Metastatic CNS tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Metastatic CNS tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Metastatic CNS tumors US Medical PG Question 1: A 57-year-old man is brought to the emergency department by his wife 20 minutes after having had a seizure. He has had recurrent headaches and dizziness for the past 2 weeks. An MRI of the brain shows multiple, round, well-demarcated lesions in the brain parenchyma at the junction between gray and white matter. This patient's brain lesions are most likely comprised of cells that originate from which of the following organs?
- A. Kidney
- B. Skin
- C. Lung (Correct Answer)
- D. Thyroid
- E. Prostate
Metastatic CNS tumors Explanation: ***Lung (Correct Answer)***
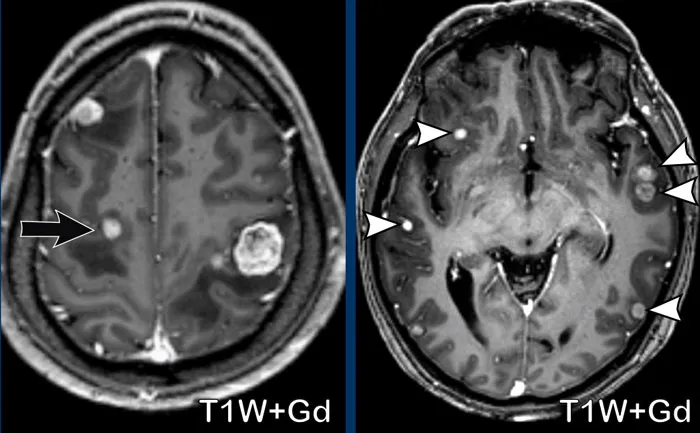
- **Lung cancer** is the most common cause of **brain metastases** in adults, accounting for approximately **50% of all cases**
- The clinical presentation—seizure, headaches, dizziness, and **multiple, round, well-demarcated lesions at the gray-white matter junction**—is classic for metastatic lung cancer
- Both **small cell and non-small cell lung cancers** have high propensity for hematogenous spread to the brain
- The watershed areas at the gray-white junction are common sites due to lodging of tumor emboli in terminal arterioles
*Kidney (Incorrect)*
- **Renal cell carcinoma (RCC)** can metastasize to the brain but accounts for only **5-10% of brain metastases**
- While RCC metastases can appear similar on imaging, lung cancer is statistically more likely given its higher prevalence
- RCC metastases are often **highly vascular and may hemorrhage**, which is not mentioned in this case
*Skin (Incorrect)*
- **Melanoma** has the **highest propensity per case** to metastasize to the brain among all cancers
- However, the **overall incidence of melanoma is much lower** than lung cancer, making it a less probable primary source
- Melanoma brain metastases often present as **hemorrhagic lesions** and would typically have skin findings or history
*Thyroid (Incorrect)*
- **Thyroid cancer** rarely metastasizes to the brain (accounts for <1% of brain metastases)
- Brain metastases from thyroid cancer typically occur in **advanced papillary or follicular carcinoma** or in **anaplastic thyroid cancer**
- More common metastatic sites for thyroid cancer are lung and bone
*Prostate (Incorrect)*
- **Prostate cancer very rarely metastasizes to the brain** (<1% of cases)
- Prostate cancer preferentially metastasizes to **bone (especially axial skeleton), lymph nodes, and liver**
- Brain metastases from prostate cancer suggest extremely advanced, aggressive disease and are exceptionally uncommon
Metastatic CNS tumors US Medical PG Question 2: A previously healthy 50-year-old woman is brought to the emergency department 30 minutes after she was observed having a seizure. On arrival, she is conscious and reports that she feels drowsy. An MRI of the brain shows a 4-cm, round, sharply demarcated mass. She undergoes resection of the mass. A photomicrograph of a section of the resected specimen is shown. This patient's mass is most likely derived from which of the following?
