Obstructive uropathies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Obstructive uropathies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Obstructive uropathies US Medical PG Question 1: A 62-year-old man comes to the physician because of increased frequency of urination. He also says that he needs to urinate 4 to 5 times nightly and has difficulty initiating a urinary stream. He has had several episodes of acute cystitis treated with ciprofloxacin during the past year. Digital rectal examination shows a firm, symmetrically enlarged, non-tender prostate. This patient is most likely to develop which of the following complications?
- A. Inflammation of the renal interstitium
- B. Blastic bone lesions
- C. Abscess formation in the prostate
- D. Impaired intracavernosal blood flow
- E. Irreversible decrease in renal function (Correct Answer)
Obstructive uropathies Explanation: ***Irreversible decrease in renal function***
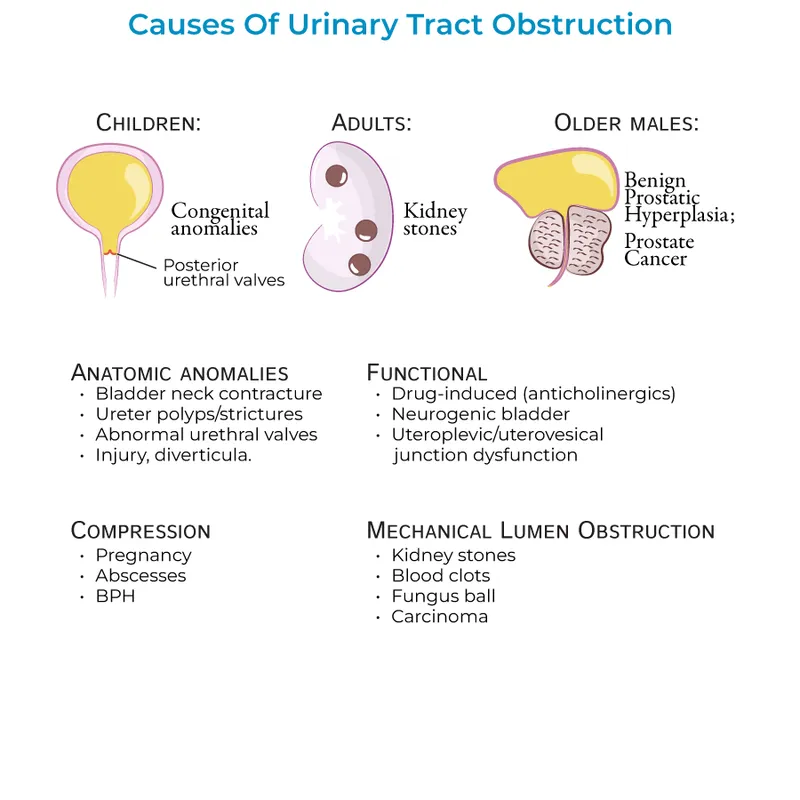
- The patient's symptoms of **increased urinary frequency**, **nocturia**, **difficulty initiating stream**, and **recurrent cystitis** in the context of a **symmetrically enlarged, firm prostate** are highly suggestive of **benign prostatic hyperplasia (BPH)** with progressive outflow obstruction.
- Chronic urinary outflow obstruction can lead to **hydronephrosis** and **backpressure on the kidneys**, eventually causing **renal parenchymal damage** and an irreversible decrease in renal function.
*Inflammation of the renal interstitium*
- While chronic obstruction can lead to **chronic pyelonephritis**, which involves interstitial inflammation, **irreversible renal function decrease** is a more encompassing and severe long-term complication of sustained BPH with urinary retention.
- **Acute interstitial nephritis** is typically associated with drug reactions or systemic diseases, rather than primarily BPH.
*Blastic bone lesions*
- **Blastic bone lesions** are characteristic of **metastatic prostate cancer**, which typically presents with an **asymmetrically firm or nodular prostate** on DRE, unlike the symmetric enlargement described here.
