Cerebrovascular diseases US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cerebrovascular diseases. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
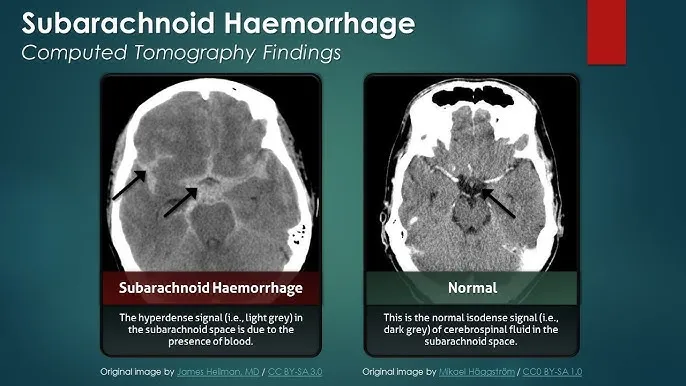
Cerebrovascular diseases US Medical PG Question 1: A 48-year-old man presents to the ER with a sudden-onset, severe headache. He is vomiting and appears confused. His wife, who accompanied him, says that he has not had any trauma, and that the patient has no relevant family history. He undergoes a non-contrast head CT that shows blood between the arachnoid and pia mater. What is the most likely complication from this condition?
- A. Hemorrhagic shock
- B. Arterial Vasospasm (Correct Answer)
- C. Renal failure
- D. Bacterial Meningitis
- E. Blindness
Cerebrovascular diseases Explanation: **Arterial Vasospasm**
- **Arterial vasospasm** is a major delayed complication of **subarachnoid hemorrhage (SAH)**, typically occurring 3-14 days after the initial bleed.
- The presence of blood products in the subarachnoid space can irritate cerebral arteries, leading to their narrowing and subsequent **delayed cerebral ischemia** or infarction.
*Hemorrhagic shock*
- **Subarachnoid hemorrhage (SAH)** typically involves bleeding within the confines of the skull, which is usually not extensive enough to cause systemic **hypovolemia** or **hemorrhagic shock**.
- **Hemorrhagic shock** would require significant external blood loss or internal bleeding into a large body cavity, which is not characteristic of an isolated SAH.
*Renal failure*
- **Renal failure** is not a direct or common complication of **subarachnoid hemorrhage (SAH)**.
- While systemic complications can sometimes arise in critically ill patients, there is no direct pathophysiological link between SAH and primary kidney injury.
*Bacterial Meningitis*
- The presence of blood in the **subarachnoid space** can cause a **chemical meningitis** due to irritation, mimicking some symptoms of bacterial meningitis.
- However, it does not typically predispose to **bacterial infection** unless there's an iatrogenic cause (e.g., lumbar puncture contamination).
*Blindness*
- While damage to the **optic nerves** or visual pathways can occur with severe neurological events or increased intracranial pressure, **blindness** is not a common or direct complication specifically arising from the bleed itself or its immediate sequelae in SAH.
- Visual disturbances are possible due to elevated **intracranial pressure** or specific anatomical lesion, but not primary blindness.
Cerebrovascular diseases US Medical PG Question 2: A 69-year-old man is brought in by his wife with acute onset aphasia for the past 5 hours. The patient's wife says that they were sitting having dinner when suddenly he was not able to speak. They delayed coming to the hospital because he had a similar episode 2 months ago which resolved within an hour. His past medical history is significant for hypercholesterolemia, managed with rosuvastatin, and a myocardial infarction (MI) 2 months ago, status post percutaneous transluminal coronary angioplasty complicated by residual angina. His family history is significant for his father who died of MI at age 60. The patient reports a 15-pack-year smoking history but denies any alcohol or recreational drug use. The vital signs include: temperature 37.0℃ (98.6℉), blood pressure 125/85 mm Hg, pulse 96/min, and respiratory rate 19/min. On physical examination, the patient has expressive aphasia. There is a weakness of the right-sided lower facial muscles. The strength in his upper and lower extremities is 4/5 on the right and 5/5 on the left. There is also a decreased sensation on his right side. A noncontrast computed tomography (CT) scan of the head is unremarkable. CT angiography (CTA) and diffusion-weighted magnetic resonance imaging (MRI) of the brain are acquired, and the findings are shown in the exhibit (see image). Which of the following is the best course of treatment in this patient?
