Asthma pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Asthma pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Asthma pathology US Medical PG Question 1: A 25-year-old woman presents to an urgent care center following a bee sting while at a picnic with her friends. She immediately developed a skin rash and swelling over her arm and face. She endorses diffuse itching over her torso. Past medical history is significant for a mild allergy to pet dander and ragweed. She occasionally takes oral contraceptive pills and diphenhydramine for her allergies. Family history is noncontributory. Her blood pressure is 119/81 mm Hg, heart rate is 101/min, respiratory rate is 21/min, and temperature is 37°C (98.6°F). On physical examination, the patient has severe edema over her face and severe stridor with inspiration at the base of both lungs. Of the following options, this patient is likely experiencing which of the following hypersensitivity reactions?
- A. Type 2 - cytotoxic hypersensitivity reaction
- B. Type 1 - anaphylactic hypersensitivity reaction (Correct Answer)
- C. Both A & B
- D. Type 4 - cell mediated (delayed) hypersensitivity reaction
- E. Type 3 - immune complex mediated hypersensitivity reaction
Asthma pathology Explanation: ***Type 1 - anaphylactic hypersensitivity reaction***
- The rapid onset of symptoms like **skin rash**, **swelling (angioedema)**, **diffuse itching (pruritus)**, and **stridor** immediately following a **bee sting** is characteristic of an immediate, IgE-mediated hypersensitivity reaction.
- This type of reaction involves the release of **histamine** and other mediators from **mast cells** and **basophils**, leading to systemic symptoms, including potential airway obstruction.
*Type 2 - cytotoxic hypersensitivity reaction*
- Type 2 hypersensitivity involves **antibodies** (IgG or IgM) binding to antigens on the surface of **target cells**, leading to cell destruction.
- Examples include **hemolytic anemia** or **transfusion reactions**, which do not match the presented symptoms of allergic rash and angioedema.
*Both A & B*
- This option is incorrect because the patient's symptoms are highly consistent with a **Type 1 reaction** and do not align with the mechanisms or clinical manifestations of a Type 2 reaction.
- The immediate and widespread allergic response points specifically to IgE-mediated anaphylaxis.
*Type 4 - cell mediated (delayed) hypersensitivity reaction*
- Type 4 hypersensitivity is a **delayed reaction** mediated by **T cells**, typically appearing 24-72 hours after exposure.
- Examples include **contact dermatitis** or the **tuberculin skin test**, which are much slower in onset and different in presentation than the immediate, severe reaction described.
*Type 3 - immune complex mediated hypersensitivity reaction*
- Type 3 hypersensitivity involves the formation of **immune complexes** (antigen-antibody complexes) that deposit in tissues, causing inflammation.
- Conditions like **serum sickness** or **lupus nephritis** are examples and typically have a slower onset and different clinical presentation (e.g., vasculitis, glomerulonephritis) compared to acute anaphylaxis.
Asthma pathology US Medical PG Question 2: A 5-year-old girl presents to the emergency room with acute airway obstruction. Physical examination shows cough, episodic wheezing, and excess mucus production. Increased quantities of which of the following would predispose the child to extrinsic asthma:
- A. Kupffer cells
- B. Th17 lymphocytes
- C. Th1 lymphocytes
- D. Treg lymphocytes
- E. Th2 lymphocytes (Correct Answer)
Asthma pathology Explanation: ***Th2 lymphocytes***
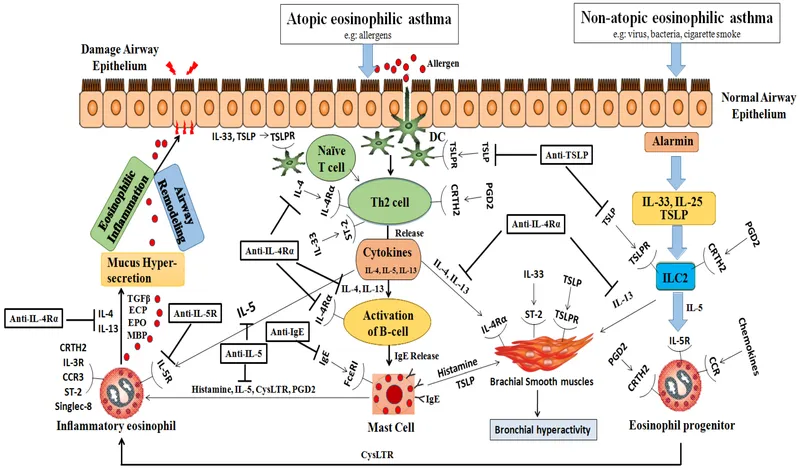
- **Th2 lymphocytes** play a central role in the pathogenesis of **extrinsic (allergic) asthma** by promoting allergic inflammation.