- Although the patient's age and prostate exam warrant consideration of prostate cancer, the clinical picture strongly favors BPH, making blastic bone lesions less likely as the primary complication.
*Abscess formation in the prostate*
- **Prostatic abscesses** typically present with acute systemic symptoms like **fever, chills, and perineal pain**, which are not mentioned in this patient's presentation.
- While recurrent urinary tract infections can increase the risk of prostatic abscess, the dominant concern here is the long-term impact of chronic obstruction.
*Impaired intracavernosal blood flow*
- **Impaired intracavernosal blood flow** is a common cause of **erectile dysfunction**, which can coexist with BPH due to shared risk factors or age, but it's not a direct complication of the urinary outflow obstruction itself.
- The patient's reported symptoms are primarily related to urination and bladder emptying, not sexual function.
Obstructive uropathies US Medical PG Question 2: A 70-year-old woman comes to the physician for the evaluation of loss of urine for the last several months. She loses small amounts of urine without warning after coughing or sneezing. She also sometimes forgets the names of her relatives. She is retired and lives at an assisted-living facility. She has type 2 diabetes mellitus and hypertension. Her older sister recently received a ventriculoperitoneal shunt. She does not smoke or drink alcohol. Medications include metformin and enalapril. Vital signs are within normal limits. She walks without any problems. Sensation to pinprick and light touch is normal. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Detrusor overactivity
- B. Urethral hypermobility
- C. Decreased cerebrospinal fluid absorption (Correct Answer)
- D. Loss of sphincter control
- E. Bacterial infection of the urinary tract
Obstructive uropathies Explanation: ***Decreased cerebrospinal fluid absorption***
- The patient's symptoms of **urinary incontinence** (losing urine without warning after coughing/sneezing) and **cognitive impairment** (forgetting names of relatives) in an older adult, especially with a family history of **ventriculoperitoneal shunt** (suggesting hydrocephalus), are highly suggestive of **Normal Pressure Hydrocephalus (NPH)**.
- Reduced reabsorption of CSF leads to ventricular enlargement and the classic NPH triad: **gait disturbance**, **urinary incontinence**, and **dementia**.
*Detrusor overactivity*
- This typically presents as **urge incontinence**, characterized by a sudden, strong need to urinate followed by involuntary urine loss, often with large volumes.
- While it causes incontinence, it does not explain the co-occurring **cognitive deficits**.
*Urethral hypermobility*
- This is a common cause of **stress incontinence**, where urine leakage occurs with increased intra-abdominal pressure (e.g., coughing, sneezing).
- However, **urethral hypermobility** does not account for the patient's **cognitive symptoms**.
*Loss of sphincter control*
- This can be a feature of **stress incontinence** or intrinsic sphincter deficiency, leading to urine leakage with exertion.
- Similar to urethral hypermobility, it does not explain the presence of **cognitive decline** in this patient.
*Bacterial infection of the urinary tract*
- A **urinary tract infection (UTI)** can cause new-onset incontinence, dysuria, urgency, and sometimes altered mental status in older adults.
- However, the patient's long-standing symptoms over "several months" and the presence of **memory loss** make a simple UTI less likely as the primary underlying cause; UTIs are typically acute.
Obstructive uropathies US Medical PG Question 3: A 66-year-old G3P3 presents with an 8-year-history of back pain, perineal discomfort, difficulty urinating, recurrent malaise, and low-grade fevers. These symptoms have recurred regularly for the past 5–6 years. She also says that there are times when she experiences a feeling of having a foreign body in her vagina. With the onset of symptoms, she was evaluated by a physician who prescribed her medications after a thorough examination and recommended a vaginal pessary, but she was non-compliant. She had 3 vaginal deliveries She has been menopausal since 51 years of age. She does not have a history of malignancies or cardiovascular disease. She has type 2 diabetes mellitus that is controlled with diet and metformin. Her vital signs include: blood pressure 110/60 mm Hg, heart rate 91/min, respiratory rate 13/min, and temperature 37.4℃ (99.3℉). On physical examination, there is bilateral costovertebral angle tenderness. The urinary bladder is non-palpable. The gynecologic examination reveals descent of the cervix to the level of the introitus. A Valsalva maneuver elicits uterine procidentia. Which pathology is most likely to be revealed by imaging in this patient?
