Obstructive lung diseases (emphysema, bronchitis) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Obstructive lung diseases (emphysema, bronchitis). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 1: A 60-year-old man who is a chronic smoker comes to the hospital with the chief complaint of shortness of breath which has worsened over the past 2 days. He also has a productive cough with yellowish sputum. There is no history of hemoptysis, chest pain, fever, palpitations, or leg swelling. He had a viral illness one week ago. He has been using an inhaler for 10 years for his respiratory disease. He sleeps with 2 pillows every night. He received 100 mg of hydrocortisone and antibiotics in the emergency department, and his symptoms have subsided. His FEV1/FVC ratio is < 0.70, and FEV1 is 40% of predicted. What is the most likely finding that can be discovered from the histology of his bronchi?
- A. Increase Reid index (Correct Answer)
- B. Curschmann spirals
- C. Non-caseating granuloma
- D. Ferruginous bodies
- E. Charcot-Leyden crystals
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Increase Reid index***
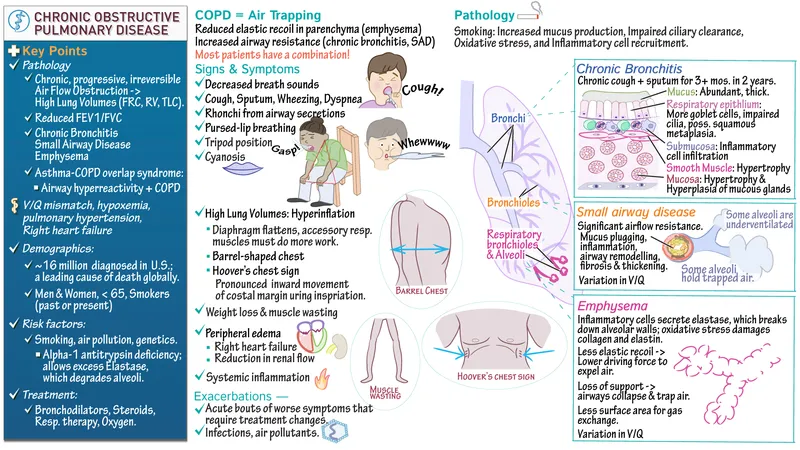
- The patient's history of **chronic smoking**, progressive dyspnea, productive cough, and **obstructive spirometry** (FEV1/FVC < 0.70, FEV1 40% predicted) are highly suggestive of **chronic bronchitis**, a component of COPD.
- An increased **Reid index** (ratio of the thickness of the submucosal gland layer to the thickness of the bronchial wall cartilage) is a characteristic histological finding in **chronic bronchitis**, reflecting **mucous gland hypertrophy** and hyperplasia.
*Curschmann spirals*
- These are **mucus plugs** that have been molded into twisted spirals from smaller airways and are characteristic of **bronchial asthma**.
- While both asthma and COPD involve airway obstruction, the patient's history (chronic smoker, long-standing symptoms, FEV1/FVC < 0.70) points more strongly to **COPD** (chronic bronchitis and/or emphysema) rather than asthma as the primary condition.
*Non-caseating granuloma*
- This is a hallmark histological finding of **sarcoidosis**, a multisystem inflammatory disease.
- The patient's symptoms and history are not consistent with sarcoidosis, and there is no mention of other typical manifestations such as erythema nodosum or hilar lymphadenopathy.
*Ferruginous bodies*
- These are **asbestos fibers** coated with an iron-containing protein, found in the lungs of individuals with **asbestosis**.
- The patient's history does not indicate any exposure to asbestos, and his symptoms are more aligned with chronic obstructive pulmonary disease.
*Charcot-Leyden crystals*
- These are microscopic crystals found in the sputum of patients with allergic diseases, particularly **bronchial asthma**, formed from the breakdown products of eosinophils.
