Tumor invasion and metastasis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tumor invasion and metastasis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Tumor invasion and metastasis US Medical PG Question 1: A researcher is studying the ability of breast cancer cells to metastasize. Neoplastic cells obtained from 30 patients with stage IV ductal carcinoma of the breast are tagged with a fluorescent antibody. The cells are then inserted into a medium resembling normal human tissue. After 2 weeks, all samples show in vitro hematogenous invasion and migration away from the original site of insertion. Which of the following properties is most likely responsible for the ability of these neoplastic cells to metastasize?
- A. Loss of cellular polarity
- B. Presence of fibrous tissue capsule
- C. Overexpression of HER2/neu
- D. Increase in N:C ratio
- E. Release of matrix metalloproteinase (Correct Answer)
Tumor invasion and metastasis Explanation: ***Release of matrix metalloproteinase***
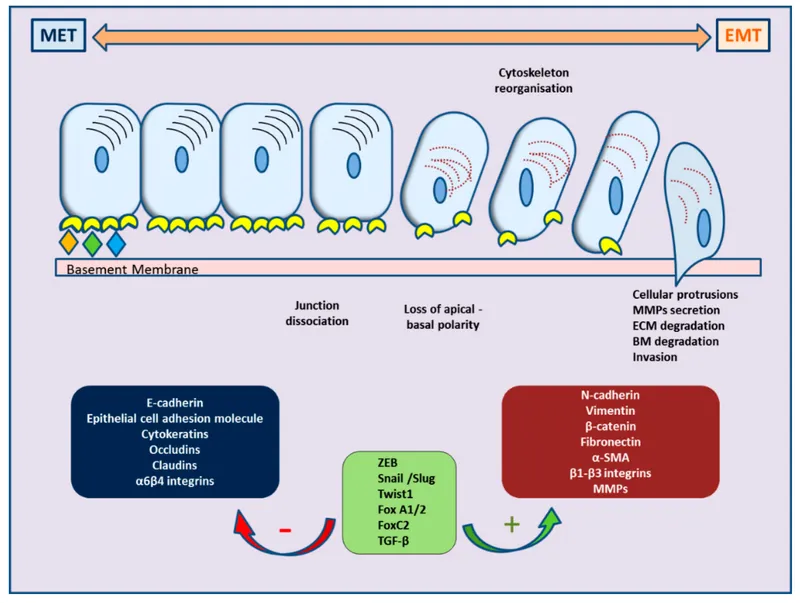
- **Matrix metalloproteinases (MMPs)** degrade components of the **extracellular matrix (ECM)** and **basement membrane**, allowing cancer cells to invade surrounding tissues and metastasize [1].
- The in vitro observation of **hematogenous invasion** and **migration** confirms the ability to break down barriers critical for metastasis [2].
*Loss of cellular polarity*
- While **loss of polarity** is a feature of malignant transformation, it primarily contributes to disorganized growth and invasion rather than the active breakdown of the physical barriers required for long-distance metastasis.
- It does not directly explain the enzymatic degradation of the **ECM** necessary for transmural passage into blood vessels [2].
*Presence of fibrous tissue capsule*
- A **fibrous tissue capsule** typically indicates a **benign tumor** or a well-demarcated malignant tumor with limited invasiveness, restricting spread.
- Its presence would hinder, rather than promote, the ability of cancer cells to metastasize.
*Overexpression of HER2/neu*
- **HER2/neu overexpression** is a marker of aggressive breast cancer and can promote cell proliferation and survival.
- However, it does not directly facilitate the enzymatic degradation of the **extracellular matrix** required for active invasion and migration [2].
**References:**
[1] Cross SS. Underwood's Pathology: A Clinical Approach. 6th ed. (Basic Pathology) introduces the student to key general principles of pathology, both as a medical science and as a clinical activity with a vital role in patient care. Part 2 (Disease Mechanisms) provides fundamental knowledge about the cellular and molecular processes involved in diseases, providing the rationale for their treatment. Part 3 (Systematic Pathology) deals in detail with specific diseases, with emphasis on the clinically important aspects., pp. 232-233.
[2] Kumar V, Abbas AK, et al.. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Neoplasia, pp. 314-316.
