Pulmonary vascular disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pulmonary vascular disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pulmonary vascular disorders US Medical PG Question 1: A 43-year-old woman presents to her primary care provider with shortness of breath. She reports a 4-month history of progressively worsening difficulty breathing with associated occasional chest pain. She is a long-distance runner but has had trouble running recently due to her breathing difficulties. Her past medical history is notable for well-controlled hypertension for which she takes hydrochlorothiazide. She had a tibial osteosarcoma lesion with pulmonary metastases as a child and successfully underwent chemotherapy and surgical resection. She has a 10 pack-year smoking history but quit 15 years ago. She drinks a glass of wine 3 times per week. Her temperature is 98.6°F (37°C), blood pressure is 140/85 mmHg, pulse is 82/min, and respirations are 18/min. On exam, she has increased work of breathing with a normal S1 and loud P2. An echocardiogram in this patient would most likely reveal which of the following?
- A. Biventricular dilatation with a decreased ejection fraction
- B. Left ventricular dilatation with an incompetent aortic valve
- C. Left atrial dilatation with mitral valve stenosis
- D. Right ventricular hypertrophy with a dilated pulmonary artery (Correct Answer)
- E. Left ventricular hypertrophy with a bicuspid aortic valve
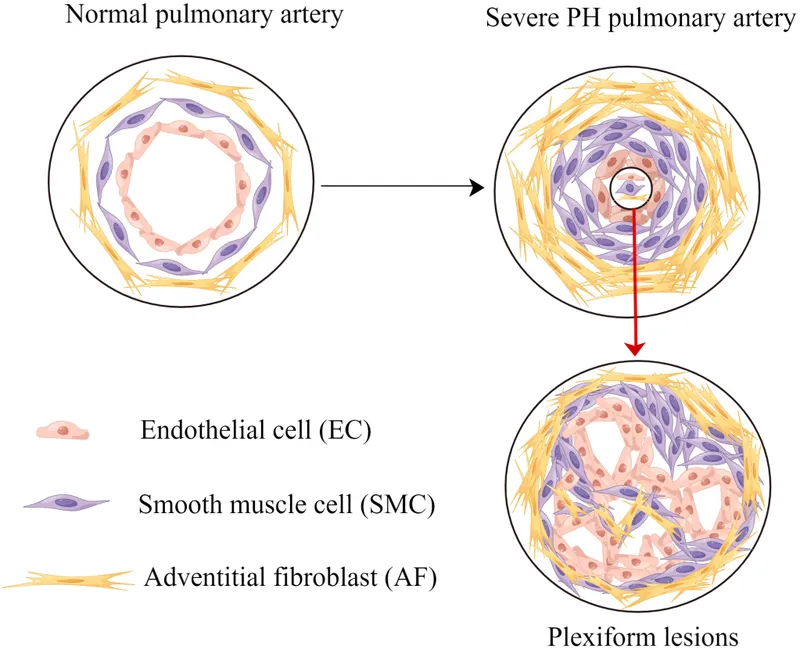
Pulmonary vascular disorders Explanation: The patient's history of **pulmonary metastases** (even successfully treated) and a **loud P2 heart sound** suggest **pulmonary hypertension**, which leads to increased afterload on the right ventricle. [1] **Pulmonary hypertension** causes the **right ventricle to hypertrophy** to overcome the elevated pulmonary arterial pressure, and the **pulmonary artery itself often dilates** due to the sustained high pressure. [1] [2] This describes **dilated cardiomyopathy**, which typically presents with **symptoms of heart failure** but doesn't specifically explain the **loud P2**, which points to pulmonary hypertension. [2]
Pulmonary vascular disorders US Medical PG Question 2: A 62-year-old woman with a history of subarachnoid hemorrhage is brought to the emergency department because of shortness of breath and sharp chest pain that worsens on inspiration. She underwent surgery for a hip fracture 3 weeks ago. Her pulse is 110/min, respirations are 20/min, and blood pressure is 112/74 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. The lungs are clear to auscultation and there is no jugular venous distention. A ventilation and perfusion scan shows a small perfusion defect in the left lower lung. A drug with which of the following mechanisms of action is most appropriate for this patient?
