Nephrotic syndrome disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nephrotic syndrome disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nephrotic syndrome disorders US Medical PG Question 1: A 43-year-old man comes to the physician for a 1-week history of swelling around his eyes and decreased urination. His pulse is 87/min, and blood pressure is 152/95 mm Hg. Physical examination shows 1+ periorbital and pretibial edema. Serum studies show a urea nitrogen concentration of 21 mg/dL and a creatinine concentration of 1.4 mg/dL. Urinalysis shows 3+ blood and 1+ protein. Further evaluation of this patient is most likely to show which of the following?
- A. Urinary rhomboid crystals
- B. Renal interstitial inflammation
- C. Hypoalbuminemia
- D. Detached renal tubular epithelial cells
- E. Red blood cell casts (Correct Answer)
Nephrotic syndrome disorders Explanation: ***Red blood cell casts***
- The patient's presentation with **periorbital and pretibial edema**, **hypertension**, elevated **creatinine**, **hematuria** (3+ blood), and mild **proteinuria** (1+ protein) is highly suggestive of **acute glomerulonephritis**.
- **Red blood cell casts** are pathognomonic for **glomerulonephritis**, indicating that red blood cells are leaking from the glomeruli and congealing in the renal tubules.
*Urinary rhomboid crystals*
- **Urinary rhomboid crystals** are typically associated with conditions like **uric acid nephrolithiasis** or gout, which are not suggested by the patient's symptoms or lab findings.
- Their presence would indicate a risk for **kidney stones**, not evidence of glomerular inflammation.
*Renal interstitial inflammation*
- **Renal interstitial inflammation** is characteristic of **acute interstitial nephritis**, which often presents with fever, rash, eosinophilia, and flank pain, usually due to drug reactions or infections.
- While kidney injury can occur, the primary findings of **hematuria** and **proteinuria** in this context strongly point away from an interstitial process as the initial diagnosis.
*Hypoalbuminemia*
- **Hypoalbuminemia** is a hallmark of **nephrotic syndrome**, characterized by severe proteinuria (>3.5 g/day), significant edema, and hyperlipidemia.
- This patient has only 1+ proteinuria, which is not severe enough to cause significant hypoalbuminemia or the full nephrotic picture.
*Detached renal tubular epithelial cells*
- **Detached renal tubular epithelial cells** and **tubular cell casts** are characteristic findings in **acute tubular necrosis (ATN)**, usually resulting from ischemia or nephrotoxins.
- While ATN can cause acute kidney injury, the prominent **hematuria** and **hypertension** in this case are more indicative of a glomerular process than tubular damage.
Nephrotic syndrome disorders US Medical PG Question 2: A 44-year-old man comes to the physician because of a 2-week history of lower extremity swelling and frothy urine. He has a history of chronic hepatitis C infection. Physical examination shows 3+ pitting edema of the lower legs and ankles. Further evaluation of this patient is most likely to show which of the following?
- A. Decreased cholesterol
- B. Decreased blood urea nitrogen
- C. Increased antithrombin III
- D. Decreased cystatin C
- E. Increased lipoproteins (Correct Answer)
Nephrotic syndrome disorders Explanation: ***Increased lipoproteins***
- The patient's symptoms (**lower extremity swelling**, **frothy urine**) and history of **hepatitis C infection** are highly suggestive of **nephrotic syndrome**.
- **Nephrotic syndrome** is characterized by severe proteinuria, leading to **hypoalbuminemia**, edema, and often **compensatory hyperlipidemia** (increased lipoproteins) due to increased hepatic synthesis of lipids.
*Decreased cholesterol*
- **Nephrotic syndrome** typically leads to **hyperlipidemia**, including **elevated cholesterol levels**, not decreased, as the liver compensates for protein loss by increasing lipid synthesis.
- This is a key diagnostic feature differentiating nephrotic syndrome from other conditions that might cause edema.
*Decreased blood urea nitrogen*
- In **nephrotic syndrome**, kidney function might initially be preserved, or kidney injury could lead to **increased BUN** if glomerular filtration rate (GFR) significantly declines.