- A. Neurons
- B. Arachnoid cells (Correct Answer)
- C. Schwann cells
- D. Oligodendrocytes
- E. Astrocytes
Metastatic CNS tumors Explanation: ***Arachnoid cells***
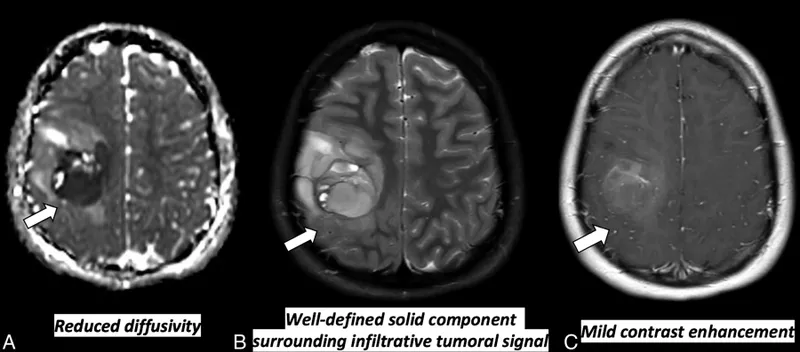
- The description of a **round, sharply demarcated mass** in an adult, often presenting with seizures, is highly characteristic of a **meningioma**.
- Meningiomas are **benign tumors** that arise from the meninges, specifically the **arachnoid cap cells** (meningothelial cells).
- These tumors are typically **well-circumscribed**, extra-axial masses that compress adjacent brain tissue.
*Neurons*
- Tumors derived from neurons, such as **gangliogliomas** or **central neurocytomas**, are less common and typically do not present as sharply demarcated masses in this location.
- While neurons are the primary functional cells of the brain, most primary brain tumors arise from **glial or mesenchymal cells**, not neurons themselves.
*Schwann cells*
- Tumors of Schwann cells are known as **schwannomas** (or acoustic neuromas if arising from cranial nerves).
- Schwannomas typically occur along **cranial nerves** (especially CN VIII) in the cerebellopontine angle, presenting with hearing loss or balance issues, which is not described here.
*Oligodendrocytes*
- Tumors originating from oligodendrocytes are **oligodendrogliomas**, which are typically **infiltrative glial tumors** rather than sharply demarcated masses.
- They often present with calcifications ("fried egg" appearance on histology) and have a different appearance, not matching the classic presentation of a benign, encapsulated mass.
*Astrocytes*
- Astrocytes give rise to various **astrocytomas** (e.g., glioblastoma, pilocytic astrocytoma), which are generally **infiltrative** and poorly demarcated.
- While they can present with seizures, their typical MRI appearance and histological features differ from the described well-circumscribed mass.
Metastatic CNS tumors US Medical PG Question 3: A 39-year-old African American woman is admitted to the hospital following a seizure with a severe post-ictal headache. She was diagnosed with breast cancer 1 year ago when she presented with a hard, rock-like, immobile mass with irregular borders accompanied by changes in the breast skin, including erythema and dimpling. She had ipsilateral mobile axillary lymphadenopathy at that time. A biopsy confirmed the diagnosis of stage 2B invasive breast cancer. Her mother died at 42 years of age due to the same type of breast cancer. A CT scan done during this admission reveals multiple metastatic lesions in the brain and liver, along with the involvement of supra- and infra-clavicular lymph nodes. Which of the following molecular profile most likely characterizes this patient?
- A. PR, ER, HER2 positive
- B. HER2 positive
- C. Progesterone receptor (PR) positive
- D. ER, PR, HER2 negative (Correct Answer)
- E. Estrogen receptor (ER) positive
Metastatic CNS tumors Explanation: ***ER, PR, HER2 negative***
- This patient's presentation with aggressive breast cancer at a relatively young age (39 years old), family history of early-onset breast cancer, rapid progression to metastatic disease in the brain and liver, and involvement of multiple lymph nodes (axillary, supra- and infra-clavicular) are all highly suggestive of a **triple-negative breast cancer (TNBC)**.
- TNBC is characterized by the absence of **estrogen receptors (ER)**, **progesterone receptors (PR)**, and **human epidermal growth factor receptor 2 (HER2)** overexpression, making it an aggressive subtype with limited targeted treatment options and a poor prognosis, consistent with the patient's rapidly worsening condition.
*PR, ER, HER2 positive*
- This molecular profile (also known as triple-positive breast cancer) generally indicates a more favorable prognosis due to the availability of **hormonal therapy** (for ER/PR positivity) and **anti-HER2 targeted therapy**.
- The aggressive course and rapid metastatic spread described in the patient are less typical for triple-positive disease, which often responds well to various targeted treatments.
*HER2 positive*
- HER2-positive breast cancer can be aggressive, but the presence of HER2 positivity allows for **HER2-targeted therapies** (e.g., trastuzumab, pertuzumab), which significantly improve outcomes.
- While HER2-positive cancers can metastasize to the brain, the overall clinical picture, especially the aggressive growth and lack of other receptor expression, aligns more with triple-negative disease.
