Atelectasis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Atelectasis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Atelectasis US Medical PG Question 1: A 70-year-old man presents to the clinic with right-sided chest pain and difficulty breathing for the past 10 days. When it began, the pain was mild, but as time went on, it increased to a level at which the man found it difficult to breathe. Two years ago, he was diagnosed with clear cell carcinoma of the kidney. Vital signs include: pulse rate is 72/min, blood pressure is 122/80 mm Hg, respiratory rate is 16/min, and temperature is 37.0°C (98.6°F). On physical examination, the trachea appears to have deviated to the left, respiratory movements are diminished, there is decreased resonance on percussion, and there is an absence of breath sounds over the right hemithorax. Which of the following is the most likely clinical diagnosis in this patient?
- A. Atelectasis
- B. Pneumothorax
- C. Pleural effusion (Correct Answer)
- D. Pulmonary embolism
- E. Pneumonia
Atelectasis Explanation: **Pleural effusion**
- The presence of **chest pain**, **dyspnea**, **tracheal deviation away from the affected side**, diminished respiratory movements, **decreased resonance on percussion**, and absence of breath sounds are classic signs of a large **pleural effusion**.
- The patient's history of **clear cell carcinoma** of the kidney suggests a metastatic cause, like **malignant pleural effusion**, contributing to the progressive symptoms.
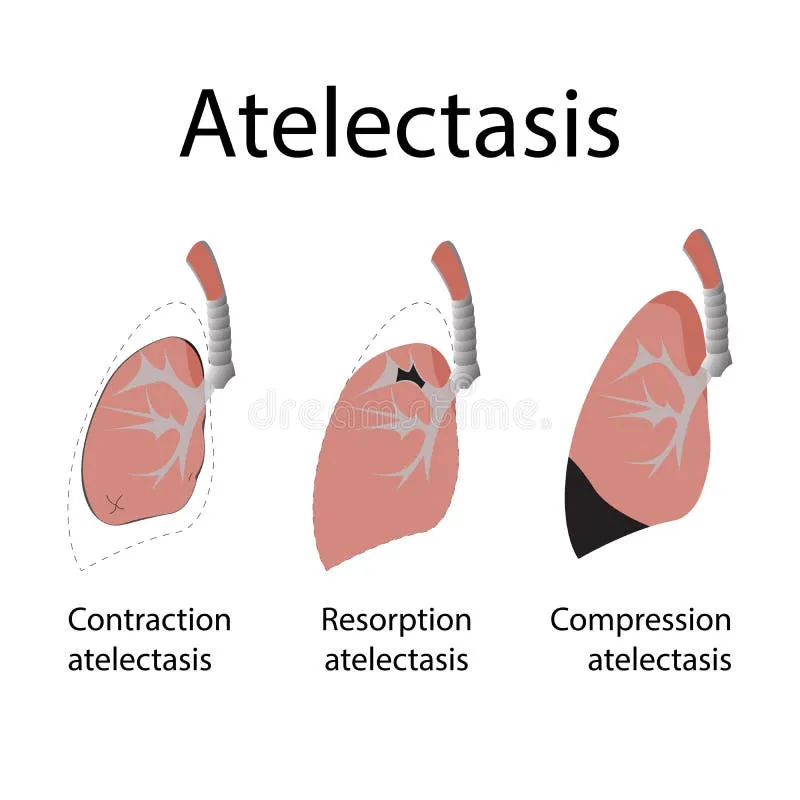
*Atelectasis*
- While atelectasis presents with **dyspnea** and **decreased breath sounds**, the trachea typically deviates **towards the affected side** due to volume loss, which contradicts the presented leftward deviation.
- Percussion in atelectasis would typically yield **dullness**, but not necessarily decreased resonance with the degree of tracheal shift seen in a large effusion.
*Pneumothorax*
- A pneumothorax would present with **hyperresonance on percussion** due to air accumulation, not decreased resonance.
- Tracheal deviation in a tension pneumothorax would be **away from the affected side**, but the characteristic percussion finding differentiates it from pleural effusion.
