Nomenclature of neoplasms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nomenclature of neoplasms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nomenclature of neoplasms US Medical PG Question 1: A 65-year-old man with a 40-pack-year smoking history presents with hemoptysis and a persistent cough. Chest CT shows a 3.5 cm centrally located mass in the right main bronchus. Positron emission tomography confirms a malignant nodule. Bronchoscopy with transbronchial biopsy is performed and a specimen sample of the nodule is sent for frozen section analysis. The tissue sample is most likely to show which of the following tumor types?
- A. Carcinoid tumor
- B. Metastasis of colorectal cancer
- C. Small cell lung carcinoma
- D. Large cell carcinoma
- E. Squamous cell carcinoma (Correct Answer)
Nomenclature of neoplasms Explanation: ***Squamous cell carcinoma***
- This is the most likely diagnosis given the **central location** in the main bronchus, **heavy smoking history**, and presentation with **hemoptysis**.
- **Squamous cell carcinoma** accounts for 25-30% of lung cancers and characteristically arises in **central/proximal airways**, making it readily accessible by **bronchoscopy**.
- Histologically, it shows **keratin pearls** and **intercellular bridges** on biopsy.
- The **central endobronchial location** and ability to obtain tissue via transbronchial biopsy strongly favor squamous cell over peripheral tumors.
*Carcinoid tumor*
- **Carcinoid tumors** are **neuroendocrine tumors** that can present as central endobronchial masses and cause hemoptysis.
- However, they are typically **slow-growing** with more indolent presentation, and PET scans show **variable uptake** (often less intense than aggressive carcinomas).
- They represent only **1-2% of lung tumors** and occur more commonly in **younger, non-smoking patients**.
*Metastasis of colorectal cancer*
- While lung is a common site for **colorectal metastases**, these typically present as **multiple peripheral nodules** rather than a solitary central endobronchial mass.
- The clinical presentation strongly suggests **primary lung cancer** rather than metastatic disease.
- Without history of colorectal cancer, this is unlikely.
*Small cell lung carcinoma*
- **Small cell lung carcinoma** (SCLC) represents 15% of lung cancers and typically presents as a **large central mass** with early mediastinal involvement.
- However, SCLC is usually **too extensive at presentation** for transbronchial biopsy alone and often requires mediastinoscopy or CT-guided biopsy.
- Histology shows **small cells with scant cytoplasm**, **salt-and-pepper chromatin**, and **oat-cell morphology**.
- While possible, the single accessible endobronchial mass is more characteristic of squamous cell.
*Large cell carcinoma*
- **Large cell carcinoma** is a **diagnosis of exclusion** made when tumors lack features of adenocarcinoma, squamous cell, or small cell differentiation.
- It typically presents as **large peripheral masses** rather than central endobronchial lesions.
- It represents only **10% of lung cancers** and is less common than squamous cell carcinoma in this clinical scenario.
Nomenclature of neoplasms US Medical PG Question 2: A 53-year-old farmer presents to the clinic for evaluation of a pigmented lesion on his arm. He states that he first noticed the lesion last year, but he believes that it has been slowly growing in size. He otherwise does not have any complaints and is generally healthy. Which of the following findings on physical exam would suggest a malignant diagnosis?
- A. Symmetrical ovoid lesion
- B. Flat lesion with symmetric hyperpigmentation
- C. Tenderness to palpation
- D. Hyperpigmented lesion with smooth borders
- E. Different pigmentation throughout the lesion (Correct Answer)
Nomenclature of neoplasms Explanation: ***Different pigmentation throughout the lesion***
- **Malignant melanoma** often presents with **multicolor variegation** or areas of differing pigmentation within the same lesion, which is a key indicator for malignancy (the "C" in ABCDE).
- This **uneven coloration** reflects the uncontrolled proliferation of melanocytes producing melanin in varying amounts and patterns, a hallmark of dysplastic changes.
*Symmetrical ovoid lesion*
- **Benign nevi** (moles) typically maintain **symmetry** in their shape and border, meaning that if you were to draw a line through the middle of the lesion, both halves would largely match.
- While some melanomas can be ovoid, **asymmetry** is a more concerning feature for malignancy, unlike the description provided here.
*Flat lesion with symmetric hyperpigmentation*
- A **benign lesion** often has **symmetric pigmentation** and a uniform color distribution, with a flat appearance.