- A. Inhibition of adenosine diphosphate receptors
- B. Activation of plasminogen
- C. Inhibition of cyclooxygenase
- D. Inhibition of vitamin K epoxide reductase
- E. Activation of antithrombin III (Correct Answer)
Pulmonary vascular disorders Explanation: ***Activation of antithrombin III***
- The patient's symptoms (shortness of breath, sharp chest pain worsening on inspiration, tachycardia, tachypnea, hypoxia) and history (hip fracture surgery 3 weeks ago, subarachnoid hemorrhage) are highly suggestive of a **pulmonary embolism (PE)**, further supported by the perfusion defect on V/Q scan.
- **Heparin**, which activates antithrombin III, is the most appropriate initial therapy for PE because of its rapid onset of action and ability to prevent further clot formation, especially given the patient's history of subarachnoid hemorrhage, which contraindicates thrombolytics unless absolutely necessary for hemodynamic instability.
*Inhibition of adenosine diphosphate receptors*
- Drugs that inhibit ADP receptors, such as **clopidogrel**, are **antiplatelet agents** used to prevent arterial clots (e.g., in myocardial infarction or stroke).
- They are not the primary treatment for an acute venous thromboembolism like a pulmonary embolism, which requires anticoagulation to prevent further fibrin formation.
*Activation of plasminogen*
- **Thrombolytic agents** (e.g., tissue plasminogen activator) activate plasminogen to dissolve existing clots.
- While effective in severe PE, their use is associated with a high risk of bleeding, especially in a patient with a recent history of **subarachnoid hemorrhage**, making them contraindicated in this scenario unless the patient is hemodynamically unstable.
*Inhibition of cyclooxygenase*
- **Aspirin** inhibits cyclooxygenase (COX), reducing prostaglandin and thromboxane A2 synthesis, thereby inhibiting platelet aggregation.
- It is an **antiplatelet agent** primarily used for arterial thrombosis prophylaxis and is not the first-line treatment for acute pulmonary embolism.
*Inhibition of vitamin K epoxide reductase*
- Drugs like **warfarin** inhibit vitamin K epoxide reductase, which interferes with the synthesis of vitamin K-dependent clotting factors.
- Warfarin is used for long-term anticoagulation, but its **slow onset of action** makes it unsuitable for acute management of pulmonary embolism; heparin is typically initiated first.
Pulmonary vascular disorders US Medical PG Question 3: A 62-year-old woman with no significant past medical history presents with progressive dyspnea on exertion over the past 6 months. Echocardiogram reveals elevated pulmonary artery pressure (PAP) of 55 mmHg with normal left ventricular ejection fraction and no evidence of left-sided valvular disease. Right heart catheterization confirms mean PAP of 50 mmHg with pulmonary capillary wedge pressure of 10 mmHg. Intraoperative administration of intravenous adenosine causes the PAP to decrease to 35 mmHg. What pharmacological therapy is most likely to provide long-term benefit for this patient?
- A. Amlodipine (Correct Answer)
- B. Bosentan
- C. Epoprostenol
- D. Sildenafil
- E. Adenosine
Pulmonary vascular disorders Explanation: ***Amlodipine***
- The patient has **idiopathic pulmonary arterial hypertension (PAH, Group 1 PH)** confirmed by elevated mean PAP >20 mmHg with normal pulmonary capillary wedge pressure (≤15 mmHg), excluding left heart disease.
- The **positive acute vasodilator response** (PAP drop >10 mmHg to <40 mmHg) during right heart catheterization indicates **vasoreactivity**, which predicts favorable response to **calcium channel blockers (CCBs)**.
- **Amlodipine** or other CCBs (nifedipine, diltiazem) are the **first-line long-term therapy** for vasoreactive idiopathic PAH, with some patients achieving near-normalization of PAP.
- Only about **10% of idiopathic PAH patients** are vasoreactive, making this finding clinically significant.
*Bosentan*
- **Bosentan** is an **endothelin receptor antagonist** used for **PAH (Group 1)**.
