Systemic effects of inflammation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Systemic effects of inflammation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Systemic effects of inflammation US Medical PG Question 1: A 6-year-old boy is presented to a pediatric clinic by his mother with complaints of fever, malaise, and cough for the past 2 days. He frequently complains of a sore throat and has difficulty eating solid foods. The mother mentions that, initially, the boy’s fever was low-grade and intermittent but later became high grade and continuous. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The past medical history is noncontributory. The boy takes a multivitamin every day. The mother reports that he does well in school and is helpful around the house. The boy’s vital signs include blood pressure 110/65 mm Hg, heart rate 110/min, respiratory rate 32/min, and temperature 38.3°C (101.0°F). On physical examination, the boy appears uncomfortable and has difficulty breathing. His heart is mildly tachycardic with a regular rhythm and his lungs are clear to auscultation bilaterally. Oropharyngeal examination shows that his palatine tonsils are covered with pus and that there is erythema of the surrounding mucosa. Which of the following mediators is responsible for this patient’s elevated temperature?
- A. Leukotriene D4
- B. Prostaglandin F2
- C. Prostaglandin E2 (Correct Answer)
- D. Thromboxane A2
- E. Prostaglandin I2
Systemic effects of inflammation Explanation: ***Prostaglandin E2***
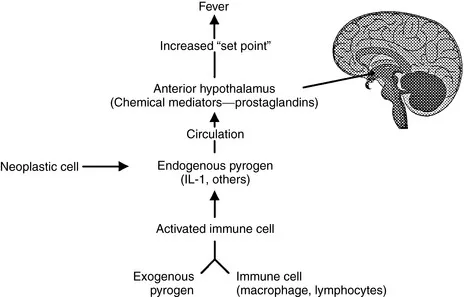
- **Prostaglandin E2 (PGE2)** is a key mediator of fever, acting directly on the **hypothalamus** to reset the body's thermoregulatory set point.
- In response to infection and inflammation, immune cells release **pyrogens** (like IL-1, TNF-alpha), which stimulate PGE2 synthesis in the brain, leading to increased body temperature.
*Leukotriene D4*
- **Leukotriene D4 (LTD4)** is a potent mediator of **bronchoconstriction** and increased **vascular permeability**, particularly in allergic reactions and asthma.
- While it plays a role in inflammation, it does not directly cause fever by altering the hypothalamic set point.
*Prostaglandin F2*
- **Prostaglandin F2 (PGF2)** has various physiological roles, including **uterine contraction** and **bronchