CNS trauma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for CNS trauma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
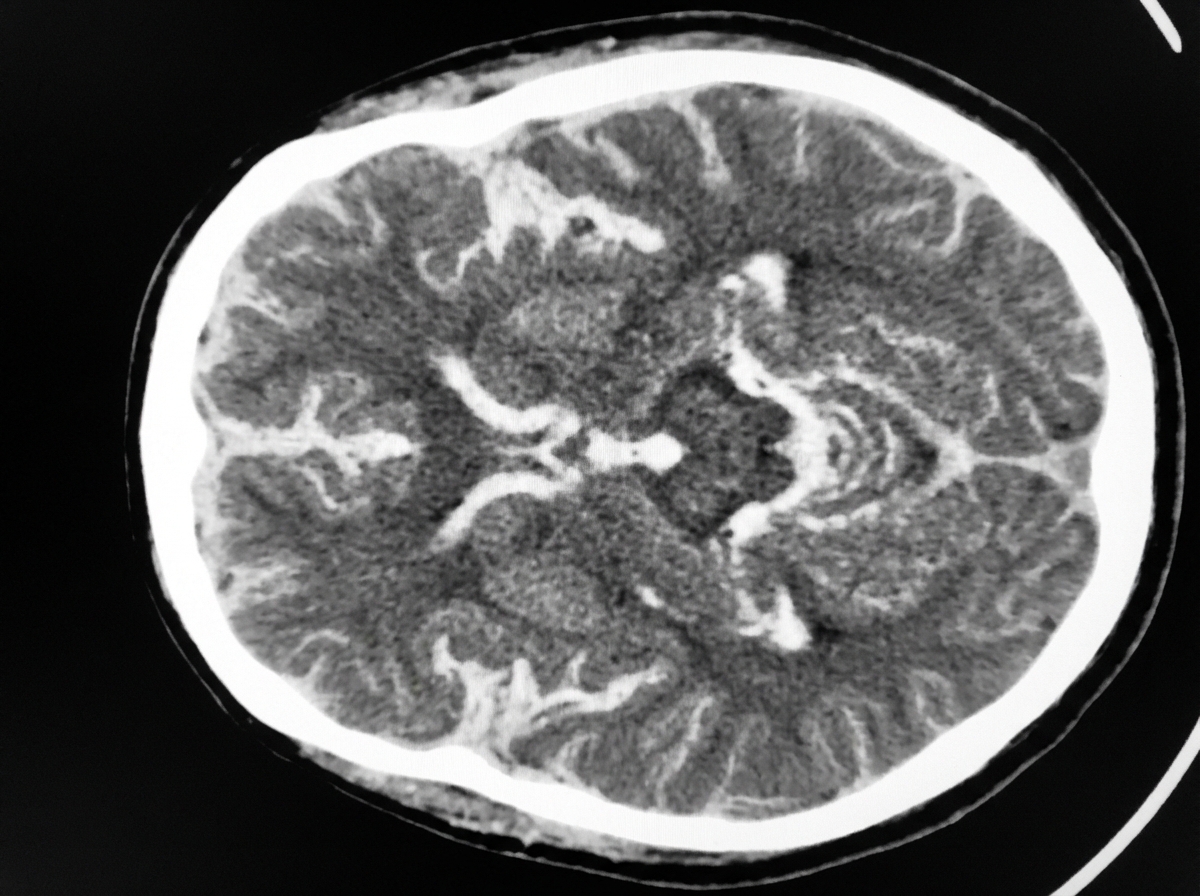
CNS trauma US Medical PG Question 1: A 54-year-old man is brought to the emergency department 30 minutes after being hit by a car while crossing the street. He had a left-sided tonic-clonic seizure and one episode of vomiting while being transported to the hospital. On arrival, he is not oriented to person, place, or time. Physical examination shows flaccid paralysis of all extremities. A CT scan of the head is shown. This patient's symptoms are most likely the result of a hemorrhage in which of the following structures?
