Pulmonary edema US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pulmonary edema. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pulmonary edema US Medical PG Question 1: A 48-year-old female suffers a traumatic brain injury while skiing in a remote area. Upon her arrival to the ER, she is severely hypoxemic and not responsive to O2 therapy. She is started on a mechanical ventilator and 2 days later upon auscultation, you note late inspiratory crackles. Which of the following is most likely normal in this patient?
- A. Alveolar-arterial gradient
- B. Left atrial pressure (Correct Answer)
- C. Type II pneumocytes
- D. Type I pneumocytes
- E. Chest X-ray
Pulmonary edema Explanation: ***Left atrial pressure***
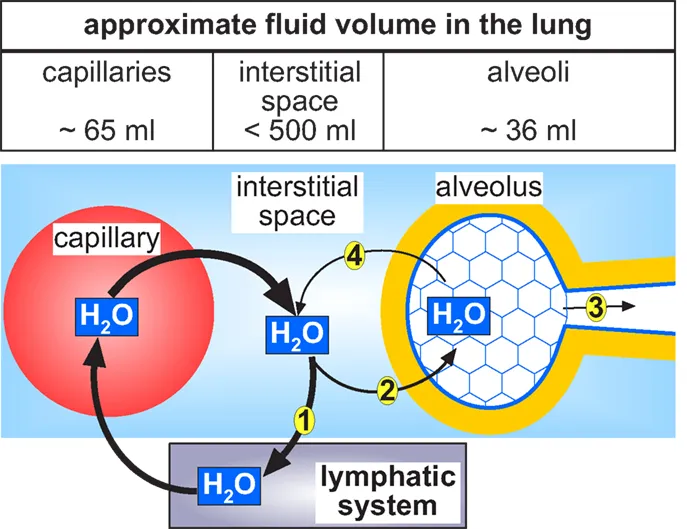
- A normal left atrial pressure would be expected in a patient with **Non-Cardiogenic Pulmonary Edema**, which is implied by her severe hypoxemia refractory to oxygen, crackles, and history of **Traumatic Brain Injury**.
- **Neurogenic Pulmonary Edema**, a form of non-cardiogenic pulmonary edema, is a known complication of severe TBI and does not primarily involve left heart failure, thus maintaining a normal left atrial pressure.
*Alveolar-arterial gradient*
- The patient's severe **hypoxemia** unresponsive to oxygen therapy indicates a significant **ventilation-perfusion mismatch** or shunt, which would lead to an *increased* alveolar-arterial gradient.
- An increased A-a gradient is characteristic of pulmonary edema, where fluid in the alveoli impairs oxygen diffusion into the capillaries.
*Type II pneumocytes*
- In **acute respiratory distress syndrome (ARDS)**, which is strongly suggested by the patient's presentation (non-cardiogenic pulmonary edema), **Type II pneumocytes often proliferate** in the reparative phase.
- While they are normally involved in **surfactant production**, their function can be impaired, and their numbers might increase to replace damaged Type I cells, so they would not be "normal."
*Type I pneumocytes*
- **Type I pneumocytes** are the primary cells responsible for **gas exchange** and are highly susceptible to injury in conditions like ARDS or pulmonary edema.
- In such a critically ill patient with diffuse alveolar damage, these cells would likely be damaged or destroyed, thus *not* normal.
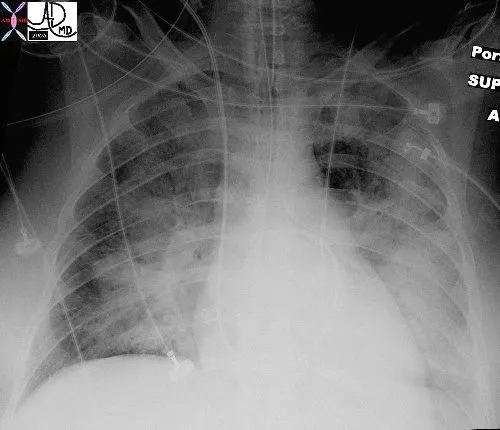
*Chest X-ray*
- Given the patient's severe hypoxemia, late inspiratory crackles, and probable pulmonary edema, her **Chest X-ray** would likely show **bilateral infiltrates** or **diffuse haziness**, characteristic of ARDS or neurogenic pulmonary edema.