- A. Aspirin
- B. Mannitol
- C. Mechanical thrombectomy (Correct Answer)
- D. IV tPA
- E. Low molecular weight heparin
Cerebrovascular diseases Explanation: ***Mechanical thrombectomy***
- The patient presents with **acute ischemic stroke** symptoms (aphasia, right-sided weakness, sensory deficits) at **5 hours from symptom onset**. Imaging (CTA showing large vessel occlusion and MRI confirming diffusion restriction) demonstrates a **large vessel occlusion**, making him a candidate for **mechanical thrombectomy**.
- Since the patient is **beyond the 4.5-hour window for IV tPA**, mechanical thrombectomy is the **primary reperfusion therapy** indicated for large vessel occlusion strokes up to **24 hours** (with appropriate imaging showing salvageable tissue).
- Mechanical thrombectomy offers the best chance for complete recanalization and improved neurological outcomes in large vessel occlusion strokes, particularly when IV tPA is not an option.
*Aspirin*
- While **aspirin** is crucial for **secondary stroke prevention**, it is not the primary acute treatment for a large vessel occlusion stroke due to its limited ability to achieve rapid and complete recanalization.
- Aspirin (or other antiplatelet therapy) is typically initiated **within 24-48 hours after stroke onset**, but only after excluding hemorrhagic transformation and after acute reperfusion therapies have been considered or completed.
*Mannitol*
- **Mannitol** is an osmotic diuretic used to reduce **intracranial pressure (ICP)** in cases of severe cerebral edema, which can be a complication of large ischemic strokes.
- It is not a primary treatment for the acute ischemic event itself, but rather a supportive measure used to manage life-threatening complications if **cerebral edema** develops and causes significant mass effect or herniation risk.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is the first-line pharmacologic treatment for acute ischemic stroke if administered **within 4.5 hours of symptom onset** in eligible patients.
- This patient presents at **5 hours**, which is **beyond the approved time window** for IV tPA administration, making him **ineligible** for thrombolytic therapy.
- Even if within the time window, patients with large vessel occlusion often require mechanical thrombectomy in addition to or instead of IV tPA for optimal outcomes.
*Low molecular weight heparin*
- **Low molecular weight heparin (LMWH)** is primarily used for **deep vein thrombosis (DVT)** prophylaxis in immobilized patients or for the treatment of established DVT/pulmonary embolism.
- It is generally **not recommended for acute ischemic stroke treatment** due to an increased risk of hemorrhagic transformation without proven benefit in recanalization or clinical outcomes.
Cerebrovascular diseases US Medical PG Question 3: A 61-year-old man is brought to the emergency room with slurred speech. According to the patient's wife, they were watching a movie together when he developed a minor headache. He soon developed difficulty speaking in complete sentences, at which point she decided to take him to the emergency room. His past medical history is notable for hypertension and hyperlipidemia. He takes aspirin, lisinopril, rosuvastatin. The patient is a retired lawyer. He has a 25-pack-year smoking history and drinks 4-5 beers per day. His father died of a myocardial infarction, and his mother died of breast cancer. His temperature is 98.6°F (37°C), blood pressure is 143/81 mmHg, pulse is 88/min, and respirations are 21/min. On exam, he can understand everything that is being said to him and is able to repeat statements without difficulty. However, when asked to speak freely, he hesitates with every word and takes 30 seconds to finish a short sentence. This patient most likely has an infarct in which of the following vascular distributions?
