Pleural diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pleural diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pleural diseases US Medical PG Question 1: A 27-year-old man presents to the emergency department with severe dyspnea and sharp chest pain that suddenly started an hour ago after he finished exercising. He has a history of asthma as a child, and he achieves good control of his acute attacks with Ventolin. On examination, his right lung field is hyperresonant along with diminished lung sounds. Chest wall motion during respiration is asymmetrical. His blood pressure is 105/67 mm Hg, respirations are 22/min, pulse is 78/min, and temperature is 36.7°C (98.0°F). The patient is supported with oxygen, given corticosteroids, and has had analgesic medications via a nebulizer. Considering the likely condition affecting this patient, what is the best step in management?
- A. CT scan
- B. ABG
- C. Chest X-rays (Correct Answer)
- D. Tube insertion
- E. Sonogram
Pleural diseases Explanation: ***Chest X-rays***
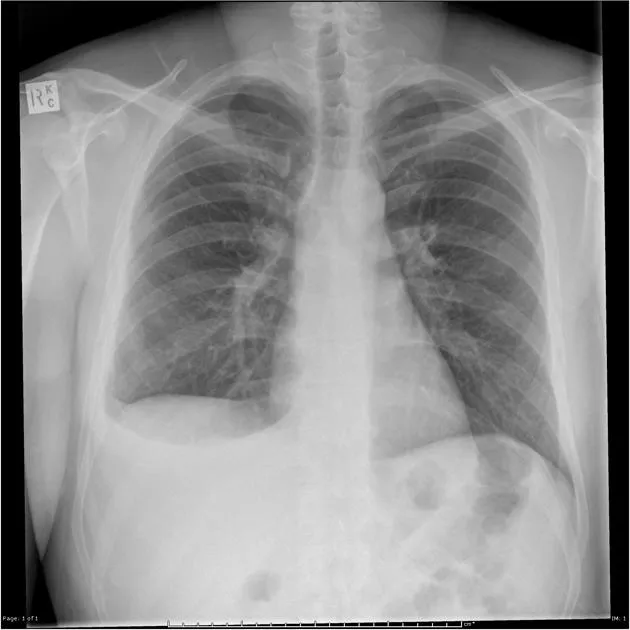
- The patient's presentation with **sudden onset dyspnea** and **sharp chest pain** post-exercise, along with **hyperresonance** and **diminished lung sounds** in the right lung field, is highly suggestive of a **spontaneous pneumothorax**.
- However, the patient is **hemodynamically stable** (BP 105/67, HR 78/min) with no signs of tension physiology (no severe hypotension, marked tachycardia, or cardiovascular collapse).
- In a stable patient with suspected pneumothorax, **chest X-ray is the appropriate first step** to confirm the diagnosis, determine the size of the pneumothorax, and guide subsequent management (observation for small pneumothorax <20%, aspiration, or tube thoracostomy for larger pneumothoraces).
- Immediate intervention without imaging is reserved for unstable patients with tension pneumothorax.
*Tube insertion*
- Chest tube insertion is the definitive treatment for large pneumothoraces (>20%) or hemodynamically unstable patients with tension pneumothorax.
- In this **stable patient**, proceeding directly to tube insertion without imaging confirmation would be premature and not following standard of care.
- The diagnosis should be confirmed and the size estimated via chest X-ray before determining if tube thoracostomy is necessary.
*CT scan*
- CT scan is not indicated as the initial diagnostic test for suspected pneumothorax.
- It provides more detail than needed for this clinical scenario and causes unnecessary delay and radiation exposure when chest X-ray is sufficient.
- CT may be useful for detecting small pneumothoraces not visible on X-ray or evaluating underlying lung disease, but is not the first-line test.
*ABG*
- An Arterial Blood Gas (ABG) might show hypoxia and respiratory alkalosis, providing information about gas exchange.
- However, ABG does not confirm the diagnosis of pneumothorax or guide immediate management decisions.
- It is an adjunctive test that does not take priority over diagnostic imaging in this scenario.
*Sonogram*
- Lung ultrasound can rapidly detect pneumothorax by showing absent lung sliding and is increasingly used in emergency settings, particularly for bedside evaluation.