- A. Renal cyst
- B. Urinary bladder polyp
- C. Renal tumor
- D. Hydronephrosis (Correct Answer)
- E. Renal calculi
Obstructive uropathies Explanation: ***Hydronephrosis***
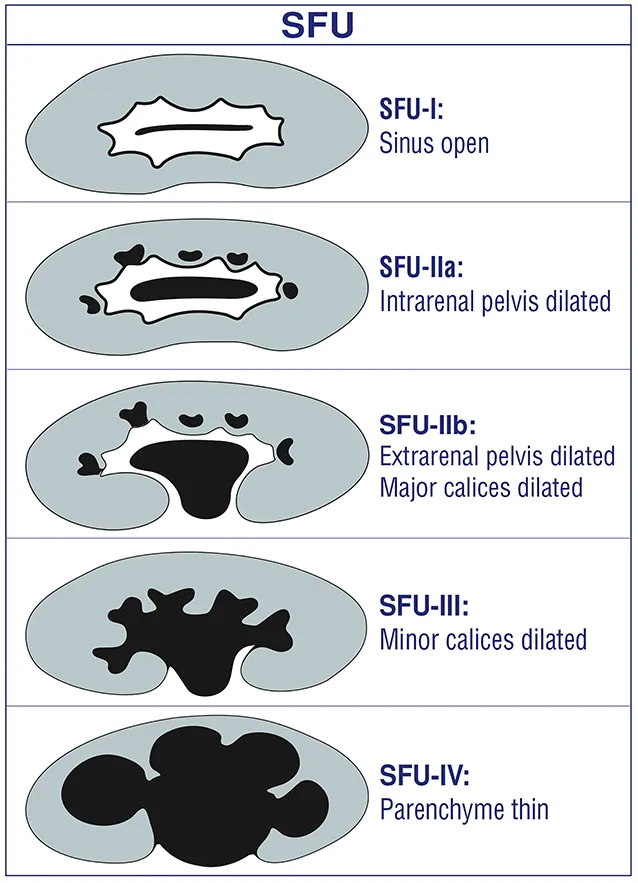
- The patient's **uterine procidentia** (third-degree uterine prolapse) can lead to **ureteral kinking** or compression, causing obstruction of urine flow.
- This obstruction, combined with recurrent back pain, malaise, low-grade fevers, and CVA tenderness, strongly suggests **hydronephrosis** due to urinary stasis and potential recurrent UTIs.
*Renal cyst*
- While common, renal cysts are typically **asymptomatic** and do not explain the recurrent fevers, malaise, and CVA tenderness.
- They are generally **not associated with urinary obstruction** leading to such systemic symptoms.
*Urinary bladder polyp*
- Bladder polyps can cause hematuria or urinary frequency but are **unlikely to cause bilateral CVA tenderness**, back pain, or systemic symptoms like fever and malaise.
- They do not typically lead to **ureteral obstruction** or hydronephrosis.
*Renal tumor*
- A renal tumor could explain systemic symptoms like malaise and low-grade fevers, but the recurrent nature over 5-6 years and the strong association with **uterine prolapse-induced obstruction** make it less likely.
- While it can cause back pain, **bilateral CVA tenderness** and difficulty urinating are not classic presenting features.
*Renal calculi*
- Renal calculi cause **severe, colicky flank pain** that radiates, and while they can cause urinary obstruction and recurrent UTIs, the patient's long-standing, constant back pain and the context of significant **uterine prolapse** make hydronephrosis a more direct consequence.
- The symptoms described are more indicative of **chronic obstruction** rather than acute stone passage.