- **Irregular pigmentation** (color variegation) within the lesion is a more concerning sign for **melanoma**, falling under the "C" (color) criteria of the ABCDEs.
*Tenderness to palpation*
- **Tenderness** is not a typical characteristic of early or even advanced **melanoma**; pain or tenderness is often associated with inflammation, infection, or trauma rather than primary skin cancer.
- While ulcerated or infected tumors can be painful, tenderness alone without other suspicious features is **not a primary diagnostic criterion** for melanoma.
*Hyperpigmented lesion with smooth borders*
- **Benign moles** typically have **smooth, regular, and well-defined borders**, making them appear round or oval.
- In contrast, **malignant melanoma** often presents with **irregular, notched, or poorly defined borders (the "B" in ABCDE),** which would be more indicative of malignancy.
Nomenclature of neoplasms US Medical PG Question 3: A 24-year-old woman with a past medical history significant only for endometriosis presents to the outpatient clinic with a 2-cm left breast mass that she first identified 6 months earlier. On review of systems, the patient states that the mass is not painful and, by her estimation, has not significantly increased in size since she first noticed it. On physical examination, there is a palpable, round, rubbery, mobile mass approximately 2 cm in diameter. Given the lesion’s characteristics and the patient’s demographics, what is the most likely diagnosis?
- A. Fibrocystic change
- B. Invasive breast carcinoma
- C. Fibroadenoma (Correct Answer)
- D. Phyllodes tumor
- E. Ductal carcinoma in situ
Nomenclature of neoplasms Explanation: ***Fibroadenoma***
- This diagnosis is supported by the patient's age (young woman), the **rubbery, mobile, well-circumscribed** nature of the mass, and its slow growth over 6 months without pain.
- Fibroadenomas are **benign tumors** made of both fibrous and glandular tissue, and their characteristics typically match this presentation.
*Fibrocystic change*
- While common in young women, fibrocystic changes often manifest as **multiple cysts**, generalized breast tenderness, or cyclical pain related to menstruation.
- The description of a single, non-tender, rubbery mass is less typical for fibrocystic changes.
*Invasive breast carcinoma*
- Though possible, **invasive breast cancer** in a 24-year-old woman is less common, and typically presents with a **hard, irregular, fixed mass** that may be painful or associated with skin changes.
- The description of a **rubbery, mobile** lesion not significantly increasing in size makes this less likely.
*Phyllodes tumor*
- This tumor is characterized by **rapid growth** and often reaches a large size, which is not consistent with the patient's report of slow growth over 6 months.
- While it can be benign, borderline, or malignant, its typical presentation is **faster-growing** than described.
*Ductal carcinoma in situ*
- **Ductal carcinoma in situ (DCIS)** is a non-invasive form of breast cancer that usually presents as **microcalcifications on mammography** and is often non-palpable.
- When palpable, it is typically a poorly defined lump, not a rubbery, mobile, well-circumscribed mass.
Nomenclature of neoplasms US Medical PG Question 4: A 27-year-old woman presents to her primary care physician because of headaches that she has had over the last three weeks. She has not had any significant past medical history though she does recall that various types of cancer run in her family. She has also noticed that she has been gaining some weight, and her feet no longer fit into her favorite shoes. On presentation, her temperature is 98.6°F (37°C), blood pressure is 159/92 mmHg, pulse is 75/min, and respirations are 16/min. Physical exam reveals 1+ edema in her lower extremities bilaterally. She is placed on captopril and presents to the emergency department two weeks later after a minor motor vehicle accident. She is cleared of any serious injuries, and as part of her workup, labs are drawn with the following results:
BUN: 47 mg/dL
Creatinine: 1.4 mg/dL
Which of the following findings would most likely also be seen in this patient?
- A. Mass present in adrenal cortex
- B. Atherosclerotic plaques blocking blood flow
- C. Mass present in adrenal medulla
- D. No lesions present
- E. String-of-beads appearance on angiography (Correct Answer)
Nomenclature of neoplasms Explanation: ***String-of-beads appearance on angiography***
- The patient's symptoms of **headaches**, **weight gain**, **bilateral lower extremity edema**, and **hypertension** (159/92 mmHg) in a young woman, especially with the presentation of acute kidney injury after beginning an ACE inhibitor (captopril), are highly suggestive of **renovascular hypertension** due to **fibromuscular dysplasia (FMD)**.