- They produce cytokines like **IL-4, IL-5, and IL-13**, which drive **IgE production**, **eosinophil activation**, and **mucus hypersecretion**, all characteristic features of asthma.
*Kupffer cells*
- **Kupffer cells** are specialized macrophages found in the liver, primarily involved in clearing pathogens and debris from the portal circulation.
- They are not directly involved in the pathogenesis of airway obstruction or allergic asthma.
*Th17 lymphocytes*
- **Th17 lymphocytes** are involved in host defense against extracellular bacteria and fungi and contribute to inflammation in autoimmune diseases.
- While they can be involved in some forms of severe asthma, they are not the primary drivers of **extrinsic, allergic asthma** characterized by IgE and eosinophilia.
*Th1 lymphocytes*
- **Th1 lymphocytes** primarily mediate cellular immunity against intracellular pathogens and are involved in delayed-type hypersensitivity reactions.
- They produce **IFN-γ**, which typically *suppresses* Th2 responses, and are therefore generally considered protective against allergic asthma.
*Treg lymphocytes*
- **Treg lymphocytes** (regulatory T cells) are crucial for maintaining immune tolerance and suppressing excessive immune responses.
- Their primary role is to *prevent* allergic and autoimmune diseases; therefore, an *increase* in their numbers would typically *reduce* the likelihood of asthma, not predispose to it.
Asthma pathology US Medical PG Question 3: A 7-year-old male is admitted to the hospital with his fourth episode of wheezing and dyspnea. His symptoms are exacerbated by mold and pollen. Which of the following is most likely to be observed in this patient?
- A. Normal FEV1/FVC
- B. Normal FEV1
- C. Abnormal chest radiograph
- D. Ground glass opacities on chest CT
- E. Sputum eosinophils (Correct Answer)
Asthma pathology Explanation: ***Sputum eosinophils***
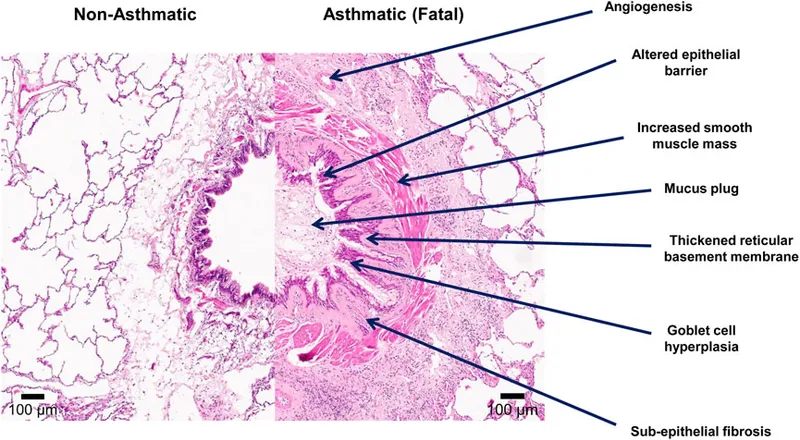
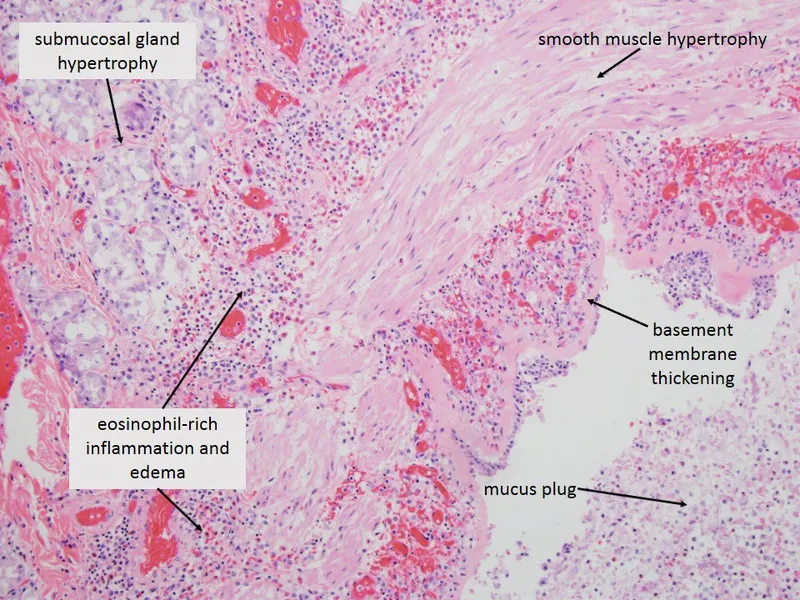
- The patient presents with recurrent wheezing, dyspnea, and exacerbations triggered by allergens (mold and pollen), which are classic signs of **asthma**.
- **Eosinophils** are key inflammatory cells in allergic asthma, and their presence in sputum is a common finding, especially during exacerbations.
*Normal FEV1/FVC*
- In asthma, there is **airway obstruction**, which typically leads to a **reduced FEV1/FVC ratio**, as FEV1 decreases proportionally more than FVC.
- A normal ratio would indicate the absence of obstructive lung disease, which contradicts the patient's symptoms.
*Normal FEV1*