*Progesterone receptor (PR) positive*
- PR positivity, often alongside ER positivity, indicates a **hormone-sensitive breast cancer**, which typically has a better prognosis and is amenable to **endocrine therapy**.
- The aggressive and rapid metastatic progression to multiple sites, including brain and liver, is not characteristic of a purely PR-positive tumor without other aggressive features.
*Estrogen receptor (ER) positive*
- ER-positive breast cancer is the most common subtype and is generally associated with a **better prognosis** and responsiveness to **endocrine therapy**.
- The patient's aggressive disease course, including early metastasis and family history of early-onset, aggressive breast cancer, does not align with the typical presentation of an exclusively ER-positive tumor.
Metastatic CNS tumors US Medical PG Question 4: A 22-year-old man comes to the physician because of headaches and blurry vision for the past 6 months. He also reports frequent episodes of vomiting over the last month. His father has died of renal cell carcinoma at the age of 37 years. Examination shows 20/40 vision bilaterally. Fundoscopic examination shows bilateral optic disc swelling and growth of capillary vessels in the temporal peripheral retina. An MRI of the brain shows an infratentorial mass. The patient undergoes surgical resection of the mass. A photomicrograph of the resected specimen is shown. Which of the following is the most likely diagnosis?
- A. Hemangioblastoma (Correct Answer)
- B. Medulloblastoma
- C. Glioblastoma
- D. Oligodendroglioma
- E. Ependymoma
Metastatic CNS tumors Explanation: ***Hemangioblastoma***
- The patient's presentation with an **infratentorial mass** causing headaches, blurry vision, and vomiting, combined with **retinal hemangiomas** (growth of capillary vessels in the temporal peripheral retina) and a family history of **renal cell carcinoma** (especially at a young age), is highly suggestive of **Von Hippel-Lindau (VHL) disease**. Hemangioblastomas are the most common CNS tumors in VHL disease and are typically found in the cerebellum, brainstem, or spinal cord.
- The photomicrograph would typically show characteristic foamy **stromal cells** with high vascularity, which are hallmarks of a hemangioblastoma.
*Medulloblastoma*
- This is a common **malignant cerebellar tumor** in children, but it typically presents in younger individuals (ages 3-8) and is less common in adults.
- While it can cause similar symptoms due to an infratentorial mass, it is not associated with **retinal hemangiomas** or **renal cell carcinoma** in the family history.
*Glioblastoma*
- Glioblastoma is a highly aggressive **supratentorial tumor** (located above the tentorium cerebelli), primarily affecting the cerebral hemispheres in older adults.
- It is uncommon in the cerebellum of young adults and does not typically present with the retinal findings or the characteristic family history seen in this case.
*Oligodendroglioma*
- Oligodendrogliomas are typically **supratentorial tumors** of the cerebral hemispheres, commonly found in the frontal lobe, and are not usually associated with retinal hemangiomas or a family history of renal cell carcinoma.
- Histologically, they are characterized by cells with clear halos (**"fried egg" appearance**) and a delicate capillary network, which would not match the expected photomicrograph features of this case.
*Ependymoma*
- Ependymomas can occur in the **fourth ventricle** (an infratentorial location), especially in children and young adults, and can cause hydrocephalus and associated symptoms.
- However, they are not typically associated with **retinal hemangiomas** or a family history of **renal cell carcinoma**, which are strong indicators of VHL disease and hemangioblastoma.
Metastatic CNS tumors US Medical PG Question 5: A 22-year-old woman comes to the physician because of hearing loss and unsteadiness while standing and walking for the past 2 months. She needs support from a wall to prevent herself from falling. She has not had any recent injuries and has no history of serious illness. Vital signs are within normal limits. Examination shows an unsteady gait. She sways when asked to stand upright with her feet together. She is unable to hear fingers rubbing next to her ears or repeat words whispered in her ears bilaterally. An MRI of the brain shows a 3-cm tumor in the right cerebellopontine angle and a 4.5-cm tumor in the left cerebellopontine angle. This patient is most likely to develop which of the following in the future?
- A. Renal cell carcinoma
- B. Telangiectasias
- C. Optic glioma
- D. Meningioma (Correct Answer)
- E. Astrocytoma
Metastatic CNS tumors Explanation: ***Meningioma***
- This patient's bilateral **vestibular schwannomas** (tumors in the **cerebellopontine angle** causing hearing loss and unsteadiness) are highly suggestive of **Neurofibromatosis type 2 (NF2)**.