Tumor invasion and metastasis US Medical PG Question 2: A 57-year-old man is brought to the emergency department by his wife 20 minutes after having had a seizure. He has had recurrent headaches and dizziness for the past 2 weeks. An MRI of the brain shows multiple, round, well-demarcated lesions in the brain parenchyma at the junction between gray and white matter. This patient's brain lesions are most likely comprised of cells that originate from which of the following organs?
- A. Kidney
- B. Skin
- C. Lung (Correct Answer)
- D. Thyroid
- E. Prostate
Tumor invasion and metastasis Explanation: ***Lung (Correct Answer)***
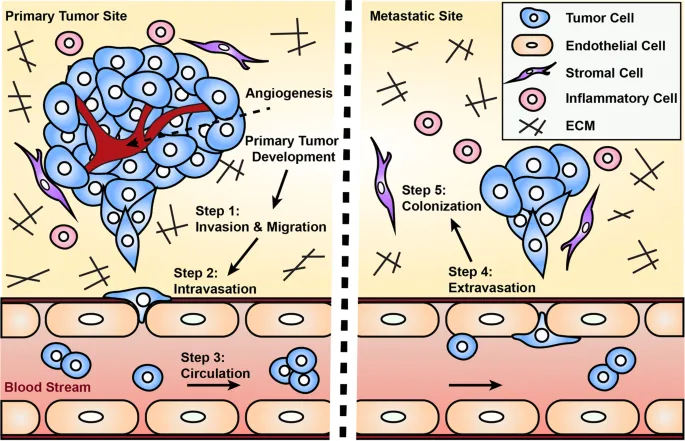
- **Lung cancer** is the most common cause of **brain metastases** in adults, accounting for approximately **50% of all cases**
- The clinical presentation—seizure, headaches, dizziness, and **multiple, round, well-demarcated lesions at the gray-white matter junction**—is classic for metastatic lung cancer
- Both **small cell and non-small cell lung cancers** have high propensity for hematogenous spread to the brain
- The watershed areas at the gray-white junction are common sites due to lodging of tumor emboli in terminal arterioles
*Kidney (Incorrect)*
- **Renal cell carcinoma (RCC)** can metastasize to the brain but accounts for only **5-10% of brain metastases**
- While RCC metastases can appear similar on imaging, lung cancer is statistically more likely given its higher prevalence
- RCC metastases are often **highly vascular and may hemorrhage**, which is not mentioned in this case
*Skin (Incorrect)*
- **Melanoma** has the **highest propensity per case** to metastasize to the brain among all cancers
- However, the **overall incidence of melanoma is much lower** than lung cancer, making it a less probable primary source
- Melanoma brain metastases often present as **hemorrhagic lesions** and would typically have skin findings or history
*Thyroid (Incorrect)*
- **Thyroid cancer** rarely metastasizes to the brain (accounts for <1% of brain metastases)
- Brain metastases from thyroid cancer typically occur in **advanced papillary or follicular carcinoma** or in **anaplastic thyroid cancer**
- More common metastatic sites for thyroid cancer are lung and bone
*Prostate (Incorrect)*
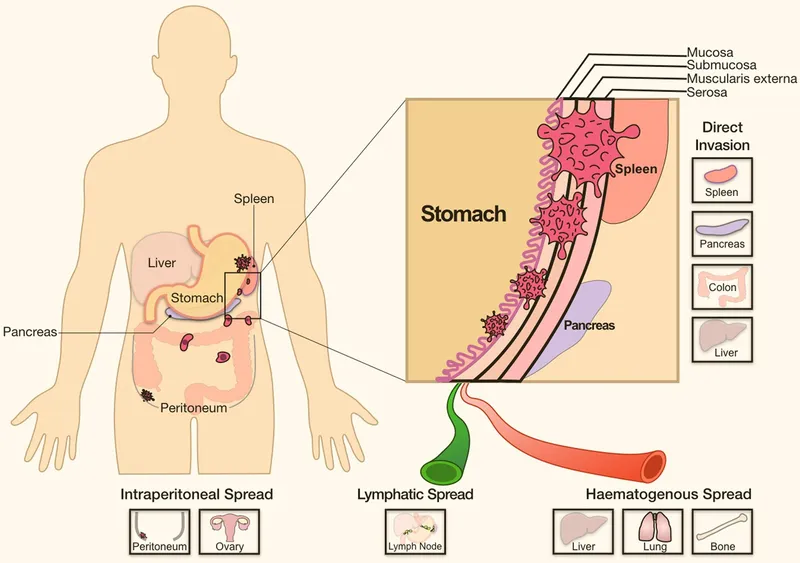
- **Prostate cancer very rarely metastasizes to the brain** (<1% of cases)
- Prostate cancer preferentially metastasizes to **bone (especially axial skeleton), lymph nodes, and liver**
- Brain metastases from prostate cancer suggest extremely advanced, aggressive disease and are exceptionally uncommon
Tumor invasion and metastasis US Medical PG Question 3: A researcher is tracing the fate of C-peptide, a product of preproinsulin cleavage. Which of the following is a true statement regarding the fate of C-peptide?