- While potentially useful, **chest X-ray remains the standard initial imaging modality** for suspected pneumothorax in most emergency departments, as it provides clear documentation of pneumothorax size and is more universally available and interpreted.
- Ultrasound may be preferred in specific situations (unstable patients, point-of-care evaluation), but chest X-ray is the conventional first-line imaging test.
Pleural diseases US Medical PG Question 2: A 61-year-old man comes to the physician because of a 3-month history of worsening exertional dyspnea and a persistent dry cough. For 37 years he has worked in a naval shipyard. He has smoked 1 pack of cigarettes daily for the past 40 years. Pulmonary examination shows fine bibasilar end-expiratory crackles. An x-ray of the chest shows diffuse bilateral infiltrates predominantly in the lower lobes and pleural reticulonodular opacities. A CT scan of the chest shows pleural plaques and subpleural linear opacities. The patient is most likely to develop which of the following conditions?
- A. Malignant mesothelioma
- B. Spontaneous pneumothorax
- C. Bronchogenic carcinoma (Correct Answer)
- D. Aspergilloma
- E. Mycobacterial infection
Pleural diseases Explanation: ***Bronchogenic carcinoma***
- This patient has **asbestosis** from 37 years of shipyard work (asbestos exposure) combined with a **40-pack-year smoking history**, creating a **synergistic risk** for lung cancer.
- Asbestos exposure alone increases lung cancer risk **5-fold**, smoking alone increases it **10-fold**, but **combined exposure increases the risk 50-fold** due to synergistic effects.
- The chest imaging findings (diffuse bilateral infiltrates, pleural reticulonodular opacities, pleural plaques, and subpleural linear opacities) confirm **asbestosis**, making **bronchogenic carcinoma** the most likely future complication.
*Malignant mesothelioma*
- While strongly associated with **asbestos exposure**, it is **not synergistic with smoking** and has a lower absolute incidence compared to bronchogenic carcinoma in patients with combined exposures.
- Mesothelioma typically presents with **unilateral pleural thickening**, pleural effusion, and chest pain rather than the diffuse parenchymal infiltrates and bibasilar crackles seen here.
*Spontaneous pneumothorax*
- Characterized by sudden lung collapse with acute chest pain and dyspnea, appearing on imaging as air in the pleural space.
- While smoking-related emphysema can lead to bullae rupture and pneumothorax, the primary findings here indicate chronic interstitial lung disease and pleural pathology from asbestos exposure.
*Mycobacterial infection*
- Would typically present with constitutional symptoms (fever, night sweats, weight loss) and possibly hemoptysis, which are not mentioned in this case.
- Imaging usually shows cavitary lesions, nodules, or upper lobe predominance, differing from the diffuse lower lobe infiltrates and pleural plaques characteristic of asbestosis.
*Aspergilloma*
- A fungal ball within a pre-existing cavity, typically seen in patients with tuberculosis, sarcoidosis, or other chronic cavitary lung diseases.
- The clinical presentation and imaging findings, particularly the occupational asbestos exposure and smoking history, point toward malignancy risk rather than fungal colonization.
