Congenital lung anomalies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital lung anomalies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital lung anomalies US Medical PG Question 1: A 3-year-old girl is brought to the emergency department by her parents with sudden onset shortness of breath. They tell the emergency physician that their daughter was lying on the bed watching television when she suddenly began gasping for air. They observed a bowl of peanuts lying next to her when they grabbed her up and brought her to the emergency department. Her respirations are 25/min, the pulse is 100/min and the blood pressure is 90/65 mm Hg. The physical findings as of now are apparently normal. She is started on oxygen and is sent in for a chest X-ray. Based on her history and physical exam findings, the cause of her current symptoms would be seen on the X-ray at which of the following sites?
- A. The superior segment of the right lower lobe
- B. The posterior segment of the right lower lobe (Correct Answer)
- C. The lingula of the left upper lobe
- D. The apical segment of the right upper lobe
- E. The apical segment of the left upper lobe
Congenital lung anomalies Explanation: ***The posterior segment of the right lower lobe***
- This is the **most common site for foreign body aspiration in a supine or lying down position** due to gravity and anatomical orientation.
- The history explicitly states the child was **"lying on the bed watching television"** when aspiration occurred, making the **posterior segment of the right lower lobe** the most gravity-dependent and therefore most likely location.
- The **right main bronchus** is wider, shorter, and more vertical than the left, making the right lung the predominant site for aspiration, and in supine position, the posterior segment is most dependent [1, 2].
*The superior segment of the right lower lobe*
- The **superior segment of the right lower lobe** is the most common site for aspiration in **upright, standing, or semi-upright positions**, not in a supine position.
- Since the child was lying down (supine), gravity would direct the aspirated peanut to the **posterior segment** rather than the superior segment.
- This would be correct if the child had aspirated while sitting upright.
*The lingula of the left upper lobe*
- The **lingula** is an uncommon site for aspiration because the **left main bronchus** has a sharper angle and smaller diameter compared to the right bronchus [2].
- The anatomical differences make aspiration into the right lung significantly more common than the left lung [2].
- The lingula is not a gravity-dependent area in the supine position.
*The apical segment of the right upper lobe*
- The **apical segment of the right upper lobe** is associated with aspiration when the patient is in **Trendelenburg position** (head lower than feet) or in extreme head-down positions.
- The described scenario of lying flat on the bed does not favor aspiration into apical segments, which are non-gravity-dependent in supine position.
- This location would be contra-gravity in the supine position.
*The apical segment of the left upper lobe*
- Aspiration into the **left upper lobe** is less frequent than the right lung due to the sharper angle of the left main bronchus [2].
- The **apical segment** would require head-down positioning (Trendelenburg) that is not described in this clinical scenario.
- This is the least likely location given both the supine position and left-sided anatomy.
Congenital lung anomalies US Medical PG Question 2: A 3-year-old boy is brought to a respiratory specialist. The family physician referred the child because of recurrent respiratory infections over the past 2 years. Chest X-rays showed a lesion of < 2 cm that includes glands and cysts in the upper lobe of the right lung. Diseases affecting the immune system were investigated and ruled out. No family history of any pulmonary disease or congenital malformations exists. He was born at full term via a normal vaginal delivery with an APGAR score of 10. Which of the following should be highly considered for effective management of this child’s condition?
- A. Lobectomy
- B. Antibiotics
- C. Observation
- D. Bronchoscopy (Correct Answer)
- E. Pneumonectomy
Congenital lung anomalies Explanation: ***Bronchoscopy***
- A **bronchoscopy** would be highly considered to **visualize** the lesion, obtain a **biopsy**, and potentially **remove** any obstructing foreign bodies or mucous plugs contributing to recurrent infections.
- Given the description of a lesion < 2 cm with glands and cysts, it is crucial to further characterize it to guide definitive treatment and rule out possibilities like a **bronchial anomaly** or a **benign tumor**.
