Rapidly progressive glomerulonephritis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Rapidly progressive glomerulonephritis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Rapidly progressive glomerulonephritis US Medical PG Question 1: A 25-year-old man is brought to the physician because of fatigue, lethargy, and lower leg swelling for 2 weeks. He also noticed that his urine appeared darker than usual and for the last 2 days he has passed only small amounts of urine. His temperature is 37.5°C (98.6°F), pulse is 88/min, respirations are 15/min, and blood pressure is 154/98 mm Hg. Examination shows 2+ pretibial edema bilaterally. Laboratory studies show:
Hemoglobin 10.9 g/dL
Leukocyte count 8200/mm3
Platelet count 220,000/mm3
Serum
Na+ 137 mEq/L
Cl- 102 mEq/L
K+ 4.8 mEq/L
HCO3- 22 mEq/L
Glucose 85 mg/dL
Urea nitrogen 34 mg/dL
Creatinine 1.4 mg/dL
Urine
Blood 2+
Protein 3+
Glucose negative
RBC 10–12/HPF with dysmorphic features
RBC casts numerous
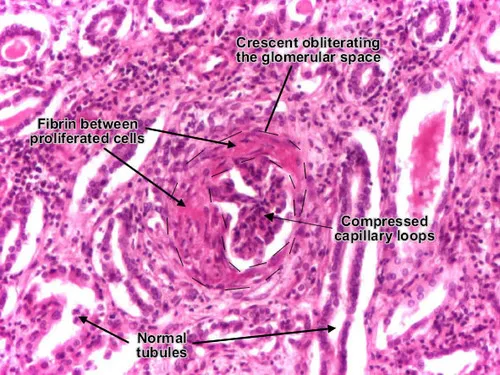
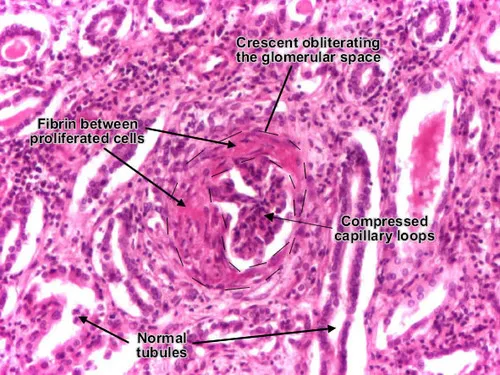
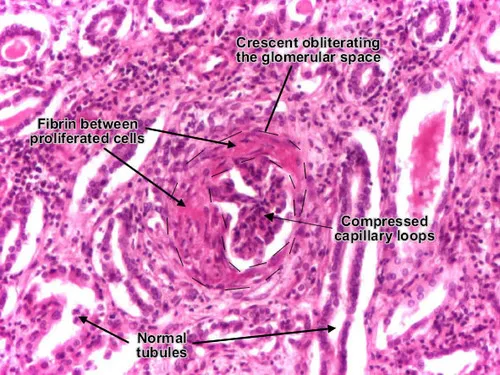
Renal biopsy specimen shows a crescent formation in the glomeruli with extracapillary cell proliferation. Which of the following is the most appropriate next step in management?
- A. Administer methylprednisolone (Correct Answer)
- B. Administer lisinopril
- C. Administer cyclosporine A
- D. Perform hemodialysis
- E. Administer rituximab
Rapidly progressive glomerulonephritis Explanation: ***Administer methylprednisolone***
- The patient presents with **rapidly progressive glomerulonephritis (RPGN)**, characterized by acute renal failure, nephritic-range proteinuria, dysmorphic red blood cells, RBC casts, and crescent formation on biopsy. **High-dose corticosteroids (e.g., methylprednisolone)** are the first-line treatment to suppress inflammation and preserve renal function in RPGN.
- The presence of **crescent formation** in the glomeruli indicates severe glomerular injury and is a hallmark of RPGN, necessitating aggressive immunosuppressive therapy like corticosteroids.
*Administer lisinopril*
- **Lisinopril**, an **ACE inhibitor**, is primarily used to manage hypertension and reduce proteinuria in chronic kidney disease, but it is not the initial treatment for acute, rapidly progressing glomerulonephritis with active inflammation.
- While the patient has hypertension (154/98 mm Hg), addressing the underlying inflammatory process with immunosuppression takes precedence over symptomatic blood pressure management in this acute setting.