- **Decreased BUN** is usually seen in conditions like liver failure, overhydration, or low protein diet, which are not suggested by the clinical picture.
*Increased antithrombin III*
- Patients with **nephrotic syndrome** typically have **decreased levels of antithrombin III** due to urinary loss of this anticoagulant protein, increasing their risk of **thrombosis**.
- Therefore, an increase in antithrombin III would be highly unlikely and is contrary to the pathophysiology of nephrotic syndrome.
*Decreased cystatin C*
- **Cystatin C** is an endogenous marker of **renal function** (similar to creatinine), and its levels usually **increase** when glomerular filtration rate (GFR) decreases, indicating kidney impairment.
- A decrease in cystatin C would suggest improved or hyper-filtration, which is not consistent with the signs of kidney damage seen in nephrotic syndrome.
Nephrotic syndrome disorders US Medical PG Question 3: A 70-year-old man with a long-standing history of diabetes mellitus type 2 and hypertension presents with complaints of constant wrist and shoulder pain. Currently, the patient undergoes hemodialysis 2 to 3 times a week and is on the transplant list for a kidney. The patient denies any recent traumas. Which of the following proteins is likely to be increased in his plasma, causing the patient’s late complaints?
- A. Amyloid precursor protein
- B. Amyloid A (AA)
- C. β2-microglobulin (Correct Answer)
- D. Transthyretin (TTR)
- E. Ig light chains
Nephrotic syndrome disorders Explanation: **β2-microglobulin**
- The patient's presentation with **chronic wrist and shoulder pain**, particularly in the setting of **long-term hemodialysis for end-stage renal disease (ESRD)**, is highly suggestive of **dialysis-related amyloidosis (DRA)**.
- **β2-microglobulin** is a small protein that is normally filtered by the kidneys. In ESRD patients on hemodialysis, it accumulates and forms amyloid deposits, primarily in joint capsules, synovium, and bones.
*Amyloid precursor protein*
- **Amyloid precursor protein (APP)** is primarily associated with **Alzheimer's disease**, where its proteolytic cleavage leads to the formation of amyloid-beta plaques in the brain.
- It is not directly implicated in joint pain or musculoskeletal amyloidosis in the context of renal failure.
*Amyloid A (AA)*
- **Amyloid A (AA)** is the protein responsible for **secondary (reactive) amyloidosis**, which is typically associated with chronic inflammatory conditions like rheumatoid arthritis or chronic infections.
- While the patient has some chronic conditions (diabetes, hypertension), his joint pain is more characteristic of dialysis-related amyloidosis, not systemic inflammation-induced AA amyloidosis.
*Transthyretin (TTR)*
- **Transthyretin (TTR)** is associated with **familial amyloid polyneuropathy** and **senile systemic amyloidosis (SSA)**, causing heart failure or carpal tunnel syndrome, but it is not directly linked to dialysis-related amyloidosis.
- The patient's symptoms are more indicative of the specific type of amyloidosis seen in ESRD.
*Ig light chains*
- **Immunoglobulin (Ig) light chains** are involved in **primary (AL) amyloidosis**, which is caused by a plasma cell dyscrasia.
- While AL amyloidosis can affect various organs, including joints, the patient's history of ESRD and hemodialysis makes **β2-microglobulin amyloidosis** the most specific and likely cause of his musculoskeletal symptoms.
Nephrotic syndrome disorders US Medical PG Question 4: A 42-year-old man presents to his primary care provider complaining of foamy urine for the last 2 weeks. He has also begun to notice swelling in his hands and feet, and he says that his shoes have not been fitting normally. On exam, the patient has a temperature of 98.8°F (37.1°C), blood pressure is 132/84 mmHg, pulse is 64/min, and respirations are 12/min. The patient has 2+ pitting edema bilaterally up to his shins. A 24-hour urine study is found to contain 9.0 g of protein. The patient is referred to a specialist and undergoes a renal biopsy. On light microscopy, the glomeruli demonstrate basement membrane thickening. On electron microscopy, subepithelial deposits are seen. Which of the following is a characteristic of this patient’s disease?
