Pyelonephritis and urinary tract infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pyelonephritis and urinary tract infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pyelonephritis and urinary tract infections US Medical PG Question 1: A 62-year-old man comes to the physician because of a 2-day history of fever, chills, and flank pain. Five days ago, he was catheterized for acute urinary retention. His temperature is 39.3°C (102.7°F). Physical examination shows right-sided costovertebral angle tenderness. Urine studies show numerous bacteria and WBC casts. Urine culture on blood agar grows mucoid, gray-white colonies. Urine culture on eosin methylene blue agar grows purple colonies with no metallic green sheen. Which of the following is the most likely causal pathogen?
- A. Escherichia coli
- B. Klebsiella pneumoniae (Correct Answer)
- C. Pseudomonas aeruginosa
- D. Proteus mirabilis
- E. Staphylococcus saprophyticus
Pyelonephritis and urinary tract infections Explanation: ***Klebsiella pneumoniae***
- The presence of **mucoid, gray-white colonies** on blood agar and **purple colonies with no metallic green sheen** on EMB agar, along with a history of catheterization, fever, and flank pain strongly suggests *Klebsiella pneumoniae*.
- *Klebsiella* is a common cause of **catheter-associated UTIs** and often produces mucoid colonies due to its capsule.
*Escherichia coli*
- *E. coli* typically produces **metallic green sheen** on EMB agar due to rapid lactose fermentation, which is absent in this case.
- While *E. coli* is a common cause of UTIs, the specific culture findings differentiate it from *Klebsiella*.
*Pseudomonas aeruginosa*
- *Pseudomonas* often produces a **grape-like odor** and distinctive **blue-green pigment** on agar, neither of which is mentioned.
- It does not ferment lactose and would thus not produce purple colonies on EMB, but rather appear as colorless or clear colonies.
*Proteus mirabilis*
- *Proteus mirabilis* is known for its **swarming motility** on agar, which creates a characteristic spreading growth pattern, not merely mucoid colonies.
- It also produces **urease**, which can lead to alkaline urine and struvite stones, but the distinguishing colony morphology is not met.
*Staphylococcus saprophyticus*
- *Staphylococcus saprophyticus* is a **Gram-positive coccus** and would not grow purple colonies on EMB agar, which is selective for Gram-negative bacteria.
- It is a common cause of UTIs in young, sexually active women, which does not fit the patient's demographic.
Pyelonephritis and urinary tract infections US Medical PG Question 2: A 28-year-old woman comes to the physician because of a 4-day history of lower abdominal pain and pain with urination. Five months ago, she was treated for gonococcal urethritis. She recently moved in with her newlywed husband. She is sexually active with her husband and they do not use condoms. Her only medication is an oral contraceptive. Her temperature is 37.5°C (99.7°F) and blood pressure is 120/74 mm Hg. There is tenderness to palpation over the pelvic region. Pelvic examination shows a normal-appearing vulva and vagina. Laboratory studies show:
Leukocyte count 8,400/mm3
Urine
pH 6.7
Protein trace
WBC 60/hpf
Nitrites positive
Bacteria positive
Which of the following is the most likely causal organism?
- A. Enterococcus faecalis
- B. Klebsiella pneumoniae
- C. Neisseria gonorrhoeae
- D. Escherichia coli (Correct Answer)
- E. Staphylococcus saprophyticus
Pyelonephritis and urinary tract infections Explanation: ***Escherichia coli***
- The presence of **nitrites** in the urine analysis strongly suggests a urinary tract infection caused by a **nitrate-reducing bacterium**, such as *E. coli*.
- *E. coli* is the **most common cause of uncomplicated UTIs**, especially in sexually active women, and the symptoms (lower abdominal pain, dysuria, pyuria, bacteriuria) are classic for a UTI.
*Enterococcus faecalis*
- While *Enterococcus faecalis* can cause UTIs, it is **less common** than *E. coli* in uncomplicated cases and typically **does not produce nitrites** in urine due to lacking nitrate reductase.
- It is more commonly associated with UTIs in hospitalized patients or those with urinary tract abnormalities.
*Klebsiella pneumoniae*
- *Klebsiella pneumoniae* can cause UTIs and is a **nitrite-producing bacterium**, but it is a **less frequent cause** of community-acquired uncomplicated UTIs compared to *E. coli*.