- A. Between the dura mater and the arachnoid mater
- B. Into the cerebral parenchyma
- C. Between the skull and the dura mater
- D. Between the arachnoid mater and the pia mater (Correct Answer)
- E. Into the ventricular system
CNS trauma Explanation: ***Between the arachnoid mater and the pia mater (Correct)***
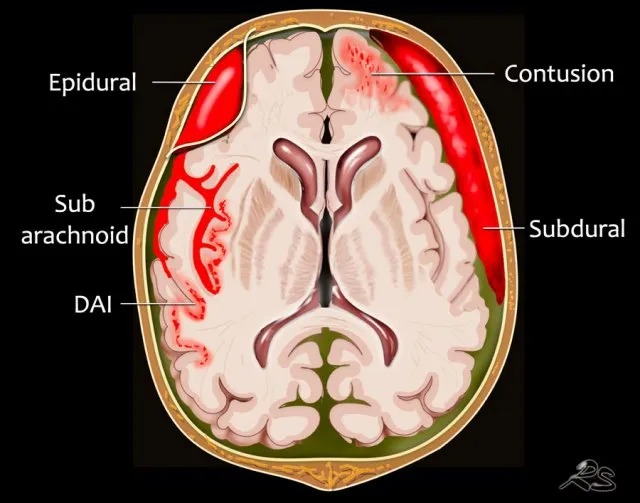
- The CT scan demonstrates diffuse high-density (white) material within the sulci and basal cisterns, indicative of a **subarachnoid hemorrhage**. This space is located between the arachnoid mater and the pia mater.
- The patient's presentation with altered mental status, seizures, vomiting, and flaccid paralysis following trauma is consistent with the severe neurological impact of a **traumatic subarachnoid hemorrhage**.
*Between the dura mater and the arachnoid mater (Incorrect)*
- Hemorrhage in this location is known as a **subdural hematoma**, which typically appears as a crescent-shaped collection of blood.
- While possible in trauma, the CT image shows blood primarily filling the sulci, not a subdural collection.
*Into the cerebral parenchyma (Incorrect)*
- This would be an **intraparenchymal hemorrhage**, appearing as a focal area of high density within the brain tissue itself.
- Although there might be some associated parenchymal injury in severe trauma, the predominant pattern seen on the CT is diffuse blood in the subarachnoid space.
*Between the skull and the dura mater (Incorrect)*
- This describes an **epidural hematoma**, often characterized by a lenticular (lens-shaped) collection of blood due to its confinement by dural attachments.
- The CT image does not show a lenticular collection of blood in this space.
*Into the ventricular system (Incorrect)*
- **Intraventricular hemorrhage** would show blood filling the cerebral ventricles.
- While subarachnoid hemorrhage can sometimes extend into the ventricles, the primary finding on this CT is diffuse blood in the subarachnoid space, not isolated ventricular blood.
CNS trauma US Medical PG Question 2: A 15-year-old boy is brought to the emergency department one hour after sustaining an injury during football practice. He collided head-on into another player while wearing a mouthguard and helmet. Immediately after the collision he was confused but able to use appropriate words. He opened his eyes spontaneously and followed commands. There was no loss of consciousness. He also had a headache with dizziness and nausea. He is no longer confused upon arrival. He feels well. Vital signs are within normal limits. He is fully alert and oriented. His speech is organized and he is able to perform tasks demonstrating full attention, memory, and balance. Neurological examination shows no abnormalities. There is mild tenderness to palpation over the crown of his head but no signs of skin break or fracture. Which of the following is the most appropriate next step?