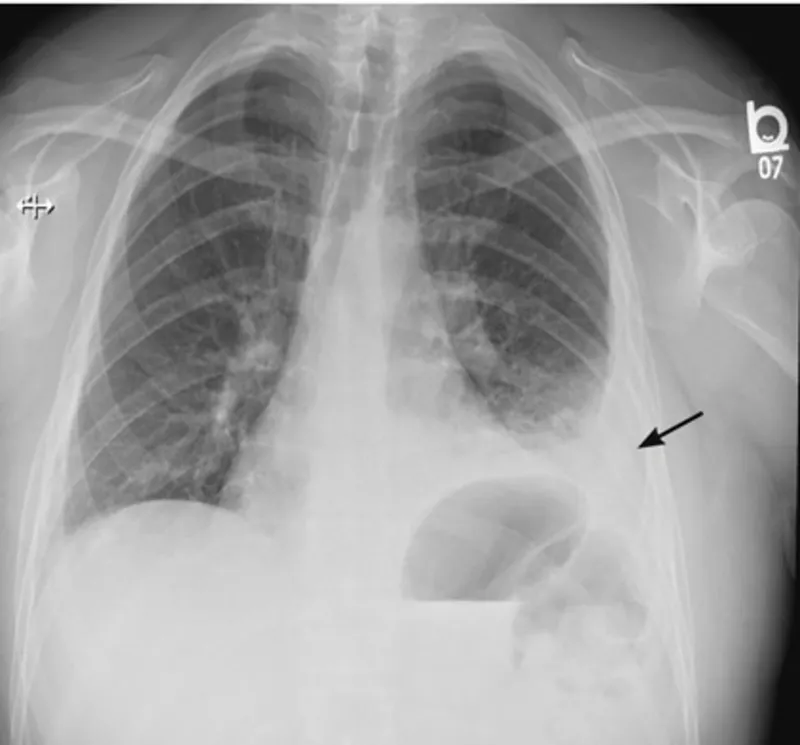
Pleural diseases US Medical PG Question 3: A 17-year-old boy is brought to the emergency department by his parents 6 hours after he suddenly began to experience dyspnea and pleuritic chest pain at home. He has a remote history of asthma in childhood but has not required any treatment since the age of four. His temperature is 98.4°F (36.9°C), blood pressure is 100/76 mmHg, pulse is 125/min, respirations are 24/min. On exam, he has decreased lung sounds and hyperresonance in the left upper lung field. A chest radiograph shows a slight tracheal shift to the right. What is the best next step in management?
- A. Needle decompression
- B. CT scan for apical blebs
- C. Observe for another six hours for resolution
- D. Chest tube placement (Correct Answer)
- E. Pleurodesis
Pleural diseases Explanation: ***Chest tube placement***
- The patient's presentation with **sudden dyspnea**, **pleuritic chest pain**, **decreased lung sounds**, **hyperresonance**, **tachycardia**, and **tracheal shift** indicates a **tension pneumothorax**, which requires immediate **chest tube insertion** for definitive management.
- While the tracheal shift might suggest tension pneumothorax, the patient's relative **hemodynamic stability** (BP 100/76, pulse 125/min) and the fact that he was stable for 6 hours implies it's a large **primary spontaneous pneumothorax** rather than an emergent tension pneumothorax. A chest tube is the appropriate next step for symptomatic patients with a large pneumothorax.
*Needle decompression*
- This procedure is reserved for true **tension pneumothorax** where there is imminent **hemodynamic compromise** (e.g., hypotension, severe tachycardia, hypoxemia) due to severe intrathoracic pressure buildup.
- The patient's blood pressure is stable, indicating that while there is a significant pneumothorax, it's not immediately life-threatening enough to warrant needle decompression before chest tube placement.
*CT scan for apical blebs*
- A **CT scan** might be useful for identifying the cause of the pneumothorax, such as **apical blebs**, but it's not an immediate management step for an acute, symptomatic pneumothorax.
- Prioritizing definitive treatment to reinflate the lung and relieve symptoms is crucial before investigating the underlying cause.
*Observe for another six hours for resolution*
- Observation is only appropriate for **small, asymptomatic pneumothoraces**.
- This patient is symptomatic with significant findings (dyspnea, chest pain, decreased lung sounds, hyperresonance, slight tracheal shift), making observation an unsafe option.
*Pleurodesis*
- **Pleurodesis** is a procedure used to prevent recurrent pneumothoraces and is typically performed after the acute event has been resolved, or for patients with **recurrent pneumothoraces**.
- It is not an acute management step for a new, symptomatic pneumothorax.
Pleural diseases US Medical PG Question 4: A 72-year-old man presents with shortness of breath and right-sided chest pain. Physical exam reveals decreased breath sounds and dull percussion at the right lung base. Chest X-ray reveals a right-sided pleural effusion. A thoracentesis was performed, removing 450 mL of light pink fluid. Pleural fluid analysis reveals:
Pleural fluid to serum protein ratio: 0.35
Pleural fluid to serum LDH ratio: 0.49
Lactate dehydrogenase (LDH): 105 IU (serum LDH Reference: 100–190)
Which of the following disorders is most likely in this patient?