- FMD characteristically presents as a **"string-of-beads"** appearance on renal angiography due to areas of stenosis alternating with aneurysmal dilations in the renal arteries.
*Mass present in adrenal cortex*
- A mass in the adrenal cortex typically causes **hyperaldosteronism (Conn syndrome)** or **Cushing's syndrome**. While hyperaldosteronism can cause hypertension and hypokalemia, it does not explain the acute kidney injury with ACE inhibitor treatment.
- Cushing's syndrome involves **central obesity**, **moon facies**, and **striae**, which are not described.
*Atherosclerotic plaques blocking blood flow*
- **Atherosclerotic renovascular disease** typically affects older individuals with a history of cardiovascular risk factors (diabetes, hyperlipidemia, smoking). This patient is young and has no such history.
- While it can cause renal artery stenosis and acute kidney injury with ACE inhibitors, the demographic profile does not fit.
*Mass present in adrenal medulla*
- A mass in the adrenal medulla suggests a **pheochromocytoma**, which causes **episodic hypertension**, **palpitations**, **sweating**, and **anxiety**.
- The patient's hypertension is sustained, and she does not present with classic symptoms of a pheochromocytoma.
*No lesions present*
- The patient's clinical presentation, including the development of acute kidney injury after starting captopril, strongly indicates an underlying renovascular pathology.
- The absence of lesions would not explain the severe, sustained hypertension and the adverse reaction to captopril.
Nomenclature of neoplasms US Medical PG Question 5: A 59-year-old man comes to the physician for evaluation of a progressively enlarging, 8-mm skin lesion on the right shoulder that developed 1 month ago. The patient has a light-skinned complexion and has had several dysplastic nevi removed in the past. A photograph of the lesion is shown. The lesion is most likely derived from cells that are also the embryological origin of which of the following tumors?
- A. Adrenal adenoma
- B. Liposarcoma
- C. Basal cell carcinoma
- D. Neuroblastoma (Correct Answer)
- E. Medullary thyroid cancer
Nomenclature of neoplasms Explanation: ***Neuroblastoma***
- The skin lesion described, with history of dysplastic nevi and progressive growth, is highly suggestive of **melanoma**. Melanoma arises from **melanocytes**, which are derived from the **neural crest**.
- **Neuroblastoma** is a tumor of the **sympathetic nervous system** that also originates from **neural crest cells**, making it the correct embryological match.
- Neuroblastoma is the **classic example** of a neural crest-derived tumor taught alongside melanoma in medical education.
*Adrenal adenoma*
- **Adrenal adenomas** are benign tumors of the adrenal cortex, which is derived from the **mesoderm**.
- This embryological origin is distinct from the neural crest origin of melanocytes.
*Liposarcoma*
- **Liposarcomas** are malignant tumors of adipose tissue, which arises from the **mesoderm**.
- This origin does not match the neural crest origin of melanocytes.
*Basal cell carcinoma*
- **Basal cell carcinoma** originates from the **basal layer of the epidermis**, which is derived from **surface ectoderm** (not neural crest).
- While it's an ectodermal derivative, it does not share the neural crest origin of melanocytes.
*Medullary thyroid cancer*
- **Medullary thyroid cancer** originates from the **parafollicular C cells** of the thyroid gland, which are also derived from the **neural crest**.
- While this shares the same embryological origin as melanoma, **neuroblastoma** is the more commonly tested and classic pairing with melanoma in standard medical examinations when discussing neural crest-derived tumors.
Nomenclature of neoplasms US Medical PG Question 6: A 32-year-old woman presents to her primary care physician for an annual checkup. She reports that she has been feeling well and has no medical concerns. Her past medical history is significant for childhood asthma but she has not experienced any symptoms since she was a teenager. Physical exam reveals a 1-centimeter hard mobile mass in the left upper outer quadrant of her breast. A mammogram was performed and demonstrated calcifications within the mass so a biopsy was obtained. The biopsy shows acinar proliferation with intralobular fibrosis. Which of the following conditions is most likely affecting this patient?
- A. Sclerosing adenosis (Correct Answer)
- B. Fibroadenoma
- C. Cystic hyperplasia
- D. Invasive lobular carcinoma
- E. Infiltrating ductal carcinoma
Nomenclature of neoplasms Explanation: ***Sclerosing adenosis***
- This condition is characterized by **acinar proliferation with intralobular fibrosis**, which exactly matches the biopsy findings mentioned in the vignette.