- A. Proximal middle cerebral artery
- B. Inferior division of the middle cerebral artery
- C. Middle cerebral artery and posterior cerebral artery watershed area
- D. Superior division of the middle cerebral artery (Correct Answer)
- E. Anterior cerebral artery and middle cerebral artery watershed area
Cerebrovascular diseases Explanation: ***Superior division of the middle cerebral artery***
- The patient's inability to speak spontaneously coupled with intact comprehension and repetition is characteristic of **Broca's aphasia**, which results from damage to **Broca's area** in the dominant frontal lobe.
- Broca's area is supplied by the **superior division of the middle cerebral artery (MCA)**.
*Proximal middle cerebral artery*
- An infarct in the proximal MCA, or the main stem, would typically lead to global aphasia if the dominant hemisphere is affected, characterized by **severe deficits in comprehension, repetition, and speech production**.
- This presentation does not align with the patient's ability to understand and repeat statements.
*Inferior division of the middle cerebral artery*
- The inferior division of the MCA supplies Wernicke's area in the dominant hemisphere.
- Damage here causes **Wernicke's aphasia**, characterized by **fluent but nonsensical speech** with **impaired comprehension** and **repetition**, which is contrary to the patient's symptoms.
*Middle cerebral artery and posterior cerebral artery watershed area*
- Watershed infarcts, especially between the MCA and posterior cerebral artery (PCA), can cause **transcortical sensory aphasia** if in the dominant hemisphere.
- This type of aphasia involves impaired comprehension but **intact repetition**, which differs from Broca's aphasia where spontaneous speech is the main deficit.
*Anterior cerebral artery and middle cerebral artery watershed area*
- Infarcts in the watershed area between the anterior cerebral artery (ACA) and MCA can result in **transcortical motor aphasia** if in the dominant hemisphere.
- This condition presents with **non-fluent speech** and **intact repetition**, similar to Broca's aphasia, but Broca's area itself is located specifically within the MCA superior division territory.
Cerebrovascular diseases US Medical PG Question 4: A 76-year-old woman with hypertension and coronary artery disease is brought to the emergency department after the sudden onset of right-sided weakness. Her pulse is 83/min and blood pressure is 156/90 mm Hg. Neurological examination shows right-sided facial drooping and complete paralysis of the right upper and lower extremities. Tongue position is normal and she is able to swallow liquids without difficulty. Knee and ankle deep tendon reflexes are exaggerated on the right. Sensation to vibration, position, and light touch is normal bilaterally. She is oriented to person, place, and time, and is able to speak normally. Occlusion of which of the following vessels is the most likely cause of this patient's current symptoms?
- A. Ipsilateral anterior cerebral artery
- B. Contralateral middle cerebral artery
- C. Anterior spinal artery
- D. Contralateral lenticulostriate artery (Correct Answer)
- E. Ipsilateral posterior inferior cerebellar artery
Cerebrovascular diseases Explanation: ***Contralateral lenticulostriate artery***
- The patient presents with **pure motor hemiparesis** affecting the face, arm, and leg equally on the right side, with **no sensory deficits, aphasia, or cognitive impairment**.
- This clinical pattern is classic for a **lacunar stroke** affecting the **internal capsule**, which is supplied by the **lenticulostriate arteries** (branches of the middle cerebral artery).
- The internal capsule contains tightly packed corticospinal and corticobulbar fibers; a small infarct here causes complete contralateral motor deficits without cortical signs.
- The **absence of cortical findings** (normal speech, cognition, and sensation) distinguishes this from cortical MCA stroke.
*Contralateral middle cerebral artery*
- A **cortical MCA stroke** would typically present with **cortical signs** such as aphasia (if left hemisphere), neglect (if right hemisphere), sensory loss, and visual field defects.
- MCA strokes usually show **arm and face > leg** weakness (the leg area is supplied by ACA).
- This patient's **pure motor syndrome** without cortical signs points to a subcortical lesion, not cortical MCA occlusion.
*Ipsilateral anterior cerebral artery*
- First, the lateralization is incorrect - symptoms are right-sided, indicating left hemisphere pathology, so it would be **contralateral** ACA.
