Renal vascular diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Renal vascular diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
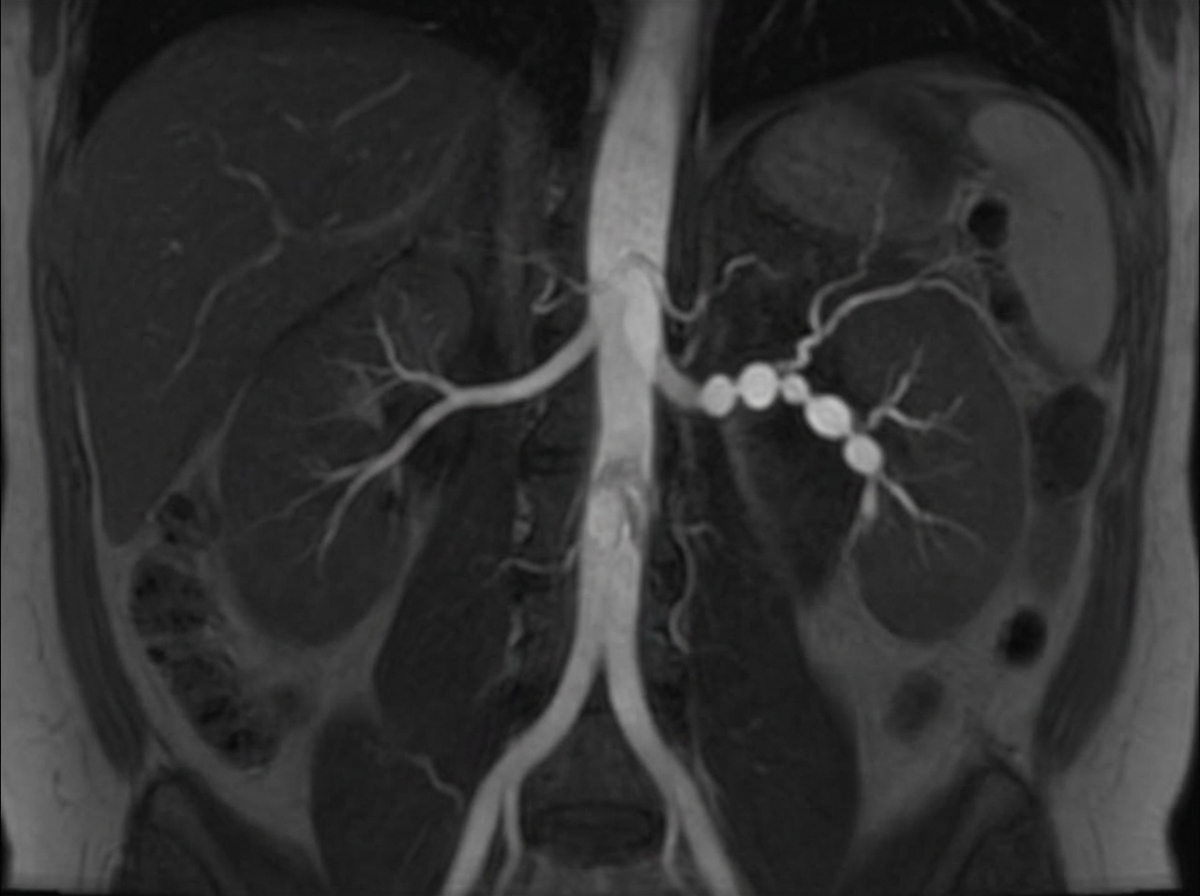
Renal vascular diseases US Medical PG Question 1: A 31-year-old woman returns to her primary care provider for a follow-up visit. At a routine health maintenance visit 2 months ago, her blood pressure (BP) was 181/97 mm Hg. She has adhered to a low-salt diet and exercises regularly. On repeat examination 1 month later, her BP was 178/93, and she was prescribed hydrochlorothiazide and lisinopril. The patient denies any complaint, except for occasional headaches. Now, her BP is 179/95 in the right arm and 181/93 in the left arm. Physical examination reveals an abdominal bruit that lateralizes to the left. A magnetic resonance angiogram of the renal arteries is shown in the image. Which of the following is the best next step for the management of this patient condition?
- A. Balloon angioplasty (Correct Answer)
- B. Intravenous phentolamine
- C. Stenting
- D. Add statin and aspirin
- E. Surgical reconstruction
Renal vascular diseases Explanation: ***Balloon angioplasty***
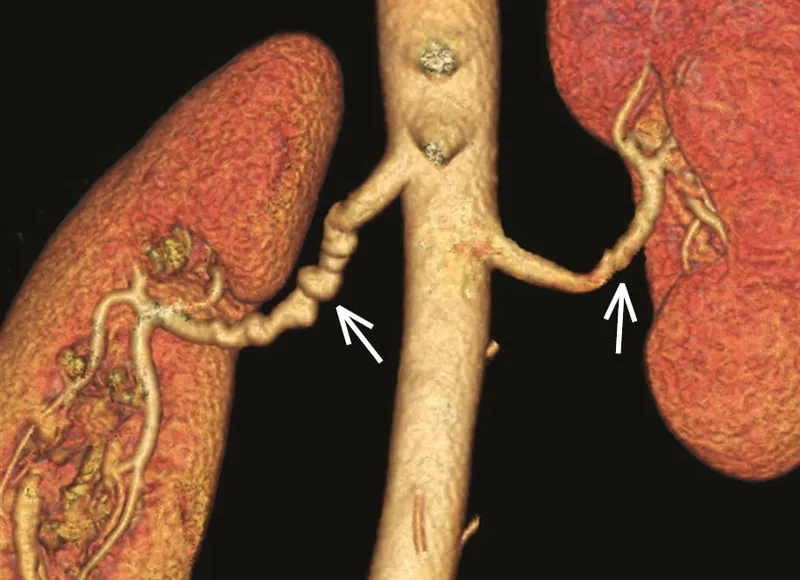
- This patient presents with **severe hypertension, particularly diastolic hypertension**, that is **refractory to standard medical therapy** (hydrochlorothiazide and lisinopril).
