Glomerular diseases overview US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Glomerular diseases overview. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Glomerular diseases overview US Medical PG Question 1: A 43-year-old man comes to the physician for a 1-week history of swelling around his eyes and decreased urination. His pulse is 87/min, and blood pressure is 152/95 mm Hg. Physical examination shows 1+ periorbital and pretibial edema. Serum studies show a urea nitrogen concentration of 21 mg/dL and a creatinine concentration of 1.4 mg/dL. Urinalysis shows 3+ blood and 1+ protein. Further evaluation of this patient is most likely to show which of the following?
- A. Urinary rhomboid crystals
- B. Renal interstitial inflammation
- C. Hypoalbuminemia
- D. Detached renal tubular epithelial cells
- E. Red blood cell casts (Correct Answer)
Glomerular diseases overview Explanation: ***Red blood cell casts***
- The patient's presentation with **periorbital and pretibial edema**, **hypertension**, elevated **creatinine**, **hematuria** (3+ blood), and mild **proteinuria** (1+ protein) is highly suggestive of **acute glomerulonephritis**.
- **Red blood cell casts** are pathognomonic for **glomerulonephritis**, indicating that red blood cells are leaking from the glomeruli and congealing in the renal tubules.
*Urinary rhomboid crystals*
- **Urinary rhomboid crystals** are typically associated with conditions like **uric acid nephrolithiasis** or gout, which are not suggested by the patient's symptoms or lab findings.
- Their presence would indicate a risk for **kidney stones**, not evidence of glomerular inflammation.
*Renal interstitial inflammation*
- **Renal interstitial inflammation** is characteristic of **acute interstitial nephritis**, which often presents with fever, rash, eosinophilia, and flank pain, usually due to drug reactions or infections.
- While kidney injury can occur, the primary findings of **hematuria** and **proteinuria** in this context strongly point away from an interstitial process as the initial diagnosis.
*Hypoalbuminemia*
- **Hypoalbuminemia** is a hallmark of **nephrotic syndrome**, characterized by severe proteinuria (>3.5 g/day), significant edema, and hyperlipidemia.
- This patient has only 1+ proteinuria, which is not severe enough to cause significant hypoalbuminemia or the full nephrotic picture.
*Detached renal tubular epithelial cells*
- **Detached renal tubular epithelial cells** and **tubular cell casts** are characteristic findings in **acute tubular necrosis (ATN)**, usually resulting from ischemia or nephrotoxins.
- While ATN can cause acute kidney injury, the prominent **hematuria** and **hypertension** in this case are more indicative of a glomerular process than tubular damage.
Glomerular diseases overview US Medical PG Question 2: A 52-year-old man presents to the Emergency Department because of bilateral leg swelling and puffiness of both eyes in the morning. His symptoms started about 2 weeks ago. He denies smoking or alcohol use and his family history is noncontributory. Today, his vital signs include a temperature of 36.8°C (98.2°F), blood pressure of 162/87 mm Hg, and a pulse of 85/min. On physical examination, he is jaundiced and there is hepatosplenomegaly and 2+ lower extremity edema up to the mid-thigh. Laboratory results are shown:
Anti-HCV
reactive
Serum albumin
3 g/dL
Urine dipstick
3+ protein
Urinalysis
10–15 red blood cells/high power field and red cell casts
Which of the following is a feature of this patient’s condition?
- A. Few immune complex deposits
- B. Phospholipase A2 receptor antibodies
- C. Subendothelial immune complex deposits (Correct Answer)
- D. Renal vasoconstriction and altered autoregulation
- E. Normal complement level
Glomerular diseases overview Explanation: ***Subendothelial immune complex deposits***
- The patient's presentation with **jaundice**, **hepatosplenomegaly**, **reactive anti-HCV**, and **nephritic-range proteinuria with red cell casts** and edema points to **hepatitis C-associated membranoproliferative glomerulonephritis (MPGN)**, also known as cryoglobulinemic glomerulonephritis.
- MPGN is characterized by **immune complex deposition** within the glomerular capillary walls, specifically in the subendothelial space, often with C3 deposits and mesangial proliferation.
