Nephritic syndrome disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nephritic syndrome disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nephritic syndrome disorders US Medical PG Question 1: A 12-year-old boy is found on a routine auditory screening to have mild high frequency hearing impairment. On exam, he has no ear pain, no focal neurological deficits, and no cardiac murmurs. He has not had any recent illness. Laboratory studies show:
Serum:
Creatinine: 0.7 mg/dl
Protein: 3.8 g/dl
Antistreptolysin O titer: 60 Todd units (12-166 normal range)
Urinalysis:
Microscopic heme
Protein: 4+
RBCs: 6/hpf
A kidney biopsy is taken. Which of the following findings is most characteristic of this patient’s disease?
- A. Thickened “tram-track” appearance of basement membrane on electron microscopy
- B. “Spike and dome” appearance on electron microscopy
- C. Crescent-moon shapes on light microscopy
- D. Large eosinophilic nodular lesions on light microscopy
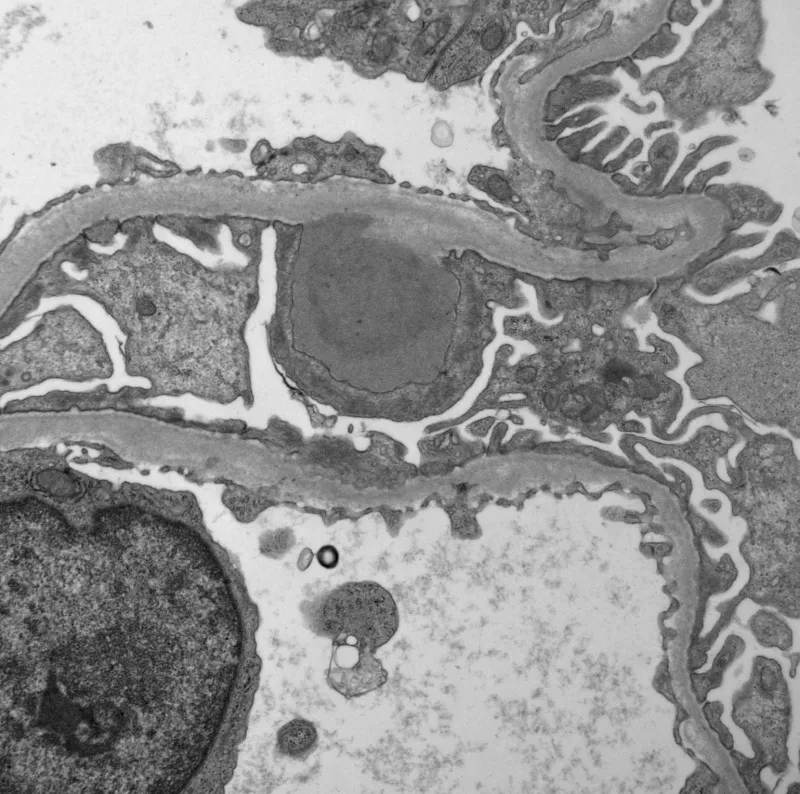
- E. “Basket-weave” pattern of basement membrane on electron microscopy (Correct Answer)
Nephritic syndrome disorders Explanation: ***“Basket-weave” pattern of basement membrane on electron microscopy***
- The combination of **Sensorineural hearing loss**, **microscopic hematuria**, and **proteinuria** in a young boy is highly suggestive of **Alport syndrome**.
- **Alport syndrome** is characterized by mutations in genes encoding **Type IV collagen**, leading to characteristic ultrastructural changes in the glomerular basement membrane, including splitting and thinning, which gives it a **"basket-weave" appearance** on electron microscopy.