- It is more often associated with healthcare-associated infections or UTIs in compromised hosts.
*Neisseria gonorrhoeae*
- While the patient has a history of gonococcal urethritis, current symptoms are more consistent with a UTI, and *Neisseria gonorrhoeae* is a **rare cause of cystitis** or pyelonephritis.
- Gonorrhea primarily causes urethritis, cervicitis, or pelvic inflammatory disease, and **does not typically produce nitrites** from nitrates in urine.
*Staphylococcus saprophyticus*
- *Staphylococcus saprophyticus* is a common cause of UTIs in young, sexually active women, but it is **nitrite-negative** because it does not possess nitrate reductase.
- The positive nitrites in the urine make *E. coli* a more likely culprit in this case.
Pyelonephritis and urinary tract infections US Medical PG Question 3: A 62-year-old man comes to the physician because of an oozing skin ulceration on his foot for 1 week. He has a history of type 2 diabetes mellitus and does not adhere to his medication regimen. Physical exam shows purulent discharge from an ulcer on the dorsum of his left foot. Pinprick sensation is decreased bilaterally to the level of the mid-tibia. A culture of the wound grows beta-hemolytic, coagulase-positive cocci in clusters. The causal organism most likely produces which of the following virulence factors?
- A. Exotoxin A
- B. M protein
- C. P fimbriae
- D. IgA protease
- E. Protein A (Correct Answer)
Pyelonephritis and urinary tract infections Explanation: ***Protein A***
- The culture finding of **beta-hemolytic, coagulase-positive cocci in clusters** is characteristic of ***Staphylococcus aureus***.
- ***Staphylococcus aureus*** produces **Protein A**, which binds to the Fc region of IgG, preventing opsonization and phagocytosis, thereby hindering the immune response.
*Exotoxin A*
- **Exotoxin A** is a virulence factor primarily produced by ***Pseudomonas aeruginosa***, particularly associated with deep tissue infections and sepsis.
- It functions as an **ADP-ribosylating toxin** that inhibits protein synthesis, but it is not characteristic of the organism isolated in this patient.
*M protein*
- **M protein** is a key virulence factor of ***Streptococcus pyogenes*** (Group A Streptococcus), responsible for preventing phagocytosis and promoting adhesion.
- ***S. pyogenes*** is beta-hemolytic but typically grows in **chains**, not clusters, and is **coagulase-negative**.
*P fimbriae*
- **P fimbriae** (pyelonephritis-associated pilus) are virulence factors predominantly found in uropathogenic strains of ***Escherichia coli***, mediating adhesion to uroepithelial cells.
- These fimbriae are associated with urinary tract infections, not typically with skin ulcers from **Gram-positive cocci in clusters**.
*IgA protease*
- **IgA protease** is a virulence factor produced by several pathogenic bacteria such as ***Neisseria gonorrhoeae***, ***Haemophilus influenzae***, and ***Streptococcus pneumoniae***.
- It cleaves IgA at hinge regions, allowing the bacteria to evade mucosal immunity, but it is not a primary virulence factor of ***Staphylococcus aureus*** or commonly associated with skin ulcers.
Pyelonephritis and urinary tract infections US Medical PG Question 4: A 26-year-old female presents to her primary care physician concerned that she has contracted a sexually transmitted disease. She states that she is having severe pain whenever she urinates and seems to be urinating more frequently than normal. She reports that her symptoms started after she began having unprotected sexual intercourse with 1 partner earlier this week. The physician obtains a urinalysis which demonstrates the following, SG: 1.010, Leukocyte esterase: Positive, Nitrites: Positive, Protein: Trace, pH: 5.0, RBC: Negative. A urease test is performed which is negative. This patient has most likely been infected with which of the following organisms?
- A. Enterobacter cloacae
- B. Staphylococcus saprophyticus
- C. Proteus mirabilis
- D. Klebsiella pneumoniae
- E. Escherichia coli (Correct Answer)
Pyelonephritis and urinary tract infections Explanation: ***Escherichia coli***
- The urinalysis findings of **positive leukocyte esterase**, **nitrites**, and **trace protein** with a slightly acidic pH (5.0) are highly suggestive of a **urinary tract infection (UTI)**.