*Pulmonary embolism*
- Pulmonary embolism primarily causes **acute dyspnea** and **pleuritic chest pain**, but typically does not produce the pronounced physical exam findings of tracheal deviation, decreased resonance, and absent breath sounds associated with a large space-occupying lesion in the pleural space.
- While it can cause a small pleural effusion, the extensive findings point against PE as the primary diagnosis.
*Pneumonia*
- Pneumonia presents with **fever**, **cough**, and usually **bronchial breath sounds** or **crackles** over the affected area, with **dullness to percussion**.
- It does not typically cause significant tracheal deviation, nor the complete absence of breath sounds over an entire hemithorax.
Atelectasis US Medical PG Question 2: A 60-year-old man presents to the emergency department complaining of worsening exertional dyspnea over the last week. He denies chest pain and lightheadedness but reports persistent cough with white sputum. His past medical history includes hypertension and diabetes mellitus. He has a 50 pack-year history of smoking but denies any illicit drug use or alcohol consumption. His temperature is 101°F (38.3°C), blood pressure is 154/104 mmHg, pulse is 110/min, respirations are 26/min, and oxygen saturation is 88% on a non-rebreather mask. Physical exam is notable for an obese man in distress. The anteroposterior diameter of the patient's chest is increased, and he has decreased breath sounds bilaterally with diffuse expiratory wheezing. Which of the following is the best next step in management?
- A. Muscarinic blocker
- B. Glucocorticoid-analog
- C. Alpha-2 blocker
- D. Beta-2 agonist (Correct Answer)
- E. Alpha-1 blocker
Atelectasis Explanation: ***Beta-2 agonist***
- The patient presents with **acute exacerbation of COPD**, evidenced by his significant smoking history (50 pack-years), barrel chest (increased AP diameter), decreased breath sounds, and diffuse expiratory wheezing.
- **Short-acting beta-2 agonists (SABAs)** like **albuterol** are **first-line bronchodilators** in acute COPD exacerbations, providing rapid relief of bronchospasm by relaxing airway smooth muscle.
- According to **GOLD guidelines**, SABAs are the primary initial bronchodilator, often combined with short-acting muscarinic antagonists (SAMAs) like ipratropium for optimal effect.
- This patient requires **immediate bronchodilation** to address severe dyspnea and hypoxemia (88% on non-rebreather).
*Muscarinic blocker*
- **Short-acting muscarinic antagonists (SAMAs)** like **ipratropium bromide** are important adjunctive bronchodilators in acute COPD exacerbations.
- While SAMAs are effective and typically used **in combination with SABAs**, they are generally considered **adjunctive rather than first-line monotherapy**.
- In clinical practice, both SABAs and SAMAs are often administered together, but when asked for the "best next step," **beta-2 agonist is the more standard initial choice**.
*Glucocorticoid-analog*
- Systemic **glucocorticoids** like **prednisone** are indeed crucial in managing acute COPD exacerbations to reduce airway inflammation and shorten recovery time.
- However, they do **not provide immediate bronchodilation**, which is the most urgent need for this patient with severe respiratory distress and hypoxemia.
- Glucocorticoids are typically administered **after or concurrent with bronchodilators**, not as the initial intervention.
*Alpha-2 blocker*
- **Alpha-2 blockers have no role** in the management of acute respiratory distress or COPD exacerbations.
- These agents are used for conditions like **hypertension** or psychiatric disorders (note: clonidine is actually an alpha-2 **agonist**, not blocker).
- They do not affect airway caliber and are completely unrelated to bronchodilation.
*Alpha-1 blocker*
- **Alpha-1 blockers** like prazosin or doxazosin are used for **hypertension or benign prostatic hyperplasia (BPH)**.
- They have **no role in acute respiratory management** or COPD exacerbations.
- These agents cause peripheral vasodilation and do not affect airway smooth muscle or bronchospasm.
Atelectasis US Medical PG Question 3: Five weeks after delivery, a 1350-g (3-lb 0-oz) male newborn has respiratory distress. He was born at 26 weeks' gestation. He required intubation and mechanical ventilation for a month following delivery and has been on noninvasive pressure ventilation for 5 days. His temperature is 36.8°C (98.2°F), pulse is 148/min, respirations are 63/min, and blood pressure is 60/32 mm Hg. Pulse oximetry on 40% oxygen shows an oxygen saturation of 91%. Examination shows moderate intercostal and subcostal retractions. Scattered crackles are heard in the thorax. An x-ray of the chest shows diffuse granular densities and basal atelectasis. Which of the following is the most likely diagnosis?