- Patients with NF2 are predisposed to developing multiple central nervous system tumors, with **meningiomas** being a common manifestation, alongside schwannomas and ependymomas.
*Renal cell carcinoma*
- This is not typically associated with **Neurofibromatosis type 2**, which primarily involves tumors of the nervous system.
- While various cancer syndromes exist, NF2 does not significantly increase the risk of **renal cell carcinoma**.
*Telangiectasias*
- **Telangiectasias** are dilated small blood vessels, often associated with conditions like **hereditary hemorrhagic telangiectasia** or **ataxia-telangiectasia**.
- They are not a characteristic feature or complication of **Neurofibromatosis type 2**.
*Optic glioma*
- **Optic gliomas** are a hallmark feature of **Neurofibromatosis type 1 (NF1)**, not NF2.
- NF1 is also associated with **café-au-lait spots** and **Lisch nodules**, which are distinct from the presentation of bilateral vestibular schwannomas.
*Astrocytoma*
- While NF2 patients can develop central nervous system tumors, **astrocytomas** are less common than **ependymomas** or **meningiomas** in this syndrome.
- The most characteristic brain tumors in NF2 are **vestibular schwannomas** and **meningiomas**.
Metastatic CNS tumors US Medical PG Question 6: A 55-year-old female presents to her primary care physician complaining of a mass in her mid-thigh. The mass has grown slowly over the past six months and is not painful. The patient’s past medical history is notable for hypertension and hyperlipidemia. She takes lisinopril and rosuvastatin. On examination, there is a firm, immobile mass on the medial aspect of the distal thigh. She has full range of motion and strength in her lower extremities and patellar reflexes are 2+ bilaterally. A biopsy of the mass reveals multiple pleomorphic smooth muscle cells with nuclear atypia. The patient subsequently initiates radiation therapy with plans to undergo surgical resection. This tumor will most strongly stain for which of the following?
- A. Cytokeratin
- B. Desmin (Correct Answer)
- C. Chromogranin
- D. Neurofilament
- E. Glial fibrillary acidic protein
Metastatic CNS tumors Explanation: ***Desmin***
- The biopsy results describe **pleomorphic smooth muscle cells with nuclear atypia**, which is characteristic of a **leiomyosarcoma**, a malignant tumor derived from smooth muscle.
- **Desmin** is a muscle-specific intermediate filament that is strongly positive in tumors of smooth muscle origin, including leiomyosarcomas, making it the most appropriate stain for diagnosis.
*Cytokeratin*
- **Cytokeratin** is an intermediate filament protein found in **epithelial cells** and is a marker for carcinomas.
- Leiomyosarcomas are mesenchymal tumors, so they would typically be **negative for cytokeratin**.
*Chromogranin*
- **Chromogranin** is a marker for **neuroendocrine tumors**, such as carcinoids and pheochromocytomas.
- This tumor's histological features and derivation from smooth muscle rule out a neuroendocrine origin.
*Neurofilament*
- **Neurofilament** proteins are found in **neurons** and are markers for tumors of neural origin, such as neuroblastomas or schwannomas.
- The presented tumor is of mesenchymal origin, not neural.
*Glial fibrillary acidic protein*
- **Glial fibrillary acidic protein (GFAP)** is an intermediate filament found in **astrocytes** and is a marker for glial tumors, such as astrocytomas and glioblastomas, which originate in the central nervous system.
- A thigh mass is not consistent with a glial tumor.
Metastatic CNS tumors US Medical PG Question 7: A 34-year-old man comes to the physician because of a 3-week history of left testicular swelling. He has no pain. He underwent a left inguinal hernia repair as a child. He takes no medications. He appears healthy. His vital signs are within normal limits. Examination shows an enlarged, nontender left testicle. When the patient is asked to cough, there is no bulge present in the scrotum. When a light is held behind the scrotum, it does not shine through. There is no inguinal lymphadenopathy. Laboratory studies show:
Hemoglobin 14.5 g/dL
Leukocyte count 8,800/mm3
Platelet count 345,000/mm3
Serum
Glucose 88 mg/dL
Creatinine 0.8 mg/dL
Total bilirubin 0.7 mg/dL
Alkaline phosphatase 35 U/L
AST 15 U/L
ALT 14 U/L
Lactate dehydrogenase 60 U/L
β-Human chorionic gonadotropin 80 mIU/mL (N < 5)
α-Fetoprotein 6 ng/mL (N < 10)
Which of the following is the most likely diagnosis?