- The combination of uncontrolled hypertension in a young woman, a **lateralizing abdominal bruit**, and the **magnetic resonance angiogram (MRA) findings consistent with fibromuscular dysplasia (FMD)** strongly suggests renovascular hypertension, for which **renal artery angioplasty is the preferred treatment**, especially in FMD due to its high success rate and low complication rate compared to stenting.
*Intravenous phentolamine*
- **Phentolamine is an alpha-adrenergic blocker** used for the short-term control of hypertensive crises, particularly those due to **pheochromocytoma** or sympathomimetic overdose.
- It is **not a definitive, long-term treatment for renovascular hypertension** and would not address the underlying anatomical lesion.
*Stenting*
- **Stenting is typically reserved for renal artery stenosis caused by atherosclerosis**, especially in older patients, or for cases of FMD with **recurrent stenosis after angioplasty or with aneurysmal disease**.
- For **initial treatment of FMD**, balloon angioplasty alone is generally preferred due to the lower rate of complications and avoidance of leaving an intimal foreign body in a young patient.
*Add statin and aspirin*
- **Statins and aspirin are crucial for managing atherosclerotic cardiovascular disease risk factors**, especially in patients with established atherosclerosis.
- While general cardiovascular health is important, these medications **do not address the underlying renovascular cause of this patient's hypertension**, which is likely fibromuscular dysplasia, and therefore will not control her severe blood pressure.
*Surgical reconstruction*
- **Surgical revascularization is typically reserved for complex cases of renovascular hypertension** where endovascular approaches have failed or are technically not feasible.
- Given the patient's likely diagnosis of FMD, **endovascular balloon angioplasty is the first-line treatment**, and surgery carries higher risks and is more invasive.
Renal vascular diseases US Medical PG Question 2: A 60-year-old African American woman presents to her family physician with shortness of breath on exertion. She also describes shortness of breath when she lies down to go to bed at night, as well as recent swelling in her ankles. Past medical history is significant for long-standing hypertension, for which she takes amlodipine and lisinopril. Her temperature is 36.8°C (98.2°F), the heart rate is 90/min, the respiratory rate is 15/min, and the blood pressure is 135/80 mm Hg. The physical exam is significant for JVD, lower extremity pitting edema, laterally displaced PMI, left ventricular heave, bilateral pulmonary crackles, and an S4 heart sound. Chest X-ray demonstrates pulmonary vascular congestion, Kerley B lines, and cardiomegaly. Echocardiogram demonstrates a preserved ejection fraction. Kidney biopsy would likely demonstrate which of the following?
- A. Thinning of the intima and media
- B. Onion-skinning
- C. Nodular sclerosis
- D. Intimal thickening and medial hypertrophy (Correct Answer)
- E. Fibrinoid necrosis
Renal vascular diseases Explanation: ***Intimal thickening and medial hypertrophy***
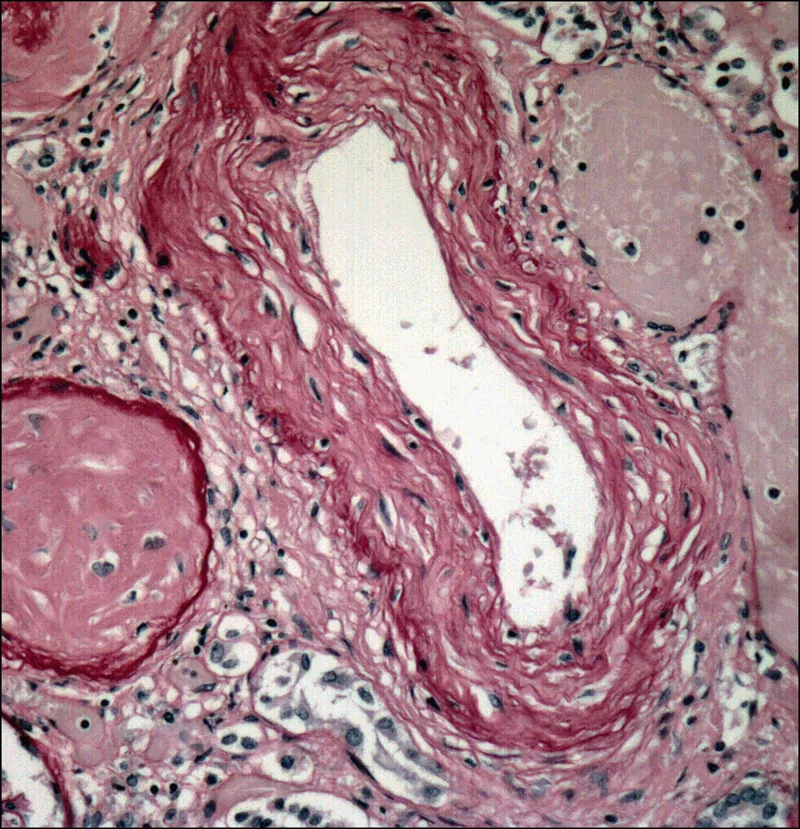
* The patient's presentation of **heart failure with preserved ejection fraction (HFpEF)**, long-standing **hypertension**, and findings like left ventricular heave and S4 heart sound strongly suggest **hypertensive cardiomyopathy**, which in turn causes **hypertensive nephrosclerosis**.