Obstructive uropathies US Medical PG Question 4: A 37-year-old woman presents to the Emergency Department after 8 hours of left sided flank pain that radiates to her groin and pelvic pain while urinating. Her medical history is relevant for multiple episodes of urinary tract infections, some requiring hospitalization, and intravenous antibiotics. In the hospital, her blood pressure is 125/83 mm Hg, pulse of 88/min, a respiratory rate of 28/min, and a body temperature of 36.5°C (97.7°F). On physical examination, she has left costovertebral tenderness and lower abdominal pain. Laboratory studies include a negative pregnancy test, mild azotemia, and a urinary dipstick that is positive for blood. Which of the following initial tests would be most useful in the diagnosis of this case?
- A. Urine osmolality
- B. Fractional excretion of sodium (FeNa+)
- C. Renal ultrasonography (Correct Answer)
- D. Contrast abdominal computed tomography
- E. Blood urea nitrogen (BUN): serum creatinine (SCr) ratio
Obstructive uropathies Explanation: ***Renal ultrasonography***
- This is the most appropriate initial imaging test to evaluate for **kidney stones** (given the flank pain radiating to groin and hematuria) and **hydronephrosis** (which can indicate obstruction) and assess for signs of **pyelonephritis** (given the history of recurrent UTIs and CVA tenderness).
- It is **non-invasive**, readily available, and avoids radiation exposure, making it suitable as a first-line diagnostic tool in this setting.
*Urine osmolality*
- This test primarily assesses the kidney's ability to **concentrate urine**, which is more relevant for evaluating fluid balance, diabetes insipidus, or other renal tubular disorders.
- It would not directly diagnose the cause of acute flank pain or urinary tract obstruction.
*Fractional excretion of sodium (FeNa+)*
- FeNa+ is used to differentiate between **prerenal azotemia** and **acute tubular necrosis**, indicating the kidney's response to hypoperfusion.
- While the patient has mild azotemia, FeNa+ would not identify the underlying cause of the flank pain, hematuria, or potential obstruction.
*Contrast abdominal computed tomography*
- While highly sensitive for diagnosing kidney stones and other renal pathologies, **contrast CT** exposes the patient to **ionizing radiation** and risks associated with contrast agents (e.g., contrast-induced nephropathy), especially with pre-existing azotemia.
- It is often reserved for cases where ultrasound is inconclusive or more detailed anatomical information is needed.
*Blood urea nitrogen (BUN): serum creatinine (SCr) ratio*
- This ratio is primarily used to differentiate between **prerenal** causes of acute kidney injury (high ratio, e.g., >20:1) and **intrinsic renal** causes (lower ratio, e.g., <15:1).
- While it can provide insight into the etiology of azotemia, it does not directly identify the cause of the patient's acute flank pain or potential urinary tract obstruction.
Obstructive uropathies US Medical PG Question 5: A 32-year-old female presents with acute onset abdominal pain accompanied by nausea, vomiting, and hematuria. She is currently taking glipizide for type 2 diabetes mellitus. Past medical history is also significant for lactose intolerance. She has just started training for a marathon, and she drinks large amounts of sports drinks to replenish her electrolytes and eats a high-protein diet to assist in muscle recovery. She admits to using laxatives sporadically to help her manage her weight. On physical exam, the patient appears distressed and has difficulty getting comfortable. Her temperature is 36.8°C (98.2°F), heart rate is 103/min, respiratory rate is 15/min, blood pressure is 105/85 mm Hg, and oxygen saturation is 100% on room air. Her BMI is 21 kg/m2. CBC, CMP, and urinalysis are ordered. Renal ultrasound demonstrates an obstruction at the ureteropelvic junction (see image). Which of the following would most likely be seen in this patient?
- A. Positional urinary retention
- B. Rebound tenderness, pain exacerbated by coughing
- C. Edema and anuria
- D. Colicky pain radiating to the groin
- E. Flank pain that does not radiate to the groin (Correct Answer)
Obstructive uropathies Explanation: ***Flank pain that does not radiate to the groin***
- An obstruction at the **ureteropelvic junction (UPJ)** typically causes **flank pain** due to distention of the renal pelvis, but it often does not involve radiation to the groin because the obstruction is proximal to the ureter's course through the pelvis.