- A. X-linked condition
- B. Antibodies to alveolar basement membrane
- C. Loss of podocyte foot processes
- D. Antibodies to phospholipase A2 receptor (Correct Answer)
- E. IgA immune complex deposition
Nephrotic syndrome disorders Explanation: ***Antibodies to phospholipase A2 receptor***
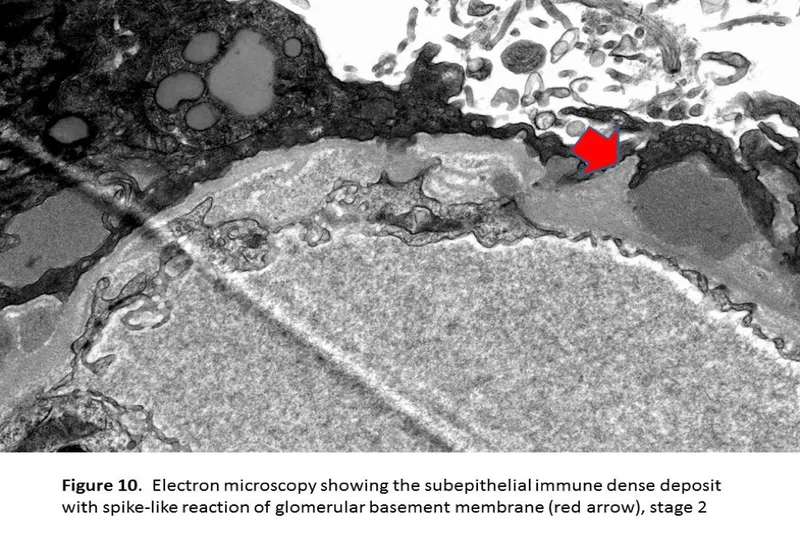
- The patient's presentation with **foamy urine**, **edema**, and **9.0 g of protein** in a 24-hour urine study indicates **nephrotic syndrome**. Renal biopsy findings of **glomerular basement membrane thickening** on light microscopy and **subepithelial deposits** on electron microscopy are characteristic of **membranous nephropathy**.
- Approximately 70-80% of primary membranous nephropathy cases are associated with **autoantibodies to the M-type phospholipase A2 receptor (PLA2R)**, a protein expressed on podocytes.
*X-linked condition*
- This description is characteristic of **Alport syndrome**, a genetic disorder leading to progressive kidney disease, hearing loss, and eye abnormalities.
- Alport syndrome presents with **hematuria** rather than significant proteinuria, and biopsy would show **laminar splitting of the glomerular basement membrane**.
*Antibodies to alveolar basement membrane*
- This describes **Goodpasture syndrome**, which is characterized by the presence of anti-glomerular basement membrane (anti-GBM) antibodies that target both the kidney and the lung.
- Patients typically present with rapidly progressive glomerulonephritis and pulmonary hemorrhage, and biopsy would show **linear IgG deposition** along the glomerular basement membrane on immunofluorescence.