* **Hypertensive nephrosclerosis** is characterized by **intimal thickening** and **medial hypertrophy** of renal arterioles, leading to **ischemia** and atrophy of glomeruli and tubules.
*Thinning of the intima and media*
* This is not a characteristic pathological change seen in hypertensive nephrosclerosis.
* In hypertension, the vessel walls typically undergo thickening due to **hypertrophy** and **hyperplasia** of smooth muscle cells and increased extracellular matrix, not thinning.
*Onion-skinning*
* **"Onion-skinning"** is a hallmark feature of **malignant hypertension**, characterized by concentric laminar thickening of the arteriolar walls.
* The patient's blood pressure (135/80 mmHg) is not consistent with malignant hypertension, which would typically involve much higher blood pressure readings.
*Nodular sclerosis*
* **Nodular sclerosis** (also known as **Kimmelstiel-Wilson lesions**) is characteristic of **diabetic nephropathy**, not primarily hypertensive nephrosclerosis.
* While diabetes and hypertension often co-exist, the prompt in this case points more directly to long-standing hypertension as the primary cause of renal damage.
*Fibrinoid necrosis*
* **Fibrinoid necrosis** of arterioles is also associated with **malignant hypertension** and some forms of vasculitis.
* This patient's blood pressure is controlled (135/80 mmHg) and does not indicate the severe, rapid increase in blood pressure seen in malignant hypertension.
Renal vascular diseases US Medical PG Question 3: A 50-year-old man is brought to the hospital after being found unresponsive in his bed in the morning. He is declared dead on arrival in the emergency room. His wife states that he always had uncontrolled hypertension despite being on multiple medications. An autopsy is performed, and the cause of his death is found to be a hemorrhage in his right basal ganglia. On microscopic examination, the branches of the renal artery have concentric endothelial proliferation with prominent narrowing of the lumen resulting in focal ischemia and hemorrhage of the renal parenchyma. Which of the following is most likely related to the findings in this patient?
- A. Raised cholesterol level in the blood
- B. Elevated ammonia level in the blood
- C. Raised calcium level in the blood
- D. Raised renin level in the blood (Correct Answer)
- E. Elevated C-reactive protein in the blood
Renal vascular diseases Explanation: ***Raised renin level in the blood***
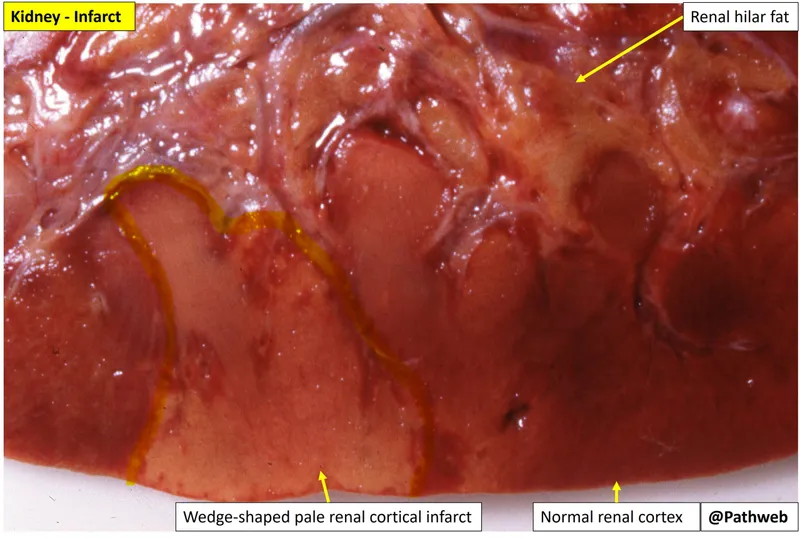
- The patient had uncontrolled **hypertension** leading to a fatal **intracerebral hemorrhage** (typical location: basal ganglia). The key autopsy finding of **concentric endothelial proliferation** with lumen narrowing in renal arteries describes **hyperplastic (proliferative) arteriolosclerosis**, also known as **"onion-skinning"** - the hallmark of **malignant hypertension**.
- In malignant hypertension, severe vascular injury causes **renal ischemia**, which triggers massive activation of the **renin-angiotensin-aldosterone system (RAAS)**, leading to markedly **elevated renin levels**. This creates a vicious cycle: renin elevation → further hypertension → more vascular injury → more renin release.