*Administer cyclosporine A*
- **Cyclosporine A** is an immunosuppressant that can be used in certain forms of glomerulonephritis, but it is typically reserved for cases that are **refractory to corticosteroids** or as a second-line agent.
- It's not typically the initial therapy for RPGN due to its potential **nephrotoxicity** and slower onset of action compared to high-dose corticosteroids.
*Perform hemodialysis*
- **Hemodialysis** is indicated for **end-stage renal disease** or severe complications of acute kidney injury, such as refractory anasarca, severe metabolic acidosis, or hyperkalemia.
- While the patient has elevated creatinine and oliguria, his condition is acute and potentially reversible with immunosuppressive therapy. Hemodialysis would be considered if medical management fails or if life-threatening complications develop.
*Administer rituximab*
- **Rituximab**, an anti-CD20 monoclonal antibody, is used in specific types of glomerulonephritis, such as **ANCA-associated vasculitis** or **membranous nephropathy** that is refractory to other treatments.
- It is not the initial treatment for undifferentiated RPGN, especially without specific serologic markers like ANCA being positive or an established diagnosis for which rituximab is the primary agent.
Rapidly progressive glomerulonephritis US Medical PG Question 2: A 6-year-old boy presents to your office with hematuria. Two weeks ago the patient had symptoms of a sore throat and fever. Although physical exam is unremarkable, laboratory results show a decreased serum C3 level and an elevated anti-DNAse B titer. Which of the following would you most expect to see on renal biopsy?
- A. Immune complex deposits with a "spike and dome" appearance on electron microscopy
- B. Large, hypercellular glomeruli on light microscopy (Correct Answer)
- C. Wirelooping and hyaline thrombi on light microscopy
- D. Polyclonal IgA deposition on immunofluorescence
- E. Antibodies to GBM resulting in a linear immunofluorescence pattern
Rapidly progressive glomerulonephritis Explanation: ***Large, hypercellular glomeruli on light microscopy***
- The clinical presentation, including recent **sore throat**, **hematuria**, decreased **C3**, and elevated **anti-DNAse B titer**, is highly suggestive of **post-streptococcal glomerulonephritis (PSGN)**.
- On light microscopy, PSGN characteristically shows **diffuse proliferative glomerulonephritis** with **enlarged, hypercellular glomeruli** due to inflammatory cell infiltration and proliferation of intrinsic glomerular cells.
*Immune complex deposits with a "spike and dome" appearance on electron microscopy*
- This "spike and dome" appearance refers to **subepithelial deposits** with new basement membrane formation, which is characteristic of **membranous nephropathy**, not PSGN.
- Membranous nephropathy typically presents with **nephrotic syndrome** in adults, which is different from the child's presentation here.
*Wirelooping and hyaline thrombi on light microscopy*
- These features, particularly **"wire-loop" lesions** and **hyaline thrombi**, suggest severe **lupus nephritis**, a manifestation of **systemic lupus erythematosus**.
- Lupus nephritis often presents with a range of kidney pathologies and systemic symptoms not seen in this patient.
*Polyclonal IgA deposition on immunofluorescence*
- **IgA deposition** in the mesangium is the hallmark of **IgA nephropathy (Berger's disease)**, which typically presents with recurrent hematuria, often after an upper respiratory infection.
- While there is hematuria and a recent infection, the decreased C3 and elevated anti-DNAse B titer point away from IgA nephropathy.
*Antibodies to GBM resulting in a linear immunofluorescence pattern*
- A **linear pattern** of IgG deposits along the glomerular basement membrane (GBM) is characteristic of **Goodpasture syndrome (anti-GBM disease)**.
- This condition involves antibodies specifically targeting the GBM and often presents with rapidly progressive glomerulonephritis and pulmonary hemorrhage, which are not described here.