- **Forced expiratory volume in 1 second (FEV1)** is typically decreased during an asthmatic exacerbation due to **bronchoconstriction** and airway narrowing.
- A normal FEV1 would be inconsistent with current breathing difficulties (wheezing and dyspnea) experienced by the patient.
*Abnormal chest radiograph*
- During an acute asthma exacerbation, a chest radiograph is often **normal** or may show signs of **hyperinflation** but generally does not show focal abnormalities.
- Significant abnormalities on chest X-ray might suggest complications like pneumonia or pneumothorax, which are not described here as the primary issue.
*Ground glass opacities on chest CT*
- **Ground glass opacities** on CT are characteristic of interstitial lung diseases or certain infections, like **pneumocystis pneumonia** or **viral pneumonia**.
- These are not typical findings in uncomplicated asthma and would suggest an alternative or coexisting pathology.
Asthma pathology US Medical PG Question 4: A 16-year-old boy with a history of severe, persistent asthma presents to the emergency department with severe shortness of breath and cough. He states that he was outside playing basketball with his friends, forgot to take his inhaler, and began to have severe difficulty breathing. On exam, he is in clear respiratory distress with decreased air movement throughout all lung fields. He is immediately treated with beta-agonists which markedly improve his symptoms. Prior to treatment, which of the following was most likely observed in this patient?
- A. Kussmaul's sign
- B. Pulsus paradoxus (Correct Answer)
- C. Friction rub
- D. Inspiratory stridor
- E. Increased breath sounds
Asthma pathology Explanation: ***Pulsus paradoxus***
* **Pulsus paradoxus** is a classic sign of **severe asthma exacerbation**, characterized by an abnormally large decrease in **systolic blood pressure** during inspiration.
* The marked improvement with **beta-agonists** confirms the likely diagnosis of acute severe asthma, making pulsus paradoxus a highly probable finding before treatment.
*Kussmaul's sign*
* **Kussmaul's sign** is a paradoxical rise in **jugular venous pressure (JVP)** during inspiration, typically seen in conditions like **constrictive pericarditis** or **right heart failure**.
* It is not associated with acute asthma exacerbations.
*Friction rub*
* A **friction rub** is a leathery or grating sound heard on auscultation, indicative of inflammation of the **pleura** (pleurisy) or **pericardium** (pericarditis).
* It is not a typical finding in asthma and would suggest an alternative or co-existing pathology.
