Peripheral nerve disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peripheral nerve disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Peripheral nerve disorders US Medical PG Question 1: A 57-year-old man presents to his primary care physician with a 2-month history of right upper and lower extremity weakness. He noticed the weakness when he started falling far more frequently while running errands. Since then, he has had increasing difficulty with walking and lifting objects. His past medical history is significant only for well-controlled hypertension, but he says that some members of his family have had musculoskeletal problems. His right upper extremity shows forearm atrophy and depressed reflexes while his right lower extremity is hypertonic with a positive Babinski sign. Which of the following is most likely associated with the cause of this patient's symptoms?
- A. HLA-DR2 haplotype
- B. Mutation in SOD1 (Correct Answer)
- C. Viral infection
- D. HLA-B8 haplotype
- E. Mutation in SMN1
Peripheral nerve disorders Explanation: ***Mutation in SOD1***
- The patient exhibits features of both **upper motor neuron (UMN)** and **lower motor neuron (LMN)** lesions, specifically **forearm atrophy** and depressed reflexes (LMN) alongside **hypertonicity** and a **positive Babinski sign** (UMN). This combination is characteristic of **amyotrophic lateral sclerosis (ALS)**.
- Mutations in the **superoxide dismutase 1 (SOD1)** gene are responsible for approximately 20% of familial ALS cases, aligning with the patient's report of "some members of his family have had musculoskeletal problems."
*HLA-DR2 haplotype*
- The **HLA-DR2 haplotype** is strongly associated with **multiple sclerosis (MS)**, an autoimmune demyelinating disease.
- While MS can cause UMN symptoms, it typically does not present with the pronounced LMN signs like **atrophy** and **depressed reflexes** seen in this patient.
*Viral infection*
- **Viral infections** can trigger various neurological conditions, such as **Guillain-Barré syndrome** (GBS) which causes demyelination of peripheral nerves.
- GBS primarily results in **ascending motor weakness** and **areflexia** (LMN signs), but it does not cause UMN signs like hypertonicity or a positive Babinski sign.
*HLA-B8 haplotype*
- The **HLA-B8 haplotype** is associated with several autoimmune diseases, including **myasthenia gravis** and **celiac disease**.
- While myasthenia gravis causes **muscle weakness**, it is characterized by **fluctuating weakness** that worsens with activity and improves with rest, affecting specific muscle groups, unlike the progressive UMN and LMN involvement seen here.
*Mutation in SMN1*
- A **mutation in the SMN1 gene** is the primary cause of **spinal muscular atrophy (SMA)**, a genetic disorder.
- SMA specifically leads to the death of **lower motor neurons** in the spinal cord, resulting in exclusively LMN signs such as **muscle weakness** and **atrophy**, without any UMN involvement (e.g., hypertonicity or Babinski sign).
Peripheral nerve disorders US Medical PG Question 2: A 29-year-old woman presents with progressive vision loss in her right eye and periorbital pain for 5 days. She says that she has also noticed weakness, numbness, and tingling in her left leg. Her vital signs are within normal limits. Neurological examination shows gait imbalance, positive Babinski reflexes, bilateral spasticity, and exaggerated deep tendon reflexes in the lower extremities bilaterally. FLAIR MRI is obtained and is shown in the image. Which of the following is the most likely cause of this patient’s condition?
- A. Amyotrophic lateral sclerosis
- B. Multiple sclerosis (Correct Answer)
- C. Acute disseminated encephalomyelitis
- D. Lead intoxication
- E. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
Peripheral nerve disorders Explanation: ***Multiple sclerosis***
- This patient's presentation with **optic neuritis** (vision loss, periorbital pain), disseminated neurological symptoms (**weakness, numbness, tingling in the left leg**, gait imbalance, spasticity, exaggerated DTRs, Babinski reflexes), and multifocal white matter lesions on MRI (FLAIR image would show **Dawson's fingers** or juxtacortical/infratentorial lesions) is highly characteristic of **multiple sclerosis**.
- The symptoms are **disseminated in space and time**, meaning different neurological deficits occurring at different locations in the CNS at different times, as suggested by the right eye and left leg involvement.