- ACA occlusion causes weakness predominantly in the **contralateral leg > arm**, with relative sparing of the face.
- This patient has equal involvement of face, arm, and leg, which is inconsistent with ACA territory.
*Anterior spinal artery*
- The **anterior spinal artery** supplies the anterior two-thirds of the spinal cord, including the corticospinal tracts and anterior horn cells.
- Occlusion causes **bilateral** motor weakness below the lesion level and bilateral loss of pain/temperature sensation.
- It does not cause **unilateral facial weakness** or the distribution of deficits seen in this patient.
*Ipsilateral posterior inferior cerebellar artery*
- Again, lateralization is incorrect - symptoms would be from **contralateral** PICA for motor findings, but PICA supplies the lateral medulla and inferior cerebellum.
- PICA occlusion causes **lateral medullary syndrome (Wallenberg syndrome)**: ataxia, vertigo, dysphagia, dysarthria, Horner syndrome, and contralateral pain/temperature loss.
- The patient's **pure motor hemiparesis** without cerebellar or brainstem signs is incompatible with PICA occlusion.
Cerebrovascular diseases US Medical PG Question 5: A 62-year-old woman comes to the physician for decreased vision and worsening headaches since this morning. She has hypertension and hypercholesterolemia. Pulse is 119/min and irregular. Current medications include ramipril and atorvastatin. Ocular and funduscopic examination shows no abnormalities. The findings of visual field testing are shown. Which of the following is the most likely cause of this patient's symptoms?
- A. Occlusion of the posterior cerebral artery (Correct Answer)
- B. Occlusion of anterior cerebral artery
- C. Degeneration of the macula
- D. Occlusion of the anterior inferior cerebellar artery
- E. Impaired perfusion of the retina
Cerebrovascular diseases Explanation: ***Occlusion of the posterior cerebral artery***
- The patient presents with **acute visual field defect** and **headache** in the context of an **irregular pulse** (atrial fibrillation).
- **Atrial fibrillation** is a major risk factor for **cardioembolic stroke**, particularly affecting the posterior circulation.
- The **posterior cerebral artery (PCA) supplies the occipital lobe**, which contains the primary visual cortex. PCA occlusion causes **contralateral homonymous hemianopia**, often with **macular sparing** due to collateral blood supply from the middle cerebral artery.
- The visual field defect pattern shown, combined with normal funduscopic examination (ruling out retinal pathology), is characteristic of **occipital cortex ischemia**.
- **Acute onset** with headache further supports an embolic stroke mechanism.
*Occlusion of anterior cerebral artery*
- Anterior cerebral artery (ACA) occlusion primarily affects the **frontal and medial parietal lobes**.
- Classic presentation includes **contralateral leg weakness** > arm weakness, sensory loss in the leg, and behavioral/personality changes.
- ACA strokes do **not cause visual field defects** or homonymous hemianopia.
*Degeneration of the macula*
- Macular degeneration causes **gradual central vision loss**, presenting with difficulty reading and central scotomas.
- This is a **chronic progressive condition**, not acute onset "since this morning."
- Would not cause **headache**, irregular pulse correlation, or the specific visual field pattern shown.
- Funduscopy would typically show **drusen** or retinal pigmentary changes.
*Occlusion of the anterior inferior cerebellar artery*
- AICA occlusion affects the **lateral pons and cerebellum**.
- Presents with **vertigo, nystagmus, ataxia, ipsilateral facial paralysis**, and hearing loss.
- Does **not affect the visual cortex** and would not cause homonymous visual field defects.
*Impaired perfusion of the retina*
- Central retinal artery occlusion causes **sudden monocular painless vision loss** (not bilateral field defects).
- Funduscopy would reveal **"cherry-red spot"** at the macula and retinal whitening.
- The question states funduscopic examination shows **no abnormalities**, excluding this diagnosis.
- Would not explain the bilateral homonymous field defect pattern.