- A. Congestive heart failure (Correct Answer)
- B. Uremia
- C. Chylothorax
- D. Pancreatitis
- E. Sarcoidosis
Pleural diseases Explanation: ***Congestive heart failure***
- The **pleural fluid to serum protein ratio of 0.35** and **LDH ratio of 0.49** fall within the criteria for a **transudative effusion** (ratios < 0.5 for protein and < 0.6 for LDH).
- **Congestive heart failure (CHF)** is a common cause of transudative pleural effusions due to increased hydrostatic pressure.
*Uremia*
- **Uremic pleuritis** typically causes an **exudative effusion**, characterized by higher protein and LDH levels in the pleural fluid.
- While patients with uremia may have pleural effusions, the fluid analysis here is not consistent with that diagnosis.
*Chylothorax*
- A **chylothorax** is characterized by a **milky-white fluid** with very high triglyceride levels (>110 mg/dL), resulting from lymphatic leakage.
- The described fluid is "light pink" and does not have the typical biochemical profile of a chylothorax.
*Pancreatitis*
- **Pancreatitis-induced pleural effusions** are almost always **exudative** and typically have **elevated amylase levels**.
- The transudative nature of the effusion rules out pancreatitis as the most likely cause.
*Sarcoidosis*
- **Sarcoidosis** can cause **pleural effusions**, but these are usually **exudative** and often accompanied by other systemic manifestations like lymphadenopathy or skin lesions.
- The presented fluid analysis does not support a diagnosis of sarcoidosis.
Pleural diseases US Medical PG Question 5: A 49-year-old man comes to the hospital for a 10-day history of cough and worsening shortness of breath. He has sharp right-sided chest pain that worsens on inspiration and coughing. Two weeks ago, the patient was admitted to the hospital after passing out on the street from alcohol intoxication but he left against medical advice. He has coronary artery disease and hypertension, and he does not take any medications. He drinks 4 cans of beer daily and has smoked 2 packs of cigarettes daily for 20 years. His temperature is 38.5°C (101.3° F), pulse is 110/min, respirations are 29/min, and blood pressure is 110/65 mmHg. Examination shows poor dentition. There is dullness to percussion at the base of the right lung. Crackles and markedly decreased breath sounds are heard over the right middle and lower lung fields. An x-ray of the chest shows a right-sided loculated pleural effusion and consolidation of the surrounding lung with visible air bronchogram; there are no rib fractures. Thoracocentesis is performed. Examination of this patient's pleural fluid is most likely to show which of the following findings?
- A. Lymphocytosis of > 90%
- B. Pleural fluid LDH/serum LDH ratio of 0.5
- C. Lactate dehydrogenase of 45 U/L
- D. Amylase of 200 U/L
- E. Glucose of 30 mg/dL (Correct Answer)
Pleural diseases Explanation: ***Glucose of 30 mg/dL***
- This patient presents with symptoms and signs of a **parapneumonic effusion** that is likely complicated, given the **loculated pleural effusion** and **low pleural fluid glucose**. Alcoholism and poor dentition increase the risk of aspiration and subsequent bacterial pneumonia leading to empyema.
- A pleural fluid glucose level of **<60 mg/dL** (or significantly lower than serum glucose) is characteristic of a complicated parapneumonic effusion or empyema due to high metabolic activity by bacteria and local inflammatory cells.
*Lymphocytosis of > 90%*
- Marked pleural fluid **lymphocytosis** (>80-90% lymphocytes) is typically seen in **tuberculous pleurisy** or malignancy, not acute bacterial pneumonia with empyema.
- This patient's acute presentation, fever, and consolidation are not typical of tuberculosis, which usually has a more subacute or chronic course.
*Pleural fluid LDH/serum LDH ratio of 0.5*
- A pleural fluid LDH/serum LDH ratio >0.6 is one of **Light's criteria** for an exudative effusion, consistent with this patient's likely empyema. A ratio of 0.5 would make the effusion less definitively exudative by certain criteria alone.
- However, for complicated parapneumonic effusions or empyema, LDH levels in the pleural fluid are typically **very high** (>1000 U/L), making the ratio with serum LDH also high, usually >0.6.
*Lactate dehydrogenase of 45 U/L*
- A pleural fluid **LDH of 45 U/L** is a very low value, typically seen in a **transudative effusion** (e.g., heart failure, cirrhosis).