*Amyotrophic lateral sclerosis*
- Primarily a **motor neuron disease** affecting both upper and lower motor neurons, causing progressive muscle weakness, atrophy, and fasciculations.
- It does not typically involve **sensory deficits** (numbness, tingling), **optic neuritis**, or extensive white matter lesions on MRI.
*Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)*
- A genetic (NOTCH3 gene) small vessel disease causing recurrent **strokes, migraine with aura**, and progressive cognitive decline, typically starting in middle age.
- While it causes white matter abnormalities on MRI, it does not typically present with **inflammatory demyelination** causing optic neuritis or the diverse neurological relapses seen in MS.
*Acute disseminated encephalomyelitis*
- This is a monophasic, immune-mediated demyelinating disorder that typically occurs **after an infection or vaccination**.
- It often has a more **acute and severe onset** with encephalopathy, and while it causes multifocal white matter lesions, it is typically a single event rather than relapsing-remitting course seen in MS.
*Lead intoxication*
- Lead poisoning can cause a variety of neurological symptoms, including **peripheral neuropathy** (motor and sensory), **encephalopathy**, and cognitive impairment.
- It does not typically cause **optic neuritis**, demyelinating lesions in the CNS, or the specific pattern of neurological deficits characteristic of MS.
Peripheral nerve disorders US Medical PG Question 3: A 63-year-old man presents to the clinic concerned about numbness and weakness in his bilateral shoulders and arms for the past 8 weeks. The symptoms started when he fell from scaffolding at work and landed on his back. Initial workup was benign and he returned to normal duty. However, his symptoms have progressively worsened since the fall. He denies fever, back pain, preceding vomiting, and diarrhea. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, ischemic heart disease, and a 48-pack-year cigarette smoking history. He takes atorvastatin, hydrochlorothiazide, lisinopril, labetalol, and metformin. His blood pressure is 132/82 mm Hg, the pulse is 72/min, and the respiratory rate is 15/min. All cranial nerves are intact. Muscle strength is reduced in the upper limbs (4/5 bilaterally) but normal in the lower limbs. Perception of sharp stimuli and temperature is reduced on his shoulders and upper arms. The vibratory sense is preserved. Sensory examination is normal in the lower limbs. What is the most likely diagnosis?
- A. Anterior cord syndrome
- B. Central cord syndrome (Correct Answer)
- C. Guillain-Barre syndrome
- D. Vitamin B12 deficiency
- E. Pontine infarction
Peripheral nerve disorders Explanation: ***Central cord syndrome***
- This syndrome typically results from a **hyperextension injury** in patients with pre-existing cervical spinal stenosis, leading to damage to the central gray matter and surrounding tracts.
- It classically presents with greater **motor weakness in the upper extremities** than in the lower extremities, and a **"cape-like" distribution of sensory loss** (impaired pain and temperature sensation) over the shoulders and arms due to spinothalamic tract involvement, as seen in this patient.
*Anterior cord syndrome*
- This syndrome is characterized by **paraplegia/quadriplegia**, dissociated sensory loss (loss of **pain and temperature sensation**), and bowel/bladder dysfunction below the level of the lesion.
- It spares **proprioception and vibratory sensation** since the posterior columns remain intact, which is not fully consistent with the patient's presentation of primarily sensory symptoms in the upper limbs with normal strength.
*Guillain-Barre syndrome*
- This is an **acute demyelinating polyneuropathy** that typically presents with **progressive, ascending weakness** and often **areflexia**, usually following an infection.
- The patient's symptoms are primarily sensory, descending, and lack significant weakness or preceding infection, making this diagnosis less likely.
*Vitamin B12 deficiency*
- This deficiency can cause **subacute combined degeneration** of the spinal cord, affecting the **posterior columns** (vibratory and proprioception loss) and **corticospinal tracts** (weakness, spasticity).
- The patient primarily has loss of pain and temperature sensation with preserved vibratory sense and normal strength, which is inconsistent with B12 deficiency.
*Pontine infarction*
- A pontine infarction would present with a constellation of cranial nerve deficits, motor weakness (hemiparesis or quadriplegia), and cerebellar signs due to its location in the brainstem.