- *E. coli* is the most common cause of UTIs, especially in young, sexually active women, and is typically **urease-negative**, consistent with the information provided.
- *E. coli* accounts for **80-90% of uncomplicated UTIs** and produces nitrites from dietary nitrates, making it the most likely pathogen in this clinical scenario.
*Enterobacter cloacae*
- While *Enterobacter cloacae* can cause UTIs, it is less common than *E. coli* in uncomplicated cases and is often associated with nosocomial infections or those in immunocompromised individuals.
- Its urease activity can vary, so a negative urease test doesn't rule it out completely but makes *E. coli* a more likely primary choice in this context.
*Staphylococcus saprophyticus*
- *S. saprophyticus* is a common cause of UTIs in young, sexually active women (second most common cause after *E. coli*) and is typically **urease-negative**, which is consistent with the negative test.
- However, the presence of **positive nitrites** points more strongly towards **Gram-negative bacteria** like *E. coli*, as *S. saprophyticus* is a **Gram-positive coccus** that does not produce nitrite reductase and therefore does not convert nitrates to nitrites.
*Proteus mirabilis*
- *Proteus mirabilis* is known for causing UTIs and is characteristically **urease-positive**, leading to alkaline urine (higher pH) and sometimes **struvite stones**.
- The **negative urease test** and acidic urine pH (5.0) in this case effectively rule out *Proteus mirabilis*.
*Klebsiella pneumoniae*
- *Klebsiella pneumoniae* can cause UTIs and is generally **urease-negative**, but it is less frequently the cause of uncomplicated UTIs compared to *E. coli*.
- Although it can produce nitrites, *E. coli* remains the most common etiology in this clinical scenario.
Pyelonephritis and urinary tract infections US Medical PG Question 5: An autopsy is being performed on an elderly man who died from a myocardial infarction. Biopsy of the heart is likely to reveal necrosis most similar to necrosis seen in which of the following scenarios?
- A. The central nervous system following a stroke
- B. An abscess
- C. The lung following a tuberculosis infection
- D. A region of kidney where blood flow is obstructed (Correct Answer)
- E. Acute pancreatitis resulting from release of enzymatically active enzymes into the pancreas
Pyelonephritis and urinary tract infections Explanation: ***A region of kidney where blood flow is obstructed***
- Myocardial infarction leads to **coagulative necrosis**, characterized by the preservation of the cell's outline but with loss of nuclei, often due to **ischemia**.
- **Kidney infarction** also results from obstructed blood flow, causing ischemia and subsequent **coagulative necrosis**, making it histologically similar to a myocardial infarction.
*The central nervous system following a stroke*
- A stroke typically causes **liquefactive necrosis** in the central nervous system, due to the high lipid content and enzymatic digestion of dead cells.
- This type of necrosis leads to the formation of a **cystic space** rather than the preserved architecture seen in coagulative necrosis.
*An abscess*
- An abscess is characterized by **liquefactive necrosis** due to a bacterial infection, involving the accumulation of pus (dead neutrophils and tissue debris).
- The inflammatory response and enzymatic digestion distinguish it from the preserved tissue architecture of coagulative necrosis.
*The lung following a tuberculosis infection*
- Tuberculosis infection typically causes **caseous necrosis** in the lung, which is a combination of coagulative and liquefactive necrosis.
- This appears as **cheesy, amorphous material** grossly, and histologically lacks the clear cell outlines of coagulative necrosis.
*Acute pancreatitis resulting from release of enzymatically active enzymes into the pancreas*
- Acute pancreatitis leads to **fat necrosis**, where pancreatic enzymes (lipase) digest adipose tissue, often forming **chalky white deposits** due to calcium saponification.
- This is distinct from coagulative necrosis, as it specifically targets fat tissue and involves enzymatic destruction rather than ischemic cell death.
Pyelonephritis and urinary tract infections US Medical PG Question 6: A 47-year-old woman with a long history of poorly controlled type 2 diabetes and recurrent urinary tract infections presents with complaints of fever, chills, and severe flank pain. On physical exam, she has left-sided costovertebral tenderness. Vitals include a temperature of 39.4°C (103.0°F), blood pressure of 125/84 mm Hg, and pulse of 84/min. She is currently taking metformin daily. Urine dipstick analysis is positive for leukocytes, nitrites, and blood. Laboratory studies show an elevated creatinine of 2.8 mg/dL (baseline 1.0 mg/dL). Urinalysis reveals fragments of tissue. What is the most likely diagnosis?