*Inspiratory stridor*
* **Inspiratory stridor** is a harsh, high-pitched sound primarily heard during inspiration, caused by **upper airway obstruction** (e.g., croup, epiglottitis, foreign body aspiration).
* While severe shortness of breath is present, the symptom relief with beta-agonists points to **lower airway obstruction** characteristic of asthma rather than upper airway issues.
*Increased breath sounds*
* In **severe asthma exacerbations**, there is significant **bronchoconstriction** and **air trapping**, leading to markedly **decreased or absent breath sounds** on auscultation, not increased.
* Increased breath sounds might be heard in consolidation (pneumonia) or early stages of bronchiole inflammation, but not in severe asthma distress.
Asthma pathology US Medical PG Question 5: A 68-year-old male smoker dies suddenly in a car accident. He had smoked 2 packs per day for 40 years. His past medical history is notable for a frequent, very productive cough, recurrent respiratory infections and occasional wheezing. He had no other medical problems. At autopsy, which of the following is most likely to be found in this patient?
- A. Increased number and activity of goblet cells (Correct Answer)
- B. Ferruginous bodies
- C. Mucous gland atrophy
- D. Interstitial fibrosis of the lung
- E. Pleural plaques
Asthma pathology Explanation: ***Increased number and activity of goblet cells***
- The patient's history of a **productive cough**, **recurrent respiratory infections**, and **wheezing** in a chronic smoker strongly indicates **chronic bronchitis**.
- **Chronic bronchitis** is pathologically characterized by **hypertrophy of mucous glands** and an **increase in goblet cell number and activity**, leading to excessive mucus production.
*Ferruginous bodies*
- **Ferruginous bodies** are typically found in **asbestosis**, a lung disease caused by asbestos exposure.
- While asbestos exposure can cause respiratory symptoms, the sudden death and clinical picture without specific exposure history do not point to asbestosis as the primary diagnosis.
*Mucous gland atrophy*
- **Mucous gland atrophy** is generally not associated with chronic smoking and the symptoms described.
- In conditions like chronic bronchitis, there is actually **hypertrophy** and **hyperplasia** of the mucous glands, leading to increased mucus production.
*Interstitial fibrosis of the lung*
- **Interstitial fibrosis** is characteristic of conditions like **idiopathic pulmonary fibrosis** or other **interstitial lung diseases**.
- While smoking is a risk factor for some forms of fibrosis, the predominant symptoms of a productive cough and recurrent infections are more indicative of chronic bronchitis rather than diffuse interstitial fibrosis.
*Pleural plaques*
- **Pleural plaques** are **fibrous thickenings of the pleura**, almost exclusively associated with **asbestos exposure**.
- They are usually asymptomatic and do not directly explain the productive cough, recurrent infections, and wheezing presented in this patient's history.
Asthma pathology US Medical PG Question 6: A 48-year-old man has smoked approximately 3 packs of cigarettes per day for the past 12 years. Which of the following pathologic changes is most likely to occur in his bronchial epithelium?
- A. Metaplasia (Correct Answer)
- B. Hyperplasia
- C. Hypertrophy
- D. Dysplasia
- E. Atrophy
Asthma pathology Explanation: ***Metaplasia***
- Chronic irritation from **cigarette smoking** can cause the **bronchial epithelium** to change from ciliated columnar to stratified squamous, a process known as **metaplasia**.
- This adaptation makes the tissue more resistant to injury but results in the loss of important protective functions like **mucociliary clearance**.
*Hyperplasia*
- **Hyperplasia** involves an increase in the number of cells in a tissue or organ, often in response to increased demand or chronic stimulation.
- While smoking can cause hyperplasia of goblet cells and mucous glands in the bronchi, the direct epithelial change in response to chronic irritation is more specifically **metaplasia**.
*Hypertrophy*
- **Hypertrophy** is an increase in the size of individual cells, leading to an increase in the size of the organ or tissue.
- This is not the primary adaptive change seen in the bronchial epithelium in response to chronic smoking; instead, cells change their type.
*Dysplasia*
- **Dysplasia** refers to disorderly cell growth, often characterized by variations in cell size, shape, and organization; it is considered a precursor to cancer.