- The combination of uncontrolled hypertension, intracerebral hemorrhage, and hyperplastic arteriolosclerosis strongly indicates a renin-driven hypertensive crisis.
*Raised cholesterol level in the blood*
- While hypercholesterolemia contributes to **atherosclerosis** and chronic vascular disease, it does not explain the acute pathological finding of **concentric endothelial proliferation (onion-skinning)**.
- Atherosclerosis involves **eccentric plaque formation** with lipid deposition, not the concentric smooth muscle and endothelial proliferation seen in malignant hypertension.
- The acute, severe nature of this patient's vascular changes points to hypertensive emergency, not atherosclerotic disease.
*Elevated ammonia level in the blood*
- **Hyperammonemia** is associated with **hepatic encephalopathy** due to severe liver dysfunction (cirrhosis, acute liver failure), which is not suggested by this patient's presentation.
- Elevated ammonia does not cause hypertension, intracerebral hemorrhage, or the specific renal vascular pathology (hyperplastic arteriolosclerosis) described.
*Raised calcium level in the blood*
- **Hypercalcemia** can cause nephrolithiasis, nephrocalcinosis, and various systemic symptoms, but it is not the primary driver of malignant hypertension or intracerebral hemorrhage.
- While chronic hypercalcemia may contribute to vascular calcification (medial calcific sclerosis), it does not produce the **acute proliferative vascular changes** (onion-skinning) characteristic of malignant hypertension.
*Elevated C-reactive protein in the blood*
- **CRP** is a non-specific inflammatory marker that may be elevated in many chronic conditions, including cardiovascular disease.
- However, CRP elevation is a **consequence** rather than a cause of vascular injury, and it does not explain the specific mechanism of malignant hypertension or the pathognomonic finding of hyperplastic arteriolosclerosis.
- The renin-angiotensin system activation is the primary pathophysiologic mechanism in this case.
Renal vascular diseases US Medical PG Question 4: A previously healthy 40-year-old woman comes to the physician because of a 3-day history of fever, headaches, and fatigue. She also reports a persistent tingling sensation in her right hand and numbness in her right arm that started this morning. Physical examination shows pallor, mild scleral icterus, and petechiae on her forearms and legs. On mental status examination, she appears confused and is only oriented to person. Laboratory studies show:
Hemoglobin 11.1 g/dL
Platelet count 39,500/mm3
Bleeding time 9 minutes
Prothrombin time 14 seconds
Partial thromboplastin time 35 seconds
Serum
Creatinine 1.7 mg/dL
Total bilirubin 2.1 mg/dL
A peripheral blood smear shows fragmented erythrocytes. Which of the following is the most likely underlying cause of this patient's condition?
- A. Antibodies against double-stranded DNA
- B. Mutation of the PIGA gene
- C. Antibodies against GpIIb/IIIa
- D. Antibodies against ADAMTS13 (Correct Answer)
- E. Absence of platelet GpIIb/IIIa receptors
Renal vascular diseases Explanation: ***Antibodies against ADAMTS13***
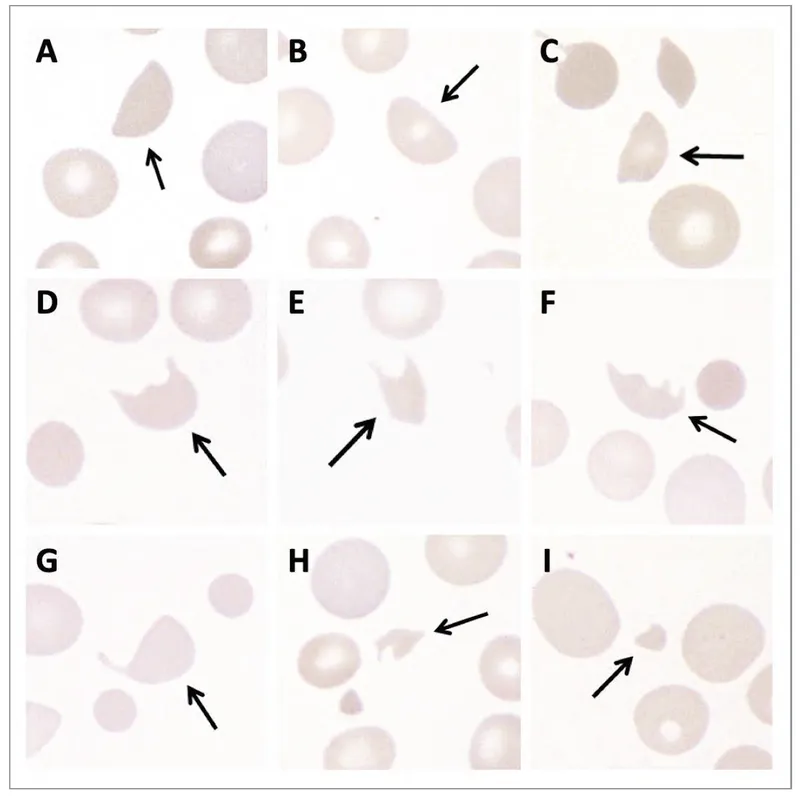
- This patient presents with a classic pentad of symptoms: **fever**, **neurologic symptoms** (confusion, tingling, numbness), **renal failure** (creatinine 1.7 mg/dL), **thrombocytopenia** (platelet count 39,500/mm3), and **microangiopathic hemolytic anemia** (pallor, scleral icterus, fragmented erythrocytes on smear). This constellation of findings is highly suggestive of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is primarily caused by a deficiency of the **ADAMTS13 enzyme**, often due to **autoantibodies** that inhibit its activity. ADAMTS13 is responsible for cleaving large **von Willebrand factor (vWF) multimers**, and its deficiency leads to the accumulation of these large multimers, promoting platelet aggregation and microthrombi formation.
