Primary CNS tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Primary CNS tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Primary CNS tumors US Medical PG Question 1: A 3-year-old boy is brought to the emergency department after losing consciousness. His parents report that he collapsed and then had repetitive, twitching movements of the right side of his body that lasted approximately one minute. He recently started to walk with support. He speaks in bisyllables and has a vocabulary of almost 50 words. Examination shows a large purple-colored patch over the left cheek. One week later, he dies. Which of the following is the most likely finding on autopsy of the brain?
- A. Subependymal giant cell astrocytoma
- B. Periventricular calcification
- C. Brainstem glioma
- D. Leptomeningeal vascular malformation (Correct Answer)
- E. Intraparenchymal cyst
Primary CNS tumors Explanation: ***Leptomeningeal vascular malformation***
- The constellation of **seizures** and a **large purple patch** on the face (**port-wine stain** or nevus flammeus) strongly suggests **Sturge-Weber syndrome**.
- **Leptomeningeal angioma** (vascular malformation) is the characteristic brain finding in Sturge-Weber syndrome, often leading to neurological deficits, seizures, and increased intracranial pressure.
*Subependymal giant cell astrocytoma*
- This tumor is pathognomonic for **tuberous sclerosis complex**, which is typically associated with **facial angiofibromas** (adenoma sebaceum) and other skin lesions like ash-leaf spots.
- While tuberous sclerosis can present with seizures, the facial lesion described in the patient (large purple patch, or port-wine stain) is not consistent with the typical skin findings of tuberous sclerosis.
*Periventricular calcification*
- **Periventricular calcifications** are a hallmark sign of **congenital cytomegalovirus (CMV)** infection.
- While CMV can cause neurological sequelae and developmental delay, the clinical presentation with a distinct facial lesion and recent onset seizures is more indicative of Sturge-Weber syndrome.
*Brainstem glioma*
- **Brainstem gliomas** typically present with **cranial nerve deficits**, **ataxia**, and long tract signs, rather than focal seizures and a port-wine stain.
- The sudden onset of seizures and collapse, along with the characteristic facial lesion, points away from a primary brainstem tumor.
*Intraparenchymal cyst*
- An **intraparenchymal cyst** is a non-specific finding that could result from various causes, such as infection, trauma, or developmental anomalies.
- It does not specifically account for the combination of seizures and the facial **port-wine stain** seen in this patient.
Primary CNS tumors US Medical PG Question 2: A 57-year-old man is brought to the emergency department by his wife 20 minutes after having had a seizure. He has had recurrent headaches and dizziness for the past 2 weeks. An MRI of the brain shows multiple, round, well-demarcated lesions in the brain parenchyma at the junction between gray and white matter. This patient's brain lesions are most likely comprised of cells that originate from which of the following organs?
- A. Kidney
- B. Skin
- C. Lung (Correct Answer)
- D. Thyroid
- E. Prostate
Primary CNS tumors Explanation: ***Lung (Correct Answer)***
- **Lung cancer** is the most common cause of **brain metastases** in adults, accounting for approximately **50% of all cases**
- The clinical presentation—seizure, headaches, dizziness, and **multiple, round, well-demarcated lesions at the gray-white matter junction**—is classic for metastatic lung cancer
- Both **small cell and non-small cell lung cancers** have high propensity for hematogenous spread to the brain
- The watershed areas at the gray-white junction are common sites due to lodging of tumor emboli in terminal arterioles
*Kidney (Incorrect)*
- **Renal cell carcinoma (RCC)** can metastasize to the brain but accounts for only **5-10% of brain metastases**
- While RCC metastases can appear similar on imaging, lung cancer is statistically more likely given its higher prevalence
- RCC metastases are often **highly vascular and may hemorrhage**, which is not mentioned in this case
*Skin (Incorrect)*
- **Melanoma** has the **highest propensity per case** to metastasize to the brain among all cancers
- However, the **overall incidence of melanoma is much lower** than lung cancer, making it a less probable primary source