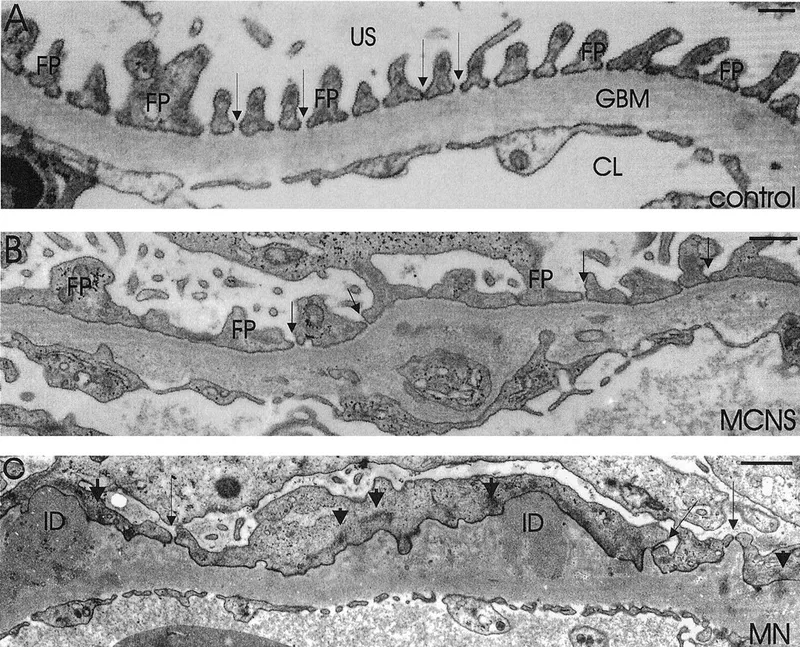
*Loss of podocyte foot processes*
- This is a characteristic finding in **minimal change disease** and **focal segmental glomerulosclerosis (FSGS)**, two other causes of nephrotic syndrome.
- Minimal change disease typically shows normal glomeruli on light microscopy, while FSGS shows segmental sclerosis. Neither shows subepithelial deposits.
*IgA immune complex deposition*
- This is the hallmark of **IgA nephropathy (Berger's disease)** or **Henoch-Schönlein purpura** in children.
- Patients typically present with **hematuria**, often macroscopic, following an upper respiratory or gastrointestinal infection. Biopsy would show IgA deposits in the mesangium, not subepithelial deposits.
Nephrotic syndrome disorders US Medical PG Question 5: A 67-year-old man presents to his primary care provider because of fatigue and loss of appetite. He is also concerned that his legs are swollen below the knee. He has had type 2 diabetes for 35 years, for which he takes metformin and glyburide. Today his temperature is 36.5°C (97.7°F), the blood pressure is 165/82 mm Hg, and the pulse is 88/min. Presence of which of the following would make diabetic kidney disease less likely in this patient?
- A. Normal-to-large kidneys on ultrasound
- B. Gradual reduction of glomerular filtration rate (GFR)
- C. Diabetic retinopathy
- D. Nephrotic range proteinuria
- E. Cellular casts in urinalysis (Correct Answer)
Nephrotic syndrome disorders Explanation: ***Cellular casts in urinalysis***
- The presence of **cellular casts**, especially **red blood cell casts** or **white blood cell casts**, suggests an active glomerular inflammatory disease (e.g., glomerulonephritis) or an interstitial nephritis, which are atypical for uncomplicated diabetic kidney disease.
- Diabetic kidney disease typically presents with bland urine sediment without significant cellular casts.
*Normal-to-large kidneys on ultrasound*
- In the early stages of diabetic kidney disease, the kidneys can be **normal in size or even enlarged** due to compensatory hypertrophy and increased renal blood flow.
- Only in **advanced stages** of chronic kidney disease from diabetes do the kidneys become atrophic and shrunken.
*Gradual reduction of glomerular filtration rate (GFR)*
- Diabetic kidney disease is characterized by a **progressive decline in GFR** over time, often correlating with the duration and control of diabetes.
- This gradual decline is a hallmark differentiating it from acute kidney injury or rapidly progressive glomerulonephritis.
*Diabetic retinopathy*
- The presence of **diabetic retinopathy** is a strong indicator of **microvascular complications** of diabetes and is highly correlated with the presence and severity of diabetic kidney disease.
- This co-occurrence supports a diagnosis of diabetic kidney disease, not ruling it out.
*Nephrotic range proteinuria*
- **Nephrotic range proteinuria** (protein excretion > 3.5 g/day) is a common manifestation of diabetic kidney disease, especially as the disease progresses to more advanced stages.
- This level of proteinuria suggests significant glomerular damage, consistent with diabetic nephropathy.