- The patient's presentation with acute abdominal pain, nausea, vomiting, hematuria, and distress is consistent with **renal colic** caused by a UPJ obstruction.
*Positional urinary retention*
- **Positional urinary retention** is typically associated with neurological conditions, prostate issues, or bladder outlet obstruction, which are not suggested by the patient's symptoms or findings.
- While an obstruction can cause urinary symptoms, the pain pattern and imaging finding of a UPJ obstruction are not characteristic of positional retention.
*Rebound tenderness, pain exacerbated by coughing*
- **Rebound tenderness** and pain exacerbated by coughing are classic signs of **peritoneal irritation** (e.g., appendicitis, peritonitis), which is not indicated by the renal ultrasound showing a UPJ obstruction.
- The patient's symptoms are localized to the urinary tract with hematuria, pointing away from a primary peritoneal process.
*Edema and anuria*
- **Edema** and **anuria** typically suggest severe renal failure or bilateral urinary tract obstruction, which is less likely with a unilateral UPJ obstruction unless there is pre-existing renal compromise or the obstruction has been prolonged and severe.
- The acute presentation with pain and hematuria, without signs of systemic fluid overload, makes these findings less probable.
*Colicky pain radiating to the groin*
- **Colicky pain radiating to the groin** is characteristic of a **ureteral stone** as it descends down the ureter, causing spasms and obstruction further along the urinary tract.
- The imaging showing an obstruction at the **ureteropelvic junction (UPJ)** indicates the obstruction is higher up, at the kidney's outlet, which typically causes flank pain without radiation to the groin.
Obstructive uropathies US Medical PG Question 6: A 58-year-old man presents to the Emergency Department after 3 hours of intense suprapubic pain associated with inability to urinate for the past day or two. His medical history is relevant for benign prostatic hyperplasia (BPH) that has been under treatment with prazosin and tadalafil. Upon admission, he is found to have a blood pressure of 180/100 mm Hg, a pulse of 80/min, a respiratory rate of 23/min, and a temperature of 36.5°C (97.7°F). He weighs 84 kg (185.1 lb) and is 175 cm (5 ft 7 in) tall. Physical exam, he has suprapubic tenderness. A bladder scan reveals 700 ml of urine. A Foley catheter is inserted and the urine is drained. Initial laboratory tests and their follow up 8 hours after admission are shown below.
Admission 8 hours after admission
Serum potassium 4.2 mmol/L Serum potassium 4.0 mmol/L
Serum sodium 140 mmol/L Serum sodium 142 mmol/L
Serum chloride 102 mmol/L Serum chloride 110 mmol/L
Serum creatinine 1.4 mg/dL Serum creatinine 1.6 mg/dL
Serum blood urea nitrogen 64 mg/dL Serum blood urea nitrogen 62 mg/dL
Urine output 250 mL Urine output 260 mL
A senior attending suggests a consultation with Nephrology. Which of the following best justifies this suggestion?
- A. Estimated glomerular filtration rate (eGFR)
- B. Urine output (Correct Answer)
- C. Serum creatinine (SCr)
- D. Serum blood urea nitrogen (BUN)
- E. Serum potassium
Obstructive uropathies Explanation: ***Urine output***
- The patient's **urine output is severely reduced** at 260 mL over 8 hours (approximately **32.5 mL/hour**), which constitutes **oliguria** (defined as <0.5 mL/kg/hr; this patient at 84 kg should produce ≥42 mL/hr).
- Despite **relief of the post-renal obstruction** via Foley catheterization, the persistent oliguria indicates **intrinsic kidney injury** rather than simple mechanical obstruction.
