Wound healing and repair US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Wound healing and repair. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Wound healing and repair US Medical PG Question 1: A 55-year-old African American female presents to her breast surgeon for a six-month follow-up visit after undergoing a modified radical mastectomy for invasive ductal carcinoma of the left breast. She reports that she feels well and her pain has been well controlled with ibuprofen. However, she is frustrated that her incisional scar is much larger than she expected. She denies any pain or pruritus associated with the scar. Her past medical history is notable for systemic lupus erythematosus and multiple dermatofibromas on her lower extremities. She has had no other surgeries. She currently takes hydroxychloroquine. On examination, a raised hyperpigmented rubbery scar is noted at the inferior border of the left breast. It appears to have extended beyond the boundaries of the initial incision. Left arm range of motion is limited due to pain at the incisional site. Abnormal deposition of which of the following molecules is most likely responsible for the appearance of this patient’s scar?
- A. Type III collagen
- B. Proteoglycan
- C. Elastin
- D. Type I collagen (Correct Answer)
- E. Type II collagen
Wound healing and repair Explanation: ***Correct: Type I collagen***
- Keloids are characterized by an **overgrowth of dense, disorganized type I collagen fibers** that extend beyond the original wound boundaries. The patient's scar is described as a **"raised, hyperpigmented, rubbery scar" that "extended beyond the boundaries of the initial incision,"** which is characteristic of a keloid.
- Patients with **African American ethnicity**, a history of **dermatofibromas** (which can predispose to keloid formation), and a lack of pain or pruritus are all consistent with a keloid.
- Type I collagen comprises **over 80% of the collagen in mature keloid tissue** and accounts for the characteristic firm, raised appearance.
*Incorrect: Type III collagen*
- **Type III collagen** is prominent during the **initial proliferative phase of wound healing** and is later replaced by type I collagen in mature scars.
- While present early in wound healing, its excessive deposition is not the primary feature of a **mature keloid** that extends beyond the wound margins.
- Normal scars have a type I to type III collagen ratio of approximately 4:1, while keloids have a much higher ratio.
*Incorrect: Proteoglycan*
- **Proteoglycans**, such as decorin and biglycan, are components of the extracellular matrix that play a role in collagen fibril assembly and tissue hydration.
- Although proteoglycans are found in keloids, their **abnormal deposition** is secondary to the extensive collagen formation and not the primary structural molecule responsible for the bulk and characteristic appearance of the scar.
*Incorrect: Elastin*
- **Elastin** provides **elasticity and recoil** to tissues, such as skin, blood vessels, and ligaments.
- Keloids are characterized by **fibrosis and rigidity**, not increased elasticity, and abnormal elastin deposition is not the hallmark of their pathogenesis.
*Incorrect: Type II collagen*
- **Type II collagen** is primarily found in **hyaline cartilage** and vitreous humor, providing resistance to intermittent pressure.
- It is **not a significant component of skin or scar tissue**, making its abnormal deposition irrelevant to the pathogenesis of cutaneous keloids.
Wound healing and repair US Medical PG Question 2: A 52-year-old woman sees you in your office with a complaint of new-onset headaches over the past few weeks. On exam, you find a 2 x 2 cm dark, irregularly shaped, pigmented lesion on her back. She is concerned because her father recently passed away from skin cancer. What tissue type most directly gives rise to the lesion this patient is experiencing?
- A. Neural crest cells (Correct Answer)
- B. Endoderm
- C. Mesoderm
- D. Ectoderm
- E. Neuroectoderm
Wound healing and repair Explanation: ***Neural crest cells***
- The suspected lesion, given its description and the patient's family history of skin cancer, is likely a **melanoma**.
- Melanoma originates from **melanocytes**, which are derived from **neural crest cells** during embryonic development.
*Endoderm*
- The endoderm gives rise to the **lining of the gastrointestinal and respiratory tracts**, as well as organs such as the liver and pancreas.
- It is not involved in the formation of melanocytes or skin lesions like melanoma.
*Mesoderm*
- The mesoderm forms tissues such as **muscle, bone, cartilage, connective tissue**, and the circulatory system.
- It does not directly give rise to melanocytes, which are the cells of origin for melanoma.
*Ectoderm*
- The ectoderm gives rise to the **epidermis, nervous system**, and sensory organs.