- A. C-peptide exits the cells via a protein channel
- B. C-peptide is further cleaved into insulin
- C. C-peptide is packaged with insulin in secretory vesicles (Correct Answer)
- D. C-peptide is immediately degraded by the proteasome
- E. C-peptide activates an intracellular signaling cascade
Tumor invasion and metastasis Explanation: ***C-peptide is packaged with insulin in secretory vesicles***
- Preproinsulin is cleaved in the **endoplasmic reticulum** to proinsulin (signal peptide removal), which is then transported to the **Golgi apparatus**.
- In the Golgi, proinsulin is cleaved by **prohormone convertases** into **insulin** and **C-peptide**, and both are stored together in **secretory vesicles** within the pancreatic beta cells.
- Upon stimulation, both insulin and C-peptide are **co-secreted** via exocytosis in equimolar amounts, making C-peptide a useful marker of endogenous insulin secretion.
*C-peptide exits the cells via a protein channel*
- C-peptide exits the beta cells via **exocytosis** of secretory granules, not through specific protein channels.
- It is **co-secreted with insulin** when secretory vesicles fuse with the plasma membrane.
- Its presence in the bloodstream in equimolar amounts with insulin makes it an indirect measure of **insulin secretion**.
*C-peptide is further cleaved into insulin*
- **C-peptide** is a product of proinsulin cleavage, alongside insulin; it is not further processed into insulin.
- Insulin itself is composed of two **peptide chains (A and B)** linked by disulfide bonds, formed after C-peptide is removed from proinsulin.
*C-peptide is immediately degraded by the proteasome*
- C-peptide is not immediately degraded by the **proteasome** upon synthesis.
- After secretion, it circulates in the blood with a **longer half-life** than insulin (approximately 30 minutes versus 4-6 minutes), allowing it to be a useful marker of endogenous insulin production.
- Its degradation occurs primarily in the **kidney**.
*C-peptide activates an intracellular signaling cascade*
- While there is some research suggesting C-peptide may have independent **biological activity** and activate certain signaling pathways extracellularly, its primary role in the context of the insulin synthesis pathway is as a **byproduct** of proinsulin processing.
- Its clinical utility is primarily as a **biomarker** of endogenous insulin secretion, particularly useful in distinguishing between endogenous and exogenous insulin in diabetic patients.
Tumor invasion and metastasis US Medical PG Question 4: A 65-year-old man with a 40-pack-year smoking history presents with hemoptysis and a persistent cough. Chest CT shows a 3.5 cm centrally located mass in the right main bronchus. Positron emission tomography confirms a malignant nodule. Bronchoscopy with transbronchial biopsy is performed and a specimen sample of the nodule is sent for frozen section analysis. The tissue sample is most likely to show which of the following tumor types?
- A. Carcinoid tumor
- B. Metastasis of colorectal cancer
- C. Small cell lung carcinoma
- D. Large cell carcinoma
- E. Squamous cell carcinoma (Correct Answer)
Tumor invasion and metastasis Explanation: ***Squamous cell carcinoma***
- This is the most likely diagnosis given the **central location** in the main bronchus, **heavy smoking history**, and presentation with **hemoptysis**.
- **Squamous cell carcinoma** accounts for 25-30% of lung cancers and characteristically arises in **central/proximal airways**, making it readily accessible by **bronchoscopy**.
- Histologically, it shows **keratin pearls** and **intercellular bridges** on biopsy.
- The **central endobronchial location** and ability to obtain tissue via transbronchial biopsy strongly favor squamous cell over peripheral tumors.