- A. Bronchopulmonary dysplasia (Correct Answer)
- B. Tracheomalacia
- C. Bronchiolitis obliterans
- D. Interstitial emphysema
- E. Pneumonia
Atelectasis Explanation: ***Bronchopulmonary dysplasia***
- The presentation of a premature infant (26 weeks' gestation) with persistent respiratory distress requiring prolonged mechanical ventilation and oxygen, along with characteristic chest X-ray findings (diffuse granular densities and basal atelectasis), is highly indicative of **bronchopulmonary dysplasia (BPD)**.
- BPD is a chronic lung disease of prematurity defined by the need for supplemental oxygen and/or positive pressure ventilation for at least 28 days after birth, with severity classified at 36 weeks postmenstrual age (or discharge if earlier).
- The pathophysiology involves ventilator-induced injury, oxygen toxicity, and inflammation in the developing lung, leading to impaired alveolarization and abnormal vascular development.
*Tracheomalacia*
- While **tracheomalacia** can cause respiratory symptoms, it typically presents with expiratory stridor, a characteristic "barking" cough, or wheezing that may improve with neck extension or prone positioning.
- It is a structural abnormality of the trachea involving weakness of the tracheal wall, and would not typically manifest with diffuse granular densities or basal atelectasis on chest X-ray in this context.
*Bronchiolitis obliterans*
- **Bronchiolitis obliterans** is irreversible obstruction of the small airways, often occurring after severe viral infections (especially adenovirus or RSV), lung transplantation, or toxic inhalational injury.
- While it can occur in neonates post-ventilation, it is less common in this specific context and would typically present with more severe obstructive findings, hyperinflation, and air trapping on imaging rather than chronic diffuse granular densities and atelectasis.
*Interstitial emphysema*
- **Pulmonary interstitial emphysema** usually occurs acutely in the first days to weeks of mechanical ventilation, characterized by air dissecting into the lung interstitium and perivascular spaces.
- While it can be a complication that contributes to the development of BPD, the persistent nature of respiratory distress five weeks post-delivery, along with diffuse granular densities and chronic radiographic changes, points toward the established chronic lung disease of BPD rather than acute interstitial emphysema.
*Pneumonia*
- Neonatal **pneumonia** would typically present with acute onset or worsening of respiratory distress, temperature instability, and signs of systemic infection.
- While a chest X-ray might show infiltrates or consolidations, the chronic progressive course over 5 weeks, history of extreme prematurity, and prolonged ventilation make BPD a more fitting diagnosis than acute pneumonia in this clinical scenario.
Atelectasis US Medical PG Question 4: A 57-year-old man presents to the clinic for a chronic cough over the past 4 months. The patient reports a productive yellow/green cough that is worse at night. He denies any significant precipitating event prior to his symptoms. He denies fever, chest pain, palpitations, weight changes, or abdominal pain, but endorses some difficulty breathing that waxes and wanes. He denies alcohol usage but endorses a 35 pack-year smoking history. A physical examination demonstrates mild wheezes, bibasilar crackles, and mild clubbing of his fingertips. A pulmonary function test is subsequently ordered, and partial results are shown below:
Tidal volume: 500 mL
Residual volume: 1700 mL
Expiratory reserve volume: 1500 mL
Inspiratory reserve volume: 3000 mL
What is the functional residual capacity of this patient?
- A. 4500 mL
- B. 2000 mL
- C. 2200 mL
- D. 3200 mL (Correct Answer)
- E. 3500 mL
Atelectasis Explanation: ***3200 mL***
- The **functional residual capacity (FRC)** is the volume of air remaining in the lungs after a normal expiration.
- It is calculated as the sum of the **expiratory reserve volume (ERV)** and the **residual volume (RV)**. In this case, 1500 mL (ERV) + 1700 mL (RV) = 3200 mL.
*4500 mL*
- This value represents the sum of the **inspiratory reserve volume (3000 mL)** and the **residual volume (1700 mL)**, which does not correspond to a standard lung volume or capacity.