- Complicated parapneumonic effusions and empyema are exudative and characterized by **high pleural fluid LDH** due to inflammation and cell lysis, usually >1000 IU/L.
*Amylase of 200 U/L*
- Elevated pleural fluid **amylase** (often > normal serum level or > two times serum level) is suggestive of **pancreatitis**, **esophageal rupture**, or malignancy.
- While aspiration can sometimes involve pancreatic enzymes if gastric contents are aspirated, the primary clinical picture aligns with bacterial pneumonia and empyema, where amylase elevation is not a key diagnostic feature.
Pleural diseases US Medical PG Question 6: A 31 year-old African-American female presents with painful shin nodules, uveitis, and calcified hilar lymph nodes. A transbronchial biopsy of the lung would most likely show which of the following histologies?
- A. Golden-brown fusiform rods
- B. Inflammation, fibrosis and cyst formation that is most prominent in subpleural regions
- C. Non-caseating granulomas (Correct Answer)
- D. Silica particles (birefringent) surrounded by collagen
- E. Patchy interstitial lymphoid infiltrate into walls of alveolar units
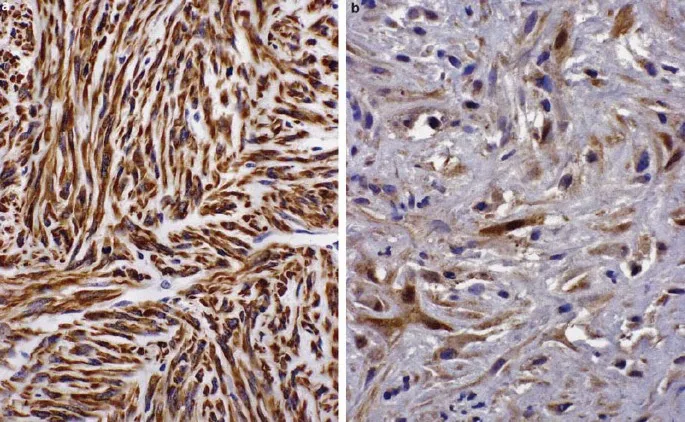
Pleural diseases Explanation: ***Non-caseating granulomas***
- The constellation of **erythema nodosum** (painful shin nodules), **uveitis**, and **hilar lymphadenopathy** in an African-American female is highly characteristic of **sarcoidosis**.
- **Sarcoidosis** is pathologically defined by the presence of **non-caseating granulomas** in affected tissues, which would be visible on a transbronchial biopsy.
*Golden-brown fusiform rods*
- These are **ferruginous bodies**, characteristic of **asbestosis**, which is not supported by the patient's presentation.
- Asbestosis would typically involve a history of **asbestos exposure** and present with **pleural plaques** or **interstitial fibrosis**.
*Inflammation, fibrosis and cyst formation that is most prominent in subpleural regions*
- This description is more indicative of **pulmonary Langerhans cell histiocytosis**, a rare disease usually associated with **smoking**.
- It does not align with the patient's specific systemic manifestations like uveitis or erythema nodosum.
*Silica particles (birefringent) surrounded by collagen*
- This describes the histological findings of **silicosis**, an occupational lung disease resulting from exposure to **silica dust**.
- Silicosis is not typically associated with uveitis or erythema nodosum.
*Patchy interstitial lymphoid infiltrate into walls of alveolar units*
- This pattern can be seen in various interstitial lung diseases, but it is not specific for sarcoidosis.
- It could be found in conditions like **lymphoid interstitial pneumonia**, which does not fit the overall clinical picture.
Pleural diseases US Medical PG Question 7: A 68-year-old male smoker dies suddenly in a car accident. He had smoked 2 packs per day for 40 years. His past medical history is notable for a frequent, very productive cough, recurrent respiratory infections and occasional wheezing. He had no other medical problems. At autopsy, which of the following is most likely to be found in this patient?
- A. Increased number and activity of goblet cells (Correct Answer)
- B. Ferruginous bodies
- C. Mucous gland atrophy
- D. Interstitial fibrosis of the lung
- E. Pleural plaques
Pleural diseases Explanation: ***Increased number and activity of goblet cells***
- The patient's history of a **productive cough**, **recurrent respiratory infections**, and **wheezing** in a chronic smoker strongly indicates **chronic bronchitis**.