- A. Discharge without activity restrictions
- B. Discharge and refrain from all physical activity for one week
- C. Observe for 6 hours in the ED and refrain from contact sports for one week (Correct Answer)
- D. Administer prophylactic levetiracetam and observe for 24 hours
- E. Administer prophylactic phenytoin and observe for 24 hours
CNS trauma Explanation: ***Observe for 6 hours in the ED and refrain from contact sports for one week***
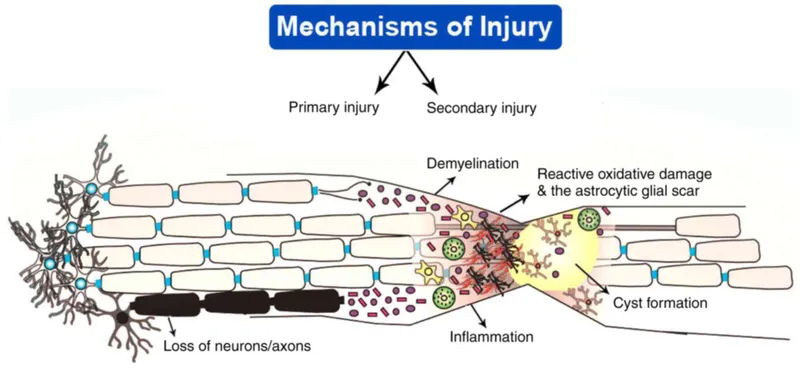
- This patient experienced a brief period of **confusion, headache, dizziness**, and **nausea** immediately after a head injury, which are symptoms consistent with a **mild traumatic brain injury (mTBI)** or **concussion**.
- Although his symptoms have resolved at presentation, observation in the ED for a few hours is prudent to ensure no delayed onset of more severe symptoms, and he should **refrain from contact sports** for at least one week as part of concussion management.
*Discharge without activity restrictions*
- Discharging without activity restrictions is unsafe given the initial symptoms of **confusion** and the potential for delayed symptom presentation or complications from a concussion.
- Concussion management requires a period of **physical and cognitive rest** to allow the brain to heal and prevent **second impact syndrome**.
*Discharge and refrain from all physical activity for one week*
- While refraining from all physical activity for one week is part of concussion management, discharging immediately without any observation period after initial neurological symptoms could be risky.
- An observation period allows for monitoring of any **worsening neurological signs** or symptoms that might indicate a more serious injury.
*Administer prophylactic levetiracetam and observe for 24 hours*
- **Prophylactic anticonvulsants** like levetiracetam are typically not recommended for routine management of **mild traumatic brain injury** or concussion.
- Their use is generally reserved for patients with more severe injuries, evolving conditions, or those who have had **seizures post-trauma**.
*Administer prophylactic phenytoin and observe for 24 hours*
- Similar to levetiracetam, **phenytoin** is an anticonvulsant and its prophylactic use is not indicated for **mild head injuries** or concussions.
- Anticonvulsant prophylaxis is associated with potential side effects and is reserved for specific high-risk scenarios, such as **severe TBI** or **penetrating head trauma**.
CNS trauma US Medical PG Question 3: A 4-month-old infant is brought to the emergency department with seizures. CT scan reveals bilateral subdural hematomas of different ages and retinal hemorrhages. Which of the following mechanisms best explains these findings?
- A. Infectious meningitis
- B. Acceleration-deceleration forces (Correct Answer)
- C. Birth trauma
- D. Genetic coagulopathy
- E. Direct impact trauma
CNS trauma Explanation: ***Acceleration-deceleration forces***
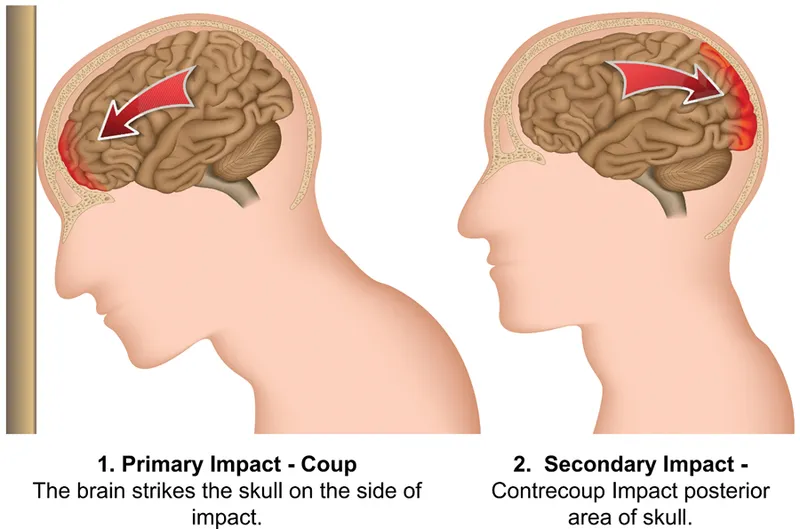
- **Bilateral subdural hematomas of different ages** and **retinal hemorrhages** are classic findings in **abusive head trauma (shaken baby syndrome)**, caused by severe acceleration-deceleration forces.