- It does not logically relate to the definition of functional residual capacity.
*2000 mL*
- This value represents the sum of the **tidal volume (500 mL)** and the **expiratory reserve volume (1500 mL)**, which is incorrect for FRC.
- This would represent the inspiratory capacity minus the inspiratory reserve volume, which is not a standard measurement used in pulmonary function testing.
*2200 mL*
- This value could be obtained by incorrectly adding the **tidal volume (500 mL)** and the **residual volume (1700 mL)**, which is not the correct formula for FRC.
- This calculation represents a miscombination of lung volumes that does not correspond to any standard pulmonary capacity measurement.
*3500 mL*
- This value is the sum of the **tidal volume (500 mL)**, the **expiratory reserve volume (1500 mL)**, and the **residual volume (1700 mL)**.
- This would represent the FRC plus the tidal volume, which is not a standard measurement and does not represent the functional residual capacity.
Atelectasis US Medical PG Question 5: A previously healthy 66-year-old woman comes to the physician because of a 3-day history of fever, cough, and right-sided chest pain. Her temperature is 38.8°C (101.8°F) and respirations are 24/min. Physical examination shows dullness to percussion, increased tactile fremitus, and egophony in the right lower lung field. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of these findings?
- A. Fluid in the interstitial space
- B. Air in the pleural space
- C. Consolidation of a lung segment (Correct Answer)
- D. Fluid in the pleural space
- E. Collapse of a lung segment
Atelectasis Explanation: ***Consolidation of a lung segment***
- The combination of **fever**, **cough**, and **chest pain** along with physical exam findings of **dullness to percussion**, **increased tactile fremitus**, and **egophony** in a specific lung field is classic for **lobar pneumonia**, which involves consolidation.
- **Consolidation** occurs when the normally air-filled alveoli become filled with inflammatory exudate (fluid, cells, and fibrin), leading to increased density of the lung tissue.
*Fluid in the interstitial space*
- **Interstitial fluid** typically causes **crackles** on auscultation and can be associated with conditions like **pulmonary edema**, but it does not usually cause **increased tactile fremitus** or **egophony**.
- **Dullness to percussion** would be less localized and tactile fremitus would not be increased as the sound transmission is not enhanced.
*Air in the pleural space*
- **Air in the pleural space (pneumothorax)** would lead to **hyperresonance** to percussion, **decreased or absent breath sounds**, and **decreased tactile fremitus**, which are opposite to the findings described.
- There would be no egophony, as sound transmission is diminished.
*Fluid in the pleural space*
- **Fluid in the pleural space (pleural effusion)** would cause **dullness to percussion** and **decreased or absent breath sounds** over the effusion.
- It would also typically result in **decreased tactile fremitus** due to the fluid separating the lung from the chest wall, unlike the increased fremitus seen with consolidation.
*Collapse of a lung segment*
- **Collapse of a lung segment (atelectasis)** would result in **dullness to percussion** and **decreased or absent breath sounds**.
- **Tactile fremitus** would be **decreased** over the affected area, not increased, because the collapsed lung tissue does not transmit vibrations as effectively.
Atelectasis US Medical PG Question 6: A 4-year-old girl is brought to the emergency department by her parents with a sudden onset of breathlessness. She has been having similar episodes over the past few months with a progressive increase in frequency over the past week. They have noticed that the difficulty in breathing is more prominent during the day when she plays in the garden with her siblings. She gets better once she comes indoors. During the episodes, she complains of an inability to breathe and her parents say that she is gasping for breath. Sometimes they hear a noisy wheeze while she breathes. The breathlessness does not disrupt her sleep. On examination, she seems to be in distress with noticeable intercostal retractions. Auscultation reveals a slight expiratory wheeze. According to her history and physical findings, which of the following mechanisms is most likely responsible for this child’s difficulty in breathing?