- Sclerosing adenosis can present as a palpable mass with **calcifications on mammography**, mimicking carcinoma, necessitating biopsy for definitive diagnosis.
*Fibroadenoma*
- Characterized by proliferation of both **stromal and epithelial elements**, often forming well-circumscribed, mobile masses.
- While it can present as a mobile mass, the specific histological finding of "acinar proliferation with intralobular fibrosis" is not the primary descriptive characteristic of a fibroadenoma.
*Cystic hyperplasia*
- This term, often used interchangeably with **fibrocystic changes**, involves the formation of cysts and an increase in fibrous tissue.
- While it can involve hyperplasia, it doesn't typically describe the distinct pattern of "acinar proliferation with intralobular fibrosis" as seen in sclerosing adenosis.
*Invasive lobular carcinoma*
- This carcinoma is characterized by its **infiltrative growth pattern** often in single file lines, and typically does not form a well-defined mass.
- While it can present with calcifications, the absence of overt malignant features and the specific benign histological description rule out this diagnosis.
*Infiltrating ductal carcinoma*
- The most common type of breast cancer, characterized by **malignant epithelial cells infiltrating the stroma**.
- The biopsy findings described ("acinar proliferation with intralobular fibrosis") are features of a benign process, not a malignant one.
Nomenclature of neoplasms US Medical PG Question 7: A 65-year-old man is admitted to the hospital because of a 1-month history of fatigue, intermittent fever, and weakness. Results from a peripheral blood smear taken during his evaluation are indicative of possible acute myeloid leukemia. Bone marrow aspiration and subsequent cytogenetic studies confirm the diagnosis. The physician sets aside an appointed time-slot and arranges a meeting in a quiet office to inform him about the diagnosis and discuss his options. He has been encouraged to bring someone along to the appointment if he wanted. He comes to your office at the appointed time with his daughter. He appears relaxed, with a full range of affect. Which of the following is the most appropriate opening statement in this situation?
- A. Your lab reports show that you have an acute myeloid leukemia
- B. What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies? (Correct Answer)
- C. You must be curious and maybe even anxious about the results of your tests.
- D. I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.
- E. Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?
Nomenclature of neoplasms Explanation: ***"What is your understanding of the reasons we did bone marrow aspiration and cytogenetic studies?"***
- This **open-ended question** allows the patient to express their current knowledge and perceptions, which helps the physician tailor the discussion.
- It establishes a **patient-centered approach**, respecting the patient's existing understanding and preparing them for further information.
*"You must be curious and maybe even anxious about the results of your tests."*
- While empathic, this statement makes an **assumption about the patient's feelings** rather than inviting them to share their own.
- It is often better to ask directly or use more open-ended questions that allow the patient to express their true emotions, especially given their **relaxed demeanor**.
*"I may need to refer you to a blood cancer specialist because of your diagnosis. You may need chemotherapy or radiotherapy, which we are not equipped for.”"*
- This statement immediately introduces **overwhelming and potentially alarming information** (referral, chemotherapy, radiotherapy) without first establishing the diagnosis or assessing the patient's readiness to receive it.
- It prematurely jumps to treatment and logistics, potentially causing **unnecessary distress** before the patient has processed the core diagnosis.
*"Would you like to know all the details of your diagnosis, or would you prefer I just explain to you what our options are?""*
- While it attempts to assess the patient's preference for information, this question is a **closed-ended "either/or" choice** that might limit the patient's ability to express nuanced needs.
- It also prematurely introduces the idea of "options" without first explaining the diagnosis in an understandable context.
*"Your lab reports show that you have an acute myeloid leukemia"*
- This is a **direct and blunt delivery of a serious diagnosis** without any preparatory context or assessment of the patient's existing knowledge or emotional state.
- Delivering such news abruptly can be shocking and overwhelming, potentially **hindering effective communication** and rapport building.