- While the patient uses an inhaler, the overall clinical picture, especially chronic smoking history and severe persistent obstruction, makes **chronic bronchitis** more likely than asthma as the predominant underlying pathology.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 2: A 28-year-old patient presents to the hospital complaining of progressively worsening dyspnea and a dry cough. Radiographic imaging is shown below. Pulmonary function testing (PFT's) reveals a decreased FEV1 and FEV1/FVC, but an increased TLC. The patient states that he does not smoke. Which of the following conditions is most consistent with the patient's symptoms?
- A. Hypersensitivity pneumonitis
- B. Chronic bronchitis
- C. Alpha1-antitrypsin deficiency (Correct Answer)
- D. Pneumothorax
- E. Asthma
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Alpha1-antitrypsin deficiency***
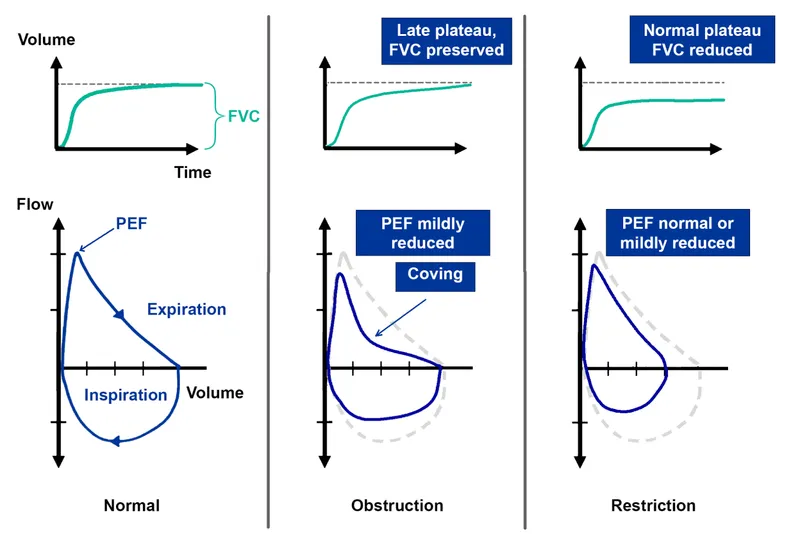
- The combination of **decreased FEV1**, **decreased FEV1/FVC**, and **increased TLC** without a history of smoking is highly suggestive of **emphysema**, which can be caused by alpha1-antitrypsin deficiency.
- This genetic condition leads to a lack of protection against **elastase**, causing early-onset panacinar emphysema, typically affecting the lung bases even in non-smokers.
*Hypersensitivity pneumonitis*
- This condition typically presents with a **restrictive pattern** on PFTs (decreased TLC, normal or increased FEV1/FVC), not an obstructive pattern with increased TLC.
- It is an immune-mediated interstitial lung disease, often presenting with symptoms like dyspnea and cough, but the PFTs are inconsistent.
*Chronic bronchitis*
- While chronic bronchitis causes an **obstructive pattern** (decreased FEV1, decreased FEV1/FVC), it primarily manifests with a **chronic productive cough** (at least three months per year for two consecutive years) and is usually associated with smoking.
- An **increased TLC** is not typical in isolated chronic bronchitis; TLC is often normal or slightly increased, but not as pronounced as in emphysema.
*Pneumothorax*
- A pneumothorax is an acute condition involving air in the pleural space, leading to sudden onset dyspnea and chest pain, and would show a **collapsed lung** on imaging, not an obstructive pattern with increased TLC.
- It results in a **reduced lung volume** and would not cause an obstructive pattern with increased TLC on PFTs.
*Asthma*
- Asthma presents with **reversible airway obstruction** (decreased FEV1, decreased FEV1/FVC) but usually involves episodic wheezing and dyspnea, often triggered by allergens.
- While TLC can be increased during severe exacerbations due to **air trapping**, patients usually respond to bronchodilators and do not typically present with progressive, non-reversible obstruction and uniformly increased TLC like emphysema.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 3: A 63-year-old man with alpha-1-antitrypsin deficiency is brought to the emergency department 1 hour after his daughter found him unresponsive. Despite appropriate care, the patient dies. At autopsy, examination of the lungs shows enlargement of the airspaces in the respiratory bronchioles and alveoli. Enzymatic activity of which of the following cells is the most likely cause of these findings?