- A. Defective chloride channel function leading to mucus plugging
- B. Chronic mucus plugging and inflammation leading to impaired mucociliary clearance
- C. Airway hyperreactivity to external allergens causing intermittent airway obstruction (Correct Answer)
- D. Inflammation leading to permanent dilation and destruction of alveoli
- E. Destruction of the elastic layers of bronchial walls leading to abnormal dilation
Atelectasis Explanation: **Airway hyperreactivity to external allergens causing intermittent airway obstruction**
- The child's symptoms of **recurrent breathlessness** and **wheezing**, especially while playing in the garden (suggesting **allergen exposure**), and subsequent improvement indoors, are highly indicative of **allergen-induced bronchoconstriction**.
- The history points to **intermittent airway obstruction** triggered by environmental factors, characteristic of conditions like **asthma** where airways are hyperresponsive to triggers.
*Defective chloride channel function leading to mucus plugging*
- This mechanism is characteristic of **cystic fibrosis**, which typically presents with chronic respiratory issues, recurrent infections, and growth failure, not the acute, intermittent, and allergen-triggered episodes described.
- While mucus plugging can occur, it's a chronic process in cystic fibrosis and doesn't align with the acute, reversible nature and specific triggers mentioned in the case.
*Chronic mucus plugging and inflammation leading to impaired mucociliary clearance*
- This describes conditions like **bronchiectasis** or chronic bronchitis, which involve persistent cough, sputum production, and recurrent infections, rather than acute episodic wheezing based on allergen exposure.
- Impaired mucociliary clearance would lead to more continuous respiratory issues, not the relief experienced upon coming indoors.
*Inflammation leading to permanent dilation and destruction of alveoli*
- This mechanism is characteristic of **emphysema**, a condition primarily seen in adults, typically due to smoking, and presenting with chronic shortness of breath and airflow limitation, rather than episodic, allergen-triggered wheezing in a child.
- Emphysema involves alveolar damage, not primarily bronchial obstruction or hyperreactivity.
*Destruction of the elastic layers of bronchial walls leading to abnormal dilation*
- This describes **bronchiectasis**, which is characterized by permanent dilation of the bronchi, leading to chronic cough with sputum production and recurrent respiratory infections.
- The symptoms presented by the child are acute, reversible episodes of breathlessness and wheezing, not indicative of permanent structural damage to the bronchial walls.
Atelectasis US Medical PG Question 7: A previously healthy 46-year-old woman comes to the physician with a one-week history of productive cough and fatigue. Two weeks ago, she had fever, nasal congestion, rhinorrhea, and myalgias that resolved with supportive care. She has not traveled out of the United States. Pulmonary examination shows dullness to percussion and increased fremitus at the right middle lobe. An x-ray of the chest is shown. A sputum sample is most likely to show which of the following findings?
- A. Septate, acute-branching hyphae
- B. Silver-staining, gram-negative bacilli
- C. Encapsulated, gram-negative coccobacilli
- D. Gram-positive, catalase-positive cocci
- E. Gram-positive, alpha-hemolytic diplococci (Correct Answer)
Atelectasis Explanation: ***Gram-positive, alpha-hemolytic diplococci***
- The patient's history of **viral illness** followed by a **productive cough** and signs of **lobar consolidation** (dullness to percussion, increased fremitus, and infiltrates on X-ray) is classic for **secondary bacterial pneumonia**.
- **_Streptococcus pneumoniae_** is the most common cause of community-acquired pneumonia following viral respiratory infections and exhibits these characteristic findings on Gram stain and culture.
- _S. pneumoniae_ appears as **gram-positive diplococci** (lancet-shaped pairs) and shows **alpha-hemolysis** (greenish discoloration) on blood agar.
*Septate, acute-branching hyphae*
- This describes **_Aspergillus_** species, which typically cause invasive fungal infections in **immunocompromised** individuals or allergic bronchopulmonary aspergillosis, not typical post-viral bacterial pneumonia.
- The clinical presentation and patient's immune status do not suggest a fungal infection.
*Silver-staining, gram-negative bacilli*
- This morphology points to organisms like **_Legionella pneumophila_**, which causes *atypical pneumonia* and requires silver stain for visualization.
- **_Legionella_** is typically associated with exposure to contaminated water sources (cooling towers, hot tubs) and would present with more systemic symptoms, which are not described here.
*Encapsulated, gram-negative coccobacilli*
- This description fits **_Haemophilus influenzae_**, which can cause community-acquired pneumonia, particularly in patients with COPD or in children.