- A. Acute cystitis
- B. Acute glomerulonephritis
- C. Acute tubular necrosis
- D. Acute interstitial nephritis
- E. Acute papillary necrosis (Correct Answer)
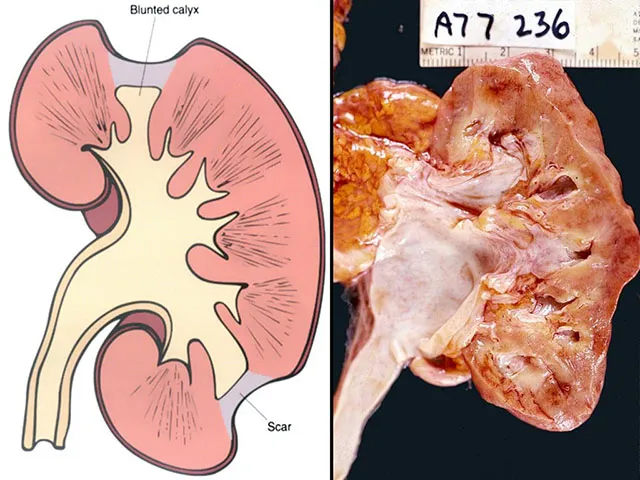
Pyelonephritis and urinary tract infections Explanation: ***Acute papillary necrosis***
- This patient's presentation with **fever, severe flank pain, costovertebral tenderness**, **elevated creatinine indicating acute kidney injury**, and **tissue fragments in urine** is classic for **acute papillary necrosis**.
- Her **poorly controlled type 2 diabetes** and **recurrent UTIs** are major risk factors. Chronic hyperglycemia causes **renal medullary ischemia**, and recurrent infections further compromise blood supply to the renal papillae.
- The **tissue fragments** represent sloughed papillae, a pathognomonic finding. The combination of **hematuria, acute kidney injury, and systemic symptoms** in a diabetic with recurrent infections strongly points to this diagnosis.
- Other risk factors include analgesic abuse, sickle cell disease, and urinary tract obstruction.
*Acute cystitis*
- **Acute cystitis** presents with **dysuria, frequency, and urgency** but typically **without fever, systemic symptoms, or costovertebral tenderness**.
- It does not cause **acute kidney injury** or **tissue fragments in urine**.
- The severe presentation with AKI and CVA tenderness indicates upper urinary tract pathology.
*Acute glomerulonephritis*
- **Acute glomerulonephritis** presents with **hematuria, proteinuria, hypertension, and edema**, often following streptococcal infection.
- It does not typically cause **fever, severe flank pain, or CVA tenderness**.
- The presence of **nitrites** and **tissue fragments** points to bacterial infection with tissue necrosis, not glomerular inflammation.
*Acute tubular necrosis*
- **Acute tubular necrosis (ATN)** causes acute kidney injury but typically follows **ischemic insult** (hypotension, surgery) or **nephrotoxic exposure** (aminoglycosides, contrast).
- ATN does not present with **fever, chills, severe flank pain, or tissue fragments in urine**.
- Urinalysis in ATN shows muddy brown casts, not tissue fragments with nitrites.
*Acute interstitial nephritis*
- **Acute interstitial nephritis (AIN)** is typically a **drug-induced hypersensitivity reaction** presenting with **fever, rash, eosinophilia**, and AKI.
- The classic triad is fever, rash, and eosinophilia, often occurring days to weeks after drug exposure.
- **Nitrites** (indicating bacterial infection) and **tissue fragments** are not consistent with AIN, which shows sterile pyuria and white blood cell casts.
Pyelonephritis and urinary tract infections US Medical PG Question 7: A 34-year-old female presents to her primary care physician with complaints of fevers, nausea/vomiting, and severe left flank pain that has developed over the past several hours. She denies any prior episodes similar to her current presentation. Physical examination is significant for a body temperature of 39.1 C and costovertebral angle tenderness. A urinalysis and urine microscopy are ordered. Which of the following findings on kidney histology would be expected in this patient?