- **Chronic bronchitis** is pathologically characterized by **hypertrophy of mucous glands** and an **increase in goblet cell number and activity**, leading to excessive mucus production.
*Ferruginous bodies*
- **Ferruginous bodies** are typically found in **asbestosis**, a lung disease caused by asbestos exposure.
- While asbestos exposure can cause respiratory symptoms, the sudden death and clinical picture without specific exposure history do not point to asbestosis as the primary diagnosis.
*Mucous gland atrophy*
- **Mucous gland atrophy** is generally not associated with chronic smoking and the symptoms described.
- In conditions like chronic bronchitis, there is actually **hypertrophy** and **hyperplasia** of the mucous glands, leading to increased mucus production.
*Interstitial fibrosis of the lung*
- **Interstitial fibrosis** is characteristic of conditions like **idiopathic pulmonary fibrosis** or other **interstitial lung diseases**.
- While smoking is a risk factor for some forms of fibrosis, the predominant symptoms of a productive cough and recurrent infections are more indicative of chronic bronchitis rather than diffuse interstitial fibrosis.
*Pleural plaques*
- **Pleural plaques** are **fibrous thickenings of the pleura**, almost exclusively associated with **asbestos exposure**.
- They are usually asymptomatic and do not directly explain the productive cough, recurrent infections, and wheezing presented in this patient's history.
Pleural diseases US Medical PG Question 8: A 44-year-old man comes to the physician because of a 5-month history of persistent cough productive of thick, yellow sputum and worsening shortness of breath. One year ago, he had similar symptoms that lasted 4 months. He has smoked two packs of cigarettes daily for the past 20 years. Physical examination shows scattered expiratory wheezing and rhonchi throughout both lung fields. Microscopic examination of a lung biopsy specimen is most likely to show which of the following findings?
- A. Decreased smooth muscle cells
- B. Decreased alveolar macrophages
- C. Increased ciliated epithelial cells
- D. Increased goblet cells (Correct Answer)
- E. Increased club cells
Pleural diseases Explanation: **Increased goblet cells**
- This patient's presentation of persistent cough with thick, yellow sputum, worsening shortness of breath, and a history of heavy smoking points towards **chronic bronchitis**.
- **Chronic bronchitis** is pathologically defined by **mucus gland hyperplasia** and **goblet cell hypertrophy** in the bronchial airways, leading to excessive mucus production.
*Decreased smooth muscle cells*
- Airway smooth muscle can undergo **hyperplasia** and **hypertrophy** in chronic obstructive pulmonary diseases (COPD) like chronic bronchitis, rather than a decrease.
- A decrease in smooth muscle cells is not a characteristic pathological finding in chronic bronchitis.
*Decreased alveolar macrophages*
- **Alveolar macrophages** are crucial for clearing inhaled particles and pathogens and are typically **increased** or functionally altered in chronic inflammatory lung conditions.
- A decrease in these immune cells would not be a typical finding in chronic bronchitis and would likely lead to increased susceptibility to infections.
*Increased ciliated epithelial cells*
- In chronic bronchitis, there is often a **loss of ciliated epithelial cells** as they are replaced by **goblet cells** and undergo **squamous metaplasia** due to chronic irritation.
- The remaining ciliated cells may be dysfunctional, impairing mucociliary clearance.
*Increased club cells*
- **Club cells** (formerly Clara cells) are non-ciliated, secretory cells found in the small airways that protect the bronchiolar epithelium.
- While they play a role in airway defense, their significant increase is not a primary or characteristic pathological feature of chronic bronchitis.
Pleural diseases US Medical PG Question 9: A 63-year-old man with alpha-1-antitrypsin deficiency is brought to the emergency department 1 hour after his daughter found him unresponsive. Despite appropriate care, the patient dies. At autopsy, examination of the lungs shows enlargement of the airspaces in the respiratory bronchioles and alveoli. Enzymatic activity of which of the following cells is the most likely cause of these findings?