- While effective for PAH, it is typically reserved for patients who are **non-vasoreactive** or who fail CCB therapy.
- Given this patient's positive vasodilator response, a **CCB trial is preferred first** due to better long-term outcomes in vasoreactive patients.
*Epoprostenol*
- **Epoprostenol** is a **prostacyclin analog** used for severe **PAH**, particularly WHO functional class III-IV.
- It requires **continuous intravenous infusion** and is reserved for more advanced or refractory PAH.
- Not appropriate as **first-line therapy** in a vasoreactive patient who can be treated with oral CCBs.
*Sildenafil*
- **Sildenafil** is a **phosphodiesterase-5 inhibitor** effective for **PAH**.
- Like bosentan, it is used for patients who are **non-vasoreactive** or have failed CCB therapy.
- In a vasoreactive patient, **CCBs are preferred** due to superior long-term outcomes in this subset.
*Adenosine*
- **Adenosine** is an **ultrashort-acting vasodilator** used as a **diagnostic agent** during right heart catheterization to assess vasoreactivity.
- It has a half-life of seconds and is **not suitable for long-term therapy**.
- Alternative agents for vasoreactivity testing include inhaled nitric oxide and intravenous epoprostenol.
Pulmonary vascular disorders US Medical PG Question 4: A 52-year-old man presents to the emergency department with sudden-onset dyspnea, tachypnea, and chest pain. He works as a long-haul truck driver, and he informs you that he recently returned to the west coast from a trip to Tennessee. His medical history is significant for gout, hypertension, hypercholesterolemia, diabetes mellitus type 2, and mild intellectual disability. He currently smokes 2 packs of cigarettes/day, drinks a 6-pack of beer/day, and he endorses a past history of injection drug use but currently denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 23/min. His physical examination shows minimal bibasilar rales, but otherwise clear lungs on auscultation, grade 2/6 holosystolic murmur, and a benign abdominal physical examination. A computed tomography angiography (CTA) demonstrates a segmental pulmonary embolism (PE). Which of the following is the most appropriate treatment plan for this patient?
- A. Consult interventional radiologist (IR) for IVC filter placement
- B. Initiate heparin
- C. Tissue plasminogen activator (tPA)
- D. Initiate heparin with a bridge to warfarin (Correct Answer)
- E. Initiate warfarin anticoagulation
Pulmonary vascular disorders Explanation: ***Initiate heparin with a bridge to warfarin***
- This patient presents with a **segmental pulmonary embolism (PE)** and is hemodynamically stable (BP 126/74 mmHg, HR 87/min), making initial anticoagulation with **heparin** followed by a bridge to **warfarin** the most appropriate treatment.
- Heparin provides rapid anticoagulation, while warfarin is initiated concurrently and takes several days to reach therapeutic levels, requiring overlap until the **International Normalized Ratio (INR)** is within the therapeutic range (2.0-3.0).
*Consult interventional radiologist (IR) for IVC filter placement*
- **Inferior vena cava (IVC) filters** are typically reserved for patients with a **contraindication to anticoagulation** or those who experience **recurrent PE despite adequate anticoagulation**.
- This patient has no stated contraindications to anticoagulation and has not failed initial therapy, so an IVC filter is not indicated at this time.
*Initiate heparin*
- While initiating **heparin** is the correct first step, it is incomplete as a long-term treatment strategy for PE.
- Patients with PE require **long-term anticoagulation** (typically 3-6 months or longer), for which warfarin or novel oral anticoagulants (NOACs) are used, following an initial period of rapid-acting anticoagulation.
*Tissue plasminogen activator (tPA)*
- **Thrombolytic therapy with tPA** is indicated for patients with **massive PE** who are **hemodynamically unstable** (e.g., hypotension, shock).
- This patient is hemodynamically stable, and his PE is segmental, so thrombolysis carries a higher risk of bleeding complications than benefits in this case.
*Initiate warfarin anticoagulation*
- **Warfarin** has a slow onset of action (3-5 days to achieve therapeutic INR) and therefore should not be used as monotherapy for initial management of acute PE.
- Initial management requires a **rapid-acting anticoagulant** like heparin or low molecular weight heparin (LMWH) to prevent further clot propagation and embolization.