- Therefore, a normal chest X-ray is highly unlikely in this clinical scenario.
Pulmonary edema US Medical PG Question 2: A 41-year-old man comes to the emergency department because of fatigue, worsening abdominal discomfort, and progressive swelling of his legs for 3 months. The swelling is worse in the evenings. His only medication is ibuprofen for occasional joint pain. The patient does not smoke and drinks 2–3 beers each weekend. His temperature is 36°C (96.8°F), pulse is 88/min, respirations are 18/min, and blood pressure is 130/80 mm Hg. Pulmonary examination shows no abnormalities. Abdominal examination shows a mildly distended abdomen with shifting dullness. The liver is palpated 2–3 cm below the right costal margin. When pressure is applied to the right upper quadrant, the patient's jugular veins become visibly distended for 15 seconds. The 2nd and 3rd metacarpophalangeal joints of both hands are tender to palpation. There is 2+ edema in the lower extremities. Which of the following is the most likely underlying cause of this patient's edema?
- A. Reduced glomerular filtration rate
- B. Macrovesicular steatosis of the liver
- C. Dermal deposition of glycosaminoglycans
- D. Impaired hepatic protein synthesis
- E. Impaired relaxation of the right ventricle (Correct Answer)
Pulmonary edema Explanation: ***Impaired relaxation of the right ventricle***
- The presence of **fatigue**, **abdominal discomfort**, **leg swelling**, **ascites with shifting dullness**, **hepatomegaly**, and particularly a positive **hepatojugular reflux** (jugular vein distension with RUQ pressure) strongly suggests **right-sided heart failure** due to impaired right ventricular relaxation, such as in **constrictive pericarditis** or **restrictive cardiomyopathy**.
- **Ibuprofen (NSAID) use** and **joint tenderness** in the metacarpophalangeal joints hint at a potential underlying inflammatory condition like rheumatoid arthritis, which can be associated with **amyloidosis** causing restrictive cardiomyopathy.
*Reduced glomerular filtration rate*
- While a reduced GFR can cause edema, it typically leads to **generalized anasarca** and is often associated with symptoms of **uremia** or significant proteinuria, which are not described.
- The prominent **hepatomegaly** and **positive hepatojugular reflux** are not primary features of renal-induced edema.
*Macrovesicular steatosis of the liver*
- **Macrovesicular steatosis** (fatty liver) itself does not directly cause significant edema or ascites unless it progresses to **cirrhosis**, which would manifest with more distinct signs of **liver failure** and portal hypertension.
- While the patient has some alcohol intake, the clinical picture with prominent hepatojugular reflux points more towards cardiac than isolated liver pathology at this stage.
*Dermal deposition of glycosaminoglycans*
- Dermal deposition of **glycosaminoglycans** is characteristic of **myxedema** (hypothyroidism), which causes non-pitting edema and is usually associated with other symptoms like **cold intolerance**, **bradycardia**, and **dry skin**, none of which are mentioned.
- The pitting edema observed in this patient is inconsistent with myxedema.
*Impaired hepatic protein synthesis*
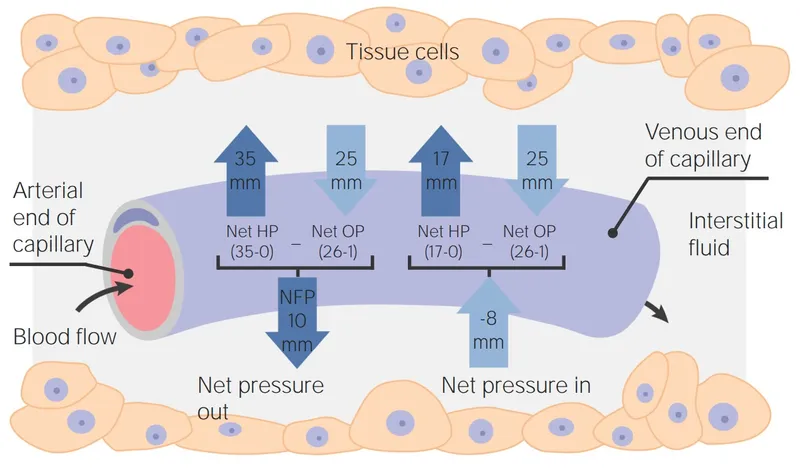
- Impaired hepatic protein synthesis, leading to **hypoalbuminemia**, can cause edema and ascites due to reduced **oncotic pressure**.