- While chronic smoking can eventually lead to dysplasia and then carcinoma, the initial and most common adaptive change in the bronchial epithelium is **metaplasia**.
*Atrophy*
- **Atrophy** is a decrease in cell size or number, leading to a reduction in the size of an organ or tissue, usually due to decreased workload, nutrition, or blood supply.
- This is not a typical response of the bronchial epithelium to chronic irritation from smoking, which tends to induce proliferative or adaptive changes.
Asthma pathology US Medical PG Question 7: A 5-year-old boy is brought to the emergency department by his parents for difficulty breathing. He was playing outside in the snow and had progressive onset of wheezing and gasping. His history is notable for eczema and nut allergies. The patient has respirations of 22/min and is leaning forward with his hands on his legs as he is seated on the table. Physical examination is notable for inspiratory and expiratory wheezes on exam. A nebulized medication is started and begins to relieve his breathing difficulties. Which of the following is increased in this patient as a result of this medication?
- A. Cyclic GMP
- B. Diacylglycerol
- C. ATP
- D. Protein kinase C
- E. Cyclic AMP (Correct Answer)
Asthma pathology Explanation: ***Correct: Cyclic AMP***
- The patient presents with an acute asthma exacerbation, likely triggered by cold weather and his atopic history (eczema, nut allergies). The nebulized medication is most likely a **beta-2 agonist** (e.g., albuterol), which acts by stimulating **adenylate cyclase**.
- This stimulation leads to an increase in intracellular **cyclic AMP (cAMP)**, which activates protein kinase A (PKA). PKA then phosphorylates various targets, leading to **bronchodilation** by relaxing airway smooth muscle.
*Incorrect: Cyclic GMP*
- **Cyclic GMP (cGMP)** is primarily involved in smooth muscle relaxation via nitric oxide signaling, not typically the target of bronchodilators used for acute asthma exacerbations.
- While some drugs like **nitrates** increase cGMP, bronchodilators like albuterol do not act through this pathway.
*Incorrect: Diacylglycerol*
- **Diacylglycerol (DAG)** is a secondary messenger produced by the hydrolysis of phosphatidylinositol 4,5-bisphosphate (PIP2) by phospholipase C.
- It is involved in various cell signaling pathways, including the activation of **protein kinase C (PKC)**, but it is not directly increased by beta-2 agonists.
*Incorrect: Protein kinase C*
- **Protein kinase C (PKC)** is a family of enzymes activated by calcium and **diacylglycerol (DAG)**, playing roles in cell growth, differentiation, and metabolism.
- Beta-2 agonists do not directly increase PKC activity; rather, they activate the adenylyl cyclase-cAMP-PKA pathway.
*Incorrect: ATP*
- **ATP (adenosine triphosphate)** is the cellular energy currency and is not specifically increased by beta-2 agonist therapy.
- While ATP is the substrate for adenylate cyclase to produce cAMP, beta-2 agonists do not increase ATP levels themselves.
Asthma pathology US Medical PG Question 8: As part of a clinical research study, microscopic analysis of tissues obtained from surgical specimens is performed. Some of these tissues have microscopic findings of an increase in the size of numerous cells within the tissue with an increase in the amount of cytoplasm, but the nuclei are uniform in size. Which of the following processes shows such microscopic findings?
- A. Liver following partial resection
- B. Female breasts at puberty
- C. Ovaries following menopause
- D. Uterine myometrium in pregnancy (Correct Answer)
- E. Cervix with chronic inflammation
Asthma pathology Explanation: ***Uterine myometrium in pregnancy***
- During pregnancy, the uterine myometrial cells undergo significant **hypertrophy** (increase in cell size) in response to hormonal stimulation, primarily *estrogen* and *progesterone*.
- This leads to a marked increase in the amount of **cytoplasm** and overall cell size, while maintaining relatively **uniform nuclei**, which precisely matches the microscopic findings described.
- The smooth muscle cells can increase **10-40 fold** in size, making this the classic example of physiologic hypertrophy.
- Note: Hyperplasia (increased cell number) also occurs but is less prominent; the microscopic findings described emphasize the hypertrophic changes.