Pulmonary vascular disorders US Medical PG Question 5: Four days after undergoing an elective total hip replacement, a 65-year-old woman develops a DVT that embolizes to the lung. Along with tachypnea, tachycardia, and cough, the patient would most likely present with a PaO2 of what?
- A. 120 mmHg
- B. 100 mmHg
- C. 85 mmHg (Correct Answer)
- D. 110 mmHg
- E. 60 mmHg
Pulmonary vascular disorders Explanation: ***85 mmHg***
- A pulmonary embolism (PE) causes a **ventilation-perfusion (V/Q) mismatch**, leading to **hypoxemia** and a reduced PaO2.
- While exact values vary, a PaO2 of 85 mmHg indicates **mild to moderate hypoxemia**, which is common in PE, especially with accompanying symptoms like tachypnea and tachycardia.
*120 mmHg*
- This value is significantly **higher than normal (75-100 mmHg)** and would indicate **hyperoxia**, which is inconsistent with acute pulmonary embolism causing respiratory distress.
- A patient with PE would typically have **reduced oxygenation**, not supernormal levels, unless receiving high-flow supplemental oxygen.
*100 mmHg*
- A PaO2 of 100 mmHg is at the **upper end of the normal range** (75-100 mmHg) and would imply **no significant hypoxemia**.
- Given the patient's symptoms of tachypnea, tachycardia, and cough following a DVT with embolization, a normal or high-normal PaO2 is unlikely without aggressive oxygen therapy (which is not stated).
*110 mmHg*
- This value is **above the normal range** and suggests **hyperoxia**, which is contrary to the pathophysiology of a pulmonary embolism.
- A PE impairs gas exchange, leading to a decrease in PaO2, not an increase.
*60 mmHg*
- A PaO2 of 60 mmHg indicates **significant hypoxemia**, which might occur in a severe, large pulmonary embolism or in a patient with underlying lung disease.
- While possible, 85 mmHg represents a more common, moderate hypoxemia seen in PE, especially given the prompt presentation of symptoms.
Pulmonary vascular disorders US Medical PG Question 6: A 60-year-old man presents to the emergency department with pleuritic chest pain. He recently returned from a vacation in Germany and noticed he felt short of breath and had chest pain the following morning. The patient is generally healthy but did have surgery on his ankle 3 weeks ago and has been less ambulatory. His temperature is 99.0°F (37.2°C), blood pressure is 137/88 mm Hg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 96% on room air. Physical exam is notable for a warm and swollen lower extremity. The physician has high clinical suspicion for pulmonary embolism given the patient's risk factors and presentation. Which of the following findings would warrant further workup with a CT angiogram?
- A. Bilateral wheezing
- B. Green sputum
- C. Decreased breath sounds over area of the lung
- D. Increased breath sounds over area of the lung
- E. Hemoptysis (Correct Answer)
Pulmonary vascular disorders Explanation: ***Hemoptysis***
- **Hemoptysis** (coughing up blood) in the presence of pleuritic chest pain, dyspnea, and risk factors for DVT (recent surgery, immobility, long travel) is a classic symptom of **pulmonary embolism (PE)**, often indicating pulmonary infarction due to arterial occlusion.
- This symptom significantly increases the clinical probability of PE, warranting immediate and definitive diagnostic imaging like a **CT pulmonary angiogram (CTPA)**.
*Bilateral wheezing*
- **Bilateral wheezing** is typically associated with diffuse airway narrowing, as seen in conditions like **asthma** or **COPD**, and is not a specific indicator of pulmonary embolism.
- While it can occur in PE due to bronchoconstriction, it is not a primary or highly specific sign that directly warrants a CT angiogram for PE when other more classic symptoms are present.
*Green sputum*
- **Green sputum** is a strong indicator of a **bacterial infection**, such as pneumonia or acute bronchitis, due to the presence of pus and bacterial products.
- This symptom would lead to workup for infection rather than directly for pulmonary embolism, although pneumonia can sometimes present with similar symptoms.