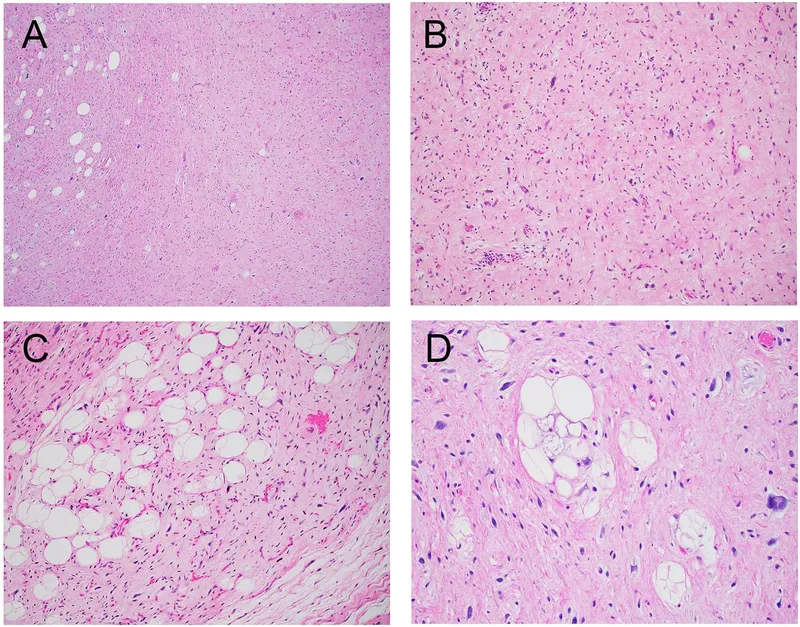
Nomenclature of neoplasms US Medical PG Question 8: An 82-year-old woman presents to the emergency department because of excruciating right flank pain and fever for the past 2 days. She states that she is having trouble urinating. Her past medical history is unremarkable. A urinalysis is performed and comes back positive for leukocytes and gram-negative bacilli. A contrast computed tomography of the abdomen is performed and reveals a large retroperitoneal mass compressing the right ureter, leading to hydronephrosis of the right kidney. The mass is excised. Histopathologic evaluation of the mass is shown in the image below, and it is determined to be malignant. Which of the following is the most likely diagnosis in this patient?
- A. Rhabdomyosarcoma
- B. Leiomyosarcoma
- C. Lipoma
- D. Teratoma
- E. Liposarcoma (Correct Answer)
Nomenclature of neoplasms Explanation: ***Liposarcoma***
- The **most common primary malignant retroperitoneal tumor** in adults, particularly in elderly patients
- Characteristically presents as a **large retroperitoneal mass** causing compressive symptoms such as hydronephrosis
- **Histopathological features** include pleomorphic lipoblasts with varying degrees of differentiation (well-differentiated, dedifferentiated, myxoid, or pleomorphic subtypes)
- The clinical presentation of an elderly patient with a malignant retroperitoneal mass strongly suggests this diagnosis
*Rhabdomyosarcoma*
- Primarily a **pediatric malignancy**, most common in children and young adults under 20 years old
- Most frequently arises in the **head and neck, genitourinary tract, or extremities**, not typically retroperitoneal
- Histologically shows skeletal muscle differentiation with rhabdomyoblasts, not lipoblastic features
*Leiomyosarcoma*
- More commonly found in the **uterus, gastrointestinal tract, or blood vessels**
- While it can occur in the retroperitoneum, it is **less common** than liposarcoma in this location
- Histologically demonstrates **smooth muscle differentiation** with spindle cells, not the lipoblastic features characteristic of the described mass
*Lipoma*
- A **benign tumor** composed of mature adipose tissue without cellular atypia
- Would not present as a **malignant mass** on histopathologic evaluation
- Generally asymptomatic and slow-growing; unlikely to cause severe symptoms like excruciating pain or obstructive hydronephrosis
*Teratoma*
- Contains tissue derived from **all three germ layers** (ectoderm, mesoderm, endoderm)
- More commonly associated with **gonadal or midline structures** (ovaries, testes, mediastinum)
- Rare in the retroperitoneum in elderly patients; histology would show diverse tissue types rather than predominantly lipoblastic features
Nomenclature of neoplasms US Medical PG Question 9: A 67-year-old man comes to the physician because of a 4-month history of fatigue and weight loss. Physical examination shows jaundice. The liver is palpated 3 cm below the right costal margin. Serum studies show an elevated alpha-fetoprotein and a prolonged prothrombin time. Genetic analysis of a liver biopsy specimen shows a G:C to T:A transversion in codon 249 of the gene coding for the TP53 protein in affected cells. Which of the following risk factors is most specific to the patient's condition?