Rapidly progressive glomerulonephritis US Medical PG Question 3: A 12-year-old girl is presented to the office by her mother with complaints of cola-colored urine and mild facial puffiness that began 5 days ago. According to her mother, she had a sore throat 3 weeks ago. Her immunization records are up to date. The mother denies fever and any change in bowel habits. The vital signs include blood pressure 138/78 mm Hg, pulse 88/min, temperature 36.8°C (98.2°F), and respiratory rate 11/min. On physical examination, there is pitting edema of the upper and lower extremities bilaterally. An oropharyngeal examination is normal. Urinalysis shows the following results:
pH 6.2
Color dark brown
Red blood cell (RBC) count 18–20/HPF
White blood cell (WBC) count 3–4/HPF
Protein 1+
Cast RBC casts
Glucose absent
Crystal none
Ketone absent
Nitrite absent
24 h urine protein excretion 0.6 g
HPF: high-power field
Which of the following would best describe the light microscopy findings in this case?
- A. Segmental sclerosis and hyalinosis
- B. Wire looping of capillaries
- C. Mesangial proliferation
- D. Hypercellular and enlarged glomeruli (Correct Answer)
- E. Crescentic proliferation consisting of glomerular parietal cells, macrophage, and fibrin
Rapidly progressive glomerulonephritis Explanation: ***Hypercellular and enlarged glomeruli***
- The patient's presentation with **cola-colored urine**, facial puffiness, edema, hypertension, and a recent history of sore throat points to **post-streptococcal glomerulonephritis (PSGN)**.
- Light microscopy in PSGN typically reveals **diffuse hypercellularity** due to proliferation of mesangial and endothelial cells, and infiltration by inflammatory cells, leading to enlarged glomeruli.
*Segmental sclerosis and hyalinosis*
- This finding is characteristic of **focal segmental glomerulosclerosis (FSGS)**, which typically presents with **nephrotic syndrome** (heavy proteinuria, hypoalbuminemia, severe edema).
- While there is proteinuria in this case, it is not in the nephrotic range, and other clinical features do not support FSGS.
*Wire looping of capillaries*
- **Wire looping** is a classic feature of **diffuse proliferative glomerulonephritis (DPGN)**, often seen in **lupus nephritis (Class III or IV)**.
- The patient’s clinical picture, particularly the antecedent sore throat and acute presentation, is not consistent with lupus nephritis.
*Mesangial proliferation*
- While mesangial proliferation occurs in PSGN, it is usually accompanied by **endocapillary proliferation** and inflammatory cell infiltration, making the glomeruli appear diffusely hypercellular and enlarged.
- Isolated mesangial proliferation is more characteristic of **IgA nephropathy**, which typically presents with recurrent episodes of gross hematuria, sometimes concurrent with or shortly after an upper respiratory infection.
*Crescentic proliferation consisting of glomerular parietal cells, macrophage, and fibrin*
- **Crescents** are pathognomonic of **rapidly progressive glomerulonephritis (RPGN)**, which involves severe and rapid loss of renal function.
- While PSGN can occasionally progress to RPGN, the typical presentation of PSGN usually does not involve prominent crescent formation unless severe.
Rapidly progressive glomerulonephritis US Medical PG Question 4: A 21-year-old male presents to your office with hematuria 3 days after the onset of a productive cough and fever. Following renal biopsy, immunofluorescence shows granular IgA deposits in the glomerular mesangium. Which of the following do you suspect in this patient?
- A. Lipoid nephrosis
- B. Berger’s disease (Correct Answer)
- C. HIV infection
- D. Systemic lupus erythematosus
- E. Poststreptococcal glomerulonephritis
Rapidly progressive glomerulonephritis Explanation: ***Berger’s disease***
- The presentation of **hematuria occurring 3 days after a respiratory infection** (productive cough and fever) is characteristic of **IgA nephropathy** or Berger's disease, showing a synpharyngitic pattern.
- **Immunofluorescence showing granular IgA deposits in the glomerular mesangium** is the histological hallmark of IgA nephropathy.
*Lipoid nephrosis*
- This condition is also known as **minimal change disease** and typically presents with **nephrotic syndrome** (heavy proteinuria, edema, hypoalbuminemia), not primarily hematuria.
- Renal biopsy would reveal **effacement of foot processes** on electron microscopy with normal light microscopy and negative immunofluorescence, unlike the IgA deposits described.
*HIV infection*
- HIV can lead to **HIV-associated nephropathy (HIVAN)**, which typically presents as **focal segmental glomerulosclerosis** (FSGS) and can include proteinuria and progressive renal failure.
- While hematuria can occur, the characteristic **IgA deposits in the mesangium** described are not typical for HIVAN.