- However, the significant **hepatomegaly** and the distinct **hepatojugular reflux** are more indicative of a circulatory issue affecting the liver, rather than primary intrinsic liver failure.
Pulmonary edema US Medical PG Question 3: The serum brain natriuretic peptide and N-terminal pro-BNP are elevated. A diagnosis of heart failure with preserved ejection fraction is made. In addition to supplemental oxygen therapy, which of the following is the most appropriate initial step in management?
- A. Intravenous dobutamine
- B. Intravenous furosemide therapy (Correct Answer)
- C. Intravenous morphine therapy
- D. Thoracentesis
- E. Intermittent hemodialysis
Pulmonary edema Explanation: ***Intravenous furosemide therapy***
- Heart failure with **preserved ejection fraction (HFpEF)** often presents with **pulmonary congestion** due to elevated filling pressures.
- **Furosemide**, a loop diuretic, effectively reduces fluid overload and associated symptoms by increasing renal excretion of sodium and water.
*Intravenous dobutamine*
- **Dobutamine** is an inotropic agent that increases myocardial contractility and heart rate.
- It is typically used for **acute decompensated heart failure with low cardiac output** and is generally avoided in HFpEF unless there is significant hypoperfusion, as it can worsen myocardial oxygen demand and diastolic dysfunction.
*Intravenous morphine therapy*
- **Morphine** can be used in acute heart failure to reduce preload and anxiety, but it is not a primary treatment for the underlying fluid overload.
- It can cause respiratory depression and hypotension, and its use is typically reserved for patients with severe pain or dyspnea not adequately managed by other therapies.
*Thoracentesis*
- **Thoracentesis** is indicated for symptomatic **pleural effusions** causing respiratory distress.
- While pleural effusions can occur in heart failure, initial management of generalized fluid overload typically involves diuretics, making thoracentesis a secondary intervention if diuretic therapy is insufficient.
*Intermittent hemodialysis*
- **Intermittent hemodialysis** is an invasive procedure primarily used for severe renal failure or refractory fluid overload that has not responded to maximal diuretic therapy.
- It is not the initial step in managing heart failure with preserved ejection fraction and would only be considered in highly selected cases with **acute kidney injury** or diuretic resistance.
Pulmonary edema US Medical PG Question 4: A 54-year-old man is brought to the emergency department 1 hour after the sudden onset of shortness of breath, epigastric pain, and sweating. He has no history of similar symptoms. He has hypertension and type 2 diabetes mellitus. Current medications include amlodipine and metformin. He has smoked one pack of cigarettes daily for 20 years. He appears weak and pale. His pulse is 56/min, respirations are 18/min, and blood pressure is 100/70 mm Hg. Cardiac examination shows normal heart sounds. The lungs are clear to auscultation. The skin is cold to the touch. An ECG is shown. Bedside transthoracic echocardiography shows normal left ventricular function. High-dose aspirin is administered. Administration of which of the following is most appropriate next step in management?
- A. Intravenous atropine
- B. Intravenous morphine
- C. Normal saline bolus (Correct Answer)
- D. Phenylephrine infusion
- E. Sublingual nitroglycerin
Pulmonary edema Explanation: ***Normal saline bolus***
- This patient presents with symptoms concerning for an inferior wall myocardial infarction (MI) which commonly affects the **right ventricle (RV)**. The ECG shows **ST elevation in leads II, III, and aVF**, confirming an inferior STEMI. Given his **hypotension (100/70 mm Hg)** and **bradycardia (56/min)**, he is likely experiencing RV involvement and is preload-dependent.
- A **normal saline bolus** is crucial to increase preload and improve cardiac output, especially in RV infarcts where reduced preload significantly impairs RV function and, consequently, left ventricular filling.