- The patient has intact cranial nerves, normal muscle strength, and specific sensory deficits limited to the shoulders and arms, which does not align with a brainstem stroke.
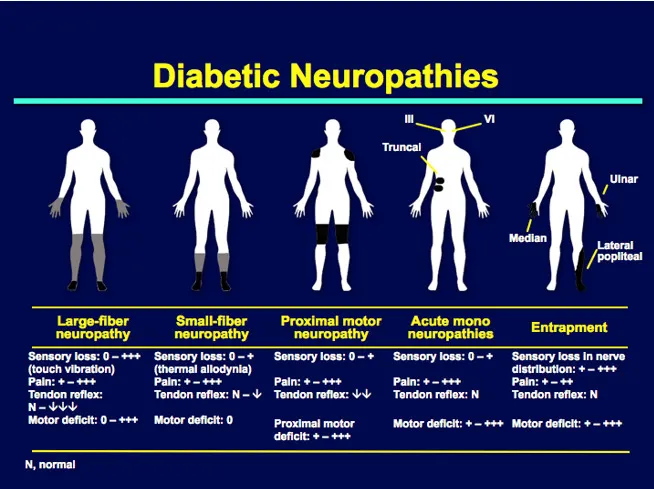
Peripheral nerve disorders US Medical PG Question 4: A 61-year-old woman comes to the physician for evaluation of numbness and a burning sensation in her feet for the past 5 months. She has type 2 diabetes mellitus and hypercholesterolemia. Her blood pressure is 119/82 mm Hg. Neurologic examination shows decreased sensation to pinprick, light touch, and vibration over the soles of both feet. There is a nontender ulcer on the plantar surface of her left foot. Pedal pulses are strong bilaterally. Her hemoglobin A1c concentration is 8.6%. Which of the following processes is most likely involved in the pathogenesis of this patient's current symptoms?
- A. Demyelination of posterior columns and lateral corticospinal tracts
- B. Increased protein deposition in endoneural vessel walls (Correct Answer)
- C. Accumulation of lipids and foam cells in arteries
- D. Elevated hydrostatic pressure in arteriolar lumen
- E. Osmotic damage to oligodendrocyte nerve sheaths
Peripheral nerve disorders Explanation: ***Increased protein deposition in endoneural vessel walls***
- The patient exhibits symptoms consistent with **diabetic neuropathy**, including numbness, burning sensation, decreased sensation to pinprick, light touch, and vibration, along with a plantar ulcer and poorly controlled diabetes (HbA1c 8.6%).
- **Chronic hyperglycemia** in diabetes leads to the accumulation of advanced glycation end products (AGEs) and activation of the polyol pathway, which cause **thickening and hyalinization of endoneural vessel walls**, impairing blood flow to peripheral nerves.
*Demyelination of posterior columns and lateral corticospinal tracts*
- **Posterior column demyelination** occurs in conditions like **vitamin B12 deficiency** (subacute combined degeneration) and results in loss of vibratory and proprioceptive sensation.
- **Lateral corticospinal tract demyelination** is associated with **motor deficits** (e.g., spasticity, weakness), which are not the primary symptoms described in this patient.
*Accumulation of lipids and foam cells in arteries*
- This process describes **atherosclerosis**, which can lead to peripheral artery disease (PAD) and contribute to foot ulcers due to **ischemia**.
- However, the patient has **strong pedal pulses**, making significant atherosclerosis of the macrovessels less likely to be the primary cause of her neuropathic symptoms.
*Elevated hydrostatic pressure in arteriolar lumen*
- **Elevated hydrostatic pressure** in arterioles (hypertension) contributes to various microvascular complications, but it is not the direct or most prominent mechanism for the **nerve damage** seen in diabetic neuropathy.
- The patient's blood pressure is relatively normotensive, making this cause less likely to be the predominant factor.
*Osmotic damage to oligodendrocyte nerve sheaths*
- **Oligodendrocytes** are responsible for myelin formation in the **central nervous system**, not the peripheral nervous system.
- While osmotic damage can occur in conditions like **rapid correction of hyponatremia** (osmotic demyelination syndrome), it primarily affects the CNS and is not typically associated with chronic diabetic peripheral neuropathy.