- A. Seminoma (Correct Answer)
- B. Leydig cell tumor
- C. Choriocarcinoma
- D. Spermatocele of testis
- E. Yolk sac tumor
Metastatic CNS tumors Explanation: **Seminoma**
- The elevated **beta-human chorionic gonadotropin (β-hCG)** in the presence of a normal alpha-fetoprotein (α-FP) is highly suggestive of seminoma, especially in a painless testicular mass in a young man.
- While AFP is typically not elevated in pure seminomas, β-hCG can be mildly to moderately elevated in approximately 10-30% of cases, consistent with this presentation.
*Leydig cell tumor*
- These tumors often produce androgens or estrogens, leading to symptoms like **precocious puberty** in boys or **gynecomastia** in adult men, which are not described.
- Serum tumor markers like β-hCG and α-FP are typically **not elevated** in Leydig cell tumors.
*Choriocarcinoma*
- This highly aggressive germ cell tumor is characterized by **markedly elevated β-hCG levels**, often much higher than 80 mIU/mL, and can also elevate α-FP.
- Given the relatively mild β-hCG elevation and normal α-FP, choriocarcinoma is less likely.
*Spermatocele of testis*
- A spermatocele is a **benign cyst** that typically transilluminates (light shines through), which is absent in this case.
- Tumor markers like β-hCG and α-FP would be **normal** in a spermatocele, ruling it out.
*Yolk sac tumor*
- Yolk sac tumors are characterized by **elevated alpha-fetoprotein (α-FP)** levels, which are normal in this patient.
- While they can also elevate β-hCG in some cases, the defining marker, α-FP, is not elevated here.
Metastatic CNS tumors US Medical PG Question 8: A 52-year-old man presents with 2 months of diarrhea, abdominal pain, and fatigue. He reports a weight loss of 4 kg (8 lb). He also says his joints have been hurting recently, as well. Past medical history is unremarkable. Review of systems is significant for problems with concentration and memory. Physical examination is unremarkable. A GI endoscopy is performed with a biopsy of the small bowel. Which of the following histologic finding would most likely be seen in this patient?
- A. PAS positive macrophages (Correct Answer)
- B. Non-caseating granulomas in the small intestine
- C. Absence of nerves in the myenteric plexus
- D. Blunting of the villi
- E. Crypt hyperplasia with increased intraepithelial lymphocytes
Metastatic CNS tumors Explanation: **PAS positive macrophages**
- The clinical presentation with **diarrhea**, abdominal pain, weight loss, joint pain, and **neurological symptoms** (problems with concentration and memory) is classic for **Whipple's disease**.
- **Whipple's disease** is caused by the bacterium **Tropheryma whipplei**, which is characterized histologically by **foamy macrophages** in the lamina propria that stain **positive with Periodic Acid-Schiff (PAS)** due to undigested bacterial cell wall material.
*Non-caseating granulomas in the small intestine*
- **Non-caseating granulomas** are characteristic of **Crohn's disease**, which typically presents with abdominal pain, diarrhea, and weight loss, but **neurological symptoms** are not a primary feature.
- While Crohn's disease can cause joint pain (arthritis), the combination of GI and neurological symptoms points away from it.
*Absence of nerves in the myenteric plexus*
- An **absence of nerves in the myenteric plexus** is the hallmark of **Hirschsprung's disease**, which is a congenital disorder primarily affecting neonates and infants, causing intestinal obstruction and chronic constipation.
- This finding is inconsistent with the patient's age and presenting symptoms of diarrhea and neurological issues.
*Blunting of the villi*
- **Villi blunting** is characteristic of **celiac disease** (gluten-sensitive enteropathy), which presents with malabsorption symptoms like diarrhea, weight loss, and abdominal pain.
- However, **celiac disease** typically does not involve **neurological symptoms** like concentration and memory problems as a prominent feature, and the PAS-positive macrophages are specific to Whipple's.
*Crypt hyperplasia with increased intraepithelial lymphocytes*
- **Crypt hyperplasia** and **increased intraepithelial lymphocytes (IELs)** are seen in various small bowel pathologies, including **celiac disease** and **microscopic colitis**.
- While these findings suggest intestinal inflammation, they are not specific to **Whipple's disease** and do not account for the characteristic neurological involvement.