*Lobectomy*
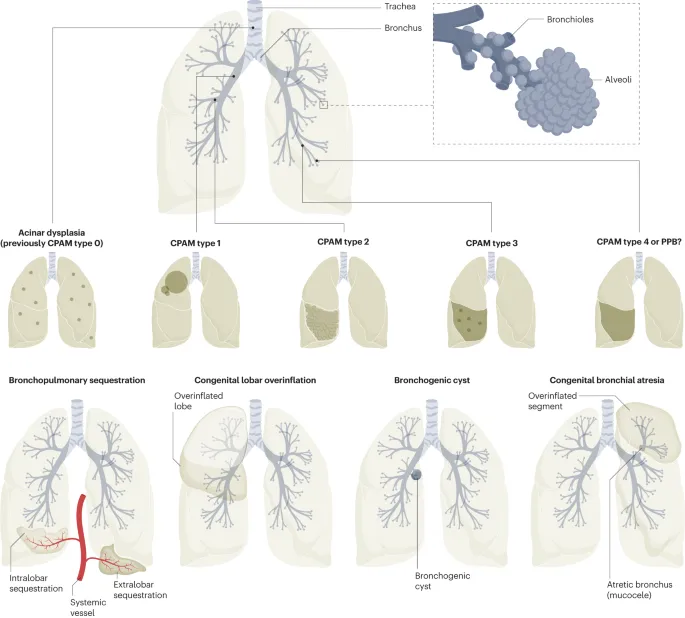
- **Lobectomy** is a surgical procedure to remove an entire lung lobe; it might be considered if the lesion is definitively diagnosed as a **congenital pulmonary airway malformation (CPAM)** or other localized, symptomatic anomaly, but not as the initial management step without a clear diagnosis.
- Doing a lobectomy without proper diagnosis might be too invasive and aggressive when other less invasive management options are available.
*Antibiotics*
- **Antibiotics** are appropriate for treating the recurrent respiratory infections themselves but will not address the underlying structural lesion causing them.
- While they might provide temporary relief from infections, they do not offer a long-term solution for the **structural abnormality** described.
*Observation*
- **Observation** might be considered for small, asymptomatic lesions, but this child has **recurrent respiratory infections**, suggesting the lesion is clinically significant and warrants intervention.
- Delaying diagnosis and treatment could lead to persistent morbidity and potentially irreversible lung damage.
*Pneumonectomy*
- **Pneumonectomy**, the removal of an entire lung, is a major and highly aggressive surgery reserved for extensive, **life-threatening conditions** such as large malignancies or widespread irreversible lung disease.
- Given the lesion is < 2 cm and localized to one lobe, a pneumonectomy is an **overly extreme measure** and not indicated at this stage.
Congenital lung anomalies US Medical PG Question 3: Five weeks after delivery, a 1350-g (3-lb 0-oz) male newborn has respiratory distress. He was born at 26 weeks' gestation. He required intubation and mechanical ventilation for a month following delivery and has been on noninvasive pressure ventilation for 5 days. His temperature is 36.8°C (98.2°F), pulse is 148/min, respirations are 63/min, and blood pressure is 60/32 mm Hg. Pulse oximetry on 40% oxygen shows an oxygen saturation of 91%. Examination shows moderate intercostal and subcostal retractions. Scattered crackles are heard in the thorax. An x-ray of the chest shows diffuse granular densities and basal atelectasis. Which of the following is the most likely diagnosis?
- A. Bronchopulmonary dysplasia (Correct Answer)
- B. Tracheomalacia
- C. Bronchiolitis obliterans
- D. Interstitial emphysema
- E. Pneumonia
Congenital lung anomalies Explanation: ***Bronchopulmonary dysplasia***
- The presentation of a premature infant (26 weeks' gestation) with persistent respiratory distress requiring prolonged mechanical ventilation and oxygen, along with characteristic chest X-ray findings (diffuse granular densities and basal atelectasis), is highly indicative of **bronchopulmonary dysplasia (BPD)**.
- BPD is a chronic lung disease of prematurity defined by the need for supplemental oxygen and/or positive pressure ventilation for at least 28 days after birth, with severity classified at 36 weeks postmenstrual age (or discharge if earlier).
- The pathophysiology involves ventilator-induced injury, oxygen toxicity, and inflammation in the developing lung, leading to impaired alveolarization and abnormal vascular development.
*Tracheomalacia*
- While **tracheomalacia** can cause respiratory symptoms, it typically presents with expiratory stridor, a characteristic "barking" cough, or wheezing that may improve with neck extension or prone positioning.