- These forces lead to the tearing of **bridging veins** and vitreoretinal traction, resulting in these distinct injuries.
*Infectious meningitis*
- While it can cause seizures, meningitis typically presents with **fever**, **lethargy**, and neck stiffness, and would not cause **subdural hematomas** or **retinal hemorrhages**.
- Its effects on the brain are usually due to inflammation and increased intracranial pressure, not traumatic injury.
*Birth trauma*
- **Birth trauma** might cause subdural hematomas, but they would typically be **acute** and of a **single age**, directly related to the birthing process.
- It is highly unlikely to cause hematomas of "different ages" in a 4-month-old infant, nor would it characteristically cause retinal hemorrhages without other signs of severe, acute trauma.
*Genetic coagulopathy*
- A **genetic coagulopathy** could predispose to bleeding, but it would typically result in more widespread or spontaneous internal bleeding, not specifically **bilateral subdural hematomas** accompanied by **retinal hemorrhages** without other trauma.
- The "different ages" of the hematomas also strongly suggest recurrent episodes of trauma rather than an underlying bleeding disorder.
CNS trauma US Medical PG Question 4: A 38-year-old man comes to the physician for a follow-up examination. He has quadriparesis as a result of a burst fracture of the cervical spine that occurred after a fall from his roof 1 month ago. He has urinary and bowel incontinence. He appears malnourished. His temperature is 37.1°C (98.8°F), pulse is 88/min, and blood pressure is 104/60 mm Hg. Examination shows spasticity in all extremities. Muscle strength is decreased in proximal and distal muscle groups bilaterally. Deep tendon reflexes are 4+ bilaterally. Plantar reflex shows extensor response bilaterally. Sensation to pinprick and temperature is absent below the neck. Sensation to vibration, position, and light touch is normal bilaterally. Rectal tone is decreased. There is a 1-cm area of erythema over the sacrum. Which of the following is the most likely cause of this patient's symptoms?
- A. Hemi-transection of the spinal cord
- B. Cavitation within the spinal cord
- C. Injury to gray matter of the spinal cord
- D. Occlusion of the posterior spinal artery
- E. Damage to the anterior spinal artery (Correct Answer)
CNS trauma Explanation: ***Damage to the anterior spinal artery***
- This typically results in **anterior cord syndrome**, characterized by bilateral loss of pain and temperature sensation, motor function (quadriparesis), and autonomic dysfunction (bowel/bladder incontinence below the level of injury).
- The **preservation of posterior column functions** (vibration, proprioception, light touch) is a hallmark of anterior spinal artery ischemia, as the posterior columns are supplied by the posterior spinal arteries.
*Hemi-transection of the spinal cord*
- This describes **Brown-Séquard syndrome**, which involves ipsilateral loss of motor function, vibration, and proprioception, and contralateral loss of pain and temperature sensation.
- The patient's symptoms are inconsistent with Brown-Séquard syndrome due to the **bilateral presentation of motor and sensory deficits**.
*Cavitation within the spinal cord*
- This condition, known as **syringomyelia**, typically presents with a **cape-like distribution of pain and temperature loss** (due to central cord involvement affecting the decussating spinothalamic fibers).
- It would usually spare motor function initially and would not explain the sudden, severe quadriparesis and complete sensory loss described.