- A. Alveolar macrophages (Correct Answer)
- B. Ciliated bronchiolar epithelial cells
- C. Elastic fibers in alveolar septa
- D. Type I pneumocytes
- E. Alveolar septal cells
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Alveolar macrophages***
- In **alpha-1-antitrypsin deficiency**, alveolar macrophages (and neutrophils) release **elastase**, which is normally inhibited by alpha-1-antitrypsin.
- Unchecked elastase activity from alveolar macrophages leads to the **destruction of elastic fibers** in the alveolar walls, causing emphysema with characteristic **panacinar** distribution (worse in lower lobes).
- This results in enlargement of airspaces distal to terminal bronchioles.
*Ciliated bronchiolar epithelial cells*
- These cells are primarily involved in **mucociliary clearance** and do not produce proteolytic enzymes that degrade elastic tissue.
- Their dysfunction would lead to impaired mucus clearance and increased susceptibility to infections, but not emphysema.
*Elastic fibers in alveolar septa*
- Elastic fibers are **extracellular matrix components**, not cells.
- While their destruction is the pathological mechanism of emphysema, they do not have enzymatic activity.
*Type I pneumocytes*
- **Type I pneumocytes** form the structural lining of the alveoli and are primarily involved in gas exchange.
- They do not produce elastase or other proteolytic enzymes responsible for tissue destruction in emphysema.
*Alveolar septal cells*
- This term broadly refers to structural cells including Type I and Type II pneumocytes.
- While these cells may be damaged secondarily in emphysema, they do not produce the elastase responsible for elastic fiber destruction.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 4: A 48-year-old man comes to the physician because of a 3-month history of worsening shortness of breath and cough productive of frothy, whitish sputum. One year ago, he had a similar episode lasting 6 months. He has smoked a pack of cigarettes daily for 25 years. Physical examination shows bluish discoloration of the tongue and lips. Scattered expiratory wheezing and rhonchi are heard throughout both lung fields. Further evaluation of this patient is most likely to show which of the following findings?
- A. Increased FEV1/FVC ratio
- B. Increased diffusing capacity for carbon monoxide
- C. Increased pulmonary capillary wedge pressure
- D. Increased serum hematocrit (Correct Answer)
- E. Normal FEV1
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Increased serum hematocrit***
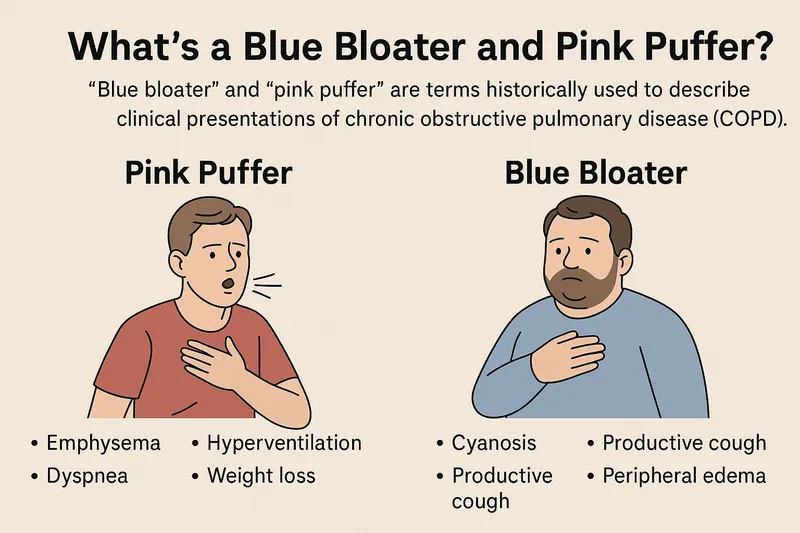
- This patient presents with symptoms highly suggestive of **chronic bronchitis**, a form of COPD, characterized by a **chronic productive cough** and **hypoxemia**.