- Melanoma brain metastases often present as **hemorrhagic lesions** and would typically have skin findings or history
*Thyroid (Incorrect)*
- **Thyroid cancer** rarely metastasizes to the brain (accounts for <1% of brain metastases)
- Brain metastases from thyroid cancer typically occur in **advanced papillary or follicular carcinoma** or in **anaplastic thyroid cancer**
- More common metastatic sites for thyroid cancer are lung and bone
*Prostate (Incorrect)*
- **Prostate cancer very rarely metastasizes to the brain** (<1% of cases)
- Prostate cancer preferentially metastasizes to **bone (especially axial skeleton), lymph nodes, and liver**
- Brain metastases from prostate cancer suggest extremely advanced, aggressive disease and are exceptionally uncommon
Primary CNS tumors US Medical PG Question 3: A 23-year-old man comes to the physician for evaluation of decreased hearing, dizziness, and ringing in his right ear for the past 6 months. Physical examination shows multiple soft, yellow plaques and papules on his arms, chest, and back. There is sensorineural hearing loss and weakness of facial muscles bilaterally. His gait is unsteady. An MRI of the brain shows a 3-cm mass near the right internal auditory meatus and a 2-cm mass at the left cerebellopontine angle. The abnormal cells in these masses are most likely derived from which of the following embryological structures?
- A. Surface ectoderm
- B. Neural tube
- C. Neural crest (Correct Answer)
- D. Notochord
- E. Mesoderm
Primary CNS tumors Explanation: ***Neural crest***
- The patient's symptoms (bilateral sensorineural hearing loss, facial weakness, unsteady gait, central masses) along with cutaneous lesions (soft, yellow plaques) are highly suggestive of **Neurofibromatosis type 2 (NF2)**.
- NF2 is characterized by **vestibular schwannomas** (acoustic neuromas) and other CNS tumors, which are derived from **Schwann cells**. Schwann cells, along with melanocytes and other peripheral nervous system components, originate from the **neural crest**.
*Surface ectoderm*
- The surface ectoderm forms structures such as the **epidermis**, hair, nails, and anterior pituitary.
- While the skin lesions are present, the primary tumors (schwannomas) are not derived from the surface ectoderm.
*Neural tube*
- The neural tube gives rise to the **central nervous system** (brain and spinal cord) and motor neurons.
- While the tumors affect the brain and cranial nerves, the specific cell type forming schwannomas (Schwann cells) does not originate directly from the neural tube.
*Notochord*
- The notochord induces the formation of the neural tube and eventually degenerates, contributing to the **nucleus pulposus** of the intervertebral discs.
- It is not involved in the pathogenesis or cellular origin of schwannomas.
*Mesoderm*
- The mesoderm gives rise to connective tissues, blood, bone, muscle, and most internal organs.
- While some tumors can have mesodermal origins, schwannomas are neuroectodermal in origin.
Primary CNS tumors US Medical PG Question 4: A previously healthy 50-year-old woman is brought to the emergency department 30 minutes after she was observed having a seizure. On arrival, she is conscious and reports that she feels drowsy. An MRI of the brain shows a 4-cm, round, sharply demarcated mass. She undergoes resection of the mass. A photomicrograph of a section of the resected specimen is shown. This patient's mass is most likely derived from which of the following?
- A. Neurons
- B. Arachnoid cells (Correct Answer)
- C. Schwann cells
- D. Oligodendrocytes
- E. Astrocytes
Primary CNS tumors Explanation: ***Arachnoid cells***
- The description of a **round, sharply demarcated mass** in an adult, often presenting with seizures, is highly characteristic of a **meningioma**.
- Meningiomas are **benign tumors** that arise from the meninges, specifically the **arachnoid cap cells** (meningothelial cells).
- These tumors are typically **well-circumscribed**, extra-axial masses that compress adjacent brain tissue.
*Neurons*
- Tumors derived from neurons, such as **gangliogliomas** or **central neurocytomas**, are less common and typically do not present as sharply demarcated masses in this location.
- While neurons are the primary functional cells of the brain, most primary brain tumors arise from **glial or mesenchymal cells**, not neurons themselves.