- While melanocytes are found in the epidermis, they are specifically derived from the **neural crest (a sub-population of ectoderm)**, not the general ectoderm.
*Neuroectoderm*
- Neuroectoderm specifically refers to the ectoderm that develops into the **nervous system**.
- While neural crest cells originate from the neuroectoderm, "neural crest cells" is a more precise answer for the origin of melanocytes.
Wound healing and repair US Medical PG Question 3: A 60-year-old male presents with fatigue, dyspnea on exertion, and lower extremity edema. Physical examination reveals an elevated jugular venous pressure and an S3 heart sound. Which of the following medications is most likely to improve this patient's symptoms?
- A. Metoprolol
- B. Furosemide (Correct Answer)
- C. Losartan
- D. Lisinopril
- E. Spironolactone
Wound healing and repair Explanation: ***Correct: Furosemide***
- The patient presents with classic signs of **heart failure with fluid overload**: dyspnea on exertion, lower extremity edema, elevated jugular venous pressure, and an S3 heart sound (indicating volume overload).
- **Furosemide**, a **loop diuretic**, is the most effective medication for **rapid symptomatic relief** in heart failure with congestion. It works by blocking sodium and water reabsorption in the loop of Henle, promoting diuresis and reducing **pulmonary congestion** and **peripheral edema**.
- While other medications like ACE inhibitors, beta-blockers, and aldosterone antagonists are crucial for **long-term mortality reduction** and disease modification, loop diuretics provide the **fastest and most direct symptomatic improvement** for fluid overload.
*Incorrect: Metoprolol*
- **Metoprolol** is a **beta-blocker** that is essential for chronic HFrEF management, providing **mortality reduction** and **reverse cardiac remodeling**.
- However, beta-blockers take **weeks to months** to show symptomatic benefit and can initially **worsen symptoms** due to negative inotropic effects, especially in acute decompensation.
- While important for long-term management, metoprolol does not provide immediate symptomatic relief from fluid overload.
*Incorrect: Losartan*
- **Losartan** is an **angiotensin receptor blocker (ARB)** used as an alternative to ACE inhibitors in HFrEF, particularly in patients who develop cough with ACE inhibitors.
- ARBs reduce **afterload** and prevent **cardiac remodeling**, contributing to improved long-term outcomes and mortality reduction.
- However, they do not directly address fluid overload and do not provide rapid symptomatic relief compared to diuretics.
*Incorrect: Spironolactone*
- **Spironolactone** is an **aldosterone antagonist** that improves mortality in HFrEF by preventing myocardial fibrosis, reducing cardiac remodeling, and preventing potassium loss.
- While beneficial for long-term management, spironolactone has **weak diuretic effects** and takes weeks to provide symptomatic benefit.
- It is not the first-line choice for **acute symptomatic relief** of volume overload, though it is an important component of chronic HFrEF therapy.
*Incorrect: Lisinopril*
- **Lisinopril** is an **ACE inhibitor** and a cornerstone of HFrEF therapy, reducing **mortality**, **hospitalizations**, and preventing **cardiac remodeling** by reducing afterload and preload.
- While ACE inhibitors improve symptoms over time, they do not provide the **rapid diuretic effect** needed for immediate relief of dyspnea and edema.
- Lisinopril is essential for long-term management but is not the most effective option for acute symptomatic improvement of fluid overload.
Wound healing and repair US Medical PG Question 4: A 56-year-old woman undergoes open reduction and internal fixation of the distal tibia 1 day after a fall. She has had rheumatoid arthritis for 12 years and diabetes mellitus for 2 years. Her medications over the past year have included metformin, prednisone, calcium supplements, and methotrexate. Prior to surgery, insulin was added to her medications, and the dose of prednisone was increased. She has had appropriate nutrition over the years with regular follow-ups with her healthcare professional. Which of the following is the most appropriate supplement to prevent wound failure in this patient?
- A. Glutamine
- B. Zinc
- C. Vitamin A
- D. Arginine
- E. Vitamin C (Correct Answer)
Wound healing and repair Explanation: ***Vitamin C***
- This patient is at high risk for **wound healing complications** due to her comorbidities (diabetes, rheumatoid arthritis) and medications (prednisone, methotrexate). **Vitamin C** (ascorbic acid) is essential for **collagen synthesis** and cross-linking, which is crucial for wound strength and tissue repair.