Peripheral nerve disorders US Medical PG Question 5: A 28-year-old man presents to the emergency department with lower extremity weakness. He was in his usual state of health until 10 days ago. He then began to notice his legs were “tiring out” during his workouts. This progressed to difficulty climbing the stairs to his apartment. He has asthma and uses albuterol as needed. He has no significant surgical or family history. He smokes marijuana daily but denies use of other recreational drugs. He is sexually active with his boyfriend of 2 years. He has never traveled outside of the country but was camping 3 weeks ago. He reports that he had diarrhea for several days after drinking unfiltered water from a nearby stream. On physical examination, he has 1/5 strength in his bilateral lower extremities. He uses his arms to get up from the chair. Achilles and patellar reflexes are absent. A lumbar puncture is performed, and results are as shown below:
Cerebral spinal fluid:
Color: Clear
Pressure: 15 cm H2O
Red blood cell count: 0 cells/µL
Leukocyte count: 3 cells/ µL with lymphocytic predominance
Glucose: 60 mg/dL
Protein: 75 mg/dL
A culture of the cerebral spinal fluid is pending. Which of the following is the part of the management for the patient’s most likely diagnosis?
- A. Aspirin
- B. Intravenous methylprednisolone
- C. Plasmapheresis (Correct Answer)
- D. Doxycycline
- E. Azithromycin
Peripheral nerve disorders Explanation: ***Plasmapheresis***
- The patient exhibits classic signs of **Guillain-Barré Syndrome (GBS)**: **ascending paralysis** starting in the lower extremities, progression over days to weeks, and **areflexia**.
- The **CSF findings** of **elevated protein** with normal cell count (**albuminocytologic dissociation**) are characteristic of GBS. Plasmapheresis is a first-line treatment, as it removes pathogenic autoantibodies from the plasma.
*Aspirin*
- **Aspirin** is an antiplatelet agent used for cardiovascular disease prevention or acute ischemic events.
- It has no role in the treatment of GBS, which is an autoimmune demyelinating polyneuropathy.
*Intravenous methylprednisolone*
- While corticosteroids like **methylprednisolone** are used for some autoimmune conditions, they have been shown to be **ineffective** and potentially harmful in GBS.
- The primary treatments for GBS are **intravenous immunoglobulin (IVIG)** and **plasmapheresis**.
*Doxycycline*
- **Doxycycline** is a broad-spectrum antibiotic commonly used for bacterial infections like Lyme disease, rickettsial infections, and some STIs.
- It is not indicated for the autoimmune pathophysiology of GBS.
*Azithromycin*
- **Azithromycin** is a macrolide antibiotic frequently used for respiratory tract infections and certain sexually transmitted infections.
- It has no therapeutic benefit in the management of GBS.
Peripheral nerve disorders US Medical PG Question 6: A 26-year-old man presents to his primary doctor with one week of increasing weakness. He reports that he first noticed difficulty walking while attending his sister's graduation last week, and yesterday he had difficulty taking his coffee cup out of the microwave. He remembers having nausea and vomiting a few weeks prior, but other than that has no significant medical history. On exam, he has decreased reflexes in his bilateral upper and lower extremities, with intact sensation. If a lumbar puncture is performed, which of the following results are most likely?
- A. High lymphocytes, high protein, low glucose, high opening pressure
- B. Normal cell count, high protein, normal glucose, normal opening pressure (Correct Answer)
- C. High neutrophils, high protein, low glucose, high opening pressure
- D. Normal cell count, normal protein, normal glucose, normal opening pressure
- E. High lymphocytes, normal protein, normal glucose, normal opening pressure
Peripheral nerve disorders Explanation: ***Normal cell count, high protein, normal glucose, normal opening pressure***
- This patient's presentation with **ascending paralysis** following a viral illness (nausea and vomiting a few weeks prior) is highly suggestive of **Guillain-Barré Syndrome (GBS)**.
- The classic cerebrospinal fluid (CSF) finding in GBS is **albuminocytologic dissociation**, characterized by a **normal white blood cell count** but **elevated protein levels** due to inflammation of nerve roots and increased permeability of the blood-nerve barrier.