*Schwann cells*
- Tumors of Schwann cells are known as **schwannomas** (or acoustic neuromas if arising from cranial nerves).
- Schwannomas typically occur along **cranial nerves** (especially CN VIII) in the cerebellopontine angle, presenting with hearing loss or balance issues, which is not described here.
*Oligodendrocytes*
- Tumors originating from oligodendrocytes are **oligodendrogliomas**, which are typically **infiltrative glial tumors** rather than sharply demarcated masses.
- They often present with calcifications ("fried egg" appearance on histology) and have a different appearance, not matching the classic presentation of a benign, encapsulated mass.
*Astrocytes*
- Astrocytes give rise to various **astrocytomas** (e.g., glioblastoma, pilocytic astrocytoma), which are generally **infiltrative** and poorly demarcated.
- While they can present with seizures, their typical MRI appearance and histological features differ from the described well-circumscribed mass.
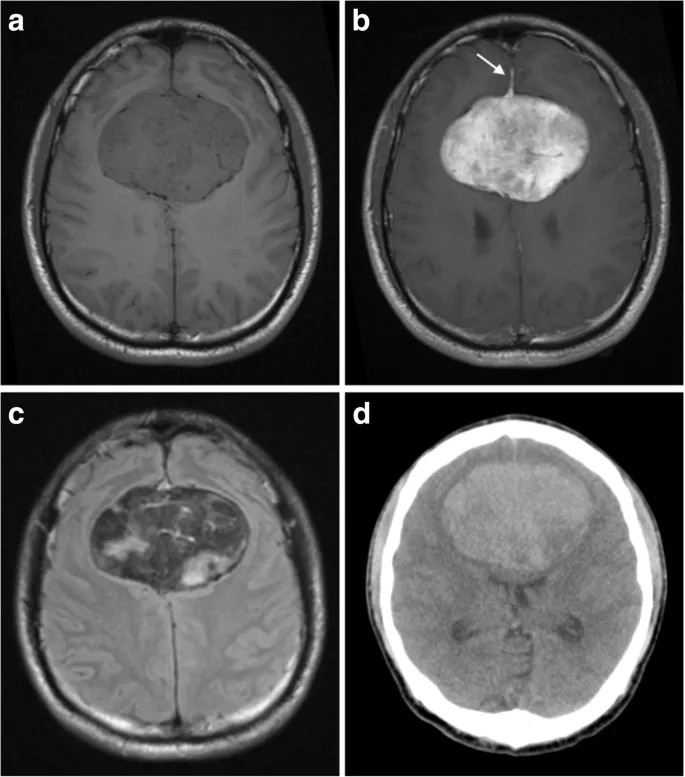
Primary CNS tumors US Medical PG Question 5: A 9-year-old girl is brought to her primary care physician because of a 4-month history of early morning headaches and worsening fatigue. The headaches are often accompanied by nausea and sometimes relieved by vomiting. She stopped going to her ballet lessons 2 weeks ago because she was embarrassed about falling frequently and having increasing difficulty performing the steps. Her temperature is 36.8°C (98.2°F), pulse is 98/min, and blood pressure is 105/65 mm Hg. She has a broad-based gait. While standing with both feet together and raising her arms, closing her eyes does not affect her balance. She is unable to perform rapid, alternating movements with her hands. An MRI of the brain is shown. Which of the following is the most likely diagnosis?
- A. Ependymoma
- B. Oligodendroglioma
- C. Pilocytic astrocytoma (Correct Answer)
- D. Acoustic schwannoma
- E. Diffuse brainstem glioma
Primary CNS tumors Explanation: ***Pilocytic astrocytoma***
- This is the most common **pediatric cerebellar tumor**, often presenting with **hydrocephalus** (causing morning headaches, nausea, and vomiting) and **cerebellar dysfunction** (ataxia, broad-based gait, dysdiadochokinesia).
- Imaging typically shows a **cystic lesion with an enhancing mural nodule**, consistent with the MRI findings of a large posterior fossa mass.