- A. Alveolar macrophages (Correct Answer)
- B. Ciliated bronchiolar epithelial cells
- C. Elastic fibers in alveolar septa
- D. Type I pneumocytes
- E. Alveolar septal cells
Pleural diseases Explanation: ***Alveolar macrophages***
- In **alpha-1-antitrypsin deficiency**, alveolar macrophages (and neutrophils) release **elastase**, which is normally inhibited by alpha-1-antitrypsin.
- Unchecked elastase activity from alveolar macrophages leads to the **destruction of elastic fibers** in the alveolar walls, causing emphysema with characteristic **panacinar** distribution (worse in lower lobes).
- This results in enlargement of airspaces distal to terminal bronchioles.
*Ciliated bronchiolar epithelial cells*
- These cells are primarily involved in **mucociliary clearance** and do not produce proteolytic enzymes that degrade elastic tissue.
- Their dysfunction would lead to impaired mucus clearance and increased susceptibility to infections, but not emphysema.
*Elastic fibers in alveolar septa*
- Elastic fibers are **extracellular matrix components**, not cells.
- While their destruction is the pathological mechanism of emphysema, they do not have enzymatic activity.
*Type I pneumocytes*
- **Type I pneumocytes** form the structural lining of the alveoli and are primarily involved in gas exchange.
- They do not produce elastase or other proteolytic enzymes responsible for tissue destruction in emphysema.
*Alveolar septal cells*
- This term broadly refers to structural cells including Type I and Type II pneumocytes.
- While these cells may be damaged secondarily in emphysema, they do not produce the elastase responsible for elastic fiber destruction.
Pleural diseases US Medical PG Question 10: A 60-year-old man who is a chronic smoker comes to the hospital with the chief complaint of shortness of breath which has worsened over the past 2 days. He also has a productive cough with yellowish sputum. There is no history of hemoptysis, chest pain, fever, palpitations, or leg swelling. He had a viral illness one week ago. He has been using an inhaler for 10 years for his respiratory disease. He sleeps with 2 pillows every night. He received 100 mg of hydrocortisone and antibiotics in the emergency department, and his symptoms have subsided. His FEV1/FVC ratio is < 0.70, and FEV1 is 40% of predicted. What is the most likely finding that can be discovered from the histology of his bronchi?
- A. Increase Reid index (Correct Answer)
- B. Curschmann spirals
- C. Non-caseating granuloma
- D. Ferruginous bodies
- E. Charcot-Leyden crystals
Pleural diseases Explanation: ***Increase Reid index***
- The patient's history of **chronic smoking**, progressive dyspnea, productive cough, and **obstructive spirometry** (FEV1/FVC < 0.70, FEV1 40% predicted) are highly suggestive of **chronic bronchitis**, a component of COPD.
- An increased **Reid index** (ratio of the thickness of the submucosal gland layer to the thickness of the bronchial wall cartilage) is a characteristic histological finding in **chronic bronchitis**, reflecting **mucous gland hypertrophy** and hyperplasia.
*Curschmann spirals*
- These are **mucus plugs** that have been molded into twisted spirals from smaller airways and are characteristic of **bronchial asthma**.
- While both asthma and COPD involve airway obstruction, the patient's history (chronic smoker, long-standing symptoms, FEV1/FVC < 0.70) points more strongly to **COPD** (chronic bronchitis and/or emphysema) rather than asthma as the primary condition.
*Non-caseating granuloma*
- This is a hallmark histological finding of **sarcoidosis**, a multisystem inflammatory disease.
- The patient's symptoms and history are not consistent with sarcoidosis, and there is no mention of other typical manifestations such as erythema nodosum or hilar lymphadenopathy.
*Ferruginous bodies*
- These are **asbestos fibers** coated with an iron-containing protein, found in the lungs of individuals with **asbestosis**.
- The patient's history does not indicate any exposure to asbestos, and his symptoms are more aligned with chronic obstructive pulmonary disease.
*Charcot-Leyden crystals*
- These are microscopic crystals found in the sputum of patients with allergic diseases, particularly **bronchial asthma**, formed from the breakdown products of eosinophils.
- While the patient uses an inhaler, the overall clinical picture, especially chronic smoking history and severe persistent obstruction, makes **chronic bronchitis** more likely than asthma as the predominant underlying pathology.
More Pleural diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.