*Carcinoid tumor*
- **Carcinoid tumors** are **neuroendocrine tumors** that can present as central endobronchial masses and cause hemoptysis.
- However, they are typically **slow-growing** with more indolent presentation, and PET scans show **variable uptake** (often less intense than aggressive carcinomas).
- They represent only **1-2% of lung tumors** and occur more commonly in **younger, non-smoking patients**.
*Metastasis of colorectal cancer*
- While lung is a common site for **colorectal metastases**, these typically present as **multiple peripheral nodules** rather than a solitary central endobronchial mass.
- The clinical presentation strongly suggests **primary lung cancer** rather than metastatic disease.
- Without history of colorectal cancer, this is unlikely.
*Small cell lung carcinoma*
- **Small cell lung carcinoma** (SCLC) represents 15% of lung cancers and typically presents as a **large central mass** with early mediastinal involvement.
- However, SCLC is usually **too extensive at presentation** for transbronchial biopsy alone and often requires mediastinoscopy or CT-guided biopsy.
- Histology shows **small cells with scant cytoplasm**, **salt-and-pepper chromatin**, and **oat-cell morphology**.
- While possible, the single accessible endobronchial mass is more characteristic of squamous cell.
*Large cell carcinoma*
- **Large cell carcinoma** is a **diagnosis of exclusion** made when tumors lack features of adenocarcinoma, squamous cell, or small cell differentiation.
- It typically presents as **large peripheral masses** rather than central endobronchial lesions.
- It represents only **10% of lung cancers** and is less common than squamous cell carcinoma in this clinical scenario.
Tumor invasion and metastasis US Medical PG Question 5: An investigator is studying the interaction between epithelial cells and calcium ion concentration. When the calcium ion concentration available to a sample of epithelial tissue is decreased, an increased gap between adjacent epithelial cells is seen on electron microscopy. This observed decrease in cell adhesion is most likely due to an effect on which of the following proteins?
- A. Actin
- B. Integrin
- C. Cadherin (Correct Answer)
- D. Claudin
- E. Cytokeratin
Tumor invasion and metastasis Explanation: ***Cadherin***
- **Cadherins** are calcium-dependent adhesion proteins that mediate cell-to-cell adhesion, particularly in epithelial tissues.
- A decrease in calcium concentration would directly impair cadherin function, leading to reduced cell adhesion and increased intercellular gaps.
*Actin*
- **Actin** is a component of the cell's cytoskeleton, involved in cell shape, motility, and intracellular transport, but not directly responsible for calcium-dependent cell adhesion between epithelial cells.
- While actin filaments interact with adhesion junctions, their primary role is structural and dynamic rather than adhesive.
*Integrin*
- **Integrins** are primarily involved in cell-to-extracellular matrix adhesion, connecting the cell to the surrounding matrix, not directly mediating calcium-dependent cell-to-cell adhesion between epithelial cells.
- They can be affected by intracellular calcium signaling but do not directly bind calcium to mediate their adhesive function in the same way cadherins do.
*Claudin*
- **Claudins** are key components of **tight junctions**, which regulate paracellular permeability and form a barrier between cells, but they are not directly responsible for calcium-dependent cell-to-cell adhesion, which is characteristic of adherens junctions.
- While tight junctions contribute to overall cell-cell contact, the observation of an *increased gap* suggests an issue with adhesive complexes like adherens junctions, where cadherins are prominent.
*Cytokeratin*
- **Cytokeratins** are intermediate filaments found in epithelial cells, providing structural support and mechanical strength.
- They are linked to desmosomes and hemidesmosomes but are not directly involved in calcium-dependent cell-to-cell adhesion.
Tumor invasion and metastasis US Medical PG Question 6: A 62-year-old woman presents to her oncologist to discuss the chemotherapy options for her newly diagnosed breast cancer. During the meeting, they discuss a drug that inhibits the breakdown of mitotic spindles in cells. Her oncologist explains that this will be more toxic to cancer cells because those cells are dividing more rapidly. Which of the following side effects is closely associated with the use of this chemotherapeutic agent?