*Few immune complex deposits*
- This is incorrect as **MPGN type I** (the most common type, frequently associated with hepatitis C) is characterized by prominent **immune complex deposition**.
- Conditions with few immune complex deposits often include **minimal change disease** or some forms of **focal segmental glomerulosclerosis (FSGS)**, which do not fit the entire clinical picture.
*Phospholipase A2 receptor antibodies*
- These antibodies are strongly associated with **idiopathic membranous nephropathy**, a different form of glomerulonephritis presenting primarily with **nephrotic syndrome**.
- While membranous nephropathy can cause proteinuria, the presence of **red cell casts** and **hepatosplenomegaly** with **HCV infection** makes MPGN much more likely.
*Renal vasoconstriction and altered autoregulation*
- This describes the pathophysiology of **hepatorenal syndrome**, a complication of advanced liver disease characterized by functional renal failure without intrinsic kidney disease.
- However, the presence of **proteinuria** and especially **red cell casts** in the urine indicates significant glomerular inflammation and **intrinsic kidney disease**, rather than functional renal impairment.
*Normal complement level*
- In **HCV-associated MPGN**, circulating **mixed cryoglobulins** lead to widespread immune complex formation and **complement activation** (primarily via the classical pathway), resulting in **decreased C4 and C3 complement levels**.
- A normal complement level would be unusual for active cryoglobulinemic glomerulonephritis.
Glomerular diseases overview US Medical PG Question 3: A 45-year-old man presents with a 3-day history of right-sided flank pain due to a lodged ureteral stone. What changes would be expected to be seen at the level of glomerular filtration?
- A. Increase in glomerular capillary oncotic pressure
- B. Increase in Bowman's space oncotic pressure
- C. Increase in filtration fraction
- D. Increase in Bowman's space hydrostatic pressure (Correct Answer)
- E. No change in filtration fraction
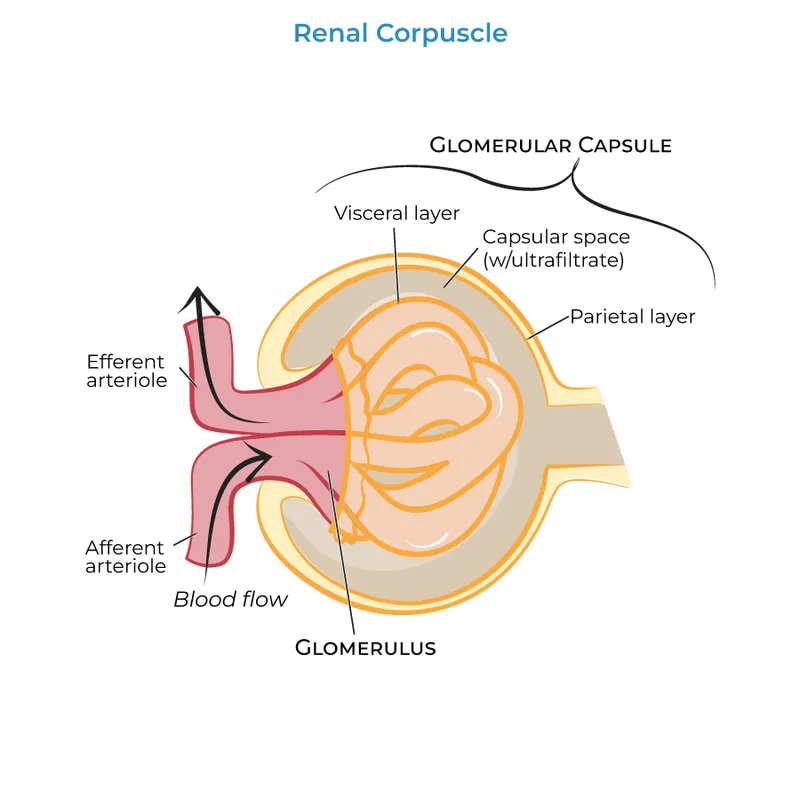
Glomerular diseases overview Explanation: ***Increase in Bowman's space hydrostatic pressure***
- A lodged ureteral stone causes **obstruction** of urine flow, leading to a backup of fluid in the renal tubules and eventually into **Bowman's space**.