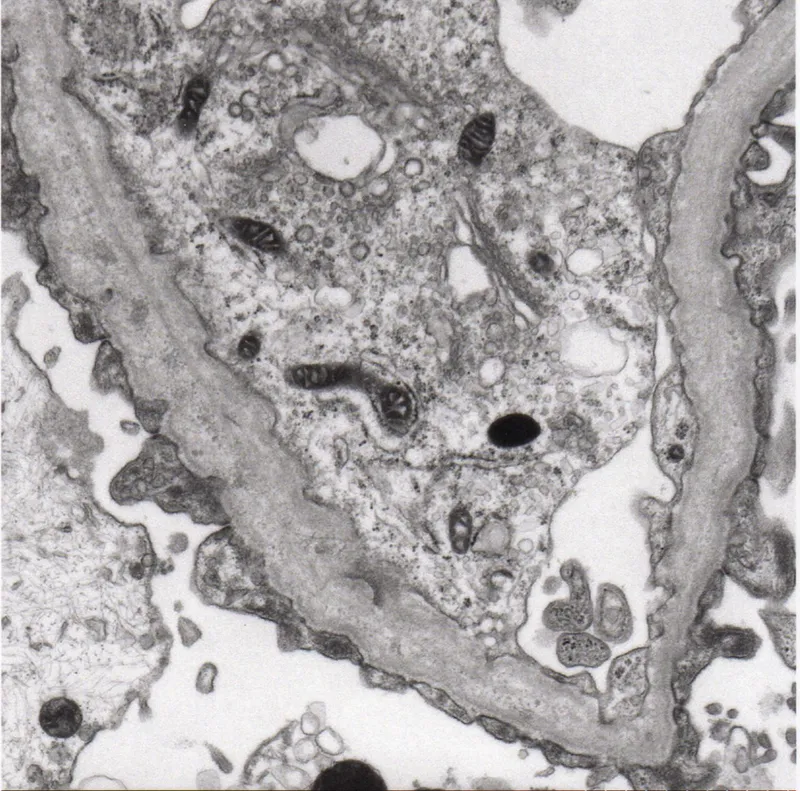
*Thickened “tram-track” appearance of basement membrane on electron microscopy*
- This finding is characteristic of **dense deposit disease** (also known as C3 glomerulopathy), where dense deposits within the glomerular basement membrane lead to a unique pattern.
- While dense deposit disease can cause hematuria and proteinuria, it is not typically associated with the high-frequency hearing loss seen in this patient.
*“Spike and dome” appearance on electron microscopy*
- This is a classic finding in **membranous nephropathy**, due to subepithelial immune deposits and new basement membrane material forming around them.
- Membranous nephropathy typically presents with **nephrotic syndrome** in adults and is not associated with hearing impairment.
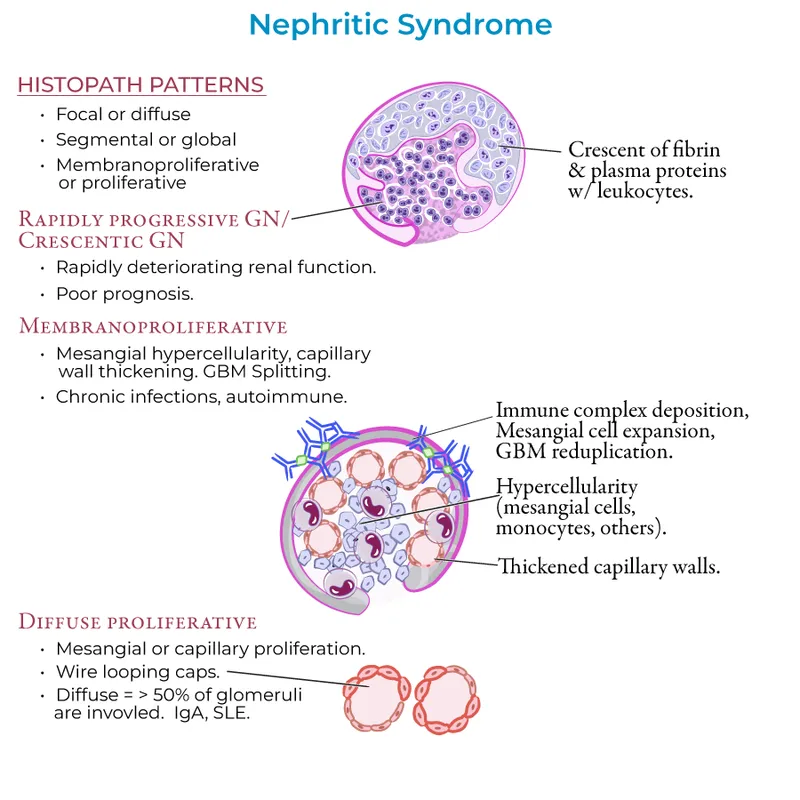
*Crescent-moon shapes on light microscopy*
- **Crescent formation** is characteristic of rapidly progressive glomerulonephritis (RPGN), indicating severe glomerular injury and often associated with systemic vasculitis or anti-GBM disease.