- While other options play a role in wound healing, Vitamin C is particularly important in patients with **impaired healing** due to chronic inflammation, corticosteroid use, and metabolic disorders, as it counteracts their negative effects on collagen formation.
*Glutamine*
- **Glutamine** is an important fuel for rapidly dividing cells, including immune cells and fibroblasts, and can be beneficial in catabolic states.
- However, its role in directly counteracting the specific challenges of this patient's wound healing (corticosteroid use, diabetes, rheumatoid arthritis) is **less direct** compared to Vitamin C's role in collagen synthesis.
*Zinc*
- **Zinc** is a cofactor for numerous enzymes involved in cell proliferation, immune function, and collagen synthesis.
- While important, zinc deficiency is not explicitly indicated, and its role as a primary intervention to prevent wound failure in a patient with **prednisone-induced healing impairment** is secondary to vitamin C.
*Vitamin A*
- **Vitamin A** can help reverse the negative effects of **corticosteroids** on wound healing by promoting epithelialization and collagen synthesis.
- While relevant due to prednisone use, its overall importance in **collagen formation** and direct wound strength is not as profound or broad as Vitamin C.
*Arginine*
- **Arginine** is a precursor for nitric oxide, which improves blood flow to wounds, and is involved in collagen formation and immune function.
- Although beneficial for wound healing, particularly in critically ill patients, it is **not the most appropriate single supplement** for addressing the specific collagen synthesis impairment seen in this patient's context of corticosteroid use and chronic disease.
Wound healing and repair US Medical PG Question 5: A 30-year-old woman dies shortly after admission to the emergency department. The family requests an autopsy to determine cause of death. During the autopsy, multiple linear, parallel marks are noted across her wrists. Which of the following patterns suggests these are hesitation marks rather than defensive wounds?
- A. Irregular, scattered marks
- B. Diagonal, deep lacerations
- C. Deep, single cuts
- D. Superficial, parallel cuts (Correct Answer)
Wound healing and repair Explanation: ***Superficial, parallel cuts***
- **Hesitation marks** are typically numerous, **superficial**, and **parallel**, reflecting a tentative or indecisive attempt and often made in the same direction.
- They tend to be concentrated in an area of the body chosen for self-harm, such as the wrists, and are usually consistent with a non-fatal intent.
*Irregular, scattered marks*
- This pattern is more indicative of **defensive wounds**, which are often scattered and irregular due to attempts to ward off an attack.
- Defensive wounds are typically found on the palms, forearms, and other areas used for protection.
*Diagonal, deep lacerations*
- **Deep lacerations**, especially if diagonal and singular, are less characteristic of hesitation marks and more suggestive of a determined attempt to inflict fatal injury or could be defensive.
- **Hesitation marks** are typically not aimed at quickly causing fatal harm.
*Deep, single cuts*
- A single, **deep cut** is often associated with a resolute intent to cause significant injury or death, rather than the hesitant, superficial nature of hesitation marks.
- This pattern would warrant further investigation into the intent and circumstances surrounding the injury.
Wound healing and repair US Medical PG Question 6: A 39-year-old man comes to the physician for a follow-up examination. He was treated for a urinary tract infection with trimethoprim-sulfamethoxazole 2 months ago. He is paraplegic as a result of a burst lumbar fracture that occurred after a fall 5 years ago. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He performs clean intermittent catheterization daily. He has smoked one pack of cigarettes daily for 19 years. His temperature is 37.1°C (98.8°F), pulse is 95/min, respirations are 14/min, and blood pressure is 120/80 mm Hg. He appears malnourished. Examination shows palpable pedal pulse. Multiple dilated tortuous veins are present over both lower extremities. There is a 2-cm wound surrounded by partial-thickness loss of skin and a pink wound bed over the right calcaneum. Neurologic examination shows paraparesis. His hemoglobin A1c is 6.5%, and fingerstick blood glucose concentration is 134 mg/dL. Which of the following is most likely to have prevented this patient's wound?