*Systemic lupus erythematosus*
- **Lupus nephritis** is a common complication of SLE, and can present with hematuria, proteinuria, and various patterns of glomerulonephritis.
- However, immunofluorescence in lupus nephritis usually shows **IgG, IgM, IgA, C3, and C1q deposits** (full-house staining), not isolated IgA deposits.
*Poststreptococcal glomerulonephritis*
- This condition typically presents with **hematuria 10-14 days after a streptococcal infection** (post-infectious glomerulonephritis), a longer latency period than seen in this patient.
- Immunofluorescence would show unique **"lumpy-bumpy" granular deposits of C3 and IgG** along the glomerular basement membrane, often with characteristic subepithelial humps on electron microscopy, rather than mesangial IgA.
Rapidly progressive glomerulonephritis US Medical PG Question 5: A 57-year-old woman comes to the clinic complaining of decreased urine output. She reports that over the past 2 weeks she has been urinating less and less every day. She denies changes in her diet or fluid intake. The patient has a history of lupus nephritis, which has resulted in end stage renal disease. She underwent a renal transplant 2 months ago. Since then she has been on mycophenolate and cyclosporine, which she takes as prescribed. The patient’s temperature is 99°F (37.2°C), blood pressure is 172/102 mmHg, pulse is 88/min, and respirations are 17/min with an oxygen saturation of 97% on room air. Labs show an elevation in serum creatinine and blood urea nitrogen. On physical examination, she has 2+ pitting edema of the bilateral lower extremities. Lungs are clear to auscultation. Urinalysis shows elevated protein. A post-void bladder scan is normal. A renal biopsy is obtained, which shows lymphocyte infiltration and intimal swelling. Which of the following is the next best step in management?
- A. Add diltiazem
- B. Nephrectomy
- C. Start intravenous steroids (Correct Answer)
- D. Add ceftriaxone
- E. Discontinue cyclosporine
Rapidly progressive glomerulonephritis Explanation: ***Start intravenous steroids***
- The patient presents with **decreased urine output**, elevated creatinine, and a recent kidney transplant with biopsy showing **lymphocyte infiltration** and **intimal swelling**, all highly suggestive of **acute cellular rejection**.
- **High-dose intravenous steroids** (e.g., methylprednisolone) are the first-line treatment for acute cellular rejection to suppress the immune response and preserve graft function.
*Add diltiazem*
- **Diltiazem** is a calcium channel blocker used to treat hypertension and arrhythmias, and it can also interfere with cyclosporine metabolism, potentially increasing its levels.
- While the patient has elevated blood pressure, adding diltiazem would not address the underlying **immune rejection** and would not be the primary intervention.
*Nephrectomy*
- **Nephrectomy** involves surgical removal of the transplanted kidney. This radical intervention is reserved for **irreversible graft failure** or severe complications like overwhelming infection or malignancy.
- Given the acute presentation and possibility of reversing rejection with immunosuppression, nephrectomy is **premature** and not the next best step.
*Add ceftriaxone*
- **Ceftriaxone** is an antibiotic used to treat bacterial infections.
- There is no clinical evidence in the stem (e.g., fever, signs of infection) to suggest a **bacterial infection** as the cause of her symptoms, making antibiotics inappropriate.
*Discontinue cyclosporine*
- **Cyclosporine** is an immunosuppressant essential for preventing transplant rejection. Discontinuing it would immediately increase the risk of more severe and potentially **irreversible rejection**.
- While cyclosporine can cause nephrotoxicity, the biopsy findings of **cellular infiltration** point more towards rejection rather than primary drug toxicity, and the primary treatment for rejection involves increasing immunosuppression, not withdrawing it.
Rapidly progressive glomerulonephritis US Medical PG Question 6: A 67-year-old man comes to the emergency department for evaluation of progressively worsening edema and decreased urine output over the past few days. He has a history of chronic sinus infections and was hospitalized last year for a suspected pneumonia with hemoptysis. Physical exam shows bilateral pitting edema of the lower extremities. Serum studies show a creatinine of 3.4 mg/dL and blood urea nitrogen of 35 mg/dL. Urine dipstick shows 3+ blood. A kidney biopsy is performed and light microscopy shows crescent-shaped glomeruli. Immunofluorescent microscopy of the tissue sample is most likely to show which of the following findings?