- This increased fluid volume in Bowman's space directly raises its **hydrostatic pressure**, which opposes glomerular filtration, thereby reducing the net filtration pressure.
*Increase in glomerular capillary oncotic pressure*
- **Glomerular capillary oncotic pressure** primarily reflects the protein concentration within the glomerular capillaries, which would not be directly increased by a ureteral stone.
- This parameter typically rises when fluid is filtered out, increasing protein concentration in the remaining blood, but not as the initial insult from obstruction.
*Increase in Bowman's space oncotic pressure*
- **Bowman's space oncotic pressure** is normally very low because the glomerular filtration barrier prevents significant protein filtration.
- An increase in this pressure would imply increased protein leakage into Bowman's space, which is not a direct consequence of a ureteral obstruction.
*Increase in filtration fraction*
- The **filtration fraction** is the ratio of glomerular filtration rate (GFR) to renal plasma flow.
- Ureteral obstruction typically **decreases GFR** due to increased Bowman's space hydrostatic pressure, which would lead to a reduction, not an increase, in the filtration fraction, assuming renal plasma flow remains stable or slightly reduced.
*No change in filtration fraction*
- Ureteral obstruction significantly impacts the forces driving glomerular filtration, primarily by increasing **Bowman's space hydrostatic pressure**.
- This change inevitably leads to a **decrease in GFR**, thus altering the filtration fraction, meaning it would not remain unchanged.
Glomerular diseases overview US Medical PG Question 4: A 44-year-old man comes to the physician because of a 2-week history of lower extremity swelling and frothy urine. He has a history of chronic hepatitis C infection. Physical examination shows 3+ pitting edema of the lower legs and ankles. Further evaluation of this patient is most likely to show which of the following?
- A. Decreased cholesterol
- B. Decreased blood urea nitrogen
- C. Increased antithrombin III
- D. Decreased cystatin C
- E. Increased lipoproteins (Correct Answer)
Glomerular diseases overview Explanation: ***Increased lipoproteins***
- The patient's symptoms (**lower extremity swelling**, **frothy urine**) and history of **hepatitis C infection** are highly suggestive of **nephrotic syndrome**.
- **Nephrotic syndrome** is characterized by severe proteinuria, leading to **hypoalbuminemia**, edema, and often **compensatory hyperlipidemia** (increased lipoproteins) due to increased hepatic synthesis of lipids.
*Decreased cholesterol*
- **Nephrotic syndrome** typically leads to **hyperlipidemia**, including **elevated cholesterol levels**, not decreased, as the liver compensates for protein loss by increasing lipid synthesis.
- This is a key diagnostic feature differentiating nephrotic syndrome from other conditions that might cause edema.
*Decreased blood urea nitrogen*
- In **nephrotic syndrome**, kidney function might initially be preserved, or kidney injury could lead to **increased BUN** if glomerular filtration rate (GFR) significantly declines.
- **Decreased BUN** is usually seen in conditions like liver failure, overhydration, or low protein diet, which are not suggested by the clinical picture.
*Increased antithrombin III*
- Patients with **nephrotic syndrome** typically have **decreased levels of antithrombin III** due to urinary loss of this anticoagulant protein, increasing their risk of **thrombosis**.
- Therefore, an increase in antithrombin III would be highly unlikely and is contrary to the pathophysiology of nephrotic syndrome.
*Decreased cystatin C*
- **Cystatin C** is an endogenous marker of **renal function** (similar to creatinine), and its levels usually **increase** when glomerular filtration rate (GFR) decreases, indicating kidney impairment.
- A decrease in cystatin C would suggest improved or hyper-filtration, which is not consistent with the signs of kidney damage seen in nephrotic syndrome.
Glomerular diseases overview US Medical PG Question 5: A 6-year-old boy presents to your office with hematuria. Two weeks ago the patient had symptoms of a sore throat and fever. Although physical exam is unremarkable, laboratory results show a decreased serum C3 level and an elevated anti-DNAse B titer. Which of the following would you most expect to see on renal biopsy?