- However, **_S. pneumoniae_** is more common in this demographic and clinical presentation, especially as a complication of viral respiratory infection.
*Gram-positive, catalase-positive cocci*
- This describes **_Staphylococcus aureus_**, which can cause severe post-influenza pneumonia, often presenting with necrotizing pneumonia, cavitation, or empyema.
- While _S. aureus_ is an important consideration after influenza, it typically causes more severe disease and is less common than _S. pneumoniae_ in otherwise healthy individuals with uncomplicated post-viral pneumonia.
Atelectasis US Medical PG Question 8: A 34-year-old man comes to the physician for a follow-up examination. He has a 3-month history of a nonproductive cough. He has been treated with diphenhydramine since his last visit 2 weeks ago, but his symptoms have persisted. He does not smoke. He drinks 3 beers on the weekends. He is 177 cm (5 ft 10 in) tall and weighs 100 kg (220.46 lbs); BMI is 35.1 kg/m2. His temperature is 37.1°C (98.8°F), pulse is 78/min, respirations are 14/min, and blood pressure is 130/80 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. Physical examination and an x-ray of the chest show no abnormalities. Which of the following is the most appropriate next step in management?
- A. Azithromycin therapy
- B. Pulmonary function testing
- C. CT scan of the chest
- D. Omeprazole therapy (Correct Answer)
- E. Oral corticosteroid therapy
Atelectasis Explanation: ***Omeprazole therapy***
- The patient's **obesity** (BMI 35.1), **nonproductive cough** lasting 3 months, and persistent symptoms despite antihistamines strongly suggest **gastroesophageal reflux disease (GERD)** as the cause.
- **Proton pump inhibitors (PPIs)** like omeprazole are the first-line treatment for GERD.
*Azithromycin therapy*
- Azithromycin is an **antibiotic** used to treat bacterial infections. There is no evidence of infection (e.g., fever, abnormal chest X-ray, purulent sputum) in this patient.
- Empiric antibiotic use for a nonproductive cough without signs of infection is generally inappropriate and can contribute to **antibiotic resistance**.
*Pulmonary function testing*
- Pulmonary function testing (PFTs) would be appropriate if there were concerns for **asthma**, **COPD**, or other intrinsic lung diseases, which are not suggested by the normal chest X-ray, oxygen saturation, and absence of wheezing or dyspnea.
- The patient's lack of smoking history also makes COPD less likely.
*CT scan of the chest*
- A CT scan of the chest would be indicated for persistent cough if the **chest X-ray were abnormal** or if there were suspicion of a malignancy, interstitial lung disease, or bronchiectasis.
- Given the normal chest X-ray and 3-month duration, a CT scan is not the initial next step, especially when there's a strong alternative diagnosis like GERD.
*Oral corticosteroid therapy*
- Oral corticosteroids are used to treat inflammatory conditions like asthma or COPD exacerbations.
- There is no indication of airflow obstruction, allergic reaction, or significant inflammation based on the clinical presentation and normal chest X-ray, making corticosteroids inappropriate.
Atelectasis US Medical PG Question 9: A 61-year-old man presents with gradually increasing shortness of breath. For the last 2 years, he has had a productive cough on most days. Past medical history is significant for hypertension and a recent admission to the hospital for pneumonia. He uses a triamcinolone inhaler and uses an albuterol inhaler as a rescue inhaler. He also takes lisinopril and a multivitamin daily. He has smoked a pack a day for the last 32 years and has no intention to quit now. Today, his blood pressure is 142/97 mm Hg, heart rate is 97/min, respiratory rate is 22/min, and temperature is 37.4°C (99.3°F). On physical exam, he has tachypnea and has some difficulty finishing his sentences. His heart has a regular rate and rhythm. Auscultation of his lungs reveals wheezing and rhonchi that improves after a deep cough. Fremitus is absent. Pulmonary function tests show FEV1/FVC of 55% with no change in FEV1 after albuterol treatment. Which of the following is the most likely pathology associated with this patient's disease?