*Antibodies against double-stranded DNA*
- Antibodies against double-stranded DNA (**anti-dsDNA antibodies**) are characteristic of **Systemic Lupus Erythematosus (SLE)**, which can present with various systemic symptoms.
- While SLE can cause thrombocytopenia and renal involvement, it typically does not cause the severe **microangiopathic hemolytic anemia** with schistocytes or the combination of symptoms seen in this patient to the extent of TTP.
*Mutation of the PIGA gene*
- A **mutation of the *PIGA* gene** is responsible for **Paroxysmal Nocturnal Hemoglobinuria (PNH)**, a clonal stem cell disorder characterized by hemolytic anemia, thrombosis, and bone marrow failure.
- While PNH involves hemolysis, it typically lacks the prominent neurological symptoms, severe thrombocytopenia with microangiopathic features, and renal failure seen in TTP.
*Antibodies against GpIIb/IIIa*
- **Antibodies against GpIIb/IIIa** (glycoprotein IIb/IIIa) receptors are the hallmark of **Immune Thrombocytopenic Purpura (ITP)**, causing accelerated platelet destruction.
- ITP primarily causes **isolated thrombocytopenia** and mucocutaneous bleeding, but it does not cause microangiopathic hemolytic anemia, renal failure, or neurological symptoms that are prominent in this patient.
*Absence of platelet GpIIb/IIIa receptors*
- The **absence of platelet GpIIb/IIIa receptors** is characteristic of **Glanzmann's thrombasthenia**, a rare inherited disorder of platelet function.
- Glanzmann's thrombasthenia leads to **mucocutaneous bleeding** due to impaired platelet aggregation, but it does not cause thrombocytopenia, hemolytic anemia, renal failure, or neurological symptoms.
Renal vascular diseases US Medical PG Question 5: A 53-year-old woman presents with a severe headache, nausea, and vomiting for the past 48 hours. Vitals show a blood pressure of 220/134 mm Hg and a pulse of 88/min. Urinalysis shows a 2+ proteinuria and RBC casts. Which of the following renal lesions is most likely to be seen in this patient?
- A. Papillary necrosis
- B. Fibrinoid necrosis (Correct Answer)
- C. Acute tubular necrosis (ATN)
- D. Acute pyelonephritis
- E. Acute interstitial nephritis (AIN)
Renal vascular diseases Explanation: ***Fibrinoid necrosis***
- The patient's presentation with **severe hypertension** (220/134 mm Hg), **proteinuria**, and **RBC casts** is highly suggestive of a **hypertensive crisis with malignant nephrosclerosis**.
- **Fibrinoid necrosis** refers to the accumulation of **fibrin-like material** in the walls of arterioles, a characteristic pathological finding in **malignant hypertension** leading to vascular damage in the kidney.
*Papillary necrosis*
- This condition is typically associated with **analgesic nephropathy**, **diabetes mellitus**, and **urinary tract obstruction** or **sickle cell disease**.
- While it can cause renal dysfunction, it does not directly explain the acute severe hypertension and RBC casts unique to hypertensive emergencies.
*Acute tubular necrosis (ATN)*
- While ATN can cause **acute kidney injury**, it is usually characterized by **muddy brown casts** and is often precipitated by **ischemic** or **nephrotoxic insults**.
- The prominent hypertension and RBC casts point away from primary ATN in this context.
*Acute pyelonephritis*
- Acute pyelonephritis is an **infection of the kidney** characterized by **fever**, **flank pain**, and **pyuria** (white blood cells in urine), usually not severe hypertension and RBC casts.
- The main findings in this patient are related to vascular damage, not infection.
*Acute interstitial nephritis (AIN)*
- AIN is often caused by **drug reactions** or systemic diseases, presenting with **fever**, **rash**, **eosinophilia**, and **white blood cell casts**.
- The clinical picture of severe hypertension and RBC casts is not typical for AIN.
Renal vascular diseases US Medical PG Question 6: A 62-year-old man comes to the physician because of fatigue and swelling of the lower legs for 3 weeks. One year ago, he had an 85% stenosis in the left anterior descending artery, for which he received 2 stents. He was diagnosed with hepatitis C 5 years ago. He has type 2 diabetes mellitus and arterial hypertension. Current medications include aspirin, metformin, and ramipril. He does not smoke or drink alcohol. His temperature is 37°C (98.6°F), pulse is 92/min, and blood pressure is 142/95 mm Hg. Examination shows 2+ pretibial edema bilaterally. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.2 g/dL
Leukocyte count 6500/mm3
Platelet count 188,000/mm3
Serum
Na+ 137 mEq/L
Cl− 105 mEq/L
K+ 5.2 mEq/L
Urea nitrogen 60 mg/dL
Glucose 110 mg/dL
Creatinine 3.9 mg/dL
Albumin 3.6 g/dL
HbA1C 6.8%
Urine
Blood negative
Glucose 1+
Protein 3+
WBC 0–1/hpf
A renal biopsy shows sclerosis in the capillary tufts and arterial hyalinosis. Which of the following is the most likely underlying mechanism of this patient's findings?