- A. Immune complex deposits with a "spike and dome" appearance on electron microscopy
- B. Large, hypercellular glomeruli on light microscopy (Correct Answer)
- C. Wirelooping and hyaline thrombi on light microscopy
- D. Polyclonal IgA deposition on immunofluorescence
- E. Antibodies to GBM resulting in a linear immunofluorescence pattern
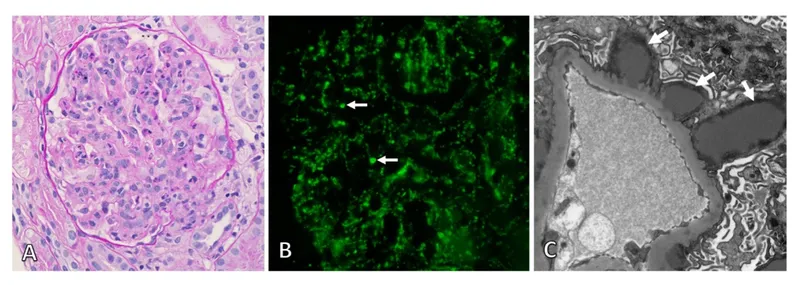
Glomerular diseases overview Explanation: ***Large, hypercellular glomeruli on light microscopy***
- The clinical presentation, including recent **sore throat**, **hematuria**, decreased **C3**, and elevated **anti-DNAse B titer**, is highly suggestive of **post-streptococcal glomerulonephritis (PSGN)**.
- On light microscopy, PSGN characteristically shows **diffuse proliferative glomerulonephritis** with **enlarged, hypercellular glomeruli** due to inflammatory cell infiltration and proliferation of intrinsic glomerular cells.
*Immune complex deposits with a "spike and dome" appearance on electron microscopy*
- This "spike and dome" appearance refers to **subepithelial deposits** with new basement membrane formation, which is characteristic of **membranous nephropathy**, not PSGN.
- Membranous nephropathy typically presents with **nephrotic syndrome** in adults, which is different from the child's presentation here.
*Wirelooping and hyaline thrombi on light microscopy*
- These features, particularly **"wire-loop" lesions** and **hyaline thrombi**, suggest severe **lupus nephritis**, a manifestation of **systemic lupus erythematosus**.
- Lupus nephritis often presents with a range of kidney pathologies and systemic symptoms not seen in this patient.
*Polyclonal IgA deposition on immunofluorescence*
- **IgA deposition** in the mesangium is the hallmark of **IgA nephropathy (Berger's disease)**, which typically presents with recurrent hematuria, often after an upper respiratory infection.
- While there is hematuria and a recent infection, the decreased C3 and elevated anti-DNAse B titer point away from IgA nephropathy.
*Antibodies to GBM resulting in a linear immunofluorescence pattern*
- A **linear pattern** of IgG deposits along the glomerular basement membrane (GBM) is characteristic of **Goodpasture syndrome (anti-GBM disease)**.
- This condition involves antibodies specifically targeting the GBM and often presents with rapidly progressive glomerulonephritis and pulmonary hemorrhage, which are not described here.
Glomerular diseases overview US Medical PG Question 6: A 21-year-old male presents to your office with hematuria 3 days after the onset of a productive cough and fever. Following renal biopsy, immunofluorescence shows granular IgA deposits in the glomerular mesangium. Which of the following do you suspect in this patient?
- A. Lipoid nephrosis
- B. Berger’s disease (Correct Answer)
- C. HIV infection
- D. Systemic lupus erythematosus
- E. Poststreptococcal glomerulonephritis
Glomerular diseases overview Explanation: ***Berger’s disease***
- The presentation of **hematuria occurring 3 days after a respiratory infection** (productive cough and fever) is characteristic of **IgA nephropathy** or Berger's disease, showing a synpharyngitic pattern.
- **Immunofluorescence showing granular IgA deposits in the glomerular mesangium** is the histological hallmark of IgA nephropathy.
*Lipoid nephrosis*
- This condition is also known as **minimal change disease** and typically presents with **nephrotic syndrome** (heavy proteinuria, edema, hypoalbuminemia), not primarily hematuria.