- The combination of **oliguria persisting after decompression** + **rising serum creatinine** (1.4→1.6 mg/dL) meets **KDIGO criteria for Stage 2 AKI** (urine output <0.5 mL/kg/hr for ≥12 hours).
- This requires **urgent nephrology consultation** to assess for acute tubular necrosis (ATN), guide fluid management during potential post-obstructive diuresis, and consider renal replacement therapy if oliguria worsens.
*Serum creatinine (SCr)*
- The serum creatinine **rose from 1.4 to 1.6 mg/dL** despite bladder decompression, which is concerning and suggests intrinsic renal injury.
- However, creatinine is a **lagging indicator** of kidney function - it takes 24-48 hours to reflect acute changes in GFR, whereas **urine output is a real-time indicator** of kidney function.
- While the rising creatinine supports the need for nephrology involvement, **urine output is the more immediate and actionable parameter** that prompted the attending's suggestion at this early time point.
*Estimated glomerular filtration rate (eGFR)*
- eGFR is **calculated from serum creatinine** using equations that assume steady-state conditions, which **do not apply in acute kidney injury**.
- In the **acute setting with rapidly changing kidney function**, eGFR calculations are unreliable and can significantly overestimate or underestimate true GFR.
- Clinicians rely more on **urine output and serial creatinine measurements** rather than eGFR when managing AKI.
*Serum blood urea nitrogen (BUN)*
- The BUN decreased slightly from 64 to 62 mg/dL, remaining elevated but showing minimal change after catheterization.
- Elevated BUN can reflect **pre-renal azotemia, dehydration, or upper GI bleeding** and is less specific for intrinsic kidney injury than oliguria.
- The **BUN:Cr ratio** is approximately 40:1 (64/1.6), suggesting a **pre-renal component**, but this alone doesn't justify urgent nephrology consultation as strongly as the persistent oliguria does.
*Serum potassium*
- Serum potassium levels remain **normal** (4.2→4.0 mmol/L) and do not indicate a metabolic emergency.
- While **hyperkalemia** is a common complication of AKI that would warrant nephrology involvement, this patient's potassium is well-controlled and not the driving concern at this time.
Obstructive uropathies US Medical PG Question 7: A 43-year-old man presents with acute-onset left flank pain for the past 6 hours. He describes the pain as severe, intermittent, colicky, and “coming in waves”, and he points to the area of the left costovertebral angle (CVA). He says he recently has been restricting oral liquid intake to only 2 glasses of water per day based on the advice of his healer. He also reports nausea and vomiting. The patient has a history of hypertension, gout, and type 2 diabetes mellitus. He is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. There is exquisite left CVA tenderness. A urinalysis shows gross hematuria. Which of the following is the next best step in the management of this patient?
- A. Non-contrast CT of the abdomen
- B. Contrast CT of the abdomen and pelvis
- C. Supine abdominal radiograph
- D. Renal ultrasound
- E. Non-contrast CT of the abdomen and pelvis (Correct Answer)
Obstructive uropathies Explanation: **Non-contrast CT of the abdomen and pelvis**
- **Non-contrast CT of the abdomen and pelvis** is the gold standard for diagnosing urolithiasis, providing high sensitivity and specificity for detecting stones, identifying their size and location, and assessing for hydronephrosis.
- The patient's presentation with **acute-onset, severe, colicky flank pain**, nausea, vomiting, gross hematuria, and CVA tenderness is highly suggestive of **renal colic due to a kidney stone**.
*Non-contrast CT of the abdomen*
- This option is **insufficient** as kidney stones can be located in the ureters within the pelvis; a scan of the abdomen alone might miss stones in the distal ureter.
- While a non-contrast CT is appropriate, the scope of only the abdomen is **incomplete** for evaluating the entire urinary tract that might be affected by stones.
*Contrast CT of the abdomen and pelvis*
- **Contrast-enhanced CT is generally not indicated** for the initial evaluation of suspected renal colic due to urolithiasis because it can obscure the visualization of urinary stones.