*Liver following partial resection*
- The liver primarily undergoes **hyperplasia** (increase in cell number) to regenerate following partial resection.
- While some hypertrophy occurs, the dominant microscopic finding is an increase in hepatocyte **number** through proliferation rather than a marked increase in individual cell size and cytoplasm as the primary feature.
*Female breasts at puberty*
- Breast development at puberty involves both **hyperplasia** of the glandular epithelium and ductal structures and **adipose tissue deposition**, driven by *estrogen* and *progesterone*.
- The findings described (marked increase in cell size and cytoplasm with uniform nuclei) are more characteristic of the extreme cell hypertrophy seen in the gravid uterus rather than the mixed growth and differentiation patterns of pubertal breast development.
*Ovaries following menopause*
- Following menopause, the ovaries undergo **atrophy**, meaning a decrease in size and cellular activity due to declining hormonal production.
- This process involves a **decrease in cell size** and number, which is the opposite of the microscopic findings described in the question.
*Cervix with chronic inflammation*
- Chronic inflammation in the cervix can cause various changes, including **squamous metaplasia** (transformation of columnar epithelium to squamous epithelium) or an influx of inflammatory cells.
- While there might be some reactive cellular changes, it does not typically involve a widespread, uniform increase in cell size and cytoplasm within existing cells as described, but rather a change in cell type or infiltration by inflammatory cells.
Asthma pathology US Medical PG Question 9: A 31-year-old man presents to his primary care physician with shortness of breath. He states that he had a “cold” 2 weeks ago and since then has had a persistent cough and worsening shortness of breath. He denies fever, chills, chest pain, sore throat, or rhinorrhea. His medical history is significant for seasonal allergies. He uses fluticasone nasal spray. He had his tonsils removed when he was 8 years of age. His mother and maternal grandfather have cirrhosis, and his father has depression and hypertension. The patient endorses that he smokes tobacco socially on the weekends and uses marijuana daily. He drinks 1-2 beers after work with his co-workers most evenings. A chest radiograph shows hyperinflation of the lungs and hyperlucency. Routine labs are drawn, as shown below.
Serum:
Na+: 139 mEq/L
Cl-: 105 mEq/L
K+: 4.0 mEq/L
HCO3-: 26 mEq/L
Urea nitrogen: 15 mg/dL
Glucose: 100 mg/dL
Creatinine: 0.8 mg/dL
Alkaline phosphatase: 98 U/L
Aspartate aminotransferase (AST, GOT): 46 U/L
Alanine aminotransferase (ALT, GPT): 49 U/L
Pulmonary function tests are pending. Which of the following is most likely to confirm the patient’s diagnosis?
- A. Enzyme-linked immunosorbent assay (Correct Answer)
- B. Bronchoalveolar lavage
- C. Abdominal ultrasound
- D. Viral hepatitis serologies
- E. Pulmonary function tests
Asthma pathology Explanation: ***Enzyme-linked immunosorbent assay (ELISA)***
- This patient's presentation with **early-onset emphysema at age 31**, **hyperinflation and hyperlucency** on chest X-ray, and **strong family history of cirrhosis** (mother and maternal grandfather) strongly suggests **alpha-1 antitrypsin deficiency**.
- **ELISA is used to measure serum alpha-1 antitrypsin levels**, which is the key confirmatory test for this diagnosis. Low levels (<50-80 mg/dL) confirm the deficiency.
- Alpha-1 antitrypsin deficiency causes **panacinar emphysema** (especially in lower lobes) and can also cause **liver cirrhosis**, explaining the family history and mildly elevated transaminases.
- Once low levels are detected, **phenotyping or genotyping** can further characterize the specific mutation (most commonly PiZZ).
*Pulmonary function tests*
- PFTs would demonstrate **obstructive lung disease** with reduced FEV1/FVC ratio and confirm the presence of airflow limitation.
- However, PFTs are **non-specific** and would not distinguish alpha-1 antitrypsin deficiency from other causes of COPD/emphysema (smoking-related, chronic bronchitis, etc.).
- While diagnostically useful for characterizing severity, PFTs do not confirm the underlying etiology.