- A. Broad-spectrum antibiotic therapy
- B. Cessation of smoking
- C. Heparin therapy
- D. Topical antibiotic therapy
- E. Frequent position changes (Correct Answer)
Wound healing and repair Explanation: ***Frequent position changes***
- This patient is paraplegic, which increases his risk for **pressure ulcers** due to prolonged immobility and sustained pressure on bony prominences like the calcaneum.
- **Frequent repositioning** redistributes pressure, preventing skin breakdown and promoting circulation, thereby avoiding pressure injuries.
*Broad-spectrum antibiotic therapy*
- The wound is described as a **partial-thickness loss** with a pink wound bed, suggesting it's not primarily an infected wound requiring broad-spectrum antibiotics to prevent its formation.
- Antibiotics are used to **treat existing infections**, not prevent pressure ulcers in a non-infected state.
*Cessation of smoking*
- While **smoking impairs wound healing** and overall vascular health, it is not the most direct or primary preventative measure for a pressure ulcer caused by immobility.
- Smoking cessation would improve **long-term vascular health** and *ulcer healing*, but frequent position changes addresses the immediate cause of pressure.
*Heparin therapy*
- **Heparin** is an anticoagulant used to prevent **thrombosis** (blood clots), which is not the primary mechanism behind pressure ulcer formation.
- While immobility can contribute to deep vein thrombosis, heparin would not prevent the **mechanical pressure-induced skin damage** that causes a calcaneal wound.
*Topical antibiotic therapy*
- Similar to systemic antibiotics, topical antibiotics are used for **treating localized infections** or preventing them in *open wounds*.
- This wound is a result of pressure, and preventing its formation requires addressing the pressure itself, not merely applying antibiotics to the skin surface.
Wound healing and repair US Medical PG Question 7: A 45-year-old man comes to his primary care provider for a routine visit. The patient mentions that while he was cooking 5 days ago, he accidentally cut himself with a meat cleaver and lost the skin at the tip of his finger. After applying pressure and ice, the bleeding stopped and he did not seek treatment. The patient is otherwise healthy and does not take any daily medications. The patient’s temperature is 98.2°F (36.8°C), blood pressure is 114/72 mmHg, pulse is 60/min, and respirations are 12/min. On exam, the patient demonstrates a 0.5 x 0.3 cm wound on the tip of his left third finger. No bone is involved, and the wound is red, soft, and painless. There are no signs of infection. Which of the following can be expected on histopathological examination of the wounded area?
- A. Platelet aggregates
- B. Epithelial cell migration from the wound borders
- C. Neutrophil migration into the wound
- D. Deposition of type III collagen (Correct Answer)
- E. Deposition of type I collagen
Wound healing and repair Explanation: ***Deposition of type III collagen***
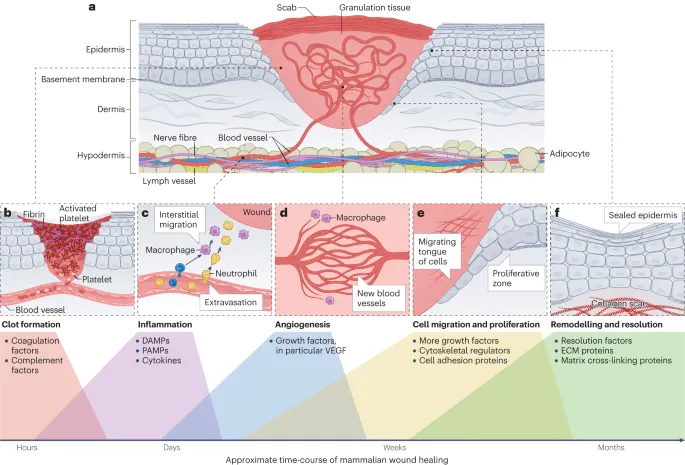
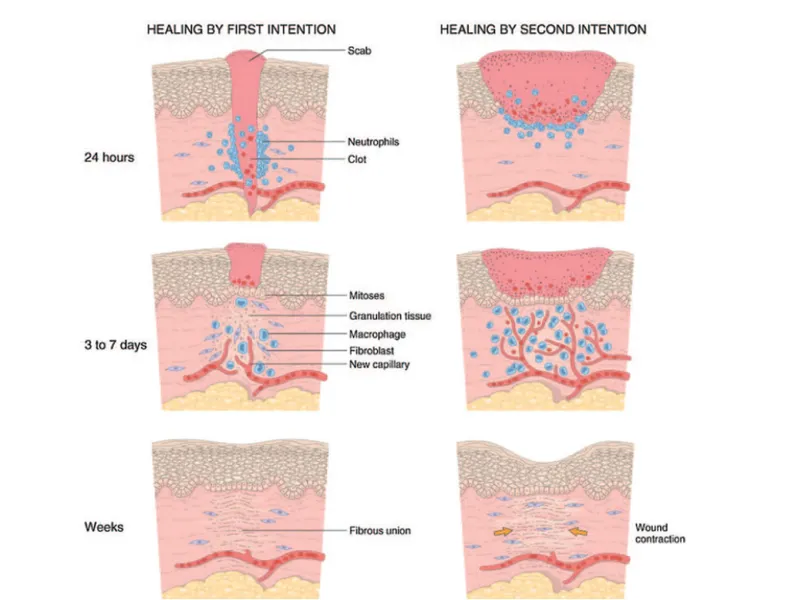
- Five days post-injury, the **proliferative phase of wound healing** is active, characterized by the formation of an initial **granulation tissue** matrix primarily composed of **Type III collagen**.