- While RPGN can cause hematuria and proteinuria, the clinical presentation with hearing loss is not typical, and the underlying pathology is different.
*Large eosinophilic nodular lesions on light microscopy*
- This describes the **Kimmelstiel-Wilson lesions** seen in **diabetic nephropathy**, which are pathognomonic for this condition.
- Diabetic nephropathy is a complication of long-standing diabetes and is not consistent with the patient's age or clinical presentation.
Nephritic syndrome disorders US Medical PG Question 2: A 22-year-old man comes to the physician because of a 2-week history of cough and decreased urination. The cough was initially nonproductive, but in the last few days he has coughed up small amounts of blood-tinged sputum with clots. He has not had any fevers, chills, or weight loss. He has smoked one pack of cigarettes daily for 5 years. Pulse is 115/min and blood pressure is 125/66 mm Hg. Physical examination shows dried blood around the lips. Serum studies show a creatinine of 2.9 mg/dL. Results of a serum antineutrophil cytoplasm antibody test are negative. A biopsy specimen of the kidney is most likely to show which of the following light microscopy findings?
- A. Thinning of the basement membrane
- B. Fibrin crescents in Bowman space (Correct Answer)
- C. Expansion of the mesangial matrix
- D. Enlarged and hypercellular glomeruli
- E. Neutrophilic infiltration of the capillaries
Nephritic syndrome disorders Explanation: ***Fibrin crescents in Bowman space***
- The patient's presentation with **hemoptysis** (coughing up blood) and **acute kidney injury** (decreased urination, elevated creatinine 2.9 mg/dL) suggests a **pulmonary-renal syndrome**. The **negative ANCA** is a key distinguishing feature pointing towards **Goodpasture syndrome (anti-GBM disease)**.
- Goodpasture syndrome is characterized by **rapidly progressive glomerulonephritis**, classically showing **crescent formation** (fibrin and proliferating parietal epithelial cells) in Bowman's space on light microscopy. The linear IgG deposition on basement membrane would be seen on immunofluorescence.
*Thinning of the basement membrane*
- This finding is characteristic of **Alport syndrome**, a hereditary nephritis presenting with hematuria, sensorineural hearing loss, and ocular abnormalities.
- The patient's acute presentation with hemoptysis and rapidly progressive renal failure is inconsistent with Alport syndrome, which typically has a more chronic course.
*Expansion of the mesangial matrix*
- **Mesangial matrix expansion** is seen in **diabetic nephropathy** and **IgA nephropathy**.
- While IgA nephropathy can cause hematuria and occasionally upper respiratory symptoms, it typically does not present with significant hemoptysis and the acute, severe renal failure seen here.
*Enlarged and hypercellular glomeruli*
- **Glomerular enlargement and hypercellularity** are features of **post-streptococcal glomerulonephritis** (diffuse proliferative glomerulonephritis).
- The absence of preceding infection history and the prominent hemoptysis with negative ANCA make this less likely than Goodpasture syndrome.
*Neutrophilic infiltration of the capillaries*
- **Neutrophilic infiltration** (endocapillary proliferation) is characteristic of **acute post-infectious glomerulonephritis**.
- The pulmonary-renal syndrome presentation without clear evidence of recent infection and negative ANCA makes this diagnosis unlikely.
Nephritic syndrome disorders US Medical PG Question 3: A 21-year-old male presents to your office with hematuria 3 days after the onset of a productive cough and fever. Following renal biopsy, immunofluorescence shows granular IgA deposits in the glomerular mesangium. Which of the following do you suspect in this patient?
- A. Lipoid nephrosis
- B. Berger’s disease (Correct Answer)
- C. HIV infection
- D. Systemic lupus erythematosus
- E. Poststreptococcal glomerulonephritis
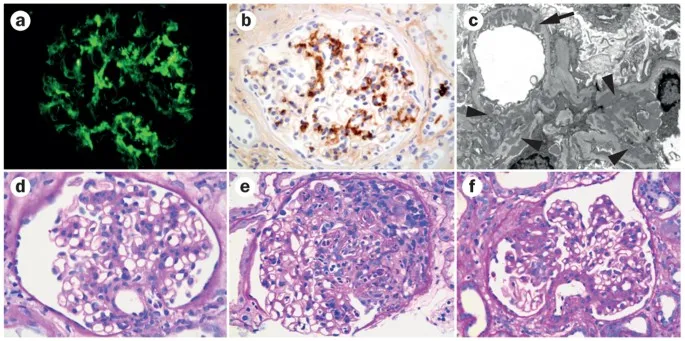
Nephritic syndrome disorders Explanation: ***Berger’s disease***
- The presentation of **hematuria occurring 3 days after a respiratory infection** (productive cough and fever) is characteristic of **IgA nephropathy** or Berger's disease, showing a synpharyngitic pattern.