*Decreased breath sounds over area of the lung*
- While localized **decreased breath sounds** can be seen with PE (e.g., due to atelectasis or pleural effusion), it is a **non-specific finding** that can also be caused by conditions like pneumonia, pleural effusion, or pneumothorax.
- It does not, on its own, provide as strong an indication for PE as hemoptysis, given the other clinical context.
*Increased breath sounds over area of the lung*
- **Increased breath sounds** (e.g., bronchial breath sounds) typically indicate lung consolidation, characteristic of **pneumonia**, where solid tissue transmits sound more efficiently.
- This finding is not associated with pulmonary embolism and would steer the diagnostic workup towards infectious processes rather than PE.
Pulmonary vascular disorders US Medical PG Question 7: A 33-year-old woman comes to the physician because of a 6-month history of worsening shortness of breath and fatigue. Her paternal uncle had similar symptoms and died of respiratory failure at 45 years of age. The lungs are clear to auscultation. Pulmonary function testing shows an FVC of 84%, an FEV1/FVC ratio of 92%, and a normal diffusion capacity. An ECG shows a QRS axis greater than +90 degrees. Genetic analysis shows an inactivating mutation in the bone morphogenetic protein receptor type II (BMPR2) gene. Which of the following is the most likely cause of this patient's symptoms?
- A. Thickening of the interventricular septum
- B. Fibrosis of the pulmonary parenchyma
- C. Chronic intravascular hemolysis
- D. Elevated left atrial pressure
- E. Elevated pulmonary arterial pressure (Correct Answer)
Pulmonary vascular disorders Explanation: ***Elevated pulmonary arterial pressure***
- The patient's symptoms (dyspnea, fatigue), family history of early respiratory failure, and the presence of an inactivating mutation in **BMPR2** are highly suggestive of **heritable pulmonary arterial hypertension (PAH)**.
- **PAH** is characterized by elevated pressures in the pulmonary arteries, leading to right ventricular strain, which is reflected by the **ECG finding of a QRS axis greater than +90 degrees** (right axis deviation).
- The **normal diffusion capacity** helps distinguish PAH from parenchymal lung diseases, and the **FEV1/FVC ratio of 92%** (elevated) with relatively preserved FVC is consistent with the restrictive physiology sometimes seen in PAH.
*Thickening of the interventricular septum*
- While septal thickening can occur in some cardiac conditions, it is not the primary cause of symptoms in the context of heritable PAH, nor is it directly indicated by the given pulmonary function tests or ECG.
- **Hypertrophic cardiomyopathy** can cause septal thickening, but it typically presents with different cardiac pathologies and is not associated with BMPR2 mutations.
*Fibrosis of the pulmonary parenchyma*
- This would cause a **restrictive lung disease** with a **reduced FVC** and **reduced diffusion capacity** due to impaired gas exchange across thickened alveolar-capillary membranes.
- The patient's **normal diffusion capacity** specifically rules out significant pulmonary fibrosis or other interstitial lung diseases.
*Chronic intravascular hemolysis*
- This condition would typically present with **anemia**, **jaundice**, **elevated LDH**, and possibly **splenomegaly**, none of which are mentioned.
- It is not associated with the BMPR2 genetic mutation or the specific PFT and ECG findings in this case.
*Elevated left atrial pressure*
- Elevated left atrial pressure (e.g., due to **left-sided heart failure** or mitral stenosis) can cause pulmonary congestion and dyspnea, but would typically lead to **pulmonary edema** with crackles on auscultation and **reduced diffusion capacity** due to fluid in the alveoli.
- The patient's clear lung auscultation and normal diffusion capacity make elevated left atrial pressure unlikely.
Pulmonary vascular disorders US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pulmonary vascular disorders Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pulmonary vascular disorders US Medical PG Question 9: A 24-year-old male was in a motor vehicle accident that caused him to fracture his femur and pelvis. After 2 days in the hospital, the patient became delirious, tachypneic, and a petechial rash was found in his upper extremities. Which of the following is most likely responsible for this patient’s symptoms?
