's history of **cardiogenic shock** (low BP 70/40 mm Hg, respiratory distress, low SpO2, low ejection fraction of 34%) led to **renal hypoperfusion** and ischemic tubular injury.
- The **fractional excretion of sodium (FENa) of 2.4%** (>2%) is characteristic of **intrinsic renal injury** (ATN), as damaged tubules cannot effectively reabsorb sodium.
- **Oliguria** (400 mL/24 hours), elevated **BUN (45 mg/dL)** and **creatinine (1.85 mg/dL)** further support acute kidney injury from ATN.
*Acute interstitial nephritis*
- This condition is typically associated with **drug hypersensitivity** (e.g., NSAIDs, antibiotics, PPIs) or **infections** and is characterized by inflammatory infiltrate in the renal interstitium.
- Urinalysis typically shows **white blood cell casts** and **eosinophiluria**, not muddy brown granular casts.
*Acute pyelonephritis*
- This is an **infection of the kidney** parenchyma, usually caused by bacterial ascension from the urinary tract.
- Symptoms often include **fever, flank pain, dysuria**, and urinalysis reveals **leukocyturia** (white blood cells) and **bacterial casts**, not muddy brown granular casts.
*Chronic kidney disease*
- While the patient has elevated creatinine and BUN, **chronic kidney disease (CKD)** develops over months to years and is characterized by persistent kidney damage or decreased function.
- Urinalysis in CKD often shows **broad waxy casts** and typically does not present with such **acute, sudden onset** of severe renal dysfunction with muddy brown granular casts.
*Acute glomerulonephritis*
- This condition involves inflammation of the glomeruli and typically presents with **hematuria, proteinuria, and red blood cell casts** (dysmorphic RBCs).
- The patient's clinical picture, including the absence of significant hematuria and the presence of **muddy brown granular casts**, does not fit acute glomerulonephritis.
Tubulointerstitial diseases US Medical PG Question 10: A 25-year-old woman, gravida 2, para 1, is brought to the emergency department at 39 weeks' gestation in active labor. Her first child was delivered at 40 weeks' gestation by elective cesarean section due to limited range of motion in her hip. The patient has sickle cell disease. She has had multiple episodes of acute chest syndrome and has required several transfusions in the past. An uncomplicated repeat cesarean section is performed, and a 2.7-kg (6-lb) infant is delivered with approx. 550 mL blood loss. Perioperatively, she received one dose of intravenous cefazolin. Following the surgery, the patient continues to bleed, and she receives a transfusion of 1 unit of packed red blood cells. One hour later, the patient begins to have flank pain and appears to be in acute distress. Her temperature is 38.5°C (101.3°F), pulse is 111/min, respirations are 22/min, and blood pressure is 99/50 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Foley catheter shows dark brown urine. Further evaluation of this patient is most likely to show which of the following?
- A. Serum antibodies against Class I HLA antigens
- B. Positive blood cultures
- C. Bilateral pulmonary infiltrates on chest x-ray
- D. Positive direct Coombs test (Correct Answer)
- E. Low levels of serum IgA immunoglobulins
Tubulointerstitial diseases Explanation: ***Positive direct Coombs test***
- The patient's symptoms (flank pain, fever, tachycardia, hypotension, dark urine) following a blood transfusion strongly indicate an **acute hemolytic transfusion reaction (AHTR)**.
- A **positive direct Coombs test** confirms AHTR by detecting antibodies coating the transfused red blood cells, indicating immune-mediated hemolysis.
*Serum antibodies against Class I HLA antigens*
- While **HLA antibodies** can form after multiple transfusions, they are primarily associated with **febrile non-hemolytic transfusion reactions** or **transfusion-related acute lung injury (TRALI)**.
- They do not typically cause the rapid and severe hemolytic signs (flank pain, dark urine, hypotension) seen in this patient.
*Positive blood cultures*
- **Bacterial contamination** of blood products can cause fever and hypotension, but it is less likely to cause immediate **flank pain** and **dark urine** indicative of hemolysis.
- Sepsis takes longer to manifest the full spectrum of symptoms like organ dysfunction.
*Bilateral pulmonary infiltrates on chest x-ray*
- **Bilateral pulmonary infiltrates** are characteristic of **TRALI**, which involves acute respiratory distress and hypoxemia.
- Although TRALI can occur post-transfusion, it does not typically present with flank pain or dark urine, which are signs of red blood cell destruction.
*Low levels of serum IgA immunoglobulins*
- **Selective IgA deficiency** can lead to severe anaphylactic reactions to transfused blood products containing IgA, especially in patients with anti-IgA antibodies.
- While severe, these reactions usually present with **bronchospasm**, **urticaria**, and potential anaphylaxis, rather than the primary hemolytic signs observed here.
More Tubulointerstitial diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.