*Intravenous atropine*
- While the patient has bradycardia, it is secondary to the inferior MI affecting the **right coronary artery**, which often supplies the **AV node**.
- Atropine is used for symptomatic bradycardia but a fluid bolus should be prioritized in RV MI with hypotension to restore preload before considering pharmacologic interventions for heart rate.
*Intravenous morphine*
- Morphine is used for pain relief in acute MI but can cause **vasodilation**, which would worsen this patient's **hypotension**.
- In cases of RV infarction, where preload dependence is critical, morphine should be used with extreme caution or avoided due to its potential to further reduce blood pressure.
*Phenylephrine infusion*
- Phenylephrine is a **pure alpha-agonist** that causes **vasoconstriction** and increases systemic vascular resistance, thereby increasing afterload.
- Increasing afterload in the setting of an acute MI, especially one with potential RV involvement and preload dependence, can severely compromise cardiac function and worsen the patient's condition.
*Sublingual nitroglycerin*
- Nitroglycerin causes **vasodilation**, reducing both preload and afterload.
- In a patient with an **inferior wall MI** and **hypotension**, nitroglycerin is contraindicated as it can profoundly reduce preload, leading to a significant drop in blood pressure and worsening shock, especially if the right ventricle is involved.
Pulmonary edema US Medical PG Question 5: An investigator is studying early post-mortem changes in the lung. Autopsies are performed on patients who died following recent hospital admissions. Microscopic examination of the lungs at one of the autopsies shows numerous macrophages with brown intracytoplasmic inclusions. A Prussian blue stain causes these inclusions to turn blue. These findings are most consistent with a pathological process that would manifest with which of the following symptoms?
- A. Purulent expectoration that worsens in the lateral recumbent position
- B. Diaphoresis that worsens at night
- C. Lower extremity swelling that worsens on standing
- D. Dry cough that worsens early in the morning
- E. Shortness of breath that worsens when supine (Correct Answer)
Pulmonary edema Explanation: ***Shortness of breath that worsens when supine***
- The presence of **hemosiderin-laden macrophages** (also known as **heart failure cells**) in the lung, indicated by brown intracytoplasmic inclusions staining positive with Prussian blue, signifies **pulmonary edema** due to chronic passive congestion.
- This condition is typically caused by **left-sided heart failure**, which often manifests as **orthopnea** (shortness of breath worse when supine) and **paroxysmal nocturnal dyspnea**.
*Purulent expectoration that worsens in the lateral recumbent position*
- **Purulent expectoration**, particularly with positional worsening, is characteristic of a **lung abscess** or **bronchiectasis**, which are infectious conditions.
- These conditions would feature neutrophils and necrotic debris, not hemosiderin-laden macrophages, as the primary microscopic finding.
*Diaphoresis that worsens at night*
- **Night sweats** and **diaphoresis** are classic symptoms of **tuberculosis** or certain malignancies like lymphoma.
- These conditions are not typically associated with hemosiderin-laden macrophages as a primary pulmonary finding.
*Lower extremity swelling that worsens on standing*
- **Dependent edema** in the lower extremities that worsens with standing is a hallmark symptom of **right-sided heart failure** or **venous insufficiency**.
- While related to heart failure, the pulmonary findings described (hemosiderin-laden macrophages) are more directly linked to chronic **left-sided heart failure** and pulmonary congestion.
*Dry cough that worsens early in the morning*
- A **dry cough** that is worse in the morning can be a symptom of **asthma**, **bronchitis**, or **GERD**.
- These conditions do not typically present with hemosiderin-laden macrophages from chronic pulmonary congestion.
Pulmonary edema US Medical PG Question 6: A 37-year-old male presents to your clinic with shortness of breath and lower extremity edema. He was born in Southeast Asia and emigrated to America ten years prior. Examination demonstrates 2+ pitting edema to the level of his knees, ascites, and bibasilar crackles, as well as an opening snap followed by a mid-to-late diastolic murmur. The patient undergoes a right heart catheterization that demonstrates a pulmonary capillary wedge pressure (PCWP) of 24 mmHg. The patient is most likely to have which of the following?