- A. Diabetes mellitus
- B. Arterial hypertension (Correct Answer)
- C. Amyloidosis
- D. Membranoproliferative glomerulonephritis
- E. Membranous nephropathy
Renal vascular diseases Explanation: ***Arterial hypertension***
- The patient's **blood pressure of 142/95 mm Hg** and history of arterial hypertension, coupled with **arterial hyalinosis** and **glomerulosclerosis (sclerosis in the capillary tufts)** seen on biopsy, strongly indicate hypertensive nephrosclerosis as the primary cause of renal damage. **Arterial hyalinosis** is the pathognomonic finding of hypertensive nephropathy, resulting from chronic endothelial injury and plasma protein deposition in vessel walls.
- The elevated **urea nitrogen (60 mg/dL)** and **creatinine (3.9 mg/dL)**, along with significant **proteinuria (3+)**, indicate substantial kidney damage, consistent with chronic hypertensive nephrosclerosis.
- The inadequate blood pressure control despite ACE inhibitor therapy (ramipril) demonstrates ongoing hypertensive injury.
*Diabetes mellitus*
- While the patient has diabetes, the biopsy finding of **arterial hyalinosis** and **glomerulosclerosis** is more characteristic of hypertensive nephrosclerosis rather than diabetic nephropathy.
- Diabetic nephropathy typically presents with **glomerular basement membrane thickening**, **mesangial expansion**, and **Kimmelstiel-Wilson nodules** (nodular glomerulosclerosis), which are not the primary biopsy findings described here.
- Additionally, the patient's **good glycemic control (HbA1C 6.8%)** makes advanced diabetic nephropathy less likely.
*Amyloidosis*
- Amyloidosis would typically show characteristic **amyloid deposits** in the glomeruli and interstitium, which stain positive with **Congo red** and exhibit apple-green birefringence under polarized light, findings not reported.
- Presentation usually includes significant proteinuria, often in the nephrotic range, and can affect multiple organs, but the specific biopsy findings of **arterial hyalinosis** point away from amyloidosis as the primary cause.
*Membranoproliferative glomerulonephritis*
- This condition is typically characterized by **mesangial and endothelial proliferation**, **glomerular basement membrane thickening** with a "tram-track" appearance (due to mesangial interposition), and often immune complex deposits.
- While the patient has hepatitis C (a known risk factor for MPGN), the biopsy findings of **glomerulosclerosis** and **arterial hyalinosis** are not specific for MPGN, and the characteristic proliferative changes are not described.
*Membranous nephropathy*
- Membranous nephropathy is primarily characterized by **subepithelial immune complex deposits** and **diffuse thickening of the glomerular basement membrane** (spike and dome appearance on silver stain).
- It is a common cause of nephrotic syndrome in adults, but the biopsy describes **glomerulosclerosis** and **arterial hyalinosis** which are not the hallmark features of membranous nephropathy.
Renal vascular diseases US Medical PG Question 7: A 48-year-old man is brought to the emergency department by his wife because of a 3-day history of increasing confusion and lethargy. He complains of decreased urine output and abdominal pain for the past month. Two months ago, he was hospitalized for pyelonephritis and treated with ceftriaxone. He has a history of chronic hepatitis C. He does not take any medications. He appears pale and irritable. His temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 98/60 mm Hg. On mental status examination, he is oriented to person but not to time or place. Physical examination shows scleral icterus and jaundice. There is 2+ pitting edema of the lower extremities. The abdomen is distended with a positive fluid wave. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 4300/mm3
Platelet count 89,000/mm3
Prothrombin time 19 sec
Serum
Urea nitrogen 71 mg/dL
Glucose 99 mg/dL
Creatinine 3.5 mg/dL
ALT 137 mg/dL
AST 154 mg/dL
Urinalysis shows no abnormalities. The FeNa is < 1%. Ultrasound of the kidneys is unremarkable. Intravenous fluids are administered for 36 hours but do not improve urine output. Which of the following is the most likely cause of the kidney dysfunction in this patient?
- A. Renal vein thrombosis
- B. Renal tubular injury
- C. Renal microvascular thrombi
- D. Decreased renal perfusion (Correct Answer)
- E. Renal interstitial inflammation
Renal vascular diseases Explanation: ***Decreased renal perfusion***
- The patient's history of **chronic hepatitis C** with signs of **liver dysfunction** (jaundice, scleral icterus, distended abdomen with fluid wave, prolonged PT, thrombocytopenia, confusion) suggests **cirrhosis** and portal hypertension, leading to **hepatorenal syndrome (HRS)**.