Cerebrovascular diseases US Medical PG Question 6: An 88-year-old woman with no significant medical history is brought to the emergency room by her daughter after a fall, where the woman lightly hit her head against a wall. The patient is lucid and complains of a mild headache. The daughter indicates that her mother did not lose consciousness after the fall. On exam, there are no focal neurological deficits, but you decide to perform a CT scan to be sure there is no intracranial bleeding. The CT scan is within normal limits and head MRI is performed (shown). Which of the following conditions has the most similar risk factor to this patient's condition?
- A. Pulmonary embolism
- B. Raynaud's phenomenon
- C. Prinzmetal's angina
- D. Abdominal aortic aneurysm
- E. Thoracic aortic aneurysm (Correct Answer)
Cerebrovascular diseases Explanation: ***Thoracic aortic aneurysm***
- The MRI images show numerous **microhemorrhages** (dark spots on the GRE/SWI sequences), indicative of **cerebral amyloid angiopathy (CAA)**, a common cause of lobar intracerebral hemorrhage in the elderly.
- CAA is most strongly associated with **advanced age** (the primary risk factor), and both CAA and **thoracic aortic aneurysm (TAA)** can be associated with **underlying connective tissue abnormalities** and vascular wall weakening processes.
- While the exact pathophysiology differs, both conditions involve progressive vascular wall degeneration that increases with age.
*Abdominal aortic aneurysm*
- While AAA is strongly associated with **advanced age**, **hypertension**, and **smoking**, it is primarily driven by **atherosclerotic degeneration** rather than the amyloid deposition seen in CAA.
- AAA has a particularly strong association with smoking (the most important modifiable risk factor), which is not characteristic of CAA.
*Pulmonary embolism*
- Primarily caused by **venous thromboembolism** (VTE) due to factors like immobility, surgery, cancer, and hypercoagulable states, which are distinct from CAA risk factors.
- While age is a risk factor for PE, the underlying mechanisms (thrombosis vs. vascular wall amyloid deposition) differ fundamentally.
*Raynaud's phenomenon*
- Characterized by **vasospasm** of small arteries and arterioles, typically triggered by cold or stress, and is often associated with connective tissue diseases.
- Its pathophysiology is unrelated to the progressive vascular wall degeneration and amyloid deposition seen in CAA.
*Prinzmetal's angina*
- Caused by **coronary artery spasm**, leading to transient myocardial ischemia, often occurring at rest and typically not associated with age-related vascular degeneration.
- The mechanism is localized vascular spasm rather than widespread degenerative arterial disease or amyloid deposition.
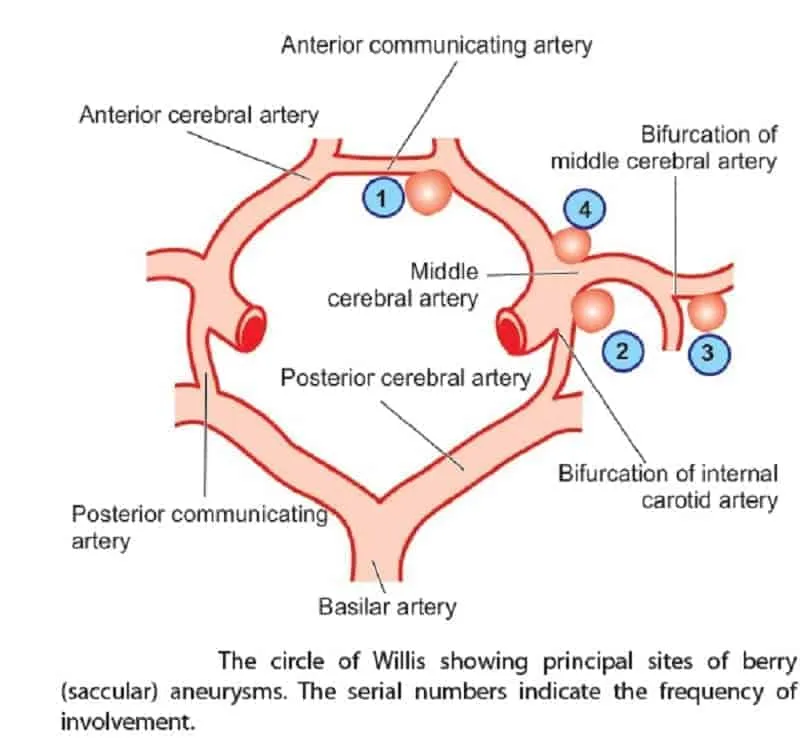