Metastatic CNS tumors US Medical PG Question 9: A 38-year-old woman comes to the physician for a 3-month history of bloody discharge from the right nipple. Her mother died of breast cancer at the age of 69 years. Mammography 6 months ago did not show any abnormalities. Examination of the breast shows expression of a small amount of serosanguinous fluid from the right nipple; there are no palpable breast masses or axillary lymphadenopathy. Ultrasonography of the right breast shows a single dilated duct. Which of the following is the most likely diagnosis?
- A. Invasive ductal carcinoma
- B. Paget disease of the breast
- C. Phyllodes tumor
- D. Breast lipoma
- E. Intraductal papilloma (Correct Answer)
Metastatic CNS tumors Explanation: ***Intraductal papilloma***
- This lesion typically presents with **bloody or serosanguinous nipple discharge** from a single duct, as described in the patient.
- It is a **benign proliferative lesion** that grows within a major lactiferous duct, often leading to ductal dilatation on ultrasound, without a palpable mass or suspicious mammographic findings.
*Invasive ductal carcinoma*
- While it can cause bloody nipple discharge, it is more commonly associated with a **palpable mass**, skin changes, or abnormal findings on mammography.
- The absence of a palpable mass, normal mammogram 6 months prior, and isolated ductal dilatation on ultrasound make it less likely in this scenario.
*Paget disease of the breast*
- This condition presents as an **eczematous lesion of the nipple and areola**, often with itching, scaling, and ulceration.
- While it can be associated with an underlying invasive or in situ carcinoma, the primary presenting symptom is skin changes, not solely nipple discharge in a seemingly normal breast.
*Phyllodes tumor*
- These are **biphasic fibroepithelial tumors** that typically present as a rapidly growing, palpable breast mass.
- They do not characteristically present with isolated nipple discharge, especially without any palpable mass.
*Breast lipoma*
- A breast lipoma is a **benign fatty tumor** that presents as a soft, mobile, non-tender lump.
- It does not cause nipple discharge and is usually easily identifiable on imaging as a fatty lesion.
Metastatic CNS tumors US Medical PG Question 10: A 35-year-old woman presents with headaches and seizures. MRI shows a well-circumscribed, calcified frontal lobe mass. Histology reveals oligodendroglioma with 1p/19q codeletion and IDH1 mutation. She undergoes gross total resection. Two years later, surveillance MRI shows a new enhancing nodule at the resection margin. Biopsy shows increased mitotic activity, microvascular proliferation, and retained 1p/19q codeletion but new CDKN2A/B homozygous deletion. What is the most critical factor in determining management strategy?
- A. The tumor has progressed to anaplastic oligodendroglioma requiring combined chemoradiation with temozolomide and RT
- B. CDKN2A/B deletion indicates transformation to glioblastoma requiring maximal therapy
- C. Retained 1p/19q codeletion predicts continued chemosensitivity to PCV regimen (Correct Answer)
- D. Loss of IDH1 mutation suggests new primary tumor requiring re-resection only
- E. Microvascular proliferation mandates anti-angiogenic therapy with bevacizumab
Metastatic CNS tumors Explanation: ***Retained 1p/19q codeletion predicts continued chemosensitivity to PCV regimen***
- The preservation of **1p/19q codeletion** in a recurrent tumor is the strongest predictor of clinical response to alkylating chemotherapy, specifically the **PCV (Procarbazine, Lomustine, Vincristine)** regimen.
- While the tumor shows histological progression, the underlying molecular subtype remains an **oligodendroglioma**, which generally carries a better prognosis and higher chemosensitivity than non-codeleted gliomas.
*The tumor has progressed to anaplastic oligodendroglioma requiring combined chemoradiation with temozolomide and RT*
- While the histology suggests a higher grade, the standard of care for 1p/19q codeleted tumors frequently favors **PCV** over **Temozolomide** due to more robust long-term survival data from clinical trials like RTOG 9402.
- Grading alone does not dictate management as much as the **molecular profile** does in modern neuro-oncology guidelines.
*CDKN2A/B deletion indicates transformation to glioblastoma requiring maximal therapy*
- Under the current WHO classification, **glioblastoma** is defined as an **IDH-wildtype** tumor; since this tumor has an **IDH1 mutation**, it cannot be classified as a glioblastoma.
- **CDKN2A/B homozygous deletion** is a marker of high-grade malignancy (WHO Grade 4) in IDH-mutant astrocytomas, but its presence in an **oligodendroglioma** does not change the lineage-defining 1p/19q status.
*Loss of IDH1 mutation suggests new primary tumor requiring re-resection only*
- **IDH1 mutations** are early, trunk events in gliomagenesis and are almost never
More Metastatic CNS tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.