- **Chronic hypoxemia** stimulates the kidneys to release **erythropoietin**, leading to secondary **polycythemia** (increased red blood cell mass) and thus an **increased hematocrit** to improve oxygen-carrying capacity.
*Increased FEV1/FVC ratio*
- This patient's symptoms (shortness of breath, productive cough, wheezing, smoking history) are classic for **chronic obstructive pulmonary disease (COPD)**, which is an **obstructive lung disease**.
- Obstructive lung diseases are characterized by **decreased FEV1/FVC ratio** due to airflow limitation, not an increased ratio.
*Increased diffusing capacity for carbon monoxide*
- In COPD, particularly chronic bronchitis and emphysema, the **diffusing capacity for carbon monoxide (DLCO)** is typically **decreased** due to destruction of alveolar-capillary membranes (emphysema) and ventilation-perfusion mismatch (chronic bronchitis).
- An increased DLCO is more commonly seen in conditions like **pulmonary hemorrhage** or **asthma**.
*Increased pulmonary capillary wedge pressure*
- **Increased pulmonary capillary wedge pressure (PCWP)** is characteristic of **left-sided heart failure**, indicating elevated left atrial and pulmonary venous pressures.
- While patients with severe COPD can develop **pulmonary hypertension** and eventually **right-sided heart failure (cor pulmonale)**, the primary pathology described here points to lung disease, not left ventricular dysfunction.
*Normal FEV1*
- In COPD, there is **airflow obstruction** that manifests as a **reduced forced expiratory volume in 1 second (FEV1)**.
- A normal FEV1 would be inconsistent with the clinical presentation of significant, worsening shortness of breath and airflow limitation.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 5: A 62-year-old woman with hypertension and type 2 diabetes mellitus comes to the physician because of increasing shortness of breath and a dry cough over the past 6 months. She has smoked 1 pack of cigarettes daily for the past 40 years. Chest auscultation shows scattered expiratory wheezes in both lung fields. Spirometry shows an FEV1:FVC ratio of 65% and an FEV1 of 70% of predicted. Her diffusing capacity for carbon monoxide (DLCO) is 42% of predicted. Which of the following is the most likely diagnosis?
- A. Pulmonary fibrosis
- B. Bronchial asthma
- C. Emphysema (Correct Answer)
- D. Bronchiectasis
- E. Chronic bronchitis
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Emphysema***
- The patient's history of **40 pack-years of smoking**, combined with **obstructive lung disease (FEV1:FVC ratio of 65%)** and a **markedly reduced DLCO (42% of predicted)**, strongly indicates emphysema.
- **DLCO reduction** is characteristic of emphysema due to the destruction of alveolar-capillary membranes, which impairs gas exchange.
*Pulmonary fibrosis*
- Pulmonary fibrosis presents with shortness of breath and dry cough, but it is a **restrictive lung disease**, meaning both FEV1 and FVC would be reduced proportionally, leading to a **normal or increased FEV1:FVC ratio**.
- While DLCO is reduced in pulmonary fibrosis, the **obstructive pattern on spirometry** rules out this diagnosis.
*Bronchial asthma*
- Asthma is characterized by **reversible airway obstruction** and often presents with wheezing and shortness of breath.
- However, asthma typically has a **normal DLCO**, as the diffusion capacity of the lung is usually preserved.
*Bronchiectasis*
- Bronchiectasis involves **permanent dilation of the bronchi** and can cause chronic cough, sputum production, and obstructive lung physiology.
- While it can cause some airflow obstruction and reduced DLCO in severe cases, the **primary features often include chronic productive cough** and recurrent infections, and the DLCO reduction is typically less severe than seen in emphysema, unless it's very advanced.
*Chronic bronchitis*
- Chronic bronchitis is defined by a **chronic productive cough** for at least 3 months in each of 2 consecutive years, in a patient for whom other causes have been excluded.