- **Immunofluorescence showing granular IgA deposits in the glomerular mesangium** is the histological hallmark of IgA nephropathy.
*Lipoid nephrosis*
- This condition is also known as **minimal change disease** and typically presents with **nephrotic syndrome** (heavy proteinuria, edema, hypoalbuminemia), not primarily hematuria.
- Renal biopsy would reveal **effacement of foot processes** on electron microscopy with normal light microscopy and negative immunofluorescence, unlike the IgA deposits described.
*HIV infection*
- HIV can lead to **HIV-associated nephropathy (HIVAN)**, which typically presents as **focal segmental glomerulosclerosis** (FSGS) and can include proteinuria and progressive renal failure.
- While hematuria can occur, the characteristic **IgA deposits in the mesangium** described are not typical for HIVAN.
*Systemic lupus erythematosus*
- **Lupus nephritis** is a common complication of SLE, and can present with hematuria, proteinuria, and various patterns of glomerulonephritis.
- However, immunofluorescence in lupus nephritis usually shows **IgG, IgM, IgA, C3, and C1q deposits** (full-house staining), not isolated IgA deposits.
*Poststreptococcal glomerulonephritis*
- This condition typically presents with **hematuria 10-14 days after a streptococcal infection** (post-infectious glomerulonephritis), a longer latency period than seen in this patient.
- Immunofluorescence would show unique **"lumpy-bumpy" granular deposits of C3 and IgG** along the glomerular basement membrane, often with characteristic subepithelial humps on electron microscopy, rather than mesangial IgA.
Nephritic syndrome disorders US Medical PG Question 4: A 20-year-old man comes to the clinic complaining of fever and a sore throat for 5 days. He receives oral penicillin from his primary doctor. After a day of antibiotic treatment, he developed gross hematuria. As a child, he recalls having multiple episodes of hematuria. The vital signs are within normal limits. On physical examination, pharyngeal edema and cervical lymphadenopathy are present. His laboratory examination reveals the following:
WBC 11,000/mm3
Neutrophils 76%
Lymphocytes 23%
Eosinophils 1%
Platelets 150,000/mm3
Hemoglobin 14 g/dL
Hct 41.2%
BUN 16 mg/dL
Creatinine 0.9 mg/dL
ASO titer 100
Urinalysis shows hematuria but no proteinuria. Immunofluorescence shows granular IgA immune complex deposits in the mesangium. Hepatitis B, hepatitis C, and HIV serology are negative. ASO titers and C3 levels are within normal limits. What is the most likely diagnosis?
- A. Berger’s disease (Correct Answer)
- B. Penicillin-induced hypersensitivity reaction
- C. Celiac disease
- D. Hemolytic uremic syndrome
- E. Post-streptococcal glomerulonephritis
Nephritic syndrome disorders Explanation: ***Berger's disease***
- The co-occurrence of **gross hematuria with an upper respiratory tract infection** (sore throat), the history of **recurrent hematuria**, and the urinalysis showing **hematuria without proteinuria** strongly suggest Berger's disease.
- The definitive diagnostic finding is the **granular IgA immune complex deposits in the mesangium** on immunofluorescence of renal biopsy, which is pathognomonic for IgA nephropathy (Berger's disease).
- The timing is classic for IgA nephropathy: hematuria occurring **concurrently or within 1-2 days** of the upper respiratory infection (synpharyngitic hematuria).
*Penicillin-induced hypersensitivity reaction*
- This condition typically presents with a **rash, fever, and eosinophilia**, not primarily with gross hematuria. While some drug-induced kidney injuries can occur, the specific IgA deposits and recurrent history point away from this.
- The patient's lab results do not show **eosinophilia** (1%), which would be expected in a hypersensitivity reaction.