- It is a structural abnormality of the trachea involving weakness of the tracheal wall, and would not typically manifest with diffuse granular densities or basal atelectasis on chest X-ray in this context.
*Bronchiolitis obliterans*
- **Bronchiolitis obliterans** is irreversible obstruction of the small airways, often occurring after severe viral infections (especially adenovirus or RSV), lung transplantation, or toxic inhalational injury.
- While it can occur in neonates post-ventilation, it is less common in this specific context and would typically present with more severe obstructive findings, hyperinflation, and air trapping on imaging rather than chronic diffuse granular densities and atelectasis.
*Interstitial emphysema*
- **Pulmonary interstitial emphysema** usually occurs acutely in the first days to weeks of mechanical ventilation, characterized by air dissecting into the lung interstitium and perivascular spaces.
- While it can be a complication that contributes to the development of BPD, the persistent nature of respiratory distress five weeks post-delivery, along with diffuse granular densities and chronic radiographic changes, points toward the established chronic lung disease of BPD rather than acute interstitial emphysema.
*Pneumonia*
- Neonatal **pneumonia** would typically present with acute onset or worsening of respiratory distress, temperature instability, and signs of systemic infection.
- While a chest X-ray might show infiltrates or consolidations, the chronic progressive course over 5 weeks, history of extreme prematurity, and prolonged ventilation make BPD a more fitting diagnosis than acute pneumonia in this clinical scenario.
Congenital lung anomalies US Medical PG Question 4: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Congenital lung anomalies Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Congenital lung anomalies US Medical PG Question 5: A mother brings her 6-month-old boy to the emergency department. She reports that her son has been breathing faster than usual for the past 2 days, and she has noted occasional wheezing. She states that prior to the difficulty breathing, she noticed some clear nasal discharge for several days. The infant was born full-term, with no complications, and no significant medical history. His temperature is 100°F (37.8°C), blood pressure is 60/30 mmHg, pulse is 120/min, respirations are 40/min, and oxygen saturation is 95% on room air. Physical exam reveals expiratory wheezing, crackles diffusely, and intercostal retractions. The child is currently playing with toys. Which of the following is the most appropriate next step in management?
- A. Monitoring (Correct Answer)
- B. Intubation
- C. Albuterol
- D. Chest radiograph
- E. Azithromycin and ceftriaxone
Congenital lung anomalies Explanation: ***Monitoring (Supportive Care)***
- This infant presents with classic **viral bronchiolitis** (tachypnea, wheezing, crackles, retractions following upper respiratory symptoms)
- The child is **clinically stable**: O2 saturation 95% on room air, alert and playing with toys
- **Current AAP guidelines** recommend **supportive care only** for bronchiolitis, which includes monitoring vital signs, assessing work of breathing, ensuring adequate hydration, and oxygen supplementation if saturation drops below 90%
- This patient requires close observation but no immediate intervention given stable vital signs and reassuring clinical appearance
*Albuterol*
- **Bronchodilators are NOT recommended** for routine use in bronchiolitis per current AAP clinical practice guidelines
- Multiple randomized controlled trials have shown **no significant benefit** from albuterol in bronchiolitis
- While a trial may be considered in select cases with strong family history of asthma, routine use is discouraged
- Bronchiolitis is caused by **small airway inflammation and mucus plugging**, not bronchospasm
*Intubation*
- **Intubation** is reserved for severe respiratory failure with impending respiratory arrest, persistent hypoxemia despite high-flow oxygen, apnea, or altered mental status
- This child has adequate oxygenation (95%), is alert, and playing—**no indication for intubation**
- Signs that would warrant intubation include lethargy, severe retractions with fatigue, O2 sat <90% despite supplementation
*Chest radiograph*
- **Not routinely indicated** in typical bronchiolitis
- Consider only if there's diagnostic uncertainty, concern for complications (pneumothorax, lobar consolidation suggesting bacterial pneumonia), or failure to improve with supportive care
- The clinical presentation is clearly consistent with bronchiolitis, and imaging would not change initial management
*Azithromycin and ceftriaxone*
- Bronchiolitis is a **viral infection** (most commonly RSV), and **antibiotics provide no benefit**
- Antibiotics should only be used if there is clear evidence of **bacterial superinfection** (high fever, focal consolidation, elevated inflammatory markers)
- Routine antibiotic use contributes to antimicrobial resistance and adverse effects
Congenital lung anomalies US Medical PG Question 6: A 3-year-old boy is brought to the emergency department by his mother because of a cough and mild shortness of breath for the past 12 hours. He has not had fever. He has been to the emergency department 4 times during the past 6 months for treatment of asthma exacerbations. His 9-month-old sister was treated for bronchiolitis a week ago. His father has allergic rhinitis. Current medications include an albuterol inhaler and a formoterol-fluticasone inhaler. He appears in mild distress. His temperature is 37.5°C (99.5°F), pulse is 101/min, respirations are 28/min, and blood pressure is 86/60 mm Hg. Examination shows mild intercostal and subcostal retractions. Pulmonary examination shows decreased breath sounds and mild expiratory wheezing throughout the right lung field. Cardiac examination shows no abnormalities. An x-ray of the chest shows hyperlucency of the right lung field with decreased pulmonary markings. Which of the following is the next best step in management?