- **HRS** is characterized by severe **renal vasoconstriction** due to systemic vasodilation and decreased effective arterial blood volume, leading to impaired renal perfusion and function that does **not respond to fluid resuscitation**, as seen in this patient.
- The **low FeNa (<1%)** reflects avid sodium retention, **unremarkable urinalysis** excludes intrinsic renal disease, and **lack of improvement with 36 hours of IV fluids** confirms the diagnosis.
*Renal vein thrombosis*
- This condition is often associated with **nephrotic syndrome** or hypercoagulable states, typically presenting with **flank pain**, hematuria, and a sudden decline in renal function.
- The patient's clinical picture and laboratory findings (e.g., **negative urinalysis**, **low FeNa**, **no response to volume expansion**) are not typical for renal vein thrombosis, which would show abnormal imaging findings.
*Renal tubular injury*
- **Acute tubular necrosis (ATN)**, a form of renal tubular injury, typically occurs after **ischemic or nephrotoxic insults** and is characterized by muddy brown granular casts on urinalysis and a **high FeNa (>2%)**.
- In this case, the **unremarkable urinalysis** and **FeNa <1%** argue against ATN or other primary tubular injury as the cause of acute kidney injury.
*Renal microvascular thrombi*
- Conditions involving renal microvascular thrombi, such as **thrombotic microangiopathy**, often present with **thrombocytopenia**, microangiopathic hemolytic anemia (schistocytes), and severe hypertension.
- While the patient has thrombocytopenia, there is **no evidence of hemolysis** or other features typical of primary microvascular thrombi, and the clinical context points to liver disease as the primary etiology.
*Renal interstitial inflammation*
- **Acute interstitial nephritis (AIN)** is usually drug-induced (e.g., antibiotics, NSAIDs) and presents with **eosinophilia**, rash, fever, and white blood cell casts in the urine.
- The patient's presentation does not include these findings, and the **unremarkable urinalysis** makes AIN less likely. The recent ceftriaxone treatment was 2 months ago, making drug-induced AIN temporally unlikely.
Renal vascular diseases US Medical PG Question 8: A 60-year-old male presents for a routine health check-up. The patient complains of reduced exercise tolerance for the past 2 years. Also, in the past year, he has noticed chest pain after climbing the stairs in his home. He has no significant past medical history or current medications. The patient reports a 45-pack-year smoking history. The vital signs include temperature 37.0°C (98.6°F), blood pressure 160/100 mm Hg, pulse 72/min, respiratory rate 15/min, and oxygen saturation 99% on room air. His body mass index (BMI) is 34 kg/m2. Physical examination is unremarkable. Laboratory studies show:
Serum total cholesterol 265 mg/dL
HDL 22 mg/dL
LDL 130 mg/dL
Triglycerides 175 mg/dL
HDL: high-density lipoprotein; LDL: low-density lipoprotein
Which of the following vascular pathologies is most likely present in this patient?
- A. Medial calcific sclerosis
- B. Deep venous thrombosis
- C. Lymphedema
- D. Atherosclerosis (Correct Answer)
- E. Hyperplastic arteriosclerosis
Renal vascular diseases Explanation: ***Atherosclerosis***
- This patient presents with multiple **risk factors for atherosclerosis**, including **hyperlipidemia** (elevated total cholesterol, LDL, and triglycerides with low HDL), **hypertension**, **obesity**, and a significant **smoking history**.
- His symptoms of **reduced exercise tolerance** and **exertional chest pain** are classic manifestations of **angina pectoris**, which is caused by narrowed coronary arteries due to atherosclerosis.
*Medial calcific sclerosis*
- Also known as **Mönckeberg arteriosclerosis**, involves calcification of the **tunica media** of muscular arteries, without significant luminal narrowing.
- While it can lead to **artery hardening**, it typically does not obstruct blood flow or cause angina, and is more common in **elderly** and **diabetic** individuals.
*Deep venous thrombosis*
- This condition involves the formation of a **blood clot in a deep vein**, usually in the legs, leading to symptoms like **leg swelling, pain, and redness**.
- The patient's symptoms of chest pain and reduced exercise tolerance are not characteristic of DVT.
*Lymphedema*
- Characterized by **swelling** in one or more limbs due to an impaired **lymphatic drainage system**.
- It does not present with chest pain or reduced exercise tolerance and is distinct from vascular pathologies affecting blood flow.
*Hyperplastic arteriosclerosis*
- This is a form of **arteriolar sclerosis** primarily seen in severe **hypertension**, characterized by **concentric thickening of arteriolar walls** due to smooth muscle cell proliferation and basement membrane duplication.
- While the patient has hypertension, his symptoms point towards obstruction of larger coronary arteries rather than widespread arteriolar changes, and his lipid profile is more indicative of atherosclerosis.
Renal vascular diseases US Medical PG Question 9: A 67-year-old man presents with pain in both legs. He says the pain is intermittent in nature and has been present for approximately 6 months. The pain increases with walking, especially downhill, and prolonged standing. It is relieved by lying down and leaning forward. Past medical history is significant for type 2 diabetes mellitus, hypercholesterolemia, and osteoarthritis. The patient reports a 56-pack-year history but denies any alcohol or recreational drug use. His vital signs include: blood pressure 142/88 mm Hg, pulse 88/min, respiratory rate 14/min, temperature 37°C (98.6°F). On physical examination, the patient is alert and oriented. Muscle strength is 5/5 in his upper and lower extremities bilaterally. Babinski and Romberg tests are negative. Pulses measure 2+ in upper and lower extremities bilaterally. Which of the following is the next best step in the management of this patient?