- A. Subendothelial deposits
- B. Mesangial deposits
- C. Intramembranous deposits
- D. No deposits (Correct Answer)
- E. Subepithelial deposits
Rapidly progressive glomerulonephritis Explanation: ***No deposits***
- The presence of **crescentic glomeruli** on light microscopy and a history of chronic sinus infections and hemoptysis strongly suggest **Granulomatosis with Polyangiitis (GPA)**, a form of **pauci-immune glomerulonephritis**.
- In pauci-immune glomerulonephritis, immunofluorescence typically shows **scanty or no immune deposits** in the glomeruli.
*Subendothelial deposits*
- **Subendothelial deposits** are characteristic of conditions like **membranoproliferative glomerulonephritis** (types I and III) or **lupus nephritis**, which typically do not present with the described clinical picture of chronic upper respiratory issues and hemoptysis.
- These deposits would be associated with significant immune complex deposition, which contradicts the "pauci-immune" nature suggested by the clinical presentation.
*Mesangial deposits*
- **Mesangial deposits** are a hallmark of **IgA nephropathy** or early stages of lupus nephritis, where IgA or other immune complexes accumulate in the mesangium.
- While IgA nephropathy can cause hematuria, the crescentic glomerulonephritis and systemic features (sinusitis, hemoptysis) point away from isolated mesangial involvement as the primary pathology.
*Intramembranous deposits*
- **Intramembranous deposits** are typically seen in conditions like **dense deposit disease** (a complement-mediated glomerulonephritis) or some forms of cryoglobulinemic glomerulonephritis.
- These conditions usually have distinct clinical presentations and specific patterns of complement activation or cryoglobulinemia, which are not indicated in this case.
*Subepithelial deposits*
- **Subepithelial deposits** (e.g., "humps") are characteristic of **post-streptococcal glomerulonephritis** and are rich in C3 and IgG.
- While post-streptococcal glomerulonephritis can cause crescent formation, the patient's age, chronic sinus issues, and hemoptysis make GPA a more fitting diagnosis.
Rapidly progressive glomerulonephritis US Medical PG Question 7: A 49-year-old female with a long history of poorly controlled diabetes mellitus visits her primary care physician with 2+ non-pitting edema in her legs. The patient has a serum creatinine of 2.9 mg/dL and a blood urea nitrogen of 61 mg/dL. A 24-hour urine collection reveals 8.5 grams of protein. A renal biopsy is obtained. Which of the following histologic findings is most likely to be seen upon tissue analysis:
- A. Normal glomeruli
- B. Crescentic proliferation in Bowman’s space
- C. Nodular thickening of the glomerular basement membrane (Correct Answer)
- D. Lymphocytic infiltration of glomerular tufts
- E. Non-caseating interstitial granuloma
Rapidly progressive glomerulonephritis Explanation: ***Nodular thickening of the glomerular basement membrane***
- The patient's history of **poorly controlled diabetes**, **nephrotic range proteinuria** (8.5 grams/24 hours), elevated creatinine, and BUN are highly suggestive of **diabetic nephropathy**.
- **Kimmelstiel-Wilson lesions**, characterized by **nodular thickening of the glomerular basement membrane** due to deposition of mesangial matrix, are pathognomonic for diabetic nephropathy.
*Normal glomeruli*
- The presence of **severe proteinuria** (8.5g/24h) and **renal insufficiency** (creatinine 2.9 mg/dL, BUN 61 mg/dL) indicates significant renal damage, making perfectly normal glomeruli highly unlikely.
- These clinical findings directly contradict a diagnosis of normal glomerular function.
*Crescentic proliferation in Bowman’s space*
- **Crescentic proliferation**, which is characterized by the accumulation of cells (macrophages, epithelial cells) in Bowman's space, is typical of rapidly progressive glomerulonephritis (RPGN).
- While RPGN can cause renal failure, it's not the primary or most characteristic finding in the context of long-standing, poorly controlled diabetes with nephrotic-range proteinuria.
*Lymphocytic infiltration of glomerular tufts*
- **Lymphocytic infiltration of glomerular tufts** is observed in certain forms of glomerulonephritis, such as lupus nephritis or some immune complex-mediated diseases.
- This finding is not characteristic of diabetic nephropathy, which primarily involves structural changes to the glomerular basement membrane and mesangium.