*High lymphocytes, high protein, low glucose, high opening pressure*
- This CSF profile, particularly **low glucose** and **high lymphocytes**, is more characteristic of **bacterial meningitis** or certain **viral encephalitides**, which do not fit the clinical picture of ascending paralysis and intact sensation.
- While GBS can have high protein, the presence of low glucose points away from GBS.
*High neutrophils, high protein, low glucose, high opening pressure*
- This CSF profile strongly suggests **acute bacterial meningitis**, characterized by a prominent **neutrophilic pleocytosis**, low glucose, and high protein, which is not consistent with the patient's symptoms of progressive weakness.
- The patient's presentation is a subacute progressive weakness, not an acute infectious process affecting the CNS.
*Normal cell count, normal protein, normal glucose, normal opening pressure*
- A completely normal CSF profile would make the diagnosis of GBS less likely, as **elevated CSF protein** is a hallmark of the condition due to nerve root inflammation.
- While GBS can sometimes have normal CSF early in the disease, in the context of progressing weakness, elevated protein is expected.
*High lymphocytes, normal protein, normal glucose, normal opening pressure*
- This CSF profile with **high lymphocytes** and otherwise normal parameters might indicate a **viral meningioencephalitis** or other lymphocytic inflammatory conditions, but it does not align with the characteristic **elevated protein** seen in GBS.
- The absence of elevated protein despite significant neurological symptoms makes this less likely for GBS.
Peripheral nerve disorders US Medical PG Question 7: A 35-year-old man is transferred to the intensive care unit after a motorcycle accident. He does not open his eyes with painful stimuli. He makes no sounds. He assumes decerebrate posture with sternal rub. His right eye is abnormally positioned downward and outward and has a dilated pupil which is not responsive to light. In contrast to this patient's findings, one would expect a patient with a diabetic mononeuropathy of the oculomotor nerve to present in which fashion?
- A. Fixed dilated pupil with normal extraocular movements
- B. Downward and outward gaze, ptosis, and a fixed, dilated pupil
- C. Ptosis only
- D. Downward and outward gaze with ptosis and a responsive pupil (Correct Answer)
- E. Inability to abduct the eye
Peripheral nerve disorders Explanation: ***Downward and outward gaze with ptosis and a responsive pupil***
- **Diabetic mononeuropathy** of the oculomotor nerve (CN III) typically spares the **pupillary fibers** because they are superficial and supplied by pial vessels, which are often unaffected by microvascular ischemia.
- This results in a **"pupil-sparing" CN III palsy**, where extraocular muscles are affected (leading to **downward and outward gaze** and **ptosis**), but the pupil remains reactive.
*Fixed dilated pupil with normal extraocular movements*
- A **fixed dilated pupil** without other extraocular movement deficits is more suggestive of a direct injury to the **iris sphincter** or a lesion affecting the efferent pupillary fibers, not typically isolated diabetic mononeuropathy.
- Normal extraocular movements contradict a significant oculomotor nerve palsy of any etiology.
*Downward and outward gaze, ptosis, and a fixed, dilated pupil*
- This constellation of symptoms, including a **fixed, dilated pupil**, is characteristic of a **compressive lesion** affecting the oculomotor nerve (e.g., aneurysm, tumor), as it damages the superficial pupillary fibers.
- Diabetic neuropathy typically involves the vasa nervorum of the central part of the nerve, sparing the superficial, parasympathetic pupillary fibers.
*Ptosis only*
- While **ptosis** is a component of oculomotor nerve palsy, it typically occurs with other signs like **downward and outward gaze**. Isolated ptosis might suggest a lesion affecting only the efferent fibers to the **levator palpebrae superioris** or a milder, incomplete palsy.
- More commonly, isolated ptosis can be due to conditions like **myasthenia gravis** or Horner's syndrome (which also includes miosis and anhidrosis).
*Inability to abduct the eye*
- **Inability to abduct the eye** (move it laterally) is a classic sign of an **abducens nerve (CN VI) palsy**, not an oculomotor nerve (CN III) palsy.