Nephrotic syndrome disorders US Medical PG Question 6: A 66-year-old white man comes to the physician because of a 10-day history of fatigue and lower leg swelling. Over the past 6 months, he has had a 3.6-kg (8-lb) weight loss. He has chronic bronchitis and uses an albuterol inhaler as needed. He has smoked one pack of cigarettes daily for 44 years and drinks one alcoholic beverage daily. His temperature is 37°C (98.6°F), pulse is 88/min, and blood pressure is 120/75 mm Hg. He appears thin. Examination shows 2+ pretibial edema bilaterally. Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Hemoglobin 11.2 g/dL
Leukocyte count 8500/mm3
Platelet count 130,000/mm3
Serum
Urea nitrogen 23 mg/dL
Glucose 77 mg/dL
Creatinine 1.6 mg/dL
Albumin 1.8 mg/dL
Total cholesterol 475 mg/dL
Urine
Blood negative
Glucose negative
Protein 4+
WBC 0–1/hpf
Fatty casts numerous
An x-ray of the chest shows a right upper lobe density. A CT scan of the chest shows a 2.5 x 3.5 x 2-cm right upper lobe mass. Which of the following is the most likely diagnosis?
- A. Thin basement membrane disease
- B. Granulomatosis with polyangiitis
- C. Rapidly progressive glomerulonephritis
- D. Membranous nephropathy (Correct Answer)
- E. Focal segmental glomerulosclerosis
Nephrotic syndrome disorders Explanation: ***Membranous nephropathy***
- This patient presents with signs of **nephrotic syndrome**: pronounced **proteinuria (4+)**, **hypoalbuminemia** (1.8 mg/dL), **hyperlipidemia** (total cholesterol 475 mg/dL), and **edema**.
- The chest x-ray and CT findings of a **right upper lobe mass** in a long-term smoker raise suspicion for a **paraneoplastic syndrome**, with **membranous nephropathy** being a common cause of nephrotic syndrome associated with solid tumors, particularly lung cancer.
*Thin basement membrane disease*
- This condition is typically associated with **microscopic hematuria** but usually **not significant proteinuria** leading to nephrotic syndrome.
- It is often asymptomatic or presents with recurrent hematuria, not the systemic symptoms of nephrotic syndrome seen here.
*Granulomatosis with polyangiitis*
- This is a **vasculitis** often affecting the kidneys, presenting as **rapidly progressive glomerulonephritis** with hematuria, red cell casts, and mild proteinuria.
- It would typically cause **systemic vasculitic symptoms** (e.g., upper and lower respiratory tract involvement, skin lesions), and the proteinuria would not typically be in the nephrotic range.
*Rapidly progressive glomerulonephritis*
- Characterized by **rapid decline in renal function** and a **nephritic urine sediment** (hematuria, red cell casts, mild proteinuria), not nephrotic-range proteinuria with fatty casts.
- While lung involvement can occur (e.g., Goodpasture syndrome, vasculitis), the presentation here is strongly indicative of nephrotic syndrome.
*Focal segmental glomerulosclerosis*
- While it causes **nephrotic syndrome**, it does not typically present with a clear **underlying malignancy** as a paraneoplastic manifestation.
- The presence of a lung mass strongly suggests a secondary cause for the glomerulopathy, making membranous nephropathy a more direct fit.
Nephrotic syndrome disorders US Medical PG Question 7: A 7-year-old girl is brought to her pediatrician by her mother because of puffiness under both eyes in the morning. The mother reports that the child has just recovered from a seasonal influenza infection a few days ago. Vital signs include: temperature 37°C (98.6°F), blood pressure 100/67 mm Hg, and pulse 95/min. On examination, there is facial edema and bilateral 2+ pitting edema over the legs. Laboratory results are shown:
Serum albumin 2.1 g/dL
Serum triglycerides 200 mg/dL
Serum cholesterol 250 mg/dL
Urine dipstick 4+ protein
Which of the following casts are more likely to be present in this patient’s urine?