*Injury to gray matter of the spinal cord*
- Isolated gray matter injury, often seen in conditions like **central cord syndrome**, primarily affects the pain and temperature pathways and may cause upper extremity weakness.
- It would not explain the **complete loss of motor function and pain/temperature sensation below the neck** while preserving posterior column function.
*Occlusion of the posterior spinal artery*
- Occlusion of the posterior spinal artery would primarily affect the **dorsal columns**, leading to loss of vibration, proprioception, and light touch.
- This patient, however, has **preserved sensation to vibration, position, and light touch**, making posterior spinal artery occlusion unlikely.
CNS trauma US Medical PG Question 5: A 2-month-old boy is brought to the emergency room by his mother who reports he has appeared lethargic for the past 3 hours. She reports that she left the patient with a new nanny this morning, and he was behaving normally. When she got home in the afternoon, the patient seemed lethargic and would not breastfeed as usual. At birth, the child had an Apgar score of 8/9 and weighed 2.8 kg (6.1 lb). Growth has been in the 90th percentile, and the patient has been meeting all developmental milestones. There is no significant past medical history, and vaccinations are up-to-date. On physical examination, the patient does not seem arousable. Ophthalmologic examination shows retinal hemorrhages. Which of the following findings would most likely be expected on a noncontrast CT scan of the head?
- A. Lens-shaped hematoma
- B. Cortical atrophy
- C. Crescent-shaped hematoma (Correct Answer)
- D. Blood in the basal cisterns
- E. Multiple cortical and subcortical infarcts
CNS trauma Explanation: ***Crescent-shaped hematoma***
- The clinical presentation with **lethargy**, a history of being with a **new caregiver**, and **retinal hemorrhages** strongly suggests **abusive head trauma** (shaken baby syndrome).
- This typically results in a **subdural hematoma**, which appears as a **crescent-shaped collection of blood** on a noncontrast CT scan, reflecting bleeding into the potential space between the dura mater and arachnoid mater.
*Lens-shaped hematoma*
- A **lens-shaped (biconvex) hematoma** on CT is characteristic of an **epidural hematoma**, which typically results from a **skull fracture** tearing a meningeal artery.
- While head trauma is present, the specific findings (retinal hemorrhages, lack of skull fracture mention, and mechanism of shaking) are more consistent with subdural rather than epidural bleeding.
*Cortical atrophy*
- **Cortical atrophy** refers to the shrinking of brain tissue and is typically seen in chronic conditions like **neurodegenerative diseases** or **long-standing severe malnutrition**.
- It does not explain the acute onset of lethargy and retinal hemorrhages immediately following a potential traumatic event in an otherwise healthy infant.
*Blood in the basal cisterns*
- **Blood in the basal cisterns** is characteristic of **subarachnoid hemorrhage**, which can be caused by ruptured aneurysms (rare in infants), arteriovenous malformations, or severe trauma.
- While abusive head trauma can sometimes cause subarachnoid bleeding, the primary finding in shaken baby syndrome is usually subdural hemorrhage, and retinal hemorrhages specifically point towards the shearing forces causing subdural bleeding.
*Multiple cortical and subcortical infarcts*
- **Multiple cortical and subcortical infarcts** indicate areas of brain tissue death due to **interrupted blood supply**, as seen in severe stroke or vasculitis.
- This is not the primary or most likely finding in abusive head trauma, though severe head trauma can sometimes lead to secondary ischemic injury due to increased intracranial pressure or vascular disruption.
CNS trauma US Medical PG Question 6: A 66-year-old woman is brought to the emergency department 4 hours after falling and hitting her head while skiing. Initially, she refused treatment, but an hour ago she began to develop a severe headache, nausea, and right leg weakness. She has osteopenia. Her only medication is a daily multivitamin. She has no visual changes and is oriented to person, time, and place. Her temperature is 37.2°C (99°F), pulse is 72/min, respirations are 18/min and regular, and blood pressure is 128/75 mm Hg. Examination shows a 5-cm bruise on the left side of her skull. The pupils are equal, round, and reactive to light and accommodation. Muscle strength is 0/5 in her right knee and foot. Which of the following is the most likely cause of this patient's symptoms?