- It causes **obstructive lung disease** and can present with wheezing but typically has a **normal or only slightly reduced DLCO**, as the primary issue is inflammation and mucus production in the airways, not destruction of the alveolar-capillary membrane.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 6: An 8-year-old boy presents to his pediatrician accompanied by his father with a complaint of chronic cough. For the past 2 months he has been coughing up yellow, foul-smelling sputum. He has been treated at a local urgent care center for multiple episodes of otitis media, sinusitis, and bronchitis since 2 years of age. His family history is unremarkable. At the pediatrician's office, his temperature is 99.2°F (37.3°C), blood pressure is 110/84 mmHg, pulse is 95/min, and respirations are 20/min. Inspection shows a young boy who coughs occasionally during examination. Pulmonary exam demonstrates diffuse wheezing and crackles bilaterally. Mild clubbing is present on the fingers. The father has brought an electrocardiogram (ECG) from the patient’s last urgent care visit that shows pronounced right axis deviation. Which of the following is the most likely etiology of this patient’s condition?
- A. Failure of neural crest cell migration
- B. Maldevelopment of pharyngeal pouches
- C. Transient bronchoconstriction
- D. Defective maturation of B-lymphocytes
- E. Decreased motility of cilia (Correct Answer)
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Decreased motility of cilia***
- The recurrent respiratory infections (**otitis media, sinusitis, bronchitis**), chronic productive cough with **foul-smelling sputum**, and **bronchiectasis** (implied by chronic cough, wheezing, crackles) are highly suggestive of **primary ciliary dyskinesia (PCD)**.
- **Clubbing** and **right axis deviation** (suggesting right ventricular hypertrophy from pulmonary hypertension) are complications of chronic lung disease such as severe bronchiectasis, which is characteristic of PCD.
*Failure of neural crest cell migration*
- This is associated with conditions like **DiGeorge syndrome** or **Hirschsprung disease**, which present with different clinical features (e.g., cardiac defects, hypocalcemia, intestinal obstruction).
- It does not directly explain the recurrent respiratory tract infections and bronchiectasis seen in this patient.
*Maldevelopment of pharyngeal pouches*
- Similar to neural crest cell defects, issues with pharyngeal pouch development (e.g., **DiGeorge syndrome**) affect the immune system and cardiac structures.
- While it can lead to recurrent infections, it typically involves **T-cell deficiencies** and specific cardiac anomalies, rather than chronic suppurative respiratory disease and bronchiectasis as the primary presentation.
*Transient bronchoconstriction*
- This describes conditions like **asthma**, which causes reversible airway narrowing and wheezing.
- However, asthma does not explain the chronic **foul-smelling sputum**, **clubbing**, persistent recurrent infections like otitis media and sinusitis, or the development of bronchiectasis.
*Defective maturation of B-lymphocytes*
- This leads to **immunodeficiencies** primarily affecting **antibody production**, such as **X-linked agammaglobulinemia**.
- While patients would experience recurrent bacterial infections, the specific pattern of chronic sinusitis, otitis, and bronchiectasis with **foul-smelling sputum** (suggesting chronic bacterial colonization and impaired clearance) points more towards a structural or ciliary defect than a purely humoral immune deficiency.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 7: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 8: A 72-year-old man is brought to the emergency department after an episode of hemoptysis. He has a chronic cough that is productive of copious sputum. Six years ago, he had a stroke that left him with difficulty swallowing. He smoked one pack of cigarettes daily for 40 years, but quit 2 years ago. His respirations are 25/min and labored. Physical examination shows digital clubbing. An x-ray of the chest shows tram track opacities in the lower lung fields. Which of the following is the most likely diagnosis?
- A. Aspiration pneumonia
- B. Bronchiectasis (Correct Answer)
- C. Emphysema
- D. Lung cancer
- E. Chronic bronchitis
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Bronchiectasis***
- The combination of **chronic cough with copious sputum**, **hemoptysis**, **digital clubbing**, and **tram track opacities** on chest x-ray is highly characteristic of bronchiectasis.
- The patient's history of difficulty swallowing following a stroke suggests a risk factor for recurrent aspirations leading to chronic infection and airway damage characteristic of bronchiectasis.