- A. Waxy casts
- B. Fatty casts (Correct Answer)
- C. Red cell casts
- D. Granular casts
- E. White cell casts
Nephrotic syndrome disorders Explanation: ***Fatty casts***
- The patient's presentation with **facial edema**, **pitting edema**, **hypoalbuminemia**, **hyperlipidemia** (increased triglycerides and cholesterol), and **heavy proteinuria** (4+ protein on urine dipstick) is highly suggestive of **nephrotic syndrome**.
- **Fatty casts** are pathognomonic for **nephrotic syndrome** because they are formed from renal tubular epithelial cells that have absorbed filtered lipids (cholesterol, triglycerides) and subsequently desquamated.
*Waxy casts*
- **Waxy casts** are typically associated with **chronic kidney disease** and indicate severe, longstanding tubular atrophy and dilation, often seen in end-stage renal disease.
- While they can be present in nephrotic syndrome if the kidney damage is severe and chronic, they are not the most characteristic cast *specifically* for the acute onset and hyperlipidemia seen here.
*Red cell casts*
- **Red cell casts** are indicative of **glomerulonephritis** (nephritic syndrome), where red blood cells leak through damaged glomerular capillaries into the renal tubules.
- This patient's presentation is characterized by **heavy proteinuria** and **edema** (nephrotic syndrome), without signs such as hematuria or hypertension that would typically suggest a nephritic picture.
*Granular casts*
- **Granular casts** are formed from degenerated cellular casts (e.g., granular breakdown products of renal tubular epithelial cells) or aggregated plasma proteins, and are non-specific indicators of **kidney damage** or **acute tubular necrosis**.
- While they can be seen in various kidney diseases, including nephrotic syndrome, they are not as specific as fatty casts for the constellation of symptoms presented.
*White cell casts*
- **White cell casts** are typically associated with **pyelonephritis** (kidney infection) or **interstitial nephritis**, indicating inflammation within the renal tubules or interstitium.
- There is no clinical or laboratory evidence of infection or inflammation suggesting pyelonephritis in this patient.
Nephrotic syndrome disorders US Medical PG Question 8: A 69-year-old white man comes to the physician because of a 15-day history of fatigue and lower leg swelling. Over the past 8 months, he has had a 3.8-kg (8.3-lb) weight loss. He has smoked one pack of cigarettes daily for 48 years. Vital signs are within normal limits. He appears thin. Examination shows 2+ pretibial edema bilaterally. An x-ray of the chest shows a right upper lobe density. Laboratory studies show:
Hemoglobin 11.3 g/dL
Leukocyte count 8600/mm3
Platelet count 140,000/mm3
Serum
Urea nitrogen 25 mg/dL
Glucose 79 mg/dL
Creatinine 1.7 mg/dL
Albumin 1.6 mg/dL
Total cholesterol 479 mg/dL
Urine
Blood negative
Glucose negative
Protein 4+
WBC 0–1/hpf
Fatty casts numerous
Light microscopic examination of a kidney biopsy reveals thickening of glomerular capillary loops and the basal membrane. Which of the following is the most likely diagnosis?
- A. Rapidly progressive glomerulonephritis
- B. Granulomatosis with polyangiitis
- C. Membranous nephropathy (Correct Answer)
- D. Focal segmental glomerulosclerosis
- E. Membranoproliferative glomerulonephritis
Nephrotic syndrome disorders Explanation: ***Membranous nephropathy***
- The patient's presentation with **nephrotic syndrome** (edema, severe proteinuria 4+, hypoalbuminemia, hyperlipidemia, and fatigue) in an older adult, along with a **right upper lobe density** concerning for malignancy, strongly suggests secondary membranous nephropathy.
- The renal biopsy finding of **thickening of glomerular capillary loops and the basal membrane** is a hallmark of membranous nephropathy.
*Rapidly progressive glomerulonephritis*
- Characterized by a **rapid decline in renal function** over days to weeks, often with oliguria and symptoms of severe systemic illness.
- While proteinuria can be present, the classic biopsy finding is **crescent formation**, which is not described here.