*Ependymoma*
- Ependymomas are also posterior fossa tumors, but they typically arise from the **floor of the fourth ventricle** and often show **calcifications** and characteristic "plastic tumor" extension into the cisterns, which are not clearly seen here.
- While they can cause hydrocephalus and cerebellar symptoms, the characteristic imaging findings differentiate it from a pilocytic astrocytoma.
*Oligodendroglioma*
- **Oligodendrogliomas** are typically found in the **cerebral hemispheres** of adults and are characterized by calcifications and slow growth.
- This patient is a child, and the tumor is located in the **posterior fossa**, making oligodendroglioma less likely.
*Acoustic schwannoma*
- **Acoustic schwannomas** arise from the vestibular portion of the **eighth cranial nerve** and primarily cause **hearing loss**, tinnitus, and balance issues.
- They are typically located at the **cerebellopontine angle** and are rare in children unless associated with neurofibromatosis type 2.
*Diffuse brainstem glioma*
- **Diffuse brainstem gliomas** cause rapid progressive **cranial nerve deficits**, ataxia, and long tract signs by infiltrating the brainstem.
- While they can cause hydrocephalus, the imaging usually shows an **expansile, poorly circumscribed lesion** within the brainstem itself, which is not the appearance here.
Primary CNS tumors US Medical PG Question 6: A 5-year-old boy is brought to the physician because of early morning headaches for the past 6 months. During this period, he has had severe nausea and occasional episodes of vomiting. For the past month, he has had difficulty walking and intermittent double vision. He was born at term and has been healthy apart from an episode of sinusitis 8 months ago that resolved spontaneously. He is at the 60th percentile for height and 50th percentile for weight. His temperature is 37.1°C (98.8°F), pulse is 80/min, and blood pressure is 105/64 mm Hg. Examination shows normal muscle strength and 2+ deep tendon reflexes bilaterally. He has a broad-based gait and impaired tandem gait. Fundoscopy shows bilateral swelling of the optic disc. There is esotropia of the left eye. Which of the following is the most likely diagnosis?
- A. Schwannoma
- B. Optic glioma
- C. Meningioma
- D. Hemangioblastoma
- E. Medulloblastoma (Correct Answer)
Primary CNS tumors Explanation: ***Medulloblastoma***
- The constellation of **early morning headaches**, **nausea/vomiting**, **papilledema** (swelling of the optic disc), **ataxia** (difficulty walking, broad-based gait, impaired tandem gait), and **cranial nerve palsy** (esotropia from abducens nerve dysfunction) in a young child strongly indicates increased intracranial pressure secondary to a posterior fossa tumor. **Medulloblastoma** is the most common malignant posterior fossa tumor in children.
- The location in the **cerebellum** explains the gait abnormalities (ataxia), and its rapid growth often leads to **hydrocephalus** and raised ICP symptoms.
*Schwannoma*
- **Schwannomas** typically arise from cranial nerves (most commonly the vestibular nerve, causing acoustic neuromas) and are rare in children.
- They tend to be **slow-growing** and usually present with localized symptoms like hearing loss or facial nerve weakness, rather than diffuse signs of increased ICP and ataxia.
*Optic glioma*
- **Optic gliomas** arise from the optic nerve and primarily cause **vision loss**, proptosis, and strabismus.
- While they can cause hydrocephalus if large and compressive, they typically do not cause pronounced cerebellar signs like ataxia, and primary presentation with early morning headaches and vomiting would be less common than vision issues.
*Meningioma*
- **Meningiomas** are typically **benign tumors** arising from the meninges that are rare in children and usually occur in older adults.
- They are slow-growing and often present with focal neurological deficits related to their location, but they are an improbable diagnosis given the age and constellation of rapidly developing symptoms of increased ICP and cerebellar dysfunction.
*Hemangioblastoma*
- **Hemangioblastomas** are vascular tumors, often associated with **von Hippel-Lindau disease**, and are typically found in the cerebellum, brainstem, or spinal cord.
- While they can cause cerebellar symptoms and increased ICP, they are more commonly seen in **adults** and are much rarer than medulloblastomas in children of this age.