*Non-caseating interstitial granuloma*
- **Non-caseating granulomas** in the kidney are a hallmark of **sarcoidosis**, an inflammatory disease that can affect various organs, including the kidneys.
- While sarcoidosis can cause renal dysfunction, it does not typically present with the specific combination of long-standing diabetes and massive proteinuria described in this case, nor is it histologically characterized by nodular glomerular changes.
Rapidly progressive glomerulonephritis US Medical PG Question 8: A 12-year-old boy comes to the physician for the evaluation of intermittent blood-tinged urine for several months. Four months ago, he had an episode of fever and sore throat that resolved without treatment after 5 days. During the past 2 years, he has also had recurrent episodes of swelling of his face and feet. 5 years ago, he was diagnosed with mild bilateral sensorineural hearing loss. His brother died of a progressive kidney disease at the age of 23. The patient appears pale. His temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 145/85 mm Hg. Slit lamp examination shows a conical protrusion of both lenses. Laboratory studies show a hemoglobin concentration of 11 g/dL, urea nitrogen concentration of 40 mg/dL, and creatinine concentration of 2.4 mg/dL. Urinalysis shows:
Blood 2+
Protein 1+
RBC 5–7/hpf
RBC casts rare
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. IgA deposits
- B. WT1 gene mutation
- C. Defective type IV collagen (Correct Answer)
- D. Autosomal-recessive kidney disease
- E. Type II hypersensitivity reaction
Rapidly progressive glomerulonephritis Explanation: ***Defective type IV collagen***
- This patient presents with a classic triad of symptoms: **progressive kidney disease** (elevated creatinine, blood-tinged urine, family history), **sensorineural hearing loss**, and **ocular abnormalities** (lenticonus on slit lamp exam). These findings are highly suggestive of **Alport syndrome**, which is caused by a defect in **type IV collagen**.
- The family history of a brother dying of progressive kidney disease at a young age further supports a genetic cause, and the intermittent blood-tinged urine after an upper respiratory infection can be a feature of Alport syndrome, often misinterpreted as IgA nephropathy early in its course.
*IgA deposits*
- **IgA nephropathy** can present with recurrent episodes of gross hematuria, often following an upper respiratory infection, similar to the initial presentation of this patient's blood-tinged urine.
- However, IgA nephropathy typically does not involve **sensorineural hearing loss** or **ocular abnormalities** like lenticonus.
*WT1 gene mutation*
- A **WT1 gene mutation** is associated with **Denys-Drash syndrome** and **Frasier syndrome**, which involve nephropathy and, in some cases, gonadal abnormalities or ambiguous genitalia.
- While these can cause kidney disease, they do not typically present with the characteristic ocular findings (lenticonus) or sensorineural hearing loss seen in this patient.
*Autosomal-recessive kidney disease*
- While Alport syndrome can have autosomal recessive inheritance (10-15% of cases), this option is too broad and does not specify the underlying **molecular defect** (type IV collagen).
- The family history pattern here (affected brother, male proband) is more consistent with **X-linked Alport syndrome** (85% of cases), and this non-specific option does not pinpoint the actual pathogenic mechanism that links all the patient's symptoms.
*Type II hypersensitivity reaction*
- A **type II hypersensitivity reaction** involves antibody-mediated cellular destruction or dysfunction, such as in Goodpasture syndrome, where antibodies attack the glomerular basement membrane.
- This mechanism does not explain the long-standing, progressive nature of kidney disease combined with sensorineural hearing loss and ocular defects. Instead, these are characteristic of an underlying structural protein defect.
Rapidly progressive glomerulonephritis US Medical PG Question 9: A 12-year-old boy presents to your office with facial swelling and dark urine. He has no other complaints other than a sore throat 3 weeks ago that resolved after 6 days. He is otherwise healthy, lives at home with his mother and 2 cats, has no recent history of travel, and no sick contacts. On physical examination his temperature is 99°F (37.2°C), blood pressure is 130/85 mmHg, pulse is 80/min, respirations are 19/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal examinations are unremarkable. There is mild periorbital and pedal edema. Urinalysis shows 12-15 RBC/hpf, 2-5 WBC/hpf, and 30 mg/dL protein. Which additional finding would you expect to see on urinalysis?