*Celiac disease*
- Celiac disease is an **autoimmune disorder of the small intestine** triggered by gluten; it primarily causes gastrointestinal symptoms like diarrhea, weight loss, and malabsorption.
- While IgA nephropathy can be associated with celiac disease, celiac disease itself would not cause the presented acute onset of **gross hematuria** or the specific renal biopsy findings.
*Hemolytic uremic syndrome*
- HUS is characterized by the triad of **microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury**.
- This patient does not have **anemia** (Hb 14 g/dL), **thrombocytopenia** (platelets 150,000/mm3), or an elevated **BUN/Creatinine** indicative of acute kidney injury.
*Post-streptococcal glomerulonephritis*
- PSGN typically occurs **1-3 weeks after a streptococcal infection**, presenting with hematuria, proteinuria, edema, and hypertension. In this case, the hematuria occurred **within days of the URI onset**, which is the typical timing for IgA nephropathy, not PSGN.
- Key lab findings for PSGN include **low C3 levels** and significantly elevated **ASO titers**, neither of which (ASO titer 100, C3 within normal limits) were present in this patient.
Nephritic syndrome disorders US Medical PG Question 5: A 35-year-old male with a history of hypertension presents with hematuria and abdominal discomfort. Ultrasound and CT scan reveal large, bilateral cysts in all regions of the kidney. What is the most likely diagnosis?
- A. Henoch-Schonlein purpura
- B. Diabetes mellitus
- C. Aortic stenosis
- D. Berger’s disease
- E. Polycystic kidney disease (Correct Answer)
Nephritic syndrome disorders Explanation: ***Polycystic kidney disease***
- The presentation of **bilateral, large renal cysts** on imaging, along with **hematuria** and **hypertension** in a 35-year-old, is classic for **autosomal dominant polycystic kidney disease (ADPKD)**.
- ADPKD is a systemic disorder that can also cause cysts in other organs and is a leading cause of **end-stage renal disease**.
*Henoch-Schonlein purpura*
- This is a **small-vessel vasculitis** characterized by palpable purpura, arthritis, abdominal pain, and renal involvement (usually IgA nephropathy).
- It does not present with **large, bilateral renal cysts**.
*Diabetes mellitus*
- **Diabetic nephropathy** is a common complication causing progressive kidney damage and is a leading cause of kidney failure.
- However, it typically manifests as **proteinuria**, progressive decline in GFR, and eventually end-stage renal disease, not large renal cysts.
*Aortic stenosis*
- **Aortic stenosis** is a valvular heart disease impacting blood flow from the heart and is entirely unrelated to renal cysts or the described kidney pathology.
- While it can be associated with bleeding disorders (e.g., Heyde's syndrome), it does not directly cause **renal disease or cysts.**
*Berger’s disease*
- Also known as **IgA nephropathy**, Berger's disease is an immune-mediated glomerulonephritis, often presenting with recurrent **gross hematuria**, particularly after an upper respiratory infection.
- It involves inflammation of the glomeruli, not the development of **large renal cysts**.
Nephritic syndrome disorders US Medical PG Question 6: A 13-year-old boy is brought to the physician because of swelling around his eyes for the past 2 days. His mother also notes that his urine became gradually darker during this time. Three weeks ago, he was treated for bacterial tonsillitis. His temperature is 37.6°C (99.7°F), pulse is 79/min, and blood pressure is 158/87 mm Hg. Examination shows periorbital swelling. Laboratory studies show:
Serum
Urea nitrogen 9 mg/dL
Creatinine 1.7 mg/dL
Urine
Protein 2+
RBC 12/hpf
RBC casts numerous
A renal biopsy would most likely show which of the following findings?
- A. Effacement of podocyte foot processes on electron microscopy
- B. Granular deposits of IgG, IgM, and C3 on immunofluorescence (Correct Answer)
- C. Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy
- D. Mesangial IgA deposits on immunofluorescence
- E. "Spike-and-dome" appearance of subepithelial deposits on electron microscopy
Nephritic syndrome disorders Explanation: ***Granular deposits of IgG, IgM, and C3 on immunofluorescence***
- This finding is characteristic of **post-streptococcal glomerulonephritis (PSGN)**, supported by the history of recent tonsillitis, periorbital swelling, dark urine, hypertension, and features of nephritic syndrome (RBC casts, proteinuria).