Primary CNS tumors US Medical PG Question 7: A 10-year-old boy is brought to his pediatrician over concern for a 2-month history of headaches. Recently, the patient has been experiencing nausea and vomiting, along with some difficulty with coordination during soccer practice last week. On exam, the patient's temperature is 98.2°F (36.8°C), blood pressure is 110/80 mmHg, pulse is 72/min, and respirations are 14/min. On further evaluation, the patient is found to have a well-encapsulated posterior fossa mass. The patient undergoes surgical resection, and the mass is found to be positive for GFAP. Which of the following is derived from the same embryologic germ layer as the cells that comprise this tumor?
- A. Ependymal cells (Correct Answer)
- B. Nucleus pulposus
- C. Schwann cells
- D. Microglia
- E. Melanocytes
Primary CNS tumors Explanation: ***Ependymal cells***
- The tumor described is a **pilocytic astrocytoma**, a common **posterior fossa tumor** in children, characterized by its **well-encapsulated** nature and **GFAP positivity**, indicating an **astrocytic origin**.
- **Astrocytes** develop from the **neuroectoderm/neural tube**, as do **ependymal cells**, which line the ventricles and central canal of the spinal cord.
*Nucleus pulposus*
- The **nucleus pulposus** is a remnant of the **notochord**, which originates from the **mesoderm**.
- This embryological origin is distinct from the **neuroectodermal** origin of the tumor cells.
*Schwann cells*
- **Schwann cells** are derived from the **neural crest**, which is also **ectodermal** but represents a different lineage than the **neural tube**.
- While both contribute to the nervous system, **neural crest cells** form the peripheral nervous system, whereas the **neural tube** forms the central nervous system.
*Microglia*
- **Microglia** are the immune cells of the CNS and are derived from the **mesoderm**, specifically from **monocytes** in the yolk sac.
- Their origin is distinct from the **neuroectodermal** lineage of astrocytes.
*Melanocytes*
- **Melanocytes** are pigment-producing cells found in the skin, hair, and eyes, and they are derived from the **neural crest**.
- This makes their embryological origin different from the **neural tube** cells that give rise to astrocytes.
Primary CNS tumors US Medical PG Question 8: An 8-year-old boy is brought to the pediatrician because his mother is concerned about recent behavioral changes. His mother states that she has started to notice that he is slurring his speech and seems to be falling more than normal. On exam, the pediatrician observes the boy has pes cavus, hammer toes, and kyphoscoliosis. Based on these findings, the pediatrician is concerned the child has a trinucleotide repeat disease. Which of the following trinucleotide repeats is this child most likely to possess?
- A. CTG
- B. GAA (Correct Answer)
- C. CGG
- D. CAG
- E. GCC
Primary CNS tumors Explanation: ***GAA***
- This trinucleotide repeat is associated with **Friedreich's ataxia**, an autosomal recessive neurodegenerative disorder.
- The presented symptoms of **ataxia** (slurred speech, falling), **pes cavus**, **hammer toes**, and **kyphoscoliosis** are classic features of Friedreich's ataxia.
*CTG*
- This trinucleotide repeat is associated with **myotonic dystrophy type 1**, an autosomal dominant disorder.
- While it causes muscle weakness, it is characterized by **myotonia** (delayed muscle relaxation), cataracts, and frontal baldness, which are not described here.
*CGG*
- This trinucleotide repeat is associated with **fragile X syndrome**, an X-linked dominant disorder.
- Fragile X syndrome primarily causes intellectual disability, behavioral issues (e.g., autism spectrum disorder), and characteristic facial features, but not the specific neurological and orthopedic findings seen in this patient.
*CAG*
- This trinucleotide repeat is associated with several neurodegenerative diseases, including **Huntington's disease**, spinocerebellar ataxias, and **dentatorubral-pallidoluysian atrophy**.
- Huntington's disease, for example, presents with chorea, cognitive decline, and psychiatric symptoms, differing from the patient's presentation.
*GCC*
- This trinucleotide repeat is associated with **fragile X-associated tremor/ataxia syndrome (FXTAS)**.