- A. Normal or decreased left ventricular end diastolic pressure (LVEDP) (Correct Answer)
- B. Decreased transmitral gradient
- C. Decreased pulmonary artery systolic pressure (PASP)
- D. Increased left ventricular end diastolic pressure (LVEDP)
- E. Increased pulmonary vascular compliance
Pulmonary edema Explanation: ***Normal or decreased left ventricular end diastolic pressure (LVEDP)***
- The patient's symptoms (opening snap, mid-to-late diastolic murmur, Southeast Asian origin) strongly suggest **mitral stenosis**.
- In mitral stenosis, the obstruction at the **mitral valve** leads to elevated left atrial pressure (reflected by the high PCWP), but the left ventricle itself is not failing, so LVEDP is typically normal or even decreased.
*Decreased transmitral gradient*
- A **mid-to-late diastolic murmur** and an **opening snap** are classic signs of mitral stenosis, indicating a high pressure gradient across the mitral valve during diastole.
- A decreased transmitral gradient would imply reduced obstruction, which contradicts the patient's strong clinical presentation.
*Decreased pulmonary artery systolic pressure (PASP)*
- Elevated pulmonary capillary wedge pressure (PCWP) of 24 mmHg indicates **pulmonary hypertension secondary to left atrial pressure elevation** in mitral stenosis.
- This consistently leads to an **increased pulmonary artery systolic pressure (PASP)**, not a decreased one, as the right ventricle has to work harder to pump blood through the high-pressure pulmonary vasculature.
*Increased left ventricular end diastolic pressure (LVEDP)*
- While PCWP is elevated due to **left atrial pressure overload** in mitral stenosis, the left ventricle itself is not volume or pressure overloaded during diastole.
- The LVEDP would only be increased if there was actual left ventricular dysfunction or aortic valve disease, which is not suggested here.
*Increased pulmonary vascular compliance*
- Chronic pulmonary hypertension, as seen in advanced mitral stenosis with high PCWP, leads to **pulmonary vascular remodeling** and **decreased pulmonary vascular compliance**.
- The pulmonary vessels become stiffer and less distensible, not more compliant.
Pulmonary edema US Medical PG Question 7: A 55-year-old man presents to the emergency department with shortness of breath and weakness. Past medical history includes coronary artery disease, arterial hypertension, and chronic heart failure. He reports that the symptoms started around 2 weeks ago and have been gradually worsening. His temperature is 36.5°C (97.7°F), blood pressure is 135/90 mm Hg, heart rate is 95/min, respiratory rate is 24/min, and oxygen saturation is 94% on room air. On examination, mild jugular venous distention is noted. Auscultation reveals bilateral loud crackles. Pitting edema of the lower extremities is noted symmetrically. His plasma brain natriuretic peptide level on rapid bedside assay is 500 pg/mL (reference range < 125 pg/mL). A chest X-ray shows enlarged cardiac silhouette. He is diagnosed with acute on chronic left heart failure with pulmonary edema and receives immediate care with furosemide. The physician proposes a drug trial with a new BNP stabilizing agent. Which of the following changes below are expected to happen if the patient is enrolled in this trial?
- A. Increased potassium release from cardiomyocytes
- B. Increased water reabsorption by the renal collecting ducts
- C. Increased blood pressure
- D. Inhibition of funny sodium channels
- E. Restricted aldosterone release (Correct Answer)
Pulmonary edema Explanation: ***Restricted aldosterone release***
- **BNP** acts to counter the **RAAS** system. By stabilizing BNP, there will be increased **natriuresis** and reduced levels of aldosterone due to its inhibitory effect on **renin secretion**.
- This **aldosterone** restriction contributes to **diuresis** and vasodilation, which ultimately helps to reduce cardiac preload and afterload.
*Increased potassium release from cardiomyocytes*
- An increase in **potassium release** from cardiomyocytes is not a direct or expected effect of a **BNP stabilizing agent**.
- BNP primarily influences **sodium** and **water balance** through renal and vascular effects, not direct cardiomyocyte potassium regulation.
*Increased water reabsorption by the renal collecting ducts*
- **BNP** promotes **natriuresis** and **diuresis**, leading to decreased water reabsorption in the renal collecting ducts.