- The use of contrast also carries risks such as **allergic reaction** and **contrast-induced nephropathy**, which are unnecessary in this acute, non-complicated setting.
*Supine abdominal radiograph*
- A supine abdominal radiograph (KUB) has **limited sensitivity** for detecting kidney stones, especially radiolucent stones (e.g., uric acid stones) or small stones.
- It also provides **poor anatomical detail** and cannot assess for hydronephrosis or other complications as effectively as CT.
*Renal ultrasound*
- Renal ultrasound can detect **hydronephrosis** and some kidney stones but is less sensitive than CT for visualizing smaller stones, especially in the ureters.
- Its diagnostic utility can be **limited by body habitus** and operator dependence, making it less reliable as a primary diagnostic tool for acute renal colic.
Obstructive uropathies US Medical PG Question 8: A 67-year-old man presents to his primary care physician complaining of frequent urination overnight. He states that for several years he has had trouble maintaining his urine stream along with the need for frequent urination, but the nighttime urination has only recently started. The patient also states that he has had 2 urinary tract infections in the last year, which he had never had previously. On exam, his temperature is 98.8°F (37.1°C), blood pressure is 124/68 mmHg, pulse is 58/min, and respirations are 13/min. On digital rectal exam, the prostate is enlarged but feels symmetric and smooth. Which of the following is a possible consequence of this condition?
- A. Increased serum creatinine (Correct Answer)
- B. Malignant transformation
- C. Increased serum AFP
- D. Increased serum hCG
- E. Increased serum ALP
Obstructive uropathies Explanation: ***Increased serum creatinine***
- Chronic **urinary retention** due to benign prostatic hyperplasia (BPH) can lead to **hydronephrosis** and **renal parenchymal damage**, impairing kidney function and increasing serum creatinine.
- The patient's symptoms of difficulty maintaining urine stream, frequent urination, and recurrent UTIs suggest BPH, which can progress to urinary obstruction and subsequent kidney dysfunction.
*Malignant transformation*
- **Benign prostatic hyperplasia (BPH)** is a non-malignant condition and does not directly undergo **malignant transformation** into prostate cancer.
- While both BPH and prostate cancer can coexist, BPH itself is not considered a premalignant lesion.
*Increased serum AFP*
- **Alpha-fetoprotein (AFP)** is a tumor marker primarily associated with **hepatocellular carcinoma** and **germ cell tumors** (e.g., testicular cancer).
- It is not associated with benign prostatic hyperplasia (BPH) or its complications.
*Increased serum hCG*
- **Human chorionic gonadotropin (hCG)** is a tumor marker most notably elevated in **choriocarcinoma** and some **germ cell tumors**.
- It has no association with benign prostatic hyperplasia (BPH) or urinary obstruction.
*Increased serum ALP*
- **Alkaline phosphatase (ALP)** can be elevated in conditions affecting the **liver** (e.g., cholestasis) or **bones** (e.g., Paget's disease, osteoblastic metastases).
- While significantly elevated ALP can indicate prostate cancer with **bone metastases**, it is not a direct consequence of uncomplicated benign prostatic hyperplasia (BPH).
Obstructive uropathies US Medical PG Question 9: An 82-year-old woman presents to the emergency department because of excruciating right flank pain and fever for the past 2 days. She states that she is having trouble urinating. Her past medical history is unremarkable. A urinalysis is performed and comes back positive for leukocytes and gram-negative bacilli. A contrast computed tomography of the abdomen is performed and reveals a large retroperitoneal mass compressing the right ureter, leading to hydronephrosis of the right kidney. The mass is excised. Histopathologic evaluation of the mass is shown in the image below, and it is determined to be malignant. Which of the following is the most likely diagnosis in this patient?