- FXTAS typically affects older adult carriers of premutation alleles for fragile X, presenting with intention tremor and gait ataxia, not the early childhood onset and specific orthopedic deformities seen here.
Primary CNS tumors US Medical PG Question 9: A 47-year-old woman comes to the physician because of a 2-month history of a lump on her neck and a 1-week history of hoarseness. Examination shows a 3-cm, firm, non-tender nodule on the anterior neck. Further evaluation confirms a thyroid malignancy, and she undergoes thyroidectomy. Histopathologic examination of the surgical specimen shows lymphatic invasion. Genetic analysis shows an activating mutation in the RET/PTC genes. Microscopic examination of the surgical specimen is most likely to also show which of the following?
- A. Pleomorphic giant cells with numerous atypical mitotic figures
- B. Cuboidal cells arranged spherically around colloid lakes
- C. Hyperplastic epithelium with colloid scalloping
- D. Calcified spherules and large oval cells with empty-appearing nuclei (Correct Answer)
- E. Sheets of polygonal cells surrounding amyloid deposition
Primary CNS tumors Explanation: ***Calcified spherules and large oval cells with empty-appearing nuclei***
- The presence of an **activating mutation in RET/PTC genes**, **lymphatic invasion**, and a new neck lump with hoarseness (suggesting nerve involvement) are highly characteristic of **papillary thyroid carcinoma**.
- Microscopic features of papillary thyroid carcinoma include **Psammoma bodies (calcified spherules)**, **Orphan Annie eye nuclei (large oval cells with empty-appearing nuclei)**, and nuclear grooves.
*Pleomorphic giant cells with numerous atypical mitotic figures*
- This description typically refers to **anaplastic thyroid carcinoma**, a highly aggressive and undifferentiated tumor.
- While anaplastic carcinoma can present with rapid growth and hoarseness, it is less commonly associated with a **RET/PTC mutation** (BRAF mutations are more common) and typically has a much poorer prognosis, often presenting with a rapidly enlarging mass rather than a 2-month history suggestive of a more indolent tumor.
*Cuboidal cells arranged spherically around colloid lakes*
- This morphology is characteristic of **follicular thyroid carcinoma** or **follicular adenoma**.
- While follicular tumors can have RET/PTC mutations in some variants, the classic features described (empty-appearing nuclei and psammoma bodies) are absent here.
*Hyperplastic epithelium with colloid scalloping*
- This describes the histologic features seen in **Graves' disease** or **diffuse toxic goiter**, a benign condition.
- It is not indicative of malignancy, and the patient's presentation with a solitary nodule and hoarseness points to a malignant process.
*Sheets of polygonal cells surrounding amyloid deposition*
- This is the classic microscopic appearance of **medullary thyroid carcinoma**.
- Medullary thyroid carcinoma is also associated with **RET mutations**, but these are typically **germline or somatic RET point mutations** (e.g., RET M918T), not RET/PTC rearrangements, and it arises from parafollicular C cells, producing calcitonin, not thyroid hormones.
Primary CNS tumors US Medical PG Question 10: A 12-year-old boy is brought to the emergency department after he vomited and said he was having double vision in school. He also says that he has been experiencing morning headaches, nausea, and dizziness over the last month. He has no past medical history and is not taking any medications. Physical exam reveals a broad-based gait, dysmetria on finger-to-nose testing, and nystagmus. Both serum and urine toxicology are negative, and radiography reveals a solid mass in the midline cerebellum that enhances after contrast administration. Biopsy of this lesion reveals cells of primitive neuroectodermal origin. Which of the following would most likely be seen on histology of this lesion?