- A. MRI of the spine (Correct Answer)
- B. CT angiography of the lower extremities
- C. Ankle-brachial index
- D. Cilostazol
- E. Epidural corticosteroid injection
Renal vascular diseases Explanation: ***MRI of the spine***
- The patient's symptoms of **intermittent leg pain worsened by walking (especially downhill) and prolonged standing**, and **relieved by lying down and leaning forward**, are highly classic for **neurogenic claudication** due to **lumbar spinal stenosis**.
- An **MRI of the spine** is the *gold standard* for diagnosing spinal stenosis, clearly visualizing nerve root compression and the degree of canal narrowing.
*CT angiography of the lower extremities*
- This imaging is used to assess **peripheral artery disease** (PAD) but the patient's symptoms are inconsistent with vascular claudication.
- **Vascular claudication** typically improves with rest, not with specific postures like leaning forward.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is a non-invasive test to screen for **peripheral artery disease (PAD)**.
- While the patient has risk factors for PAD (diabetes, hypercholesterolemia, smoking), his symptoms are classic for neurogenic claudication, and his **2+ pulses** in the lower extremities make PAD less likely.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used to treat symptoms of **intermittent claudication** caused by **peripheral artery disease (PAD)**.
- Since the patient's symptoms are more consistent with neurogenic claudication rather than vascular claudication, cilostazol would not be the appropriate initial step.
*Epidural corticosteroid injection*
- An **epidural corticosteroid injection** is a treatment option for symptomatic spinal stenosis but is not the *initial diagnostic step*.
- Diagnosis with an **MRI** is necessary before considering targeted therapeutic interventions like injections.
Renal vascular diseases US Medical PG Question 10: A 70-year-old man is brought to the emergency department by his wife because of lethargy, confusion, and nausea for the past 2 days. He has previously been healthy and has no past medical history. His only medications are a daily multivitamin and acetaminophen, which he takes daily for hip pain. Vital signs are within normal limits. He is disoriented to place and time but recognizes his wife. The remainder of his physical examination shows no abnormalities. Laboratory studies show a hemoglobin concentration of 9.1 g/dL, a serum calcium concentration of 14.7 mg/dL, and a serum creatinine of 2.2 mg/dL (previously 0.9 mg/dL). Which of the following is the most likely underlying mechanism of this patient's condition?
- A. Increased serum levels of 1,25-hydroxyvitamin D
- B. Excessive consumption of calcium
- C. Excess PTH secretion from parathyroid glands
- D. Ectopic PTHrP release
- E. Overproliferation of plasma cells (Correct Answer)
Renal vascular diseases Explanation: ***Overproliferation of plasma cells***
- The patient presents with **hypercalcemia** (14.7 mg/dL), acute **kidney injury** (creatinine 2.2 mg/dL from 0.9 mg/dL), and **anemia** (hemoglobin 9.1 g/dL). These three findings, especially in an elderly patient, strongly suggest **multiple myeloma**, which is characterized by the overproliferation of plasma cells in the bone marrow.
- The overproliferation of plasma cells in multiple myeloma leads to the production of **osteoclast-activating factors**, resulting in increased bone resorption and subsequent hypercalcemia.
*Increased serum levels of 1,25-hydroxyvitamin D*
- While **elevated vitamin D levels** can cause hypercalcemia, it typically occurs due to excessive supplementation or granulomatous diseases (e.g., sarcoidosis). There is no history of either in this patient.
- This mechanism would not explain the accompanying **anemia** or **acute kidney injury** (beyond what hypercalcemia itself might induce), which are prominent features here.
*Excessive consumption of calcium*
- **Milk-alkali syndrome**, caused by excessive intake of calcium and absorbable alkali, can lead to hypercalcemia, metabolic alkalosis, and renal insufficiency.
- However, the patient's history does not indicate excessive calcium intake, and this etiology would not typically explain significant **anemia**.
*Excess PTH secretion from parathyroid glands*
- **Primary hyperparathyroidism** results in increased PTH, leading to hypercalcemia and often low or normal phosphate. While it can cause kidney stones and bone issues, it does not typically cause **anemia** or the rapid progression of kidney injury seen here.
- The patient's creatinine has doubled in a short period, which is more suggestive of an acute insult or a systemic disease like myeloma, rather than chronic changes from primary hyperparathyroidism.
*Ectopic PTHrP release*
- **Parathyroid hormone-related protein (PTHrP)** can be ectopically secreted by various malignancies (e.g., squamous cell carcinoma of the lung, renal cell carcinoma), leading to **humoral hypercalcemia of malignancy**.
- While this can cause **hypercalcemia** and related kidney issues, it typically does not directly cause **anemia** in the same way as multiple myeloma, where **bone marrow infiltration** by plasma cells directly suppresses hematopoiesis. The constellation of hypercalcemia, anemia, and acute kidney injury points more specifically to multiple myeloma.
More Renal vascular diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.