- A. Rhabdomyosarcoma
- B. Leiomyosarcoma
- C. Lipoma
- D. Teratoma
- E. Liposarcoma (Correct Answer)
Obstructive uropathies Explanation: ***Liposarcoma***
- The **most common primary malignant retroperitoneal tumor** in adults, particularly in elderly patients
- Characteristically presents as a **large retroperitoneal mass** causing compressive symptoms such as hydronephrosis
- **Histopathological features** include pleomorphic lipoblasts with varying degrees of differentiation (well-differentiated, dedifferentiated, myxoid, or pleomorphic subtypes)
- The clinical presentation of an elderly patient with a malignant retroperitoneal mass strongly suggests this diagnosis
*Rhabdomyosarcoma*
- Primarily a **pediatric malignancy**, most common in children and young adults under 20 years old
- Most frequently arises in the **head and neck, genitourinary tract, or extremities**, not typically retroperitoneal
- Histologically shows skeletal muscle differentiation with rhabdomyoblasts, not lipoblastic features
*Leiomyosarcoma*
- More commonly found in the **uterus, gastrointestinal tract, or blood vessels**
- While it can occur in the retroperitoneum, it is **less common** than liposarcoma in this location
- Histologically demonstrates **smooth muscle differentiation** with spindle cells, not the lipoblastic features characteristic of the described mass
*Lipoma*
- A **benign tumor** composed of mature adipose tissue without cellular atypia
- Would not present as a **malignant mass** on histopathologic evaluation
- Generally asymptomatic and slow-growing; unlikely to cause severe symptoms like excruciating pain or obstructive hydronephrosis
*Teratoma*
- Contains tissue derived from **all three germ layers** (ectoderm, mesoderm, endoderm)
- More commonly associated with **gonadal or midline structures** (ovaries, testes, mediastinum)
- Rare in the retroperitoneum in elderly patients; histology would show diverse tissue types rather than predominantly lipoblastic features
Obstructive uropathies US Medical PG Question 10: A 12-year-old boy presents to your office with facial swelling and dark urine. He has no other complaints other than a sore throat 3 weeks ago that resolved after 6 days. He is otherwise healthy, lives at home with his mother and 2 cats, has no recent history of travel, and no sick contacts. On physical examination his temperature is 99°F (37.2°C), blood pressure is 130/85 mmHg, pulse is 80/min, respirations are 19/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal examinations are unremarkable. There is mild periorbital and pedal edema. Urinalysis shows 12-15 RBC/hpf, 2-5 WBC/hpf, and 30 mg/dL protein. Which additional finding would you expect to see on urinalysis?
- A. Fatty casts
- B. RBC casts (Correct Answer)
- C. WBC casts
- D. Granular casts
- E. Hyaline casts
Obstructive uropathies Explanation: ***RBC casts***
- The patient's presentation with **facial swelling**, **dark urine**, and a history of a recent **sore throat** points toward **post-streptococcal glomerulonephritis (PSGN)**.
- **RBC casts** are a hallmark microscopic finding in **glomerulonephritis**, indicating **glomerular inflammation** and bleeding.
*Fatty casts*
- **Fatty casts** are characteristic of **nephrotic syndrome**, which primarily involves heavy proteinuria and generalized edema.
- While there is some proteinuria and edema, the dark urine and history of recent infection are more consistent with nephritic syndrome.
*Hyaline casts*
- **Hyaline casts** are composed of Tamm-Horsfall proteins and can be found in healthy individuals, or in conditions like **dehydration** or **fever**.
- They are a non-specific finding and do not indicate specific renal pathology like glomerulonephritis.
*WBC casts*
- **WBC casts** are typically seen in **pyelonephritis** (kidney infection) or **interstitial nephritis**, indicating inflammation within the renal tubules.
- The patient's primary symptoms and lab findings are more consistent with glomerular disease rather than an infection of the renal parenchyma.
*Granular casts*
- **Granular casts** are formed from degenerated cellular casts or protein aggregates and are often seen in **acute tubular necrosis (ATN)** or **chronic kidney disease**.
- While they suggest renal parenchymal injury, they are not as specific for glomerulonephritis as RBC casts, especially in a subacute presentation like this.
More Obstructive uropathies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.