- Renal biopsy would reveal **effacement of foot processes** on electron microscopy with normal light microscopy and negative immunofluorescence, unlike the IgA deposits described.
*HIV infection*
- HIV can lead to **HIV-associated nephropathy (HIVAN)**, which typically presents as **focal segmental glomerulosclerosis** (FSGS) and can include proteinuria and progressive renal failure.
- While hematuria can occur, the characteristic **IgA deposits in the mesangium** described are not typical for HIVAN.
*Systemic lupus erythematosus*
- **Lupus nephritis** is a common complication of SLE, and can present with hematuria, proteinuria, and various patterns of glomerulonephritis.
- However, immunofluorescence in lupus nephritis usually shows **IgG, IgM, IgA, C3, and C1q deposits** (full-house staining), not isolated IgA deposits.
*Poststreptococcal glomerulonephritis*
- This condition typically presents with **hematuria 10-14 days after a streptococcal infection** (post-infectious glomerulonephritis), a longer latency period than seen in this patient.
- Immunofluorescence would show unique **"lumpy-bumpy" granular deposits of C3 and IgG** along the glomerular basement membrane, often with characteristic subepithelial humps on electron microscopy, rather than mesangial IgA.
Glomerular diseases overview US Medical PG Question 7: A 37-year-old African-American man presents to his primary care provider with a history of fatigue and nausea that started about 6 months ago. His symptoms have slowly gotten worse and now he has trouble climbing the stairs to his 3rd floor apartment without resting. Past medical history is significant for poorly controlled HIV and a remote history of heroin addiction. Today his temperature is 36.9°C (98.4°F), the blood pressure is 118/72 mm Hg, and the pulse is 75/min. Physical examination reveals morbid obesity and 1+ pitting edema of both lower extremities. Urine dipstick reveals 2+ proteinuria. Urinalysis shows no abnormal findings. Which of the following is the most likely etiology of this patient condition?
- A. Amyloidosis
- B. Focal segmental glomerulosclerosis (Correct Answer)
- C. Membranoproliferative glomerulonephritis
- D. Minimal change disease
- E. Membranous nephropathy
Glomerular diseases overview Explanation: **Focal segmental glomerulosclerosis**
- **HIV-associated nephropathy (HIVAN)**, a form of FSGS, is highly probable in this patient given their history of **poorly controlled HIV**, African-American ethnicity, and presentation with proteinuria and edema.
- **HIVAN** typically presents as **nephrotic syndrome** with rapid progression to end-stage renal disease, particularly in African-American individuals with high viral loads.
*Amyloidosis*
- While amyloidosis can cause proteinuria and nephrotic syndrome, it is typically associated with **chronic inflammatory conditions** or **monoclonal gammopathy**, neither of which are prominent in this patient's history.
- The patient's presentation with poorly controlled HIV and African-American ethnicity makes FSGS a more specific and likely diagnosis.
*Membranoproliferative glomerulonephritis*
- **MPGN** is often associated with **chronic infections like hepatitis C** or **autoimmune diseases**, which are not indicated in this case.
- While it can manifest with proteinuria and edema, the strong association with HIV in an African-American patient points away from MPGN as the primary etiology.
*Minimal change disease*
- **Minimal change disease** classically causes **nephrotic syndrome in children** and is often responsive to corticosteroids.
- Its etiology is typically idiopathic, and it is less likely to present in an adult with a history of HIV and progressive symptoms over several months.
*Membranous nephropathy*
- **Membranous nephropathy** is a common cause of nephrotic syndrome in adults and can be idiopathic or secondary to conditions like **lupus**, **hepatitis B**, or certain medications.
- The patient's specific risk factors, particularly HIV and African-American ethnicity, are not the typical associations for membranous nephropathy, making FSGS a more fitting diagnosis.