- The granular deposition pattern reflects the immune complex-mediated nature of PSGN, where **antigen-antibody complexes** deposit in the glomeruli.
*Effacement of podocyte foot processes on electron microscopy*
- This is the hallmark finding in **minimal change disease**, which typically presents with abrupt onset of nephrotic syndrome (severe proteinuria, hypoalbuminemia, edema) without hematuria or hypertension.
- The patient's presentation with **dark urine** (hematuria), hypertension, and RBC casts is inconsistent with minimal change disease.
*Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy*
- This describes the characteristic changes seen in **Alport syndrome**, an inherited disorder affecting collagen IV.
- Alport syndrome presents with **hematuria**, progressive renal failure, and often includes hearing loss and ocular abnormalities, which are not mentioned in this acute presentation.
*Mesangial IgA deposits on immunofluorescence*
- This is the diagnostic feature of **IgA nephropathy (Berger's disease)**.
- IgA nephropathy often presents with **recurrent macroscopic hematuria** occurring concurrent with or shortly after an upper respiratory infection, rather than 2-3 weeks later like PSGN.
*"Spike-and-dome" appearance of subepithelial deposits on electron microscopy*
- This appearance is characteristic of **membranous nephropathy**, which is a common cause of **nephrotic syndrome** in adults.
- Membranous nephropathy typically presents with significant proteinuria and edema, and it is less common in children with acute nephritic symptoms like those described.
Nephritic syndrome disorders US Medical PG Question 7: A 35-year-old woman who was recently ill with an upper respiratory infection presents to the emergency department with weakness in her lower limbs and difficulty breathing. Her symptoms began with a burning sensation in her toes along with numbness. She claims that the weakness has been getting worse over the last few days and now involving her arms and face. Currently, she is unable to get up from the chair without some assistance. Her temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the heart rate is 99/min, the respiratory rate is 12/min, and the oxygen saturation is 95% on room air. On physical examination, she has diminished breath sounds on auscultation of bilateral lung fields with noticeably poor inspiratory effort. Palpation of the lower abdomen reveals a palpable bladder. Strength is 3 out of 5 symmetrically in the lower extremities bilaterally. The sensation is intact. What is the most likely diagnosis?
- A. Guillain-Barré syndrome (Correct Answer)
- B. Adrenoleukodystrophy
- C. Myasthenia Gravis
- D. Multiple sclerosis
- E. Acute disseminated encephalomyelitis
Nephritic syndrome disorders Explanation: ***Guillain-Barré syndrome***
- The patient presents with **ascending paralysis** (weakness starting in lower limbs and progressing upwards to arms and face) following an **upper respiratory infection**, which is a classic presentation of GBS.
- The presence of **respiratory compromise** (difficulty breathing, diminished breath sounds, poor inspiratory effort), **dysautonomia** (palpable bladder due to urinary retention), and the pattern of **symmetrical weakness with intact sensation** are characteristic features of GBS.
- GBS typically presents with areflexia and shows albumino-cytologic dissociation on CSF analysis (elevated protein with normal cell count).
*Adrenoleukodystrophy*
- This is a rare, **X-linked genetic disorder** that primarily affects white matter in the brain and spinal cord, typically presenting in childhood with neurological deficits, not an acute ascending paralysis after an infection.
- It involves demyelination and adrenal insufficiency, which are not suggested by the acute onset and progressive neurological symptoms described.
*Myasthenia Gravis*
- Myasthenia gravis typically presents with **fluctuating muscle weakness** that worsens with activity and improves with rest, often affecting ocular and bulbar muscles first.
- The progression of weakness in this case is constant and ascending, not fluctuating, and there is no mention of characteristic findings like ptosis or diplopia.
*Multiple sclerosis*
- MS is characterized by **demyelinating lesions** in the central nervous system, leading to neurological symptoms that are often **disseminated in space and time**, meaning they affect different parts of the body at different times.
- While it can cause weakness, the acute onset of rapidly progressive, ascending, symmetrical paralysis following an infection is not typical for MS; MS symptoms are usually more insidious or relapsing-remitting.
*Acute disseminated encephalomyelitis*
- ADEM is an **acute inflammatory demyelinating disease** of the central nervous system that typically follows an infection or vaccination, but it usually presents with **encephalopathy** (altered mental status), multifocal neurological deficits, and often affects the brain and spinal cord diffusely.