- A. Airway hypersensitivity
- B. Chronic granulomatous inflammation with bilateral hilar lymphadenopathy
- C. Consolidation and red hepatization
- D. Inflamed bronchus with hypertrophy and hyperplasia of mucous glands (Correct Answer)
- E. Permanent bronchial dilation
Atelectasis Explanation: ***Inflamed bronchus with hypertrophy and hyperplasia of mucous glands***
- The patient's history of a **productive cough for 2 years**, a **32-pack-year smoking history**, and **irreversible obstructive lung disease** (FEV1/FVC of 55% with no change after albuterol) are classic signs of **chronic bronchitis**.
- The defining pathological feature of chronic bronchitis involves **inflammation of the large airways**, leading to **mucous gland hypertrophy** and **hyperplasia**, resulting in excessive mucus production and airway obstruction.
*Airway hypersensitivity*
- **Airway hypersensitivity** is characteristic of **asthma**, where triggers cause sudden bronchoconstriction, which is typically **reversible** with bronchodilators.
- The patient's FEV1/FVC ratio **did not improve with albuterol**, indicating an irreversible obstruction not typical of hypersensitivity alone.
*Chronic granulomatous inflammation with bilateral hilar lymphadenopathy*
- This description is characteristic of **sarcoidosis**, a systemic inflammatory disease.
- While sarcoidosis can cause respiratory symptoms, it does not fit the typical presentation of **chronic productive cough** in a heavy smoker, and the classic PFT findings for sarcoidosis are **restrictive**, not obstructive.
*Consolidation and red hepatization*
- **Consolidation** and **red hepatization** are pathological features seen in the acute phase of **lobar pneumonia**, reflecting alveolar inflammation and exudation.
- The patient had a recent admission for pneumonia, but his current chronic symptoms and PFT results point to an underlying **obstructive lung disease (chronic bronchitis)**, not acute pneumonia.
*Permanent bronchial dilation*
- **Permanent bronchial dilation** is known as **bronchiectasis**, which results from chronic inflammation and infection leading to destruction of the bronchial walls.
- While chronic bronchitis can sometimes lead to bronchiectasis, the primary and most direct pathological finding for the symptoms described (chronic productive cough in a smoker with irreversible obstruction) is the **inflammation and mucous gland changes** within the bronchi.
Atelectasis US Medical PG Question 10: A 31 year-old African-American female presents with painful shin nodules, uveitis, and calcified hilar lymph nodes. A transbronchial biopsy of the lung would most likely show which of the following histologies?
- A. Golden-brown fusiform rods
- B. Inflammation, fibrosis and cyst formation that is most prominent in subpleural regions
- C. Non-caseating granulomas (Correct Answer)
- D. Silica particles (birefringent) surrounded by collagen
- E. Patchy interstitial lymphoid infiltrate into walls of alveolar units
Atelectasis Explanation: ***Non-caseating granulomas***
- The constellation of **erythema nodosum** (painful shin nodules), **uveitis**, and **hilar lymphadenopathy** in an African-American female is highly characteristic of **sarcoidosis**.
- **Sarcoidosis** is pathologically defined by the presence of **non-caseating granulomas** in affected tissues, which would be visible on a transbronchial biopsy.
*Golden-brown fusiform rods*
- These are **ferruginous bodies**, characteristic of **asbestosis**, which is not supported by the patient's presentation.
- Asbestosis would typically involve a history of **asbestos exposure** and present with **pleural plaques** or **interstitial fibrosis**.
*Inflammation, fibrosis and cyst formation that is most prominent in subpleural regions*
- This description is more indicative of **pulmonary Langerhans cell histiocytosis**, a rare disease usually associated with **smoking**.
- It does not align with the patient's specific systemic manifestations like uveitis or erythema nodosum.
*Silica particles (birefringent) surrounded by collagen*
- This describes the histological findings of **silicosis**, an occupational lung disease resulting from exposure to **silica dust**.
- Silicosis is not typically associated with uveitis or erythema nodosum.
*Patchy interstitial lymphoid infiltrate into walls of alveolar units*
- This pattern can be seen in various interstitial lung diseases, but it is not specific for sarcoidosis.
- It could be found in conditions like **lymphoid interstitial pneumonia**, which does not fit the overall clinical picture.
More Atelectasis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.