Glomerular diseases overview US Medical PG Question 8: A 13-year-old boy is brought to the physician because of swelling around his eyes for the past 2 days. His mother also notes that his urine became gradually darker during this time. Three weeks ago, he was treated for bacterial tonsillitis. His temperature is 37.6°C (99.7°F), pulse is 79/min, and blood pressure is 158/87 mm Hg. Examination shows periorbital swelling. Laboratory studies show:
Serum
Urea nitrogen 9 mg/dL
Creatinine 1.7 mg/dL
Urine
Protein 2+
RBC 12/hpf
RBC casts numerous
A renal biopsy would most likely show which of the following findings?
- A. Effacement of podocyte foot processes on electron microscopy
- B. Granular deposits of IgG, IgM, and C3 on immunofluorescence (Correct Answer)
- C. Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy
- D. Mesangial IgA deposits on immunofluorescence
- E. "Spike-and-dome" appearance of subepithelial deposits on electron microscopy
Glomerular diseases overview Explanation: ***Granular deposits of IgG, IgM, and C3 on immunofluorescence***
- This finding is characteristic of **post-streptococcal glomerulonephritis (PSGN)**, supported by the history of recent tonsillitis, periorbital swelling, dark urine, hypertension, and features of nephritic syndrome (RBC casts, proteinuria).
- The granular deposition pattern reflects the immune complex-mediated nature of PSGN, where **antigen-antibody complexes** deposit in the glomeruli.
*Effacement of podocyte foot processes on electron microscopy*
- This is the hallmark finding in **minimal change disease**, which typically presents with abrupt onset of nephrotic syndrome (severe proteinuria, hypoalbuminemia, edema) without hematuria or hypertension.
- The patient's presentation with **dark urine** (hematuria), hypertension, and RBC casts is inconsistent with minimal change disease.
*Splitting and alternating thickening and thinning of the glomerular basement membrane on light microscopy*
- This describes the characteristic changes seen in **Alport syndrome**, an inherited disorder affecting collagen IV.
- Alport syndrome presents with **hematuria**, progressive renal failure, and often includes hearing loss and ocular abnormalities, which are not mentioned in this acute presentation.
*Mesangial IgA deposits on immunofluorescence*
- This is the diagnostic feature of **IgA nephropathy (Berger's disease)**.
- IgA nephropathy often presents with **recurrent macroscopic hematuria** occurring concurrent with or shortly after an upper respiratory infection, rather than 2-3 weeks later like PSGN.
*"Spike-and-dome" appearance of subepithelial deposits on electron microscopy*
- This appearance is characteristic of **membranous nephropathy**, which is a common cause of **nephrotic syndrome** in adults.
- Membranous nephropathy typically presents with significant proteinuria and edema, and it is less common in children with acute nephritic symptoms like those described.
Glomerular diseases overview US Medical PG Question 9: A 56-year-old woman presents to the emergency department with several episodes in which she felt "dizzy." She has had these symptoms on and off for the past year and can recall no clear exacerbating factor or time of day when her symptoms occur. She has a perpetual sensation of fullness in her ear but otherwise has no symptoms currently. Her temperature is 97.6°F (36.4°C), blood pressure is 122/77 mmHg, pulse is 85/min, respirations are 13/min, and oxygen saturation is 98% on room air. Cardiopulmonary exam is unremarkable. The patient's gait is stable. Which of the following is also likely to be found in this patient?
- A. Gradually improving symptoms
- B. Conductive hearing loss
- C. Positional vertigo
- D. Sensorineural hearing loss (Correct Answer)
- E. Vertical nystagmus
Glomerular diseases overview Explanation: ***Sensorineural hearing loss***
- The sensation of **aural fullness**, recurrent dizzy spells without clear triggers, and the episodic nature of symptoms are classic for **Ménière's disease**.
- **Ménière's disease** is characterized by the triad of **vertigo**, **tinnitus**, and **sensorineural hearing loss**, often accompanied by ear fullness.
*Gradually improving symptoms*
- **Ménière's disease** is a chronic, progressive condition, and symptoms typically **fluctuate** in severity and can worsen over time, rather than gradually improving.
- While periods of remission can occur, the underlying pathology does make a steady improvement unlikely without intervention.
*Conductive hearing loss*
- **Conductive hearing loss** results from problems with sound transmission to the inner ear, such as **earwax** or **ossicular chain dysfunction**.