- While it can cause weakness, the prominent ascending paralysis, intact sensation, and lack of encephalopathy make GBS a more fitting diagnosis.
Nephritic syndrome disorders US Medical PG Question 8: A 19-year-old woman is brought to the emergency room by her mother. She found her daughter pale, cold to the touch, and collapsed next to her bed earlier this morning. The patient has no previous medical or psychiatric history, but the mother does report that her daughter has not had her periods for the last 3 months. In the emergency department, the patient is alert and oriented. Her vitals include: blood pressure 80/60 mm Hg supine, heart rate 55/min. On physical examination, the patient appears pale and emaciated. A urine pregnancy test is negative. She is suspected of having an eating disorder. Which of the following treatment options would be contraindicated in this patient?
- A. Olanzapine
- B. Bupropion (Correct Answer)
- C. Cognitive-behavioral therapy
- D. Selective serotonin reuptake inhibitors
- E. High caloric food
Nephritic syndrome disorders Explanation: ***Bupropion***
- **Bupropion** is contraindicated in patients with **anorexia nervosa** or **bulimia nervosa** due to the increased risk of **seizures**.
- Patients with eating disorders often have electrolyte imbalances and metabolic derangements, which further lower the seizure threshold.
*Olanzapine*
- **Olanzapine**, an atypical antipsychotic, can be used in patients with anorexia nervosa to help with **weight gain** and reduce rigid thinking patterns.
- It is particularly useful when significant **anxiety** or **psychotic features** are present, which can exacerbate the eating disorder.
*Cognitive-behavioral therapy*
- **Cognitive-behavioral therapy (CBT)** is a cornerstone of treatment for eating disorders, including anorexia nervosa.
- It helps patients identify and change distorted thoughts and behaviors related to food, weight, and body image.
*Selective serotonin reuptake inhibitors*
- **SSRIs** may be used in anorexia nervosa, primarily after **weight restoration**, to address co-occurring **depression** or **anxiety disorders**.
- They are generally not effective for acute weight gain but can prevent relapse and treat underlying mood disturbances.
*High caloric food*
- Providing **high-caloric food** and nutritional rehabilitation is essential in managing anorexia nervosa to reverse the state of **malnutrition**.
- This must be done carefully to avoid **refeeding syndrome**, a potentially fatal shift in fluid and electrolytes that can occur with rapid refeeding.
Nephritic syndrome disorders US Medical PG Question 9: A 32-year-old man visits his family physician for 10 months of persistent left flank pain, weight loss, and fatigue. Also, he has had hematuria a couple of times in the last month. His mother was diagnosed and treated for a pheochromocytoma when she was 36 years old, and his father died at 45 years due to myocardial infarction. His personal medical history is not relevant. He does not smoke and used to be a varsity athlete in high school and university. Physical examination shows temporal wasting, pale mucous membranes and palms, a palpable mass in the left flank, and a varicocele that does not reduce upon recumbency. His family physician sends the patient to the emergency department for an abdominal computed tomography (CT) scan, which shows a complex left renal mass and a hemangioblastoma in T10. A biopsy of the renal mass is ordered by the oncology team, which demonstrates compact cells with prominent nucleoli, eosinophilic cytoplasm within a network of a small and thin-walled vasculature. What is the most likely type of tumor in this patient?
- A. Collecting duct carcinoma
- B. Clear-cell carcinoma (Correct Answer)
- C. Oncocytic carcinoma
- D. Papillary carcinoma
- E. Chromophobe carcinoma
Nephritic syndrome disorders Explanation: ***Clear-cell carcinoma***
- This patient's presentation with a **renal mass**, hemangioblastoma, a family history of **pheochromocytoma** (his mother), and an early death of his father (likely from heart disease associated with pheochromocytoma) is highly suggestive of **Von Hippel-Lindau (VHL) syndrome**. **Clear cell renal cell carcinoma** is the most common renal tumor associated with VHL syndrome.
- The biopsy description of **compact cells with prominent nucleoli**, **eosinophilic cytoplasm**, and a **network of small and thin-walled vasculature** is characteristic of clear cell renal cell carcinoma.
*Collecting duct carcinoma*
- This is a rare and aggressive subtype of **renal cell carcinoma** that typically presents with a mass in the renal medulla, often with central necrosis.