- A. Dietary aflatoxin exposure (Correct Answer)
- B. Alcoholism
- C. Schistosomiasis
- D. Hemochromatosis
- E. Hepatitis C infection
Nomenclature of neoplasms Explanation: ***Dietary aflatoxin exposure***
- The **TP53 mutation** (G:C to T:A transversion at codon 249) is a **signature mutation** strongly associated with **aflatoxin B1 exposure**, particularly in hepatocellular carcinoma.
- Aflatoxins are potent **carcinogens produced by Aspergillus fungi**, often found in contaminated food storage in tropical regions.
*Schistosomiasis*
- This parasitic infection is a risk factor for **squamous cell carcinoma of the bladder** and, to a lesser extent, **cholangiocarcinoma**, but not typically hepatocellular carcinoma with this specific TP53 mutation signature.
- It primarily affects the **urinary bladder** and intestines, leading to chronic inflammation and fibrosis.
*Alcoholism*
- Chronic alcoholism is a major risk factor for **cirrhosis** and **hepatocellular carcinoma** due to continuous liver damage and regeneration.
- However, it does not typically cause the **specific TP53 codon 249 mutation** seen in this patient.
*Hemochromatosis*
- This genetic disorder causes **iron overload**, leading to liver damage, **cirrhosis**, and an increased risk of **hepatocellular carcinoma**.
- While it predisposes to liver cancer, it is not associated with the **specific G:C to T:A TP53 mutation** described.
*Hepatitis C infection*
- Chronic hepatitis C is a leading cause of **cirrhosis** and **hepatocellular carcinoma** worldwide due to chronic inflammation and hepatocyte turnover.
- Similar to alcoholism, it is a significant risk factor for liver cancer but does not specifically cause the **TP53 codon 249 mutation** linked to aflatoxin.
Nomenclature of neoplasms US Medical PG Question 10: A 33-year-old woman comes to the physician 1 week after noticing a lump in her right breast. Fifteen years ago, she was diagnosed with osteosarcoma of her left distal femur. Her father died of an adrenocortical carcinoma at the age of 41 years. Examination shows a 2-cm, firm, immobile mass in the lower outer quadrant of the right breast. A core needle biopsy of the mass shows adenocarcinoma. Genetic analysis in this patient is most likely to show a defect in which of the following genes?
- A. BRCA1
- B. KRAS
- C. TP53 (Correct Answer)
- D. Rb
- E. PTEN
Nomenclature of neoplasms Explanation: ***TP53***
- This patient's presentation with **early-onset breast cancer**, a history of **osteosarcoma** at a young age, and a father's death from **adrenocortical carcinoma** at 41 years strongly suggests **Li-Fraumeni syndrome**.
- Li-Fraumeni syndrome is an autosomal dominant disorder caused by a germline mutation in the **tumor suppressor gene TP53**, increasing the risk for multiple primary cancers at a young age.
*BRCA1*
- While **BRCA1 mutations** are associated with an increased risk of breast and ovarian cancer, they are not typically linked to osteosarcoma or adrenocortical carcinoma.
- The constellation of cancers in this patient is more indicative of Li-Fraumeni syndrome than solely a BRCA1-related cancer syndrome.
*KRAS*
- **KRAS** is an oncogene commonly mutated in several cancers, including pancreatic, colorectal, and lung cancer, but is not primarily associated with either Li-Fraumeni syndrome or the specific tumors seen in this family history.
- Mutations in KRAS are typically somatic mutations acquired during a person's lifetime, not germline mutations causing inherited cancer syndromes like the one suggested here.
*Rb*
- Mutations in the **retinoblastoma (Rb) gene** are associated with retinoblastoma and an increased risk of osteosarcoma, but not typically with adrenocortical carcinoma or breast cancer as part of a classic inherited syndrome.
- The combination of breast cancer, osteosarcoma, and adrenocortical carcinoma points more specifically to TP53.
*PTEN*
- **PTEN mutations** are associated with Cowden syndrome, which increases the risk for breast cancer, thyroid cancer, and endometrial cancer, along with benign growths.
- However, Cowden syndrome does not typically include osteosarcoma or adrenocortical carcinoma as prominent features, making PTEN less likely than TP53 for this specific family history.
More Nomenclature of neoplasms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.