- A. Fatty casts
- B. RBC casts (Correct Answer)
- C. WBC casts
- D. Granular casts
- E. Hyaline casts
Rapidly progressive glomerulonephritis Explanation: ***RBC casts***
- The patient's presentation with **facial swelling**, **dark urine**, and a history of a recent **sore throat** points toward **post-streptococcal glomerulonephritis (PSGN)**.
- **RBC casts** are a hallmark microscopic finding in **glomerulonephritis**, indicating **glomerular inflammation** and bleeding.
*Fatty casts*
- **Fatty casts** are characteristic of **nephrotic syndrome**, which primarily involves heavy proteinuria and generalized edema.
- While there is some proteinuria and edema, the dark urine and history of recent infection are more consistent with nephritic syndrome.
*Hyaline casts*
- **Hyaline casts** are composed of Tamm-Horsfall proteins and can be found in healthy individuals, or in conditions like **dehydration** or **fever**.
- They are a non-specific finding and do not indicate specific renal pathology like glomerulonephritis.
*WBC casts*
- **WBC casts** are typically seen in **pyelonephritis** (kidney infection) or **interstitial nephritis**, indicating inflammation within the renal tubules.
- The patient's primary symptoms and lab findings are more consistent with glomerular disease rather than an infection of the renal parenchyma.
*Granular casts*
- **Granular casts** are formed from degenerated cellular casts or protein aggregates and are often seen in **acute tubular necrosis (ATN)** or **chronic kidney disease**.
- While they suggest renal parenchymal injury, they are not as specific for glomerulonephritis as RBC casts, especially in a subacute presentation like this.
Rapidly progressive glomerulonephritis US Medical PG Question 10: A 13-year-old boy is brought to the physician because of swelling around his eyes for the past 2 days. His mother also notes that his urine became gradually darker during this time. Three weeks ago, he was treated for bacterial tonsillitis. His temperature is 37.6°C (99.7°F), pulse is 79/min, and blood pressure is 158/87 mm Hg. Examination shows periorbital swelling. Laboratory studies show:
Serum
Urea nitrogen 9 mg/dL
Creatinine 1.7 mg/dL
Urine
Protein 2+
RBC 12/hpf
RBC casts numerous
A renal biopsy would most likely show which of the following findings?
- A. Effacement of podocyte foot processes on electron microscopy
- B. Granular deposits of IgG, IgM, and C3 on immunofluorescence (Correct Answer)
- C. Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy
- D. Mesangial IgA deposits on immunofluorescence
- E. "Spike-and-dome" appearance of subepithelial deposits on electron microscopy
Rapidly progressive glomerulonephritis Explanation: ***Granular deposits of IgG, IgM, and C3 on immunofluorescence***
- This finding is characteristic of **post-streptococcal glomerulonephritis (PSGN)**, supported by the history of recent tonsillitis, periorbital swelling, dark urine, hypertension, and features of nephritic syndrome (RBC casts, proteinuria).
- The granular deposition pattern reflects the immune complex-mediated nature of PSGN, where **antigen-antibody complexes** deposit in the glomeruli.
*Effacement of podocyte foot processes on electron microscopy*
- This is the hallmark finding in **minimal change disease**, which typically presents with abrupt onset of nephrotic syndrome (severe proteinuria, hypoalbuminemia, edema) without hematuria or hypertension.
- The patient's presentation with **dark urine** (hematuria), hypertension, and RBC casts is inconsistent with minimal change disease.
*Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy*
- This describes the characteristic changes seen in **Alport syndrome**, an inherited disorder affecting collagen IV.
- Alport syndrome presents with **hematuria**, progressive renal failure, and often includes hearing loss and ocular abnormalities, which are not mentioned in this acute presentation.
*Mesangial IgA deposits on immunofluorescence*
- This is the diagnostic feature of **IgA nephropathy (Berger's disease)**.
- IgA nephropathy often presents with **recurrent macroscopic hematuria** occurring concurrent with or shortly after an upper respiratory infection, rather than 2-3 weeks later like PSGN.
*"Spike-and-dome" appearance of subepithelial deposits on electron microscopy*
- This appearance is characteristic of **membranous nephropathy**, which is a common cause of **nephrotic syndrome** in adults.
- Membranous nephropathy typically presents with significant proteinuria and edema, and it is less common in children with acute nephritic symptoms like those described.
More Rapidly progressive glomerulonephritis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.