- A. Upward brainstem herniation
- B. Extracranial herniation
- C. Uncal herniation
- D. Subfalcine herniation (Correct Answer)
- E. Tonsillar herniation
CNS trauma Explanation: ***Subfalcine herniation***
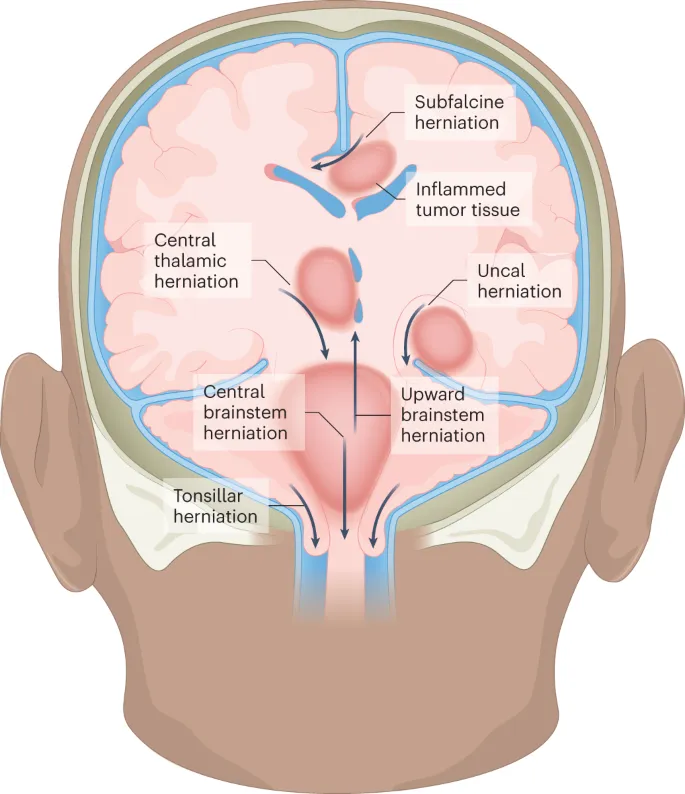
- The patient's presentation with a **traumatic brain injury** followed by **delayed neurological symptoms** including severe headache, nausea, and contralateral leg weakness suggests a mass effect on the brain.
- **Subfalcine herniation** occurs when the **cingulate gyrus** is pushed under the **falx cerebri**, often compressing the **anterior cerebral artery** and causing **contralateral leg weakness** as seen in this patient.
*Upward brainstem herniation*
- This type of herniation typically involves the cerebellum moving upward through the **tentorial incisura**, often presenting with **oculomotor nerve dysfunction** and **loss of consciousness**.
- The patient's mental status is preserved, and she does not exhibit typical signs of brainstem compression.
*Extracranial herniation*
- **Extracranial herniation** refers to brain tissue protruding outside the cranial vault, usually through a **skull defect** or after **craniectomy**.
- This patient has no mention of a skull defect or prior surgery that would predispose her to this type of herniation.
*Uncal herniation*
- **Uncal herniation** involves the medial temporal lobe (uncus) moving over the **tentorium cerebelli**, classically causing ipsilateral **fixed and dilated pupil** due to **oculomotor nerve (CN III) compression**.
- The patient's pupils are equal, round, and reactive to light, which rules out major uncal herniation.
*Tonsillar herniation*
- **Tonsillar herniation** involves the **cerebellar tonsils** descending through the **foramen magnum**, compressing the brainstem and often leading to **respiratory and cardiac irregularities**.
- The patient's vital signs are stable, and she does not have respiratory or cardiac symptoms indicative of tonsillar herniation.