*Granulomatosis with polyangiitis*
- This is a systemic vasculitis often involving the **upper and lower respiratory tracts** and kidneys, commonly presenting with **hemoptysis, sinusitis, and glomerulonephritis**.
- While a lung density is present, the absence of **hemoptysis** and the specific biopsy findings of membranous nephropathy make it less likely.
*Focal segmental glomerulosclerosis*
- This typically causes nephrotic syndrome but is characterized by **segmental sclerosis of glomeruli** on biopsy.
- While it can be idiopathic or secondary, the specific biopsy description and association with a potential malignancy point away from FSGS.
*Membranoproliferative glomerulonephritis*
- This condition presents with features of both **nephrotic and nephritic syndromes** and is characterized by a "tram-track" appearance on biopsy due to mesangial cell proliferation and basement membrane splitting.
- This specific microscopic finding is not mentioned in the patient's biopsy report.
Nephrotic syndrome disorders US Medical PG Question 9: A 41-year-old African American woman presents to her primary care physician with a 3-week history of lower extremity edema and shortness of breath. She says that she has also noticed that she gets fatigued more easily and has been gaining weight. Her past medical history is significant for sickle cell disease and HIV infection for which she is currently taking combination therapy. Physical exam is significant for periorbital and lower extremity edema. Laboratory testing is significant for hypoalbuminemia, and urinalysis demonstrates 4+ protein. Which of the following would most likely be seen on kidney biopsy in this patient?
- A. Birefringence under polarized light
- B. Segmental scarring (Correct Answer)
- C. Subepithelial deposits
- D. Expansion of the mesangium
- E. Normal glomeruli
Nephrotic syndrome disorders Explanation: ***Segmental scarring***
- The patient's history of **HIV infection**, symptoms of **nephrotic syndrome** (edema, weight gain, fatigue, hypoalbuminemia, 4+ proteinuria), and African American ethnicity are highly suggestive of **HIV-associated nephropathy (HIVAN)**.
- HIVAN is a form of **collapsing focal segmental glomerulosclerosis (FSGS)**, a condition characterized by **segmental scarring** and collapse of the glomerular tuft. In HIVAN, this scarring is severe and progressive.
*Birefringence under polarized light*
- This finding is characteristic of **amyloidosis**, where protein deposits (amyloid) accumulate in tissues and exhibit apple-green birefringence under Congo red stain and polarized light.
- While amyloidosis can cause nephrotic syndrome, it is not the most common kidney pathology in an HIV-positive patient with these specific features.
*Subepithelial deposits*
- **Subepithelial deposits** with a characteristic "spike and dome" appearance on electron microscopy are pathognomonic for **membranous glomerulonephritis**.
- This type of glomerulonephritis is not typically associated with HIV infection, nor does it typically present with the rapidly progressive decline seen in HIVAN.
*Expansion of the mesangium*
- **Mesangial expansion** is a common feature in several glomerular diseases, including **diabetic nephropathy** and early-stage IgA nephropathy.
- While it can be present in some forms of FSGS, it is not the primary or most characteristic finding for HIVAN, which is better described by collapsing glomeruli and segmental scarring.
*Normal glomeruli*
- Given the patient's profound **proteinuria (4+)**, hypoalbuminemia, and symptoms of **nephrotic syndrome**, it is highly unlikely that the glomeruli would appear normal on biopsy.
- Normal glomeruli would not explain the significant kidney dysfunction and proteinuria observed in this patient.
Nephrotic syndrome disorders US Medical PG Question 10: A 36-year-old man comes to the physician for a 4-week history of swollen legs. He has difficulty putting on socks because of the swelling. Two years ago, he was diagnosed with sleep apnea. He takes no medications. He emigrated from Guatemala with his family when he was a child. He is 171 cm (5 ft 6 in) tall and weighs 115 kg (253 lb); BMI is 39 kg/m2. His pulse is 91/min and blood pressure is 135/82 mm Hg. Examination shows periorbital and bilateral lower extremity edema.