- A. Photosensitivity
- B. Peripheral neuropathy (Correct Answer)
- C. Paralytic ileus
- D. Hemorrhagic cystitis
- E. Pulmonary fibrosis
Tumor invasion and metastasis Explanation: ***Peripheral neuropathy***
- Drugs that inhibit the breakdown of **mitotic spindles** are **microtubule-targeting agents** (e.g., **taxanes** like paclitaxel/docetaxel, **vinca alkaloids** like vincristine/vinblastine).
- These agents interfere with **microtubule function** in neurons, leading to **axonal damage** and **peripheral neuropathy**.
- This is the **most characteristic and common dose-limiting toxicity** of microtubule inhibitors, affecting sensory and motor nerves (numbness, tingling, weakness in extremities).
*Photosensitivity*
- **Photosensitivity** is a common adverse effect associated with certain chemotherapeutic agents like **fluorouracil** (5-FU) or **methotrexate**, but is not linked to microtubule inhibitors.
- It involves an increased sensitivity to UV light, often manifesting as a rash or exaggerated sunburn.
*Paralytic ileus*
- **Paralytic ileus** can occur with **vinca alkaloids** (especially vincristine) due to autonomic neuropathy affecting the **enteric nervous system**.
- However, this is **less common** than peripheral neuropathy and occurs more specifically with vincristine rather than taxanes.
- **Peripheral neuropathy** is the more pervasive, dose-limiting, and universally characteristic side effect across all microtubule inhibitors.
*Hemorrhagic cystitis*
- **Hemorrhagic cystitis** is a classic side effect of **alkylating agents** like **cyclophosphamide** and **ifosfamide**, which produce the toxic metabolite **acrolein**.
- It is prevented/managed with **mesna**, which inactivates acrolein.
- Not associated with microtubule inhibitors.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a known side effect of certain chemotherapeutic drugs, most notably **bleomycin** and **busulfan**.
- This adverse effect is not associated with agents that target **mitotic spindle breakdown**.
Tumor invasion and metastasis US Medical PG Question 7: A 76-year-old woman comes to the physician for evaluation of a 3-month history of vulvar itching and pain. She was diagnosed with lichen sclerosus 4 years ago. She has smoked 1 pack of cigarettes daily for 35 years. Physical examination shows a 2.5-cm nodular, ulcerative lesion on the vaginal introitus and left labia minora with surrounding erythema. Punch biopsy shows squamous cell carcinoma. A CT scan of the chest, abdomen, and pelvis shows enlarged lymph nodes concerning for metastatic disease. Which of the following lymph node regions is the most likely primary site of metastasis?
- A. Superficial inguinal (Correct Answer)
- B. Internal iliac
- C. External iliac
- D. Inferior mesenteric
- E. Para-aortic
Tumor invasion and metastasis Explanation: ***Superficial inguinal***
- The **vulva** drains primarily into the **superficial inguinal lymph nodes**, making them the most likely first site for metastatic spread from vulvar squamous cell carcinoma.
- The lesion's location on the **vaginal introitus** and **labia minora** directly correlates with this lymphatic drainage pathway.
*Internal iliac*
- **Internal iliac nodes** receive drainage mainly from deep pelvic structures like the cervix, upper vagina, and uterus, not directly from the vulva.
- Metastasis to these nodes usually occurs after involvement of more superficial nodes or in advanced disease with deeper invasion.
*External iliac*
- **External iliac nodes** generally drain the lower extremities and deeper pelvic structures (e.g., bladder, distal ureter), not the vulva as a primary site.
- Involvement here would typically indicate more advanced local spread or secondary metastasis from other pelvic nodes.
*Inferior mesenteric*
- **Inferior mesenteric nodes** drain the hindgut and its derivatives, including the distal colon and rectum, which are distant from the vulva.
- This region is not involved in the lymphatic drainage of the vulva.
*Para-aortic*
- **Para-aortic nodes** drain structures like the ovaries, fallopian tubes, and upper uterus; they are too superior for primary vulvar lymphatic drainage.
- Metastasis to these nodes from vulvar cancer would signify widespread, very advanced disease and not a primary site of spread.
Tumor invasion and metastasis US Medical PG Question 8: A 78-year-old man receives chemotherapy for advanced hepatocellular carcinoma. Despite appropriate therapy, he dies 4 months later. Histopathological examination of the cancer cells shows the presence of a transmembrane efflux pump protein that is known to cause decreased intracellular concentrations of chemotherapeutic drugs. Which of the following best describes this membrane protein?