- A BNP stabilizing agent would therefore **decrease water reabsorption**, working against the action of **ADH**.
*Increased blood pressure*
- **BNP** acts as a **vasodilator** and promotes fluid excretion, which typically leads to a **reduction** in blood pressure.
- Stabilizing BNP would therefore be expected to maintain or reduce **blood pressure**, not increase it.
*Inhibition of funny sodium channels*
- **Funny channels** (If channels) are primarily found in the **pacemaker cells** of the heart and are involved in controlling heart rate.
- While BNP can influence heart rate indirectly, its primary mechanism of action does not involve direct **inhibition of funny sodium channels**.
Pulmonary edema US Medical PG Question 8: A 72-year-old man with type 2 diabetes mellitus, hypertension, and systolic heart failure comes to the physician because of a 5-day history of progressively worsening shortness of breath at rest. Physical examination shows jugular venous distention, diffuse crackles over the lower lung fields, and bilateral lower extremity edema. As a part of treatment, he is given a derivative of a hormone that acts by altering guanylate cyclase activity. This drug has been found to reduce pulmonary capillary wedge pressure and causes systemic hypotension as an adverse effect. The drug is most likely a derivative of which of the following hormones?
- A. Prostacyclin
- B. Aldosterone
- C. Somatostatin
- D. Brain natriuretic peptide (Correct Answer)
- E. Angiotensin II
Pulmonary edema Explanation: ***Brain natriuretic peptide***
- **Brain natriuretic peptide (BNP)** derivatives, like nesiritide, activate **guanylate cyclase**, leading to increased cGMP, vasodilation, and reduced preload/afterload, alleviating heart failure symptoms.
- The patient's symptoms (shortness of breath, jugular venous distention, crackles, edema) are classic for **acute decompensated heart failure**, making a BNP derivative an appropriate treatment.
*Prostacyclin*
- **Prostacyclin** analogs (e.g., epoprostenol) are primarily used for **pulmonary hypertension** due to their potent vasodilatory effects in the pulmonary circulation.
- They activate **adenylyl cyclase** (increasing cAMP), not guanylate cyclase (which increases cGMP), representing a different mechanism of action.
*Aldosterone*
- **Aldosterone** is a mineralocorticoid that promotes **sodium and water retention** and potassium excretion, exacerbating heart failure symptoms.
- Its antagonists (e.g., spironolactone) are used in chronic heart failure but do not directly act via guanylate cyclase for acute symptom relief.
*Somatostatin*
- **Somatostatin** is a peptide hormone that **inhibits the secretion of various hormones**, including growth hormone, insulin, and glucagon.
- It is used in conditions like acromegaly or variceal bleeding and has no direct role in heart failure management via guanylate cyclase.
*Angiotensin II*
- **Angiotensin II** is a potent vasoconstrictor and a key component of the **renin-angiotensin-aldosterone system (RAAS)**, contributing to hypertension and heart failure progression.
- Drugs targeting angiotensin II (ACE inhibitors, ARBs) reduce its effects but do not act by directly altering guanylate cyclase activity; instead, they block its receptors or synthesis.
Pulmonary edema US Medical PG Question 9: A 25-year-old man is in the middle of an ascent up a mountain, at an elevation of about 4,500 meters. This is the 4th day of his expedition. His friend notices that in the last few hours, he has been coughing frequently and appears to be short of breath. He has used his albuterol inhaler twice in the past 4 hours, but it does not seem to help. Within the past hour, he has coughed up some frothy, slightly pink sputum and is now complaining of nausea and headache. Other than his asthma, which has been well-controlled on a steroid inhaler, he is healthy. Which of the following is the most likely cause of this man’s symptoms?
- A. An acute asthma exacerbation
- B. Non-cardiogenic pulmonary edema (Correct Answer)
- C. Pneumothorax
- D. Pulmonary embolism
- E. Acute heart failure
Pulmonary edema Explanation: ***Non-cardiogenic pulmonary edema***
- The patient's symptoms of **dyspnea**, cough, and **frothy, pink sputum** at high altitude (4,500 meters) are classic signs of **High-Altitude Pulmonary Edema (HAPE)**, a form of non-cardiogenic pulmonary edema.