CNS trauma US Medical PG Question 7: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
CNS trauma Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
CNS trauma US Medical PG Question 8: A 68-year-old man is brought to the emergency department by his wife because of a 2-week history of progressive disorientation and a 1-day history of left-sided weakness and difficulty speaking. The wife reports that the patient had a minor fall 4 months ago, during which he may have hit his head. He has hypertension and hyperlipidemia. He drinks 3–4 bottles of beer daily. He is only oriented to person. Neurological examination shows moderate spastic weakness, decreased sensation, and increased deep tendon reflexes in the left upper and lower extremities. A CT scan of the head is shown. Which of the following is the most likely cause of this patient's condition?
- A. Tearing of bridging veins (Correct Answer)
- B. Embolus to middle cerebral artery
- C. Injury to middle meningeal artery
- D. Bleeding from intraventricular vascular malformation
- E. Damage to lenticulostriate arteries
CNS trauma Explanation: ***Tearing of bridging veins***
- The patient's presentation with progressive disorientation, left-sided weakness, and difficulty speaking, occurring months after a minor head trauma, is highly suggestive of a **chronic subdural hematoma**. This typically results from the tearing of **bridging veins** traversing the subdural space.
- Risk factors like **advanced age** (brain atrophy stretches bridging veins), **alcoholism** (which leads to brain atrophy and increased fall risk), and his symptoms progressing over weeks further support this diagnosis.
*Embolus to middle cerebral artery*
- An **embolic stroke** typically presents with a **sudden onset** of neurological deficits, not a progressive deterioration over weeks as seen in this patient.
- While an MCA stroke could cause left-sided weakness and aphasia, the **history of head trauma** and delayed, progressive symptoms are not characteristic.
*Injury to middle meningeal artery*
- Injury to the middle meningeal artery usually leads to an **epidural hematoma**, which presents acutely with a **lucid interval** followed by rapid neurological decline.
- The CT scan of an epidural hematoma shows a **biconvex (lenticular) shape**, whereas a subdural hematoma has a crescent shape.
*Bleeding from intraventricular vascular malformation*
- Intraventricular bleeding from a vascular malformation typically causes **acute hydrocephalus**, severe headache, and rapid neurological deterioration with signs of increased intracranial pressure.
- This scenario does not fit the several-week progressive course or the delayed presentation after trauma.
*Damage to lenticulostriate arteries*
- Damage to the lenticulostriate arteries (often due to hypertension) is a common cause of **lacunar strokes**, which can lead to pure motor or pure sensory deficits.
- While the patient has hypertension, the clinical presentation of progressive symptoms over weeks following head trauma is not typical for a lacunar stroke.
CNS trauma US Medical PG Question 9: A 35-year-old woman presents with headaches and seizures. MRI shows a well-circumscribed, calcified frontal lobe mass. Histology reveals oligodendroglioma with 1p/19q codeletion and IDH1 mutation. She undergoes gross total resection. Two years later, surveillance MRI shows a new enhancing nodule at the resection margin. Biopsy shows increased mitotic activity, microvascular proliferation, and retained 1p/19q codeletion but new CDKN2A/B homozygous deletion. What is the most critical factor in determining management strategy?
- A. The tumor has progressed to anaplastic oligodendroglioma requiring combined chemoradiation with temozolomide and RT
- B. CDKN2A/B deletion indicates transformation to glioblastoma requiring maximal therapy
- C. Retained 1p/19q codeletion predicts continued chemosensitivity to PCV regimen (Correct Answer)
- D. Loss of IDH1 mutation suggests new primary tumor requiring re-resection only
- E. Microvascular proliferation mandates anti-angiogenic therapy with bevacizumab
CNS trauma Explanation: ***Retained 1p/19q codeletion predicts continued chemosensitivity to PCV regimen***
- The preservation of **1p/19q codeletion** in a recurrent tumor is the strongest predictor of clinical response to alkylating chemotherapy, specifically the **PCV (Procarbazine, Lomustine, Vincristine)** regimen.
- While the tumor shows histological progression, the underlying molecular subtype remains an **oligodendroglioma**, which generally carries a better prognosis and higher chemosensitivity than non-codeleted gliomas.