- This type of collagen forms thinner, more flexible fibers that provide a temporary scaffold for tissue regeneration before being gradually replaced by stronger Type I collagen.
*Platelet aggregates*
- **Platelet aggregation** occurs immediately after injury as part of **hemostasis**, forming a plug to stop bleeding.
- By five days, this initial phase would have concluded, and the primary focus would be on tissue repair and regeneration.
*Epithelial cell migration from the wound borders*
- **Epithelial cell migration** for re-epithelialization typically occurs within the first 24-48 hours after injury, forming a new epidermal layer over the wound.
- While it continues, the dominant histological feature at day 5 in an open wound of this size would be **granulation tissue formation** in the dermis.
*Neutrophil migration into the wound*
- **Neutrophil migration** is a hallmark of the **inflammatory phase**, peaking within 24-48 hours post-injury to clear debris and microbes.
- By day 5, the inflammatory phase would be subsiding, and macrophages would be more prevalent, signaling the transition to the proliferative phase.
*Deposition of type I collagen*
- **Type I collagen** is the predominant collagen found in mature scar tissue and is deposited during the later **remodeling phase** of wound healing.
- While some Type I collagen may be present, **Type III collagen** is characteristic of the early granulation tissue prominent at day 5.
Wound healing and repair US Medical PG Question 8: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
Wound healing and repair Explanation: ***Keloid scar formation***
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Wound healing and repair US Medical PG Question 9: A 37-year-old man presents to his primary care physician because he has had constipation for the last several weeks. He has also been feeling lethargic and complains that this winter has been particularly cold. He also complains that he has been gaining weight despite no change in his normal activities. He reveals that two months prior to presentation he had what felt like the flu for which he took Tylenol and did not seek medical attention. Several days after this he developed anterior neck pain. Which of the following findings would most likely be seen on biopsy of this patient's abnormality?
- A. Focal hyperplasia
- B. Germinal follicles
- C. Scalloped clear areas
- D. Fibrous tissue
- E. Granulomatous inflammation (Correct Answer)
Wound healing and repair Explanation: ***Granulomatous inflammation***
- The patient's presentation with **constipation**, **lethargy**, **cold intolerance**, and **weight gain** after a flu-like illness followed by **anterior neck pain** is highly suggestive of **subacute granulomatous thyroiditis (de Quervain thyroiditis)**.
- A biopsy of the thyroid in cases of de Quervain thyroiditis typically reveals **granulomatous inflammation** with scattered **giant cells** and lymphocytes, reflecting the destructive inflammatory process.
*Focal hyperplasia*
- **Focal hyperplasia** is characterized by an increase in the number of thyroid follicular cells and is seen in conditions like **Graves' disease** or **multinodular goiter**, particularly when the gland is overstimulated.
- This finding would not be expected in subacute granulomatous thyroiditis, where the primary pathology is destruction rather than proliferation.
*Germinal follicles*
- **Germinal follicles** are characteristic of chronic lymphocytic thyroiditis (**Hashimoto's thyroiditis**), an autoimmune condition where the thyroid gland is infiltrated by lymphocytes, plasma cells, and macrophages.