- The headache and nausea are consistent with **acute mountain sickness**, which often precedes HAPE, and the ineffectiveness of albuterol points away from asthma.
*An acute asthma exacerbation*
- While the patient has a history of asthma, the **frothy, pink sputum** is atypical for asthma and strongly suggests alveolar fluid.
- The ineffectiveness of albuterol, a bronchodilator, further suggests a cause other than **bronchoconstriction** as the primary issue.
*Pneumothorax*
- A pneumothorax typically presents with **sudden onset unilateral pleuritic chest pain** and dyspnea, which can be severe.
- It would not usually cause frothy, pink sputum and is not directly linked to high altitude in the absence of trauma.
*Pulmonary embolism*
- A pulmonary embolism often causes **sudden onset dyspnea, pleuritic chest pain, and sometimes hemoptysis**, but **pink, frothy sputum** is less common.
- There are no risk factors for PE mentioned, such as prolonged immobility or recent surgery.
*Acute heart failure*
- While acute heart failure can cause **pulmonary edema with frothy, pink sputum**, the patient is a young, otherwise healthy man with no cardiac risk factors.
- The context of **high altitude** strongly points to HAPE over acute heart failure as the cause of pulmonary edema.
Pulmonary edema US Medical PG Question 10: An 82-year-old woman is admitted to the hospital because of wet gangrene on her right leg. Two days after admission, she becomes increasingly confused and tachypneic. She is intubated and ventilatory support is initiated. Her temperature is 39.6°C (102.5°F), pulse is 127/min, and blood pressure is 83/47 mm Hg. The ventilator is set at a FiO2 of 100% and a respiratory rate of 20/min. An arterial blood gas checked 30 minutes after intubation shows a PCO2 of 41 mm Hg and a PO2 of 55 mm Hg. Despite appropriate care, the patient dies from respiratory failure. Further evaluation of this patient is most likely to show which of the following findings?
- A. Fluid in the alveolar space (Correct Answer)
- B. Abscess in the lung parenchyma
- C. Nodular thickening of the interlobular septa
- D. Emboli in the pulmonary vasculature
- E. Hyperinflation of the lungs
Pulmonary edema Explanation: ***Fluid in the alveolar space***
- The patient's presentation with **wet gangrene** and subsequent development of **confusion**, **tachypnea**, **fever**, **tachycardia**, and **hypotension** is consistent with **septic shock**.
- The **severe hypoxemia** (PO2 of 55 mm Hg despite 100% FiO2) in the setting of sepsis strongly suggests **Acute Respiratory Distress Syndrome (ARDS)**, which is characterized by **non-cardiogenic pulmonary edema** or **fluid accumulation in the alveolar space**.
*Abscess in the lung parenchyma*
- A lung abscess typically presents with **purulent sputum**, **fever**, and **cough**, and while it can cause hypoxemia, it usually doesn't lead to such profound widespread respiratory failure with a normal PCO2 in the initial stages.
- The primary issue here is diffuse lung injury causing severe oxygenation impairment, not a localized collection of pus.
*Nodular thickening of the interlobular septa*
- This finding is more characteristic of **lymphangitic carcinomatosis** or certain types of **pulmonary fibrosis**, which are typically chronic conditions.
- It would not explain the acute onset of severe hypoxemia and respiratory failure in a patient with sepsis.
*Emboli in the pulmonary vasculature*
- While a **pulmonary embolism** can cause hypoxemia and could be considered in a patient with immobility, the **clinical context of septic shock** with **systemic inflammatory response** makes **ARDS the most likely diagnosis**.
- The **profound refractory hypoxemia despite 100% FiO2** and the **bilateral diffuse nature** of gas exchange impairment in this septic patient are classic for ARDS rather than PE.
- Additionally, the patient has a clear **source of infection** (wet gangrene) leading to sepsis-induced ARDS.
*Hyperinflation of the lungs*
- **Hyperinflation** is characteristic of **obstructive lung diseases** like **COPD** or **asthma**.
- It does not explain the acute onset of severe hypoxemia and respiratory failure in the context of sepsis, nor would it lead to the specific blood gas findings observed here.
More Pulmonary edema US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.