*Aspiration pneumonia*
- While the patient has a risk factor for aspiration due to difficulty swallowing, aspiration pneumonia typically presents as an acute infection with fever and infiltrates, rather than chronic symptoms and specific radiographic findings like **tram track opacities** and **digital clubbing**.
- Aspiration pneumonia may lead to bronchiectasis if chronic, but it is not the most definitive diagnosis given the full constellation of findings described.
*Emphysema*
- Emphysema is a form of COPD characterized by destruction of alveolar walls and presents with **dyspnea**, **barrel chest**, and often a history of smoking, but does not typically cause **hemoptysis** or **tram track opacities**.
- Chest x-rays in emphysema usually show **hyperinflation** and **flattened diaphragms**, not specific airway dilation.
*Lung cancer*
- While **hemoptysis** and **chronic cough** can be symptoms of lung cancer, and the patient has a significant smoking history, lung cancer does not typically cause **copious sputum** or **tram track opacities**.
- Although digital clubbing can occur with lung cancer as a paraneoplastic syndrome, the presence of **tram track opacities** is pathognomonic for bronchiectasis and points strongly to this diagnosis.
*Chronic bronchitis*
- Chronic bronchitis is defined by a **chronic productive cough** for at least three months in two consecutive years and is associated with smoking.
- However, it does not typically cause **hemoptysis**, **digital clubbing**, or the specific **tram track opacities** seen on x-ray, which indicate bronchial wall thickening and dilation.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 9: A 61-year-old male presents to your office with fever and dyspnea on exertion. He has been suffering from chronic, non-productive cough for 1 year. You note late inspiratory crackles on auscultation. Pulmonary function tests reveal an FEV1/FVC ratio of 90% and an FVC that is 50% of the predicted value. Which of the following would you most likely see on a biopsy of this patient's lung?
- A. Arteriovenous malformations
- B. Hyaline membranes
- C. Charcot-Leyden crystals
- D. Subpleural cystic enlargement (Correct Answer)
- E. Linear immunofluorescence along alveolar basement membranes
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Subpleural cystic enlargement***
- The patient's presentation with **dyspnea, non-productive cough, late inspiratory crackles**, and **restrictive lung disease** (normal FEV1/FVC ratio of 90% with reduced FVC of 50%) is highly suggestive of **pulmonary fibrosis**.
- **Subpleural cystic enlargement** (honeycombing) is the characteristic histological finding in advanced pulmonary fibrosis, particularly in the **usual interstitial pneumonia (UIP)** pattern seen in **idiopathic pulmonary fibrosis (IPF)**.
- The chronic, progressive nature (1-year history) and the restrictive PFT pattern make this the most likely biopsy finding.
*Arteriovenous malformations*
- These are abnormal vascular connections between arteries and veins that can cause **hypoxemia** and are typically associated with **hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)**.
- They do not explain the restrictive PFT pattern or the typical presentation of chronic progressive fibrosis with late inspiratory crackles.
*Linear immunofluorescence along alveolar basement membranes*
- This finding on **direct immunofluorescence** with **IgG deposition** is characteristic of **Goodpasture syndrome** (anti-GBM disease), which causes pulmonary hemorrhage and rapidly progressive glomerulonephritis.
- This condition presents with **hemoptysis** and **acute renal failure**, not chronic non-productive cough, and would show an obstructive or mixed pattern if hemorrhage were present.
*Hyaline membranes*
- **Hyaline membranes** are proteinaceous material lining alveoli seen in **acute respiratory distress syndrome (ARDS)** or **diffuse alveolar damage (DAD)**.
- The patient's **chronic 1-year symptoms** and restrictive PFTs indicate chronic interstitial lung disease, not acute lung injury.
*Charcot-Leyden crystals*
- **Charcot-Leyden crystals** are formed from breakdown of **eosinophils** and are found in conditions with eosinophilic inflammation, such as **asthma** or **eosinophilic pneumonia**.
- While these conditions can cause cough and dyspnea, they would typically show an **obstructive pattern** (reduced FEV1/FVC) in asthma, not the restrictive pattern seen here.