- The oculomotor nerve is responsible for most other extraocular movements (adduction, elevation, depression).
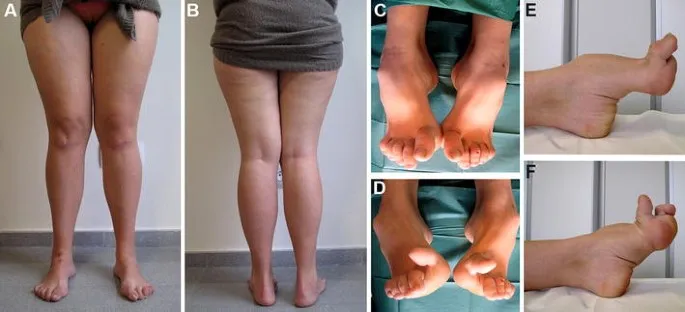
Peripheral nerve disorders US Medical PG Question 8: A 35-year-old man presents to the primary care office with a recent history of frequent falls. He had been able to walk normally until about a year ago when he started noticing that both of his legs felt weak. He's also had some trouble with feeling in his feet. These 2 problems have caused multiple falls over the last year. On physical exam, he has notable leg and foot muscular atrophy and 4/5 strength throughout his bilateral lower extremities. Sensation to light touch and pinprick is absent up to the mid-calf. Ankle jerk reflex is absent bilaterally. A photo of the patient's foot is shown. Which of the following best describes the etiology of this patient's condition?
- A. Metabolic
- B. Genetic (Correct Answer)
- C. Ischemic
- D. Autoimmune
- E. Infectious
Peripheral nerve disorders Explanation: ***Genetic***
- The combination of **progressive weakness and sensory deficits** starting in the distal extremities, **muscle atrophy**, absent ankle jerks, and the characteristic foot deformity (*pes cavus* and hammertoes, visible in the image) in a 35-year-old strongly suggests a hereditary neuropathy, most commonly **Charcot-Marie-Tooth disease (CMT)**.
- CMT is a group of inherited neurological disorders characterized by slowly progressive degeneration of peripheral nerves, leading to distal muscle weakness and sensory loss, and is the most prevalent inherited peripheral neuropathy.
*Metabolic*
- While metabolic conditions can cause neuropathy (e.g., **diabetes**), they typically present with a more classic "stocking-glove" distribution of sensory loss, and the characteristic foot deformities and progressive severe atrophy seen here are less typical as initial presentation without a clear history of underlying metabolic disease.
- Absence of other metabolic derangements, such as diabetes, thyroid dysfunction, or vitamin deficiencies, makes this less likely to be the primary cause.
*Ischemic*
- **Ischemic neuropathies** are usually acute, painful, and often associated with vascular risk factors or specific arterial occlusions, which are not described in this patient's chronic, bilateral, and symmetric presentation.
- There is no mention of claudication or other signs of vascular insufficiency.
*Autoimmune*
- **Autoimmune neuropathies** like **Guillain-Barré Syndrome (GBS)** or **Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP)** often have a more acute or subacute onset (GBS) or relapsing-remitting course (CIDP), and GBS typically presents with ascending weakness reaching a nadir and then improving, which is not consistent with this patient's chronic, progressive course.
- While CIDP can be chronic, the classic inherited foot deformities are not typically seen, and the pattern of nerve involvement might differ.
*Infectious*
- **Infectious neuropathies** (e.g., HIV, Lyme disease, leprosy) would typically have associated systemic symptoms, a different progression pattern, or specific exposures that are not mentioned in the patient's history.
- The chronic, slowly progressive nature with specific deformities makes a common infectious cause less likely compared to a genetic disorder.
Peripheral nerve disorders US Medical PG Question 9: A 44-year-old woman presents to her primary care physician’s office with episodes of pain in her right hand. She says that the pain is most significant at night and awakens her from sleep numerous times. When she experiences this pain, she immediately puts her hand under warm running water or shakes her hand. She has also experienced episodes of numbness in the affected hand. Driving and extending the right arm also provoke her symptoms. She denies any trauma to the hand or associated weakness. Medical history is notable for hypothyroidism treated with levothyroxine. She works as a secretary for a law firm. On physical exam, when the patient hyperflexes her wrist, pain and paresthesia affect the first 3 digits of the right hand. Which of the following is the confirmatory diagnostic test for this patient?