*Bronchoalveolar lavage*
- **Bronchoalveolar lavage (BAL)** is useful for diagnosing **infections**, **interstitial lung diseases**, **malignancies**, or **alveolar hemorrhage**.
- It is not indicated for confirming emphysema or alpha-1 antitrypsin deficiency, as these are diagnosed through clinical presentation, imaging, and serologic testing.
*Abdominal ultrasound*
- An **abdominal ultrasound** could evaluate for **liver disease** (cirrhosis, hepatomegaly) associated with alpha-1 antitrypsin deficiency.
- While it might reveal liver involvement, it does not confirm the pulmonary diagnosis or the underlying enzymatic deficiency itself.
- It would be considered as part of a comprehensive evaluation but is not the confirmatory test.
*Viral hepatitis serologies*
- These would test for **hepatitis A, B, C** infection, which are common causes of cirrhosis and elevated transaminases.
- However, the patient's respiratory symptoms, imaging findings of emphysema, young age, and family history point toward alpha-1 antitrypsin deficiency rather than viral hepatitis.
- While worth checking given the liver enzyme elevation, this would not confirm the primary diagnosis.
Asthma pathology US Medical PG Question 10: A 43-year-old man presents to the emergency department following a work-related accident in which both arms were amputated. The patient lost a substantial amount of blood prior to arrival, and his bleeding is difficult to control due to arterial damage and wound contamination with debris. His complete blood count (CBC) is significant for a hemoglobin (Hgb) level of 5.3 g/dL. The trauma surgery resident initiates the massive transfusion protocol and orders whole blood, O negative, which she explains is the universal donor. The patient receives 6 units of O negative blood prior to admission. He subsequently develops fever, chills, hematuria, and pulmonary edema. Several hours later, the patient goes into hemodynamic shock requiring the emergent administration of vasopressors. Of the following options, which hypersensitivity reaction occurred?
- A. Type 1 hypersensitivity reaction
- B. Combined type 1 and type 4 hypersensitivity reaction
- C. Type 3 hypersensitivity reaction
- D. Type 2 hypersensitivity reaction (Correct Answer)
- E. Type 4 hypersensitivity reaction
Asthma pathology Explanation: ***Type 2 hypersensitivity reaction***
- This scenario describes an **acute hemolytic transfusion reaction (AHTR)**, a classic example of a **Type II hypersensitivity reaction**. The recipient's antibodies (IgM) recognize and bind to antigens on the transfused red blood cells, leading to their destruction (hemolysis) via complement activation and cellular mechanisms.
- Symptoms like **fever, chills, hematuria (due to hemoglobinuria)**, and subsequent **shock** are characteristic of AHTR, even with O negative blood if other minor blood group antigens (e.g., Kell, Duffy) are incompatible or if the patient developed antibodies against these from previous transfusions or pregnancies.
*Type 1 hypersensitivity reaction*
- This type involves **IgE-mediated mast cell degranulation** and is associated with allergic reactions such as anaphylaxis, asthma, and hives.
- While anaphylaxis can cause shock, the systemic symptoms of **hemolysis and hematuria** are not characteristic of a Type 1 reaction.
*Combined type 1 and type 4 hypersensitivity reaction*
- This combination is uncommon in an acute transfusion setting and does not align with the presented symptoms.
- Type 1 is immediate allergic, and Type 4 is delayed cell-mediated, neither fully explaining the hemolytic features observed.
*Type 3 hypersensitivity reaction*
- This reaction involves the formation of **immune complexes** (antigen-antibody complexes) that deposit in tissues, leading to inflammation and damage (e.g., serum sickness, lupus nephritis).
- While immune complexes can cause systemic symptoms, the prominent hemolytic features and immediate presentation of a transfusion reaction are more indicative of Type 2.
*Type 4 hypersensitivity reaction*
- This is a **delayed type hypersensitivity** reaction mediated by **T cells**, taking 24-72 hours or longer to develop (e.g., contact dermatitis, tuberculin skin test).
- The acute onset of symptoms following transfusion makes a Type 4 reaction highly unlikely.
More Asthma pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.