- A. Azithromycin therapy
- B. Racemic epinephrine
- C. Albuterol nebulization
- D. CT of the lung
- E. Bronchoscopy (Correct Answer)
Congenital lung anomalies Explanation: ***Bronchoscopy***
- The patient's history of recurrent respiratory symptoms, unilateral wheezing and decreased breath sounds, and radiological findings of **unilateral hyperlucency** and **decreased pulmonary markings** strongly suggest a **foreign body aspiration**.
- **Bronchoscopy** is both diagnostic and therapeutic in this situation, allowing for direct visualization and removal of the foreign body.
*Azithromycin therapy*
- This is an **antibiotic** and would be used for bacterial infections, which are not indicated here given the clinical picture of a suspected foreign body.
- Antibiotics are not effective for mechanical obstruction of the airway.
*Racemic epinephrine*
- Racemic epinephrine is used for conditions like **croup** to reduce airway edema.
- It would not address an inhaled **foreign body**, which is a mechanical obstruction.
*Albuterol nebulization*
- While albuterol is used for bronchospasm, the unilateral nature of the findings and the history of recurrent issues point away from simple asthma exacerbation.
- Albuterol would likely not relieve the obstruction caused by a **foreign body**.
*CT of the lung*
- While CT could help identify a foreign body, it exposes the child to **radiation** and is not the definitive treatment.
- Bronchoscopy offers both diagnosis and immediate treatment, making it superior to CT as the *next best step*.
Congenital lung anomalies US Medical PG Question 7: A 31 year-old African-American female presents with painful shin nodules, uveitis, and calcified hilar lymph nodes. A transbronchial biopsy of the lung would most likely show which of the following histologies?
- A. Golden-brown fusiform rods
- B. Inflammation, fibrosis and cyst formation that is most prominent in subpleural regions
- C. Non-caseating granulomas (Correct Answer)
- D. Silica particles (birefringent) surrounded by collagen
- E. Patchy interstitial lymphoid infiltrate into walls of alveolar units
Congenital lung anomalies Explanation: ***Non-caseating granulomas***
- The constellation of **erythema nodosum** (painful shin nodules), **uveitis**, and **hilar lymphadenopathy** in an African-American female is highly characteristic of **sarcoidosis**.
- **Sarcoidosis** is pathologically defined by the presence of **non-caseating granulomas** in affected tissues, which would be visible on a transbronchial biopsy.
*Golden-brown fusiform rods*
- These are **ferruginous bodies**, characteristic of **asbestosis**, which is not supported by the patient's presentation.
- Asbestosis would typically involve a history of **asbestos exposure** and present with **pleural plaques** or **interstitial fibrosis**.
*Inflammation, fibrosis and cyst formation that is most prominent in subpleural regions*
- This description is more indicative of **pulmonary Langerhans cell histiocytosis**, a rare disease usually associated with **smoking**.
- It does not align with the patient's specific systemic manifestations like uveitis or erythema nodosum.
*Silica particles (birefringent) surrounded by collagen*
- This describes the histological findings of **silicosis**, an occupational lung disease resulting from exposure to **silica dust**.
- Silicosis is not typically associated with uveitis or erythema nodosum.