- While Hashimoto's can cause hypothyroidism, the preceding flu-like illness and acute neck pain make de Quervain thyroiditis a more likely diagnosis.
*Scalloped clear areas*
- **Scalloped clear areas** at the colloid-epithelial interface, also known as **colloid resorption vacuoles**, are a histological feature of **hyperactive thyroid follicles**, typically seen in conditions causing hyperthyroidism like **Graves' disease**.
- The patient's symptoms of lethargy, cold intolerance, and weight gain indicate hypothyroidism, which can follow the initial hyperthyroid phase of de Quervain thyroiditis but are not indicative of active hyperfunction on biopsy at this stage.
*Fibrous tissue*
- An increased amount of **fibrous tissue** is characteristic of **Riedel's thyroiditis**, a rare condition characterized by dense fibrosis that replaces normal thyroid parenchyma and can extend into surrounding neck structures.
- This patient's presentation with a preceding febrile illness and neck pain is not typical for Riedel's thyroiditis, which usually presents as a hard, fixed mass without an antecedent viral infection.
Wound healing and repair US Medical PG Question 10: A 33-year-old Caucasian female presents to her primary care provider for skin problems and difficulty breathing. She has not sought medical care in over 10 years due to anxiety around physicians. However, she has experienced gradual onset of diffuse pruritus, skin induration, and limited finger mobility over the past 5 years that has negatively impacted her work as an accountant. More recently, she has developed exertional shortness of breath and is concerned that it may impact her ability to care for her 3-year-old son. She reports no prior medical conditions and takes fish oil. She smokes 1 pack of cigarettes per day and drinks socially. Her temperature is 98.6°F (37°C), blood pressure is 145/85 mmHg, pulse is 85/min, and respirations are 22/min. On exam, she appears anxious with minimally increased work of breathing. Dry rales are heard at her lung bases bilaterally. Her fingers appear shiny and do not have wrinkles on the skin folds. A normal S1 and S2 are heard on cardiac auscultation. This patient’s lung disease is caused by increased secretion of which of the following substances within the lungs?
- A. Interleukin 1
- B. Tumor necrosis factor alpha
- C. Interleukin 2
- D. Transforming growth factor beta (Correct Answer)
- E. Interferon gamma
Wound healing and repair Explanation: ***Transforming growth factor beta***
- The patient's symptoms of **diffuse pruritus, skin induration, limited finger mobility**, exertional shortness of breath, and **shiny fingers without wrinkles** are highly suggestive of **systemic sclerosis (scleroderma)**.
- The lung disease in scleroderma, often **interstitial lung disease (ILD)**, is characterized by **fibrosis driven by excessive collagen deposition**, a process significantly mediated by **transforming growth factor beta (TGF-β)**.
*Interleukin 1*
- **Interleukin-1 (IL-1)** is a pro-inflammatory cytokine primarily involved in acute inflammation and fever, not directly implicated as the primary driver of fibrosis in scleroderma-associated lung disease.
- While IL-1 can contribute to inflammation in various autoimmune diseases, it does not directly stimulate the **fibrotic pathways** in the same manner as TGF-β.
*Tumor necrosis factor alpha*
- **Tumor necrosis factor-alpha (TNF-α)** is a prominent pro-inflammatory cytokine involved in many autoimmune and inflammatory conditions, including rheumatoid arthritis.
- Although it plays a role in the inflammatory process, TNF-α is not considered the primary mediator responsible for the **fibrotic changes** seen in systemic sclerosis.
*Interleukin 2*
- **Interleukin-2 (IL-2)** is crucial for the proliferation and differentiation of T cells, particularly regulatory T cells, and is primarily involved in immune regulation and response to infection.
- Its direct role in the **pathogenesis of fibrosis** in the context of scleroderma-associated lung disease is not as central as that of TGF-β.
*Interferon gamma*
- **Interferon-gamma (IFN-γ)** is a cytokine predominantly associated with anti-viral responses and the activation of macrophages and natural killer cells in cell-mediated immunity.
- While it has immunomodulatory effects, IFN-γ is generally considered to have **anti-fibrotic properties** in some contexts, rather than promoting fibrosis in scleroderma.
More Wound healing and repair US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.