- A. Thrombotic clot in the pulmonary artery
- B. Aspiration of oropharyngeal contents
- C. Alveolar foamy exudates with disc shaped cysts seen with methenamine silver stain
- D. Fat microglobules in the microvasculature (Correct Answer)
- E. Type I and type II pneumocyte damage due to neutrophils
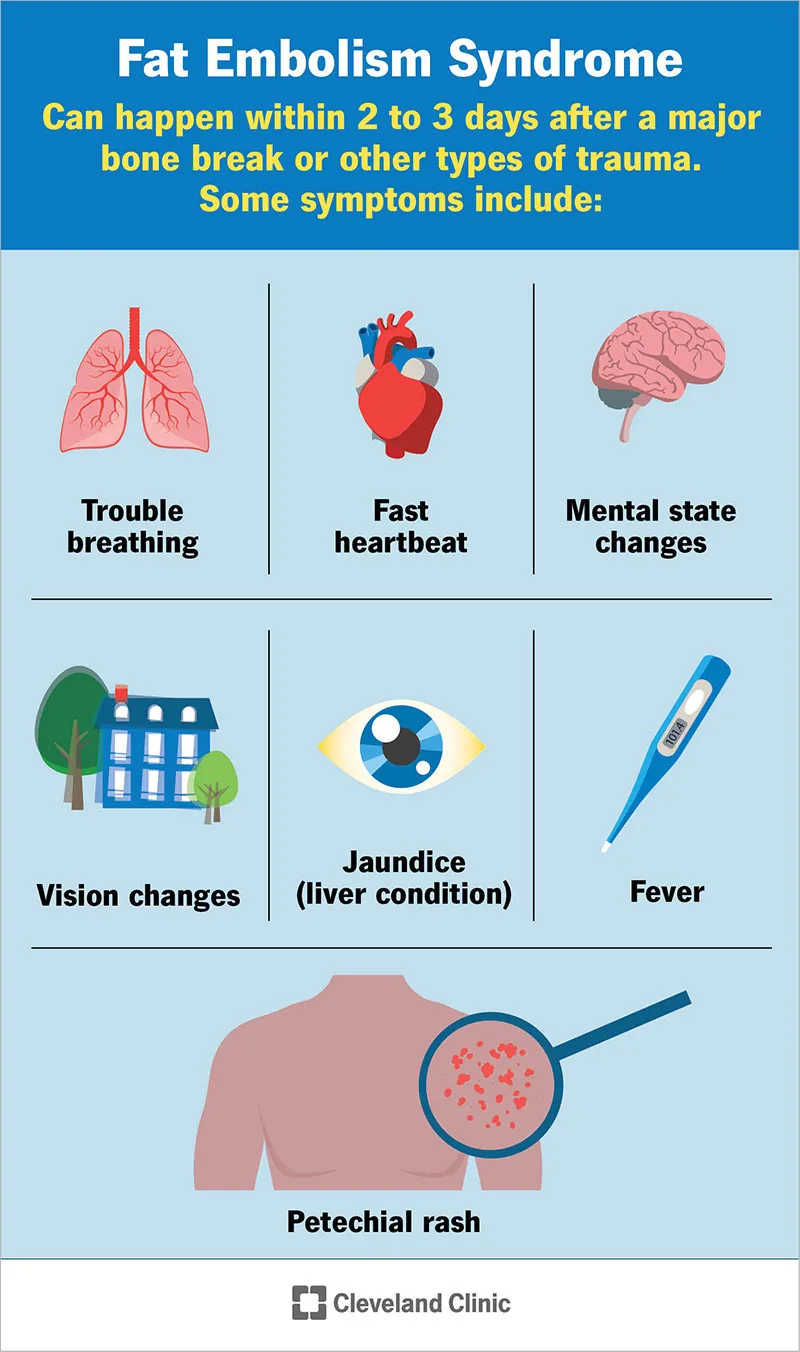
Pulmonary vascular disorders Explanation: ***Fat microglobules in the microvasculature***
- This scenario describes **fat embolism syndrome (FES)**, often triggered by trauma to long bones (like the femur) or the pelvis.
- The classic triad of FES includes **respiratory distress (tachypnea)**, **neurological symptoms (delirium)**, and a **petechial rash**, which perfectly matches the patient's presentation.