Obstructive lung diseases (emphysema, bronchitis) US Medical PG Question 10: A 31-year-old man presents to his primary care physician with shortness of breath. He states that he had a “cold” 2 weeks ago and since then has had a persistent cough and worsening shortness of breath. He denies fever, chills, chest pain, sore throat, or rhinorrhea. His medical history is significant for seasonal allergies. He uses fluticasone nasal spray. He had his tonsils removed when he was 8 years of age. His mother and maternal grandfather have cirrhosis, and his father has depression and hypertension. The patient endorses that he smokes tobacco socially on the weekends and uses marijuana daily. He drinks 1-2 beers after work with his co-workers most evenings. A chest radiograph shows hyperinflation of the lungs and hyperlucency. Routine labs are drawn, as shown below.
Serum:
Na+: 139 mEq/L
Cl-: 105 mEq/L
K+: 4.0 mEq/L
HCO3-: 26 mEq/L
Urea nitrogen: 15 mg/dL
Glucose: 100 mg/dL
Creatinine: 0.8 mg/dL
Alkaline phosphatase: 98 U/L
Aspartate aminotransferase (AST, GOT): 46 U/L
Alanine aminotransferase (ALT, GPT): 49 U/L
Pulmonary function tests are pending. Which of the following is most likely to confirm the patient’s diagnosis?
- A. Enzyme-linked immunosorbent assay (Correct Answer)
- B. Bronchoalveolar lavage
- C. Abdominal ultrasound
- D. Viral hepatitis serologies
- E. Pulmonary function tests
Obstructive lung diseases (emphysema, bronchitis) Explanation: ***Enzyme-linked immunosorbent assay (ELISA)***
- This patient's presentation with **early-onset emphysema at age 31**, **hyperinflation and hyperlucency** on chest X-ray, and **strong family history of cirrhosis** (mother and maternal grandfather) strongly suggests **alpha-1 antitrypsin deficiency**.
- **ELISA is used to measure serum alpha-1 antitrypsin levels**, which is the key confirmatory test for this diagnosis. Low levels (<50-80 mg/dL) confirm the deficiency.
- Alpha-1 antitrypsin deficiency causes **panacinar emphysema** (especially in lower lobes) and can also cause **liver cirrhosis**, explaining the family history and mildly elevated transaminases.
- Once low levels are detected, **phenotyping or genotyping** can further characterize the specific mutation (most commonly PiZZ).
*Pulmonary function tests*
- PFTs would demonstrate **obstructive lung disease** with reduced FEV1/FVC ratio and confirm the presence of airflow limitation.
- However, PFTs are **non-specific** and would not distinguish alpha-1 antitrypsin deficiency from other causes of COPD/emphysema (smoking-related, chronic bronchitis, etc.).
- While diagnostically useful for characterizing severity, PFTs do not confirm the underlying etiology.
*Bronchoalveolar lavage*
- **Bronchoalveolar lavage (BAL)** is useful for diagnosing **infections**, **interstitial lung diseases**, **malignancies**, or **alveolar hemorrhage**.
- It is not indicated for confirming emphysema or alpha-1 antitrypsin deficiency, as these are diagnosed through clinical presentation, imaging, and serologic testing.
*Abdominal ultrasound*
- An **abdominal ultrasound** could evaluate for **liver disease** (cirrhosis, hepatomegaly) associated with alpha-1 antitrypsin deficiency.
- While it might reveal liver involvement, it does not confirm the pulmonary diagnosis or the underlying enzymatic deficiency itself.
- It would be considered as part of a comprehensive evaluation but is not the confirmatory test.
*Viral hepatitis serologies*
- These would test for **hepatitis A, B, C** infection, which are common causes of cirrhosis and elevated transaminases.
- However, the patient's respiratory symptoms, imaging findings of emphysema, young age, and family history point toward alpha-1 antitrypsin deficiency rather than viral hepatitis.
- While worth checking given the liver enzyme elevation, this would not confirm the primary diagnosis.
More Obstructive lung diseases (emphysema, bronchitis) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.