Serum
Albumin 3.1 g/dL
Total cholesterol 312 mg/dL
Urine
Blood negative
Protein +4
RBC 1-2/hpf
RBC cast negative
Fatty casts numerous
A renal biopsy is obtained. Which of the following is most likely to be seen under light microscopy of the patient's renal biopsy specimen?
- A. Diffuse thickening of glomerular capillaries
- B. Amyloid deposition in the mesangium
- C. Eosinophilic nodules within the glomeruli
- D. Fibrin crescents within the glomerular space
- E. Segmental sclerosis of the glomeruli (Correct Answer)
Nephrotic syndrome disorders Explanation: ***Segmental sclerosis of the glomeruli***
- The patient presents with **nephrotic syndrome** (edema, proteinuria, hypoalbuminemia, hypercholesterolemia) and **obesity** (BMI 39 kg/m2), which are strong risk factors for **focal segmental glomerulosclerosis (FSGS)**.
- **FSGS** is characterized by **segmental sclerosis** within some glomeruli, often affecting juxtamedullary glomeruli initially.
*Diffuse thickening of glomerular capillaries*
- **Diffuse thickening of glomerular capillaries** (due to subepithelial immune complex deposition causing SPIKES on silver stain) is characteristic of **membranous nephropathy**, which typically presents with nephrotic syndrome but is not directly linked to obesity in the way FSGS is.
- While membranous nephropathy could cause nephrotic syndrome, the association with **morbid obesity** makes FSGS a stronger consideration.
*Amyloid deposition in the mesangium*
- **Amyloid deposition** typically presents with nephrotic syndrome and is associated with chronic inflammatory conditions or plasma cell dyscrasias, not primarily with obesity or the specific presentation described.
- On light microscopy, amyloid appears as **acellular, eosinophilic congophilic deposits** in the mesangium and capillary walls, showing apple-green birefringence under polarized light, which is not suggested by the clinical picture.
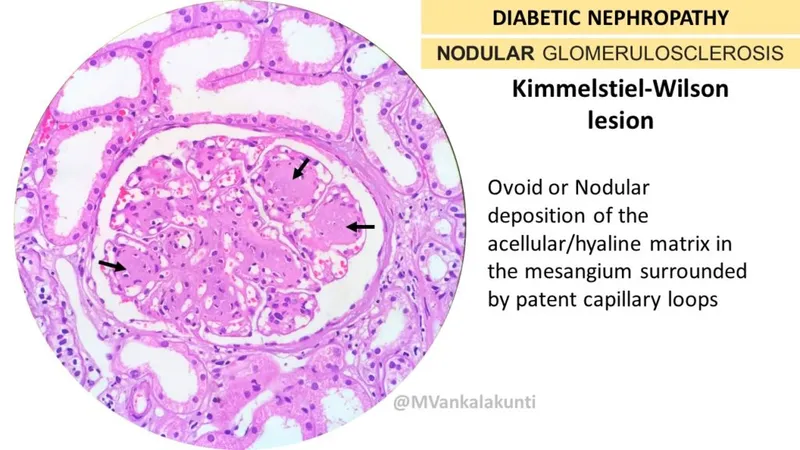
*Eosinophilic nodules within the glomeruli*
- **Eosinophilic nodules within the glomeruli** (Kimmelstiel-Wilson lesions) are characteristic of **diabetic nephropathy**, which commonly causes nephrotic syndrome.
- While the patient is obese, there is no information about diabetes or hyperglycemia to suggest diabetic nephropathy as the primary cause.
*Fibrin crescents within the glomerular space*
- **Fibrin crescents within the glomerular space** are indicative of **rapidly progressive glomerulonephritis (RPGN)**, which typically presents as nephritic syndrome (hematuria, hypertension, azotemia) rather than pure nephrotic syndrome.
- The patient's urine microscopic findings show only 1-2 RBC/hpf and no RBC casts, making RPGN unlikely.
More Nephrotic syndrome disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.