- Its histological features involve atypical cells arranged in **tubules or ducts**, which does not match the description of compact cells with eosinophilic cytoplasm.
*Oncocytic carcinoma*
- **Oncocytic carcinoma** is a rare and generally benign tumor. It is characterized histologically by cells with abundant, granular eosinophilic cytoplasm.
- While it has eosinophilic cytoplasm, it lacks the prominent nucleoli and compact cell arrangement seen in the biopsy, and it is not typically associated with VHL syndrome.
*Papillary carcinoma*
- **Papillary carcinoma** is characterized by cells arranged in papillary formations or tubular structures. It is generally associated with different genetic syndromes (e.g., hereditary papillary renal carcinoma).
- The histological description provided, particularly the "compact cells" and vasculature, does not fit the typical papillary architecture.
*Chromophobe carcinoma*
- **Chromophobe carcinoma** is characterized by large cells with distinct cell borders and pale, flocculent cytoplasm. It typically has a good prognosis.
- This type of carcinoma is generally not associated with VHL syndrome and its histological features do not align with the biopsy description of compact cells with eosinophilic cytoplasm and prominent nucleoli.
Nephritic syndrome disorders US Medical PG Question 10: A 12-year-old boy comes to the physician for the evaluation of intermittent blood-tinged urine for several months. Four months ago, he had an episode of fever and sore throat that resolved without treatment after 5 days. During the past 2 years, he has also had recurrent episodes of swelling of his face and feet. 5 years ago, he was diagnosed with mild bilateral sensorineural hearing loss. His brother died of a progressive kidney disease at the age of 23. The patient appears pale. His temperature is 37°C (98.6°F), pulse is 70/min, and blood pressure is 145/85 mm Hg. Slit lamp examination shows a conical protrusion of both lenses. Laboratory studies show a hemoglobin concentration of 11 g/dL, urea nitrogen concentration of 40 mg/dL, and creatinine concentration of 2.4 mg/dL. Urinalysis shows:
Blood 2+
Protein 1+
RBC 5–7/hpf
RBC casts rare
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. IgA deposits
- B. WT1 gene mutation
- C. Defective type IV collagen (Correct Answer)
- D. Autosomal-recessive kidney disease
- E. Type II hypersensitivity reaction
Nephritic syndrome disorders Explanation: ***Defective type IV collagen***
- This patient presents with a classic triad of symptoms: **progressive kidney disease** (elevated creatinine, blood-tinged urine, family history), **sensorineural hearing loss**, and **ocular abnormalities** (lenticonus on slit lamp exam). These findings are highly suggestive of **Alport syndrome**, which is caused by a defect in **type IV collagen**.
- The family history of a brother dying of progressive kidney disease at a young age further supports a genetic cause, and the intermittent blood-tinged urine after an upper respiratory infection can be a feature of Alport syndrome, often misinterpreted as IgA nephropathy early in its course.
*IgA deposits*
- **IgA nephropathy** can present with recurrent episodes of gross hematuria, often following an upper respiratory infection, similar to the initial presentation of this patient's blood-tinged urine.
- However, IgA nephropathy typically does not involve **sensorineural hearing loss** or **ocular abnormalities** like lenticonus.
*WT1 gene mutation*
- A **WT1 gene mutation** is associated with **Denys-Drash syndrome** and **Frasier syndrome**, which involve nephropathy and, in some cases, gonadal abnormalities or ambiguous genitalia.
- While these can cause kidney disease, they do not typically present with the characteristic ocular findings (lenticonus) or sensorineural hearing loss seen in this patient.
*Autosomal-recessive kidney disease*
- While Alport syndrome can have autosomal recessive inheritance (10-15% of cases), this option is too broad and does not specify the underlying **molecular defect** (type IV collagen).
- The family history pattern here (affected brother, male proband) is more consistent with **X-linked Alport syndrome** (85% of cases), and this non-specific option does not pinpoint the actual pathogenic mechanism that links all the patient's symptoms.
*Type II hypersensitivity reaction*
- A **type II hypersensitivity reaction** involves antibody-mediated cellular destruction or dysfunction, such as in Goodpasture syndrome, where antibodies attack the glomerular basement membrane.
- This mechanism does not explain the long-standing, progressive nature of kidney disease combined with sensorineural hearing loss and ocular defects. Instead, these are characteristic of an underlying structural protein defect.
More Nephritic syndrome disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.