Cerebrovascular diseases US Medical PG Question 7: A 67-year old woman is brought to the emergency department after she lost consciousness while at home. Her daughter was with her at the time and recalls that her mother was complaining of a diffuse headache and nausea about 2 hours before the incident. The daughter says that her mother has not had any recent falls and was found sitting in a chair when she lost consciousness. She has hypertension. Current medications include amlodipine, a daily multivitamin, and acetaminophen. She has smoked 1/2 pack of cigarettes daily for the past 45 years. Her pulse is 92/min, respirations are 10/min, and blood pressure is 158/100 mm Hg. She is disoriented and unable to follow commands. Examination shows nuchal rigidity. She has flexor posturing to painful stimuli. Fundoscopic examination is notable for bilateral vitreous hemorrhages. Laboratory studies are within normal limits. An emergent non-contrast CT scan of the head is obtained and shows a diffuse hemorrhage at the base of the brain that is largest over the left hemisphere. Which of the following is the most likely cause of this patient's symptoms?
- A. Intracranial arterial dissection
- B. Ruptured saccular aneurysm (Correct Answer)
- C. Ruptured mycotic aneurysm
- D. Spinal arteriovenous malformation
- E. Intracranial arteriovenous malformation
Cerebrovascular diseases Explanation: ***Ruptured saccular aneurysm***
- The sudden onset of a "thunderclap" headache, **nuchal rigidity**, diffuse hemorrhage at the base of the brain, and **vitreous hemorrhages (Terson syndrome)** are all highly suggestive of a **subarachnoid hemorrhage (SAH)**, most commonly caused by a ruptured saccular aneurysm. Her history of **hypertension and smoking** are significant risk factors for aneurysm formation and rupture.
- The disorientation and flexor posturing indicate severe neurological compromise due to increased **intracranial pressure** and brainstem involvement, consistent with a large SAH.
*Intracranial arterial dissection*
- While an intracranial arterial dissection can cause hemorrhage, it typically presents with neck pain, lower cranial nerve palsies, or ischemic stroke symptoms due to **thromboembolism**, which are not prominent features here.
- The **diffuse hemorrhage at the base of the brain** and bilateral vitreous hemorrhages are more characteristic of a ruptured aneurysm than a dissection.
*Ruptured mycotic aneurysm*
- A mycotic aneurysm results from an **infectious embolus** lodging in an artery, leading to vessel wall weakening and rupture. This would typically be seen in the context of **endocarditis** or other systemic infections, for which there is no evidence in this patient.
- The patient's presentation lacks systemic signs of infection (e.g., fever, new heart murmur, or elevated inflammatory markers) that would point to an infectious etiology.
*Spinal arteriovenous malformation*
- A spinal arteriovenous malformation (AVM) would present with **spinal cord symptoms** such as back pain, weakness, sensory deficits, or bladder/bowel dysfunction, not primarily with a diffuse intracranial hemorrhage or severe headache.
- While it could theoretically cause a hemorrhage, the clinical presentation and CT findings are unequivocally localized to the **brain**, making a spinal origin unlikely.
*Intracranial arteriovenous malformation*
- An intracranial AVM can cause **intracerebral hemorrhage** or, less commonly, subarachnoid hemorrhage, but the hemorrhages tend to be more localized within the brain parenchyma or along the AVM itself.
- Though an AVM could be a differential, the classic presentation including **thunderclap headache**, Terson syndrome, and diffuse basilar hemorrhage is a more classic presentation of a **ruptured saccular aneurysm**.