- A. Magnetic resonance imaging
- B. Needle electromyography
- C. Nerve conduction studies (Correct Answer)
- D. Nerve biopsy
- E. Tinel test
Peripheral nerve disorders Explanation: ***Nerve conduction studies***
- **Nerve conduction studies (NCS)** are the most sensitive and specific diagnostic test for **carpal tunnel syndrome**, definitively confirming median nerve compression.
- They measure the speed and amplitude of electrical signals through the **median nerve** at the wrist, identifying slowed conduction across the carpal tunnel.
*Magnetic resonance imaging*
- While MRI can visualize soft tissues and nerve pathology, it is not typically the **first-line confirmatory test** for carpal tunnel syndrome due to its lower sensitivity compared to NCS.
- MRI is more useful for identifying **structural abnormalities** like tumors or synovitis, which might cause secondary nerve compression.
*Needle electromyography*
- **Electromyography (EMG)** involves inserting a needle into muscles to assess their electrical activity; it helps evaluate for **axonopathy** and muscle denervation.
- While EMG is often performed alongside NCS, it primarily assesses muscle function and nerve damage severity, rather than directly confirming nerve compression itself, which is best done by NCS.
*Nerve biopsy*
- **Nerve biopsy** is an invasive procedure generally reserved for diagnosing demyelinating or infiltrative neuropathies when less invasive tests are inconclusive.
- It carries risks and is **unnecessary** and inappropriate for diagnosing a common compressive neuropathy like carpal tunnel syndrome.
*Tinel test*
- The **Tinel test** is a clinical provocative maneuver where percussion over the median nerve at the wrist elicits tingling or pain.
- It is a **screening tool** and part of the physical exam for carpal tunnel syndrome, but it is not a confirmatory diagnostic test due to its variable sensitivity and specificity.
Peripheral nerve disorders US Medical PG Question 10: An 8-year-old boy is brought to the pediatrician because his mother is concerned about recent behavioral changes. His mother states that she has started to notice that he is slurring his speech and seems to be falling more than normal. On exam, the pediatrician observes the boy has pes cavus, hammer toes, and kyphoscoliosis. Based on these findings, the pediatrician is concerned the child has a trinucleotide repeat disease. Which of the following trinucleotide repeats is this child most likely to possess?
- A. CTG
- B. GAA (Correct Answer)
- C. CGG
- D. CAG
- E. GCC
Peripheral nerve disorders Explanation: ***GAA***
- This trinucleotide repeat is associated with **Friedreich's ataxia**, an autosomal recessive neurodegenerative disorder.
- The presented symptoms of **ataxia** (slurred speech, falling), **pes cavus**, **hammer toes**, and **kyphoscoliosis** are classic features of Friedreich's ataxia.
*CTG*
- This trinucleotide repeat is associated with **myotonic dystrophy type 1**, an autosomal dominant disorder.
- While it causes muscle weakness, it is characterized by **myotonia** (delayed muscle relaxation), cataracts, and frontal baldness, which are not described here.
*CGG*
- This trinucleotide repeat is associated with **fragile X syndrome**, an X-linked dominant disorder.
- Fragile X syndrome primarily causes intellectual disability, behavioral issues (e.g., autism spectrum disorder), and characteristic facial features, but not the specific neurological and orthopedic findings seen in this patient.
*CAG*
- This trinucleotide repeat is associated with several neurodegenerative diseases, including **Huntington's disease**, spinocerebellar ataxias, and **dentatorubral-pallidoluysian atrophy**.
- Huntington's disease, for example, presents with chorea, cognitive decline, and psychiatric symptoms, differing from the patient's presentation.
*GCC*
- This trinucleotide repeat is associated with **fragile X-associated tremor/ataxia syndrome (FXTAS)**.
- FXTAS typically affects older adult carriers of premutation alleles for fragile X, presenting with intention tremor and gait ataxia, not the early childhood onset and specific orthopedic deformities seen here.
More Peripheral nerve disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.