*Thrombotic clot in the pulmonary artery*
- A **pulmonary embolism (PE)** can cause tachypnea and delirium, but it typically does not present with a **petechial rash**.
- PE is usually due to a **venous thromboembolism** from deep leg veins, though trauma can increase risk, the rash points away from a simple thrombotic PE.
*Aspiration of oropharyngeal contents*
- **Aspiration pneumonia** can cause respiratory distress, but it doesn't typically lead to **delirium or a petechial rash** in this timeframe.
- The symptoms would likely include fever, cough, and infiltrates on chest X-ray.
*Alveolar foamy exudates with disc-shaped cysts seen with methenamine silver stain*
- This description is characteristic of **Pneumocystis pneumonia** (*Pneumocystis jirovecii*), an opportunistic infection typically seen in immunocompromised individuals.
- It would not manifest acutely after trauma with a petechial rash.
*Type I and type II pneumocyte damage due to neutrophils*
- This describes **acute respiratory distress syndrome (ARDS)**, which can be a complication of severe trauma.
- While ARDS could cause respiratory distress and potentially delirium, it generally doesn't present with a **petechial rash** as a hallmark symptom in this context.
Pulmonary vascular disorders US Medical PG Question 10: A newborn girl is rushed to the neonatal ICU after an emergency cesarean section due to unstable vital signs after delivery. The pregnancy was complicated due to oligohydramnios and pulmonary hypoplasia. Gestation was at 38 weeks. APGAR scores were 6 and 8 at 1 and 5 minutes respectively. The newborn’s temperature is 37.0°C (98.6°F), the blood pressure is 60/40 mm Hg, the respiratory rate is 45/min, and the pulse is 140/min. Physical examination reveals irregularly contoured bilateral abdominal masses. Abdominal ultrasound reveals markedly enlarged echogenic kidneys (5 cm in the vertical dimension) with multiple cysts in the cortex and medulla. This patient is at highest risk of which of the following complications?
- A. Portal hypertension (Correct Answer)
- B. Subarachnoid hemorrhage
- C. Acute renal failure
- D. Recurrent UTI
- E. Emphysema
Pulmonary vascular disorders Explanation: ***Portal hypertension***
* The presentation of **oligohydramnios**, **pulmonary hypoplasia**, and **enlarged, echogenic kidneys with multiple cysts** in a newborn is consistent with **autosomal recessive polycystic kidney disease (ARPKD)**.
* ARPKD is invariably associated with **congenital hepatic fibrosis**, which leads to **portal hypertension** due to periportal fibrosis and obstruction of intrahepatic portal blood flow. This is the hallmark extra-renal complication of ARPKD.
*Subarachnoid hemorrhage*
* Subarachnoid hemorrhage from berry aneurysm rupture is associated with **autosomal dominant polycystic kidney disease (ADPKD)**, not ARPKD.
* There are no specific clinical features or imaging findings in this case that would suggest intracranial hemorrhage as the highest risk complication.
*Acute renal failure*
* While neonates with ARPKD can develop renal insufficiency and progressive chronic kidney disease, the question asks for the "highest risk **complication**" rather than the primary disease manifestation.
* **Portal hypertension from congenital hepatic fibrosis** is the most significant distinct complication that develops as a consequence of ARPKD, often manifesting in childhood with hepatosplenomegaly, esophageal varices, and hypersplenism.
*Recurrent UTI*
* Recurrent UTIs require structural abnormalities like vesicoureteral reflux or urinary stasis, which are not primary features of ARPKD.
* While children with kidney disease may have increased infection risk, recurrent UTIs are not a direct or characteristic complication of the cystic kidney disease in ARPKD.
*Emphysema*
* **Pulmonary hypoplasia** (underdeveloped lungs from oligohydramnios/Potter sequence) is present in this case, but this is not the same as emphysema.
* Emphysema involves destruction of alveolar walls and is typically seen in adults with chronic obstructive pulmonary disease or alpha-1 antitrypsin deficiency, not in neonates with pulmonary hypoplasia.
More Pulmonary vascular disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.