- A. Enlarged, hypercellular glomeruli with 'wire-looping' of capillaries
- B. Neutrophils filling the lumens of the renal tubules (Correct Answer)
- C. Scarring of the glomeruli
- D. Interstitial fibrosis and lymphocytic infiltrate
- E. Thickening of the capillaries and glomerular basement membrane
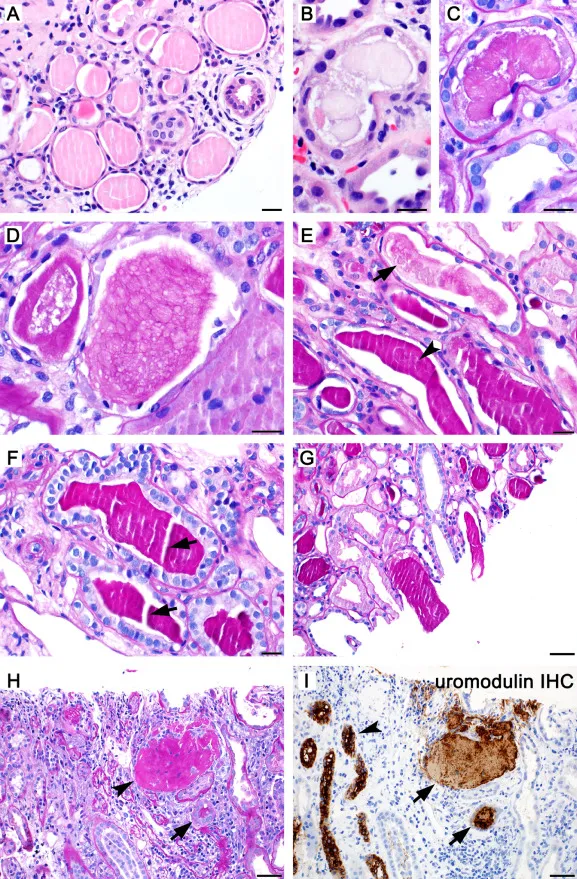
Pyelonephritis and urinary tract infections Explanation: ***Neutrophils filling the lumens of the renal tubules***
- This patient's symptoms (fevers, nausea/vomiting, severe left flank pain, fever, and costovertebral angle tenderness) are highly suggestive of **acute pyelonephritis**, an infection of the kidney parenchyma.
- Histologically, acute pyelonephritis is characterized by an acute inflammatory infiltrate, primarily **neutrophils**, within the **renal tubules** and interstitial tissue, often forming **abscesses**.
*Enlarged, hypercellular glomeruli with 'wire-looping' of capillaries*
- This description is characteristic of **diffuse proliferative glomerulonephritis**, often associated with conditions like **systemic lupus erythematosus (SLE)**.
- The clinical presentation of sudden-onset severe flank pain and fever is not typical for glomerulonephritis, which usually presents with hematuria, proteinuria, and edema.
*Scarring of the glomeruli*
- **Glomerulosclerosis** (scarring of the glomeruli) is a feature of chronic kidney disease and various chronic glomerular disorders, not acute pyelonephritis.
- Patients with glomerular scarring typically present with signs of chronic kidney injury, such as persistent proteinuria and declining renal function, rather than acute infectious symptoms.
*Interstitial fibrosis and lymphocytic infiltrate*
- This is a hallmark of **chronic interstitial nephritis**, which can be caused by long-term drug use, autoimmune diseases, or chronic obstructive uropathy.
- While lymphocytes indicate inflammation, the presence of fibrosis suggests a chronic process, differing from the acute bacterial infection seen in pyelonephritis.
*Thickening of the capillaries and glomerular basement membrane*
- This finding is suggestive of various glomerular diseases, such as **membranous nephropathy** or **diabetic nephropathy**, where the glomerular basement membrane is significantly altered.
- Such conditions typically manifest with proteinuria and nephrotic or nephritic syndromes, not the acute infectious symptoms described.
Pyelonephritis and urinary tract infections US Medical PG Question 8: A 48-year-old man comes to the emergency department because of a 2-hour history of severe left-sided colicky flank pain that radiates towards his groin. He has vomited twice. Last year, he was treated with ibuprofen for swelling and pain of his left toe. He drinks 4-5 beers most days of the week. Examination shows left costovertebral angle tenderness. An upright x-ray of the abdomen shows no abnormalities. A CT scan of the abdomen and pelvis shows an 9-mm stone in the proximal ureter on the left. Which of the following is most likely to be seen on urinalysis?