- A. G protein
- B. Cadherin
- C. P-glycoprotein (Correct Answer)
- D. Tyrosine receptor
- E. Channel protein
Tumor invasion and metastasis Explanation: **P-glycoprotein**
- **P-glycoprotein** (also known as **MDR1**) is a well-known **efflux pump** that actively transports many chemotherapy drugs out of cancer cells, leading to **multidrug resistance**.
- Its presence explains the **decreased intracellular concentrations** of chemotherapy drugs and the poor response to treatment in this patient.
*G protein*
- **G proteins** are intracellular signaling molecules that mediate responses to various extracellular stimuli, not primarily involved in drug efflux.
- They are typically associated with **G protein-coupled receptors** and downstream signaling pathways, not direct drug transport.
*Cadherin*
- **Cadherins** are cell adhesion molecules that play a crucial role in cell-cell binding and maintaining tissue structure.
- They are not involved in the active transport of drugs across the cell membrane.
*Tyrosine receptor*
- **Tyrosine kinase receptors** are transmembrane proteins that bind to growth factors and initiate intracellular signaling cascades, promoting cell growth and differentiation.
- They are involved in signaling, not in the active transport of chemotherapy drugs out of the cell.
*Channel protein*
- **Channel proteins** facilitate the passive diffusion of ions or small molecules across the cell membrane, typically down their electrochemical gradient.
- While they are transmembrane proteins, they do not actively pump drugs out against a concentration gradient, which is characteristic of multidrug resistance.
Tumor invasion and metastasis US Medical PG Question 9: A 62-year-old man seeks evaluation at a local walk-in clinic for mid-low back pain of several weeks. He has tried different rehabilitation therapies and medications with no improvement. He was prescribed some pain medications and sent home last week, but the patient presents today with difficulty walking and worsening of his back pain. He was referred to the ER, where he was examined and found to have hypoesthesia from T12 to S4–S5, significant muscle weakness in both lower limbs, and reduced knee and ankle deep tendon reflexes. A hypotonic anal sphincter with conserved deep anal pressure was demonstrated on digital rectal examination, as well as a multinodular, asymmetric prostate. Imaging studies showed multiple sclerotic bone lesions along the spine. Subsequently, a prostate core biopsy was obtained which confirmed the diagnosis of prostate cancer. Which of the following characteristics would you expect in the specimen?
- A. Well-formed glands with an increase in interglandular stroma
- B. Fat invasion
- C. Prostatic intraepithelial neoplasia
- D. Small, closely-packed, well-formed glands
- E. Perineural invasion (Correct Answer)
Tumor invasion and metastasis Explanation: ***Perineural invasion***
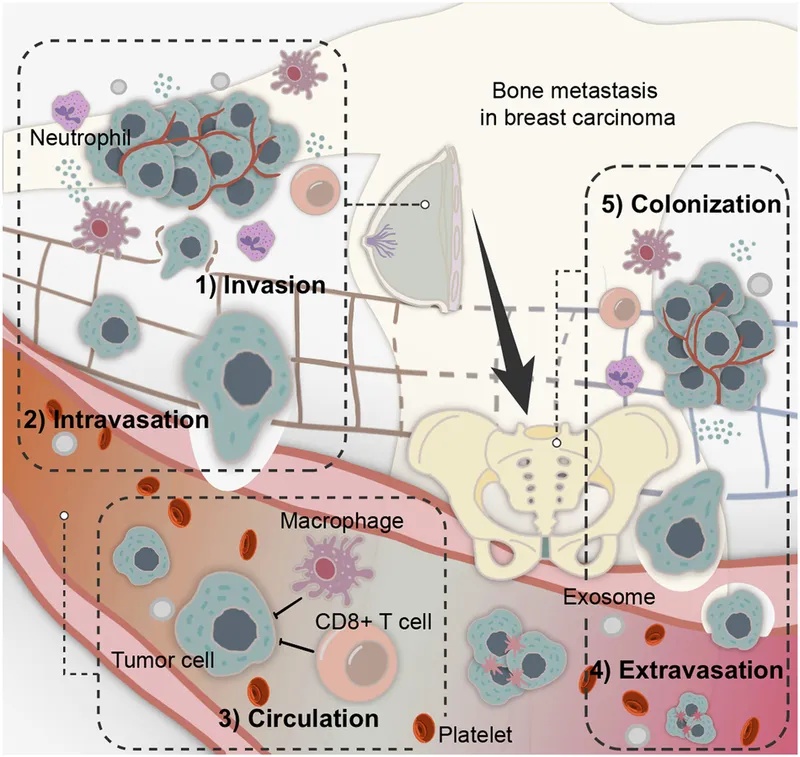
- **Perineural invasion** is a common finding in prostate adenocarcinoma, indicating that cancer cells have invaded the nerves surrounding the prostatic glands. This feature is often associated with a higher Gleason score and increased likelihood of extraprostatic extension and metastasis.