Cerebrovascular diseases US Medical PG Question 8: A 68-year-old woman is brought to the emergency department after being found unresponsive in her bedroom in a nursing home facility. Her past medical history is relevant for hypertension, diagnosed 5 years ago, for which she has been prescribed a calcium channel blocker and a thiazide diuretic. Upon admission, she is found with a blood pressure of 200/116 mm Hg, a heart rate of 70/min, a respiratory rate of 15 /min, and a temperature of 36.5°C (97.7°F). Her cardiopulmonary auscultation is unremarkable, except for the identification of a 4th heart sound. Neurological examination reveals the patient is stuporous, with eye-opening response reacting only to pain, no verbal response, and flexion withdrawal to pain. Both pupils are symmetric, with the sluggish pupillary response to light. A noncontrast CT of the head is performed and is shown in the image. Which of the following is the most likely etiology of this patient’s condition?
- A. Arteriovenous malformation rupture
- B. Venous sinus thrombosis
- C. Hemorrhagic transformation
- D. Charcot-Bouchard aneurysm rupture (Correct Answer)
- E. Dural arteriovenous fistula
Cerebrovascular diseases Explanation: ***Charcot-Bouchard aneurysm rupture***
- The patient's history of **uncontrolled hypertension** and presentation with **intracerebral hemorrhage** in the deep brain structures (likely basal ganglia or thalamus, as seen on CT) are highly characteristic of a ruptured Charcot-Bouchard aneurysm.
- These aneurysms are caused by chronic hypertension leading to microaneurysms in the small perforating arteries, which then rupture.
*Arteriovenous malformation rupture*
- AVMs can cause intracerebral hemorrhage, but they are typically **congenital** and often present at a younger age or with other symptoms like seizures or headaches prior to rupture.
- The CT image shows a localized hematoma, not typical for the more diffuse or lobar hemorrhage often associated with AVMs.
*Venous sinus thrombosis*
- This condition involves clotting in the cerebral venous sinuses, often leading to **venous infarction** and sometimes hemorrhagic transformation.
- While it can cause neurological deficits and hemorrhage, it typically presents with different imaging findings (e.g., delta sign on contrast CT, specific MRI findings) and symptoms like severe headaches and papilledema, which are not explicitly described here.
*Hemorrhagic transformation*
- Hemorrhagic transformation refers to an **ischemic stroke** that subsequently bleeds, often within the infarcted tissue.
- While possible, the sudden onset in an elderly hypertensive patient with a singular, well-defined deep hemorrhage on CT is more indicative of a primary hypertensive hemorrhage due to aneurysmal rupture rather than a conversion from ischemia, especially without prior signs of ischemic stroke.
*Dural arteriovenous fistula*
- DAVFs are abnormal connections between dural arteries and veins, which can lead to venous hypertension and hemorrhage.
- However, they are **rarer** than hypertensive hemorrhages and often present with pulsatile tinnitus, proptosis, or specific imaging findings of dilated draining veins, which are not present in this scenario.
Cerebrovascular diseases US Medical PG Question 9: A 47-year-old man presents as a new patient at an outpatient clinic. He has never seen a physician before, but was motivated by his 40-year-old brother's recent heart attack and seeks to optimize his health. In particular, he read that uncontrolled atherosclerosis can lead to a heart attack. Which molecule is downregulated in response to the advent of atherosclerosis?
- A. Tumor necrosis factor
- B. Serotonin
- C. Nitric oxide (Correct Answer)
- D. Interleukin 1
- E. Thromboxane A2
Cerebrovascular diseases Explanation: ***Nitric oxide***
- **Nitric oxide (NO)** is a potent **vasodilator** and **anti-inflammatory** molecule produced by endothelial cells. In atherosclerosis, endothelial dysfunction leads to reduced NO bioavailability.
- Decreased NO production contributes to vasoconstriction, increased platelet aggregation, and enhanced smooth muscle cell proliferation, all of which promote **atherosclerotic plaque formation** and progression.