- A. Rhomboid-shaped crystals
- B. Coffin-lid-like crystals
- C. Red blood cell casts
- D. Wedge-shaped crystals (Correct Answer)
- E. Hexagon-shaped crystals
Pyelonephritis and urinary tract infections Explanation: ***Wedge-shaped crystals***
- The patient's history of **left toe swelling and pain** (suggestive of **gout**) and **alcohol consumption** strongly indicate **hyperuricemia** and predisposition to **uric acid stone** formation.
- **Uric acid stones are radiolucent**, which explains why the **X-ray showed no abnormalities** despite a 9-mm stone being visible on CT scan—this is a classic presentation.
- **Uric acid crystals** appear as **wedge-shaped, rhomboid, or pleomorphic** yellow-brown crystals in **acidic urine** (pH <5.5).
- This is the most likely finding on urinalysis given the clinical context.
*Rhomboid-shaped crystals*
- **Rhomboid-shaped crystals** are also characteristic of **uric acid**, making this another acceptable description of the same crystal type.
- Both "wedge-shaped" and "rhomboid" refer to **uric acid crystals**; however, "wedge-shaped" is the more commonly used descriptor in clinical practice.
- If this were an option and wedge-shaped were not available, it would also be correct, but wedge-shaped is the better answer when both are present.
*Coffin-lid-like crystals*
- **Coffin-lid crystals** are characteristic of **struvite stones** (magnesium ammonium phosphate), which form in **alkaline urine** (pH >7) and are associated with **urease-producing bacteria** (e.g., Proteus, Klebsiella).
- Struvite stones are **radiopaque** and would be visible on X-ray, which contradicts this presentation.
- The patient has no signs of urinary tract infection.
*Red blood cell casts*
- **RBC casts** indicate **glomerular bleeding** and are seen in conditions like **glomerulonephritis**, not obstructive uropathy from stones.
- While **hematuria** (RBCs in urine) is common with nephrolithiasis, **RBC casts** are not typical and would suggest primary renal parenchymal disease.
*Hexagon-shaped crystals*
- **Hexagonal crystals** are pathognomonic for **cystine stones**, which occur in **cystinuria**, a rare autosomal recessive disorder of amino acid transport.
- Cystine stones are **weakly radiopaque** and would show faint opacity on X-ray.
- This condition typically presents in childhood or young adulthood, not at age 48, and has no association with gout.
Pyelonephritis and urinary tract infections US Medical PG Question 9: A 22-month-old girl is brought to the emergency department with a 24-hour history of fever, irritability, and poor feeding. The patient never experienced such an episode in the past. She met the normal developmental milestones, and her vaccination history is up-to-date. She takes no medications, currently. Her temperature is 38.9°C (102.0°F). An abdominal examination reveals general tenderness without organomegaly. The remainder of the physical examination shows no abnormalities. Laboratory studies show the following results:
Urine
Blood 1+
WBC 10–15/hpf
Bacteria Many
Nitrite Positive
Urine culture from a midstream collection reveals 100,000 CFU/mL of Escherichia coli. Which of the following interventions is the most appropriate next step in evaluation?
- A. No further testing
- B. Voiding cystourethrography
- C. Renal and bladder ultrasonography (Correct Answer)
- D. Intravenous pyelography
- E. Dimercaptosuccinic acid renal scan
Pyelonephritis and urinary tract infections Explanation: ***Renal and bladder ultrasonography***
- For a febrile infant or young child (2 to 24 months) with a first **culture-proven urinary tract infection (UTI)**, renal and bladder ultrasonography is the recommended imaging study.
- This imaging is crucial to evaluate for **anatomic abnormalities** of the kidneys and urinary tract that could predispose to recurrent infections or renal damage.
- Current AAP guidelines recommend ultrasound as the **initial imaging modality** to assess for conditions like vesicoureteral reflux (VUR), hydronephrosis, or obstructive uropathy.
*No further testing*
- This option is incorrect because a **febrile UTI** in a young child warrants imaging to rule out **underlying genitourinary abnormalities** that could predispose to recurrent infections or renal damage.
- Skipping further evaluation could miss conditions like **vesicoureteral reflux (VUR)** or obstructive uropathy.