*The tumor has progressed to anaplastic oligodendroglioma requiring combined chemoradiation with temozolomide and RT*
- While the histology suggests a higher grade, the standard of care for 1p/19q codeleted tumors frequently favors **PCV** over **Temozolomide** due to more robust long-term survival data from clinical trials like RTOG 9402.
- Grading alone does not dictate management as much as the **molecular profile** does in modern neuro-oncology guidelines.
*CDKN2A/B deletion indicates transformation to glioblastoma requiring maximal therapy*
- Under the current WHO classification, **glioblastoma** is defined as an **IDH-wildtype** tumor; since this tumor has an **IDH1 mutation**, it cannot be classified as a glioblastoma.
- **CDKN2A/B homozygous deletion** is a marker of high-grade malignancy (WHO Grade 4) in IDH-mutant astrocytomas, but its presence in an **oligodendroglioma** does not change the lineage-defining 1p/19q status.
*Loss of IDH1 mutation suggests new primary tumor requiring re-resection only*
- **IDH1 mutations** are early, trunk events in gliomagenesis and are almost never
CNS trauma US Medical PG Question 10: A 55-year-old man presents with progressive supranuclear gaze palsy, axial rigidity, and frequent falls. MRI shows midbrain atrophy with hummingbird sign. He dies 7 years later. Autopsy reveals globose neurofibrillary tangles in the basal ganglia and brainstem. Tau immunostaining shows 4-repeat tau predominance. His brother had similar symptoms. Genetic testing reveals a MAPT mutation. How does this change the pathogenic understanding and potential therapeutic approach?
- A. It suggests prion-like propagation requiring anti-aggregation compounds
- B. It demonstrates autoimmune etiology requiring immunosuppression
- C. It reveals mitochondrial dysfunction requiring coenzyme Q10 supplementation
- D. It confirms primary tauopathy amenable to tau-directed antisense oligonucleotide therapy (Correct Answer)
- E. It indicates concurrent alpha-synuclein pathology requiring dual-target therapy
CNS trauma Explanation: ***It confirms primary tauopathy amenable to tau-directed antisense oligonucleotide therapy***
- The presence of **MAPT mutations** and **4-repeat (4R) tau** predominance confirms that tau dysfunction is the primary driver of the neurodegenerative process in this **Progressive Supranuclear Palsy (PSP)** phenotype.
- Targeting the underlying genetic cause with **antisense oligonucleotides (ASOs)** can reduce the expression of toxic tau protein, offering a disease-modifying approach rather than just symptomatic relief.
*It suggests prion-like propagation requiring anti-aggregation compounds*
- While **prion-like seeding** occurs in tauopathies, the discovery of a **MAPT mutation** specifically points to a genetic production error rather than isolated misfolding propagation.
- **Anti-aggregation compounds** are a general strategy, but they do not address the primary genetic driver identified by the mutation in this specific case.
*It demonstrates autoimmune etiology requiring immunosuppression*
- **PSP** and related **tauopathies** are degenerative proteinopathies, not autoimmune conditions, and show no response to **immunosuppressive therapy**.
- The **hummingbird sign** and **globose tangles** are classic markers of protein deposition, not inflammatory-mediated demyelination or vasculitis.
*It reveals mitochondrial dysfunction requiring coenzyme Q10 supplementation*
- Although some **mitochondrial deficit** is seen in neurodegeneration, it is a downstream effect and not the primary cause identified by a **MAPT mutation**.
- **Coenzyme Q10** has failed to show significant disease-modifying efficacy in clinical trials for primary tauopathies like **PSP**.
*It indicates concurrent alpha-synuclein pathology requiring dual-target therapy*
- The **MAPT mutation** and **4R tau** findings are specific to tauopathies; **alpha-synuclein** is the hallmark of synucleinopathies like **Parkinson’s disease** or **Multiple System Atrophy (MSA)**.
- Clinical features like the **hummingbird sign** (midbrain atrophy) and **axial rigidity** without resting tremors strongly favor a pure tau pathology over a dual-pathology state.
More CNS trauma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.