- A. Rosettes with small blue cells (Correct Answer)
- B. Rosenthal fibers
- C. Tooth enamel-like calcification
- D. Foamy cells and high vascularity
- E. Perivascular pseudorosettes
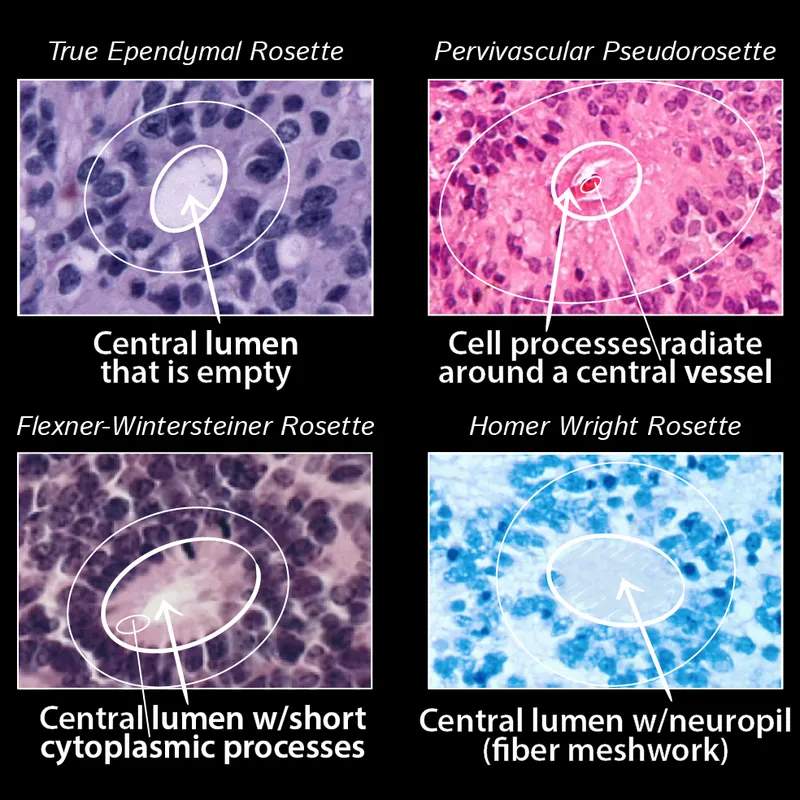
Primary CNS tumors Explanation: ***Rosettes with small blue cells***
- The description of a **midline cerebellar mass** in a child, presenting with signs of **increased intracranial pressure (headaches, vomiting, double vision)** and **cerebellar dysfunction (broad-based gait, dysmetria, nystagmus)**, is classic for **medulloblastoma**.
- **Medulloblastomas** are primitive neuroectodermal tumors (PNETs) known for their distinctive histology of **small, round, blue cells** forming **Homer-Wright rosettes**.
*Rosenthal fibers*
- **Rosenthal fibers** are eosinophilic, corkscrew-shaped structures that are characteristic histological features of **pilocytic astrocytomas**.
- While pilocytic astrocytomas can be cerebellar and common in children, the question describes a "solid mass of primitive neuroectodermal origin" rather than the typical cystic lesion with mural nodule associated with pilocytic astrocytomas, and the aggressive presentation points away from pilocytic astrocytoma.
*Tooth enamel-like calcification*
- **Tooth enamel-like calcification** is a pathognomonic feature of **craniopharyngiomas**, which are typically supratentorial (in the sellar region) and cause symptoms related to pituitary dysfunction and optic chiasm compression, not cerebellar dysfunction.
- The location and symptoms provided in the vignette do not match the typical presentation of a craniopharyngioma.
*Foamy cells and high vascularity*
- **Foamy cells and high vascularity** are characteristic features of **hemangioblastomas**, which are typically seen in adults, often associated with **von Hippel-Lindau disease**, and are more commonly located in the cerebellum.
- However, the patient's age (12-year-old) and the description of cells of "primitive neuroectodermal origin" do not align with the typical presentation or origin of hemangioblastomas.
*Perivascular pseudorosettes*
- **Perivascular pseudorosettes** are the classic histological finding in **ependymomas**, another common pediatric brain tumor.
- While ependymomas can occur in the posterior fossa, they typically arise from the floor of the fourth ventricle and are not described as having primitive neuroectodermal origin in the same way medulloblastomas are, and the specific rosettes formed by medulloblastomas are Homer-Wright rosettes.
More Primary CNS tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.