*Tumor necrosis factor*
- **Tumor necrosis factor-alpha (TNF-α)** is a **pro-inflammatory cytokine** that plays a significant role in the pathogenesis of atherosclerosis.
- It is **upregulated** in response to atherosclerotic plaque formation, contributing to endothelial activation, leukocyte recruitment, and smooth muscle cell proliferation.
*Serotonin*
- **Serotonin (5-hydroxytryptamine)** is primarily known for its role as a neurotransmitter but also acts as a **vasoconstrictor** and promotes platelet aggregation.
- While it can be released from activated platelets in the context of vascular injury, it is not consistently **downregulated** in atherosclerosis; rather, its effects can contribute to disease progression.
*Interleukin 1*
- **Interleukin-1 (IL-1)**, particularly IL-1β, is a major **pro-inflammatory cytokine** critically involved in the immune response in atherosclerosis.
- It is **upregulated** in atherosclerotic plaques, contributing to systemic inflammation, endothelial dysfunction, and vascular smooth muscle cell activation.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is a potent **vasoconstrictor** and **platelet aggregator** produced by activated platelets.
- Its levels are **increased** in atherosclerosis, contributing to hypercoagulability and increased risk of thrombotic events like myocardial infarction.
Cerebrovascular diseases US Medical PG Question 10: A 72-year-old man comes to the physician because of a 6-month history of intermittent dull abdominal pain that radiates to the back. He has smoked one pack of cigarettes daily for 50 years. His blood pressure is 145/80 mm Hg. Abdominal examination shows generalized tenderness and a pulsatile mass in the periumbilical region on deep palpation. Further evaluation of the affected blood vessel is most likely to show which of the following?
- A. Obliterative inflammation of the vasa vasorum
- B. Formation of giant cells in the tunica media
- C. Necrotizing inflammation of the entire vessel wall
- D. Fragmentation of elastic tissue in the tunica media (Correct Answer)
- E. Accumulation of foam cells in the tunica intima
Cerebrovascular diseases Explanation: ***Fragmentation of elastic tissue in the tunica media***
- This patient's presentation with **intermittent dull abdominal pain radiating to the back**, a **pulsatile periumbilical mass**, and a history of **heavy smoking** is highly suggestive of an **abdominal aortic aneurysm (AAA)**.
- The pathological hallmark of AAA is **degradation and fragmentation of elastic tissue in the tunica media**, caused by chronic inflammation and increased activity of **matrix metalloproteinases (MMPs)**.
- This medial degeneration leads to **weakening of the vessel wall** and progressive **dilation**, ultimately forming an aneurysm.
- While atherosclerosis initiates the process, the actual aneurysm formation is characterized by this elastic tissue destruction in the media.
*Accumulation of foam cells in the tunica intima*
- This describes the **early lesion of atherosclerosis**, which is a **risk factor** for AAA development.
- However, when examining an **established AAA**, the predominant finding is not intimal foam cells but rather **medial degeneration** with elastic tissue fragmentation.
- Atherosclerosis is the underlying cause, but the question asks about findings in the affected vessel (the aneurysm itself).
*Obliterative inflammation of the vasa vasorum*
- This is characteristic of **syphilitic aortitis** (tertiary syphilis), which typically affects the **ascending thoracic aorta**.
- While syphilis can cause aneurysms, the patient's presentation and demographics are more consistent with atherosclerotic AAA.
*Formation of giant cells in the tunica media*
- This finding is associated with **giant cell arteritis** (temporal arteritis), which affects large and medium-sized arteries, particularly the temporal and ophthalmic arteries.
- It presents with headache, jaw claudication, and visual disturbances—features absent in this case.
*Necrotizing inflammation of the entire vessel wall*
- This describes **necrotizing vasculitis** such as **polyarteritis nodosa**, which affects medium-sized muscular arteries.
- While vasculitis can cause aneurysms, the clinical picture of AAA in an elderly smoker with atherosclerotic risk factors points to atherosclerotic pathogenesis, not primary vasculitis.
More Cerebrovascular diseases US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.