- While not visible on gross examination, its presence on biopsy can influence staging and treatment decisions for prostate cancer, particularly regarding the risk of recurrence and spread to other tissues.
*Well-formed glands with an increase in interglandular stroma*
- This description is more indicative of **benign prostatic hyperplasia (BPH)**, a non-cancerous enlargement of the prostate, characterized by an increase in both glandular and stromal components.
- In BPH, the glands typically remain well-formed, and the stroma often proliferates, but these features do not represent malignancy.
*Fat invasion*
- **Fat invasion** is not a typical characteristic of prostate cancer within the prostate gland itself, as the prostate is not primarily composed of fat.
- While prostate cancer can invade periprostatic fatty tissue if it extends beyond the prostatic capsule, fat invasion within the biopsy specimen from the prostate proper is not a diagnostic feature of adenocarcinoma.
*Prostatic intraepithelial neoplasia*
- **Prostatic intraepithelial neoplasia (PIN)** is a pre-malignant lesion where the prostatic ductal and acinar cells show cytologic atypia but remain confined within the basement membrane.
- While PIN (especially high-grade PIN) can be associated with prostate cancer and may precede its development, it is not cancer itself and is not the definitive diagnosis in this case where prostate cancer has been confirmed.
*Small, closely-packed, well-formed glands*
- This description could represent a **low-grade prostate adenocarcinoma** (Gleason pattern 3), where the glands are still relatively well-formed but are more numerous and crowded than in benign tissue.
- However, compared to perineural invasion, which is a more definitive sign of aggressive behavior and advanced disease in a patient presenting with metastatic features (sclerotic bone lesions, neurologic symptoms), this histological finding alone is less specific for the advanced cancer described.
Tumor invasion and metastasis US Medical PG Question 10: A 61-year-old Caucasian male presents to your office complaining of morning headaches of 6 weeks duration. A head MRI reveals a likely metastasis of unknown origin in the supratentorial region of the brain. On biopsy, the neoplastic mass is shown to have a mutation in BRAF, a protein kinase, in which a glutamic acid is substituted for valine at position 600 of the protein. Where did this metastasis most likely originate?
- A. Stomach
- B. Skin (Correct Answer)
- C. Breast
- D. Brain
- E. Bone
Tumor invasion and metastasis Explanation: ***Skin***
- A brain metastasis with a **V600E BRAF mutation** is highly suggestive of **melanoma**, a type of skin cancer.
- Melanoma frequently metastasizes to the **brain**, and the BRAF V600E mutation is a common and actionable target in advanced melanoma.
*Stomach*
- Stomach cancers (gastric adenocarcinomas) less commonly metastasize to the brain compared to melanoma.
- While BRAF mutations can occur in gastric cancer, the **V600E mutation** is not typically a defining feature of gastric cancer metastases to the brain.
*Breast*
- Breast cancer can metastasize to the brain, but the presence of a **BRAF V600E mutation** is not a characteristic genetic alteration for breast cancer.
- Common mutations in breast cancer include those in **ER, PR, and HER2** receptors or **PIK3CA**, not BRAF V600E.
*Brain*
- The question states the mass is a **metastasis of unknown origin**, implying it did not originate in the brain itself.
- Primary brain tumors like **gliomas** would not be described as metastases and have a different mutational spectrum.
*Bone*
- Bone cancers (sarcomas) or metastases to the bone usually do not present with a **BRAF V600E mutation** as their primary driver for brain metastasis.
- While various cancers can metastasize to bone, the specific mutation points away from a bone origin.
More Tumor invasion and metastasis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.