*Patchy interstitial lymphoid infiltrate into walls of alveolar units*
- This pattern can be seen in various interstitial lung diseases, but it is not specific for sarcoidosis.
- It could be found in conditions like **lymphoid interstitial pneumonia**, which does not fit the overall clinical picture.
Congenital lung anomalies US Medical PG Question 8: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Congenital lung anomalies Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Congenital lung anomalies US Medical PG Question 9: A 31-year-old man presents to his primary care physician with shortness of breath. He states that he had a “cold” 2 weeks ago and since then has had a persistent cough and worsening shortness of breath. He denies fever, chills, chest pain, sore throat, or rhinorrhea. His medical history is significant for seasonal allergies. He uses fluticasone nasal spray. He had his tonsils removed when he was 8 years of age. His mother and maternal grandfather have cirrhosis, and his father has depression and hypertension. The patient endorses that he smokes tobacco socially on the weekends and uses marijuana daily. He drinks 1-2 beers after work with his co-workers most evenings. A chest radiograph shows hyperinflation of the lungs and hyperlucency. Routine labs are drawn, as shown below.
Serum:
Na+: 139 mEq/L
Cl-: 105 mEq/L
K+: 4.0 mEq/L
HCO3-: 26 mEq/L
Urea nitrogen: 15 mg/dL
Glucose: 100 mg/dL
Creatinine: 0.8 mg/dL
Alkaline phosphatase: 98 U/L
Aspartate aminotransferase (AST, GOT): 46 U/L
Alanine aminotransferase (ALT, GPT): 49 U/L
Pulmonary function tests are pending. Which of the following is most likely to confirm the patient’s diagnosis?
- A. Enzyme-linked immunosorbent assay (Correct Answer)
- B. Bronchoalveolar lavage
- C. Abdominal ultrasound
- D. Viral hepatitis serologies
- E. Pulmonary function tests
Congenital lung anomalies Explanation: ***Enzyme-linked immunosorbent assay (ELISA)***
- This patient's presentation with **early-onset emphysema at age 31**, **hyperinflation and hyperlucency** on chest X-ray, and **strong family history of cirrhosis** (mother and maternal grandfather) strongly suggests **alpha-1 antitrypsin deficiency**.
- **ELISA is used to measure serum alpha-1 antitrypsin levels**, which is the key confirmatory test for this diagnosis. Low levels (<50-80 mg/dL) confirm the deficiency.
- Alpha-1 antitrypsin deficiency causes **panacinar emphysema** (especially in lower lobes) and can also cause **liver cirrhosis**, explaining the family history and mildly elevated transaminases.
- Once low levels are detected, **phenotyping or genotyping** can further characterize the specific mutation (most commonly PiZZ).
*Pulmonary function tests*
- PFTs would demonstrate **obstructive lung disease** with reduced FEV1/FVC ratio and confirm the presence of airflow limitation.
- However, PFTs are **non-specific** and would not distinguish alpha-1 antitrypsin deficiency from other causes of COPD/emphysema (smoking-related, chronic bronchitis, etc.).
- While diagnostically useful for characterizing severity, PFTs do not confirm the underlying etiology.
*Bronchoalveolar lavage*
- **Bronchoalveolar lavage (BAL)** is useful for diagnosing **infections**, **interstitial lung diseases**, **malignancies**, or **alveolar hemorrhage**.
- It is not indicated for confirming emphysema or alpha-1 antitrypsin deficiency, as these are diagnosed through clinical presentation, imaging, and serologic testing.
*Abdominal ultrasound*
- An **abdominal ultrasound** could evaluate for **liver disease** (cirrhosis, hepatomegaly) associated with alpha-1 antitrypsin deficiency.
- While it might reveal liver involvement, it does not confirm the pulmonary diagnosis or the underlying enzymatic deficiency itself.
- It would be considered as part of a comprehensive evaluation but is not the confirmatory test.
*Viral hepatitis serologies*
- These would test for **hepatitis A, B, C** infection, which are common causes of cirrhosis and elevated transaminases.
- However, the patient's respiratory symptoms, imaging findings of emphysema, young age, and family history point toward alpha-1 antitrypsin deficiency rather than viral hepatitis.
- While worth checking given the liver enzyme elevation, this would not confirm the primary diagnosis.
More Congenital lung anomalies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.