- **Ménière's disease** specifically affects the inner ear (cochlea and vestibular system), leading to **sensorineural hearing loss** due to endolymphatic hydrops.
*Positional vertigo*
- **Positional vertigo** suggests conditions like **Benign Paroxysmal Positional Vertigo (BPPV)**, where vertigo is triggered by specific head movements due to otolith displacement.
- In this patient, the vertigo is described as recurrent and "on and off" without "clear exacerbating factor," which is less consistent with positional vertigo.
*Vertical nystagmus*
- **Vertical nystagmus** is typically indicative of **central vestibular lesions** or brainstem dysfunction.
- The symptoms presented, including aural fullness and episodic dizziness, point towards a **peripheral vestibular disorder** like Ménière's disease, which usually causes horizontal or rotatory nystagmus during acute attacks.
Glomerular diseases overview US Medical PG Question 10: A 36-year-old man comes to the physician for a 4-week history of swollen legs. He has difficulty putting on socks because of the swelling. Two years ago, he was diagnosed with sleep apnea. He takes no medications. He emigrated from Guatemala with his family when he was a child. He is 171 cm (5 ft 6 in) tall and weighs 115 kg (253 lb); BMI is 39 kg/m2. His pulse is 91/min and blood pressure is 135/82 mm Hg. Examination shows periorbital and bilateral lower extremity edema.
Serum
Albumin 3.1 g/dL
Total cholesterol 312 mg/dL
Urine
Blood negative
Protein +4
RBC 1-2/hpf
RBC cast negative
Fatty casts numerous
A renal biopsy is obtained. Which of the following is most likely to be seen under light microscopy of the patient's renal biopsy specimen?
- A. Diffuse thickening of glomerular capillaries
- B. Amyloid deposition in the mesangium
- C. Eosinophilic nodules within the glomeruli
- D. Fibrin crescents within the glomerular space
- E. Segmental sclerosis of the glomeruli (Correct Answer)
Glomerular diseases overview Explanation: ***Segmental sclerosis of the glomeruli***
- The patient presents with **nephrotic syndrome** (edema, proteinuria, hypoalbuminemia, hypercholesterolemia) and **obesity** (BMI 39 kg/m2), which are strong risk factors for **focal segmental glomerulosclerosis (FSGS)**.
- **FSGS** is characterized by **segmental sclerosis** within some glomeruli, often affecting juxtamedullary glomeruli initially.
*Diffuse thickening of glomerular capillaries*
- **Diffuse thickening of glomerular capillaries** (due to subepithelial immune complex deposition causing SPIKES on silver stain) is characteristic of **membranous nephropathy**, which typically presents with nephrotic syndrome but is not directly linked to obesity in the way FSGS is.
- While membranous nephropathy could cause nephrotic syndrome, the association with **morbid obesity** makes FSGS a stronger consideration.
*Amyloid deposition in the mesangium*
- **Amyloid deposition** typically presents with nephrotic syndrome and is associated with chronic inflammatory conditions or plasma cell dyscrasias, not primarily with obesity or the specific presentation described.
- On light microscopy, amyloid appears as **acellular, eosinophilic congophilic deposits** in the mesangium and capillary walls, showing apple-green birefringence under polarized light, which is not suggested by the clinical picture.
*Eosinophilic nodules within the glomeruli*
- **Eosinophilic nodules within the glomeruli** (Kimmelstiel-Wilson lesions) are characteristic of **diabetic nephropathy**, which commonly causes nephrotic syndrome.
- While the patient is obese, there is no information about diabetes or hyperglycemia to suggest diabetic nephropathy as the primary cause.
*Fibrin crescents within the glomerular space*
- **Fibrin crescents within the glomerular space** are indicative of **rapidly progressive glomerulonephritis (RPGN)**, which typically presents as nephritic syndrome (hematuria, hypertension, azotemia) rather than pure nephrotic syndrome.
- The patient's urine microscopic findings show only 1-2 RBC/hpf and no RBC casts, making RPGN unlikely.
More Glomerular diseases overview US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.