*Voiding cystourethrography*
- **Voiding cystourethrography (VCUG)** was historically recommended for all young children after a first UTI but is now reserved for specific situations, such as **abnormal renal/bladder ultrasound findings** or recurrent UTIs.
- VCUG involves radiation exposure and catheterization, making it less favorable as a first-line imaging study.
*Intravenous pyelography*
- **Intravenous pyelography (IVP)** involves intravenous contrast and radiation, making it an **invasive and high-radiation study** that has largely been replaced by ultrasound and CT for evaluating the urinary tract.
- It is not recommended as the initial imaging of choice for a child with a first UTI due to its **risks and availability of safer alternatives**.
*Dimercaptosuccinic acid renal scan*
- A **dimercaptosuccinic acid (DMSA) renal scan** is primarily used to detect **renal scarring** and assesses differential renal function.
- While it can be useful in identifying long-term consequences of UTIs, it is not the primary imaging study for initial evaluation of **ureteral or bladder abnormalities** in a first febrile UTI.
Pyelonephritis and urinary tract infections US Medical PG Question 10: A 12-year-old girl is brought to the physician by her mother because she has been waking up multiple times at night to go to the bathroom even though she avoids drinking large amounts of water close to bedtime. She has no significant medical history apart from 3 episodes of lower urinary tract infections treated with nitrofurantoin in the past 2 years. Her family emigrated from Nigeria 10 years ago. Physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 14.2 g/dL
MCV 92 fL
Reticulocytes 1.5%
Serum
Osmolality 290 mOsmol/kg H2O
Urine
Leukocytes negative
Nitrite negative
Glucose negative
Osmolality 130 mOsmol/kg H2O
Hemoglobin electrophoresis shows:
HbA 56%
HbS 43%
HbF 1%
This patient is at greatest risk for which of the following conditions?
- A. Transient arrest of erythropoiesis
- B. Necrosis of the renal papillae (Correct Answer)
- C. Sickling in the cerebral vessels
- D. Autoinfarction of the spleen
- E. Pigment stones in the biliary tract
Pyelonephritis and urinary tract infections Explanation: ***Necrosis of the renal papillae***
- This patient has **sickle cell trait (HbAS)**, indicated by HbA 56% and HbS 43%. Individuals with sickle cell trait are particularly susceptible to **renal papillary necrosis** due to sickling in the renal medulla, which is a hypoxic and hyperosmolar environment.
- The symptoms of **nocturia** and **polyuria** (frequent nighttime urination despite avoiding fluids) along with a **low urine osmolality** (130 mOsmol/kg H2O) despite normal serum osmolality (290 mOsmol/kg H2O) suggest impaired concentrating ability of the kidneys, a common finding in early renal damage associated with sickle cell trait.
*Transient arrest of erythropoiesis*
- **Transient aplastic crisis** or erythropoiesis arrest is primarily associated with **sickle cell disease (HbSS)**, often triggered by parvovirus B19 infection, leading to a precipitous drop in hemoglobin.
- This patient's hemoglobin is within the normal range, and her reticulocyte count is not suggestive of acute aplasia.
*Sickling in the cerebral vessels*
- **Cerebral vessel sickling** leading to stroke is a severe complication predominantly associated with **homozygous sickle cell disease (HbSS)**, where a much higher percentage of HbS leads to widespread vaso-occlusive crises.
- While individuals with sickle cell trait have a very small, albeit increased, risk of stroke compared to the general population, it is not the *greatest risk* among the options for their specific genotype and given clinical presentation.
*Autoinfarction of the spleen*
- **Splenic autoinfarction** (autosplenectomy) is a hallmark complication of **sickle cell anemia (HbSS)**, occurring due to repeated vaso-occlusive episodes in the splenic microcirculation.
- Patients with sickle cell trait typically have a normal-sized spleen and do not experience autoinfarction.
*Pigment stones in the biliary tract*
- **Pigment gallstones** are a common complication of **chronic hemolytic anemia**, such as that seen in **sickle cell disease (HbSS)**, due to increased bilirubin production from red blood cell breakdown.
- Patients with sickle cell trait do not typically experience chronic hemolysis and therefore have no increased risk of pigment gallstones compared to the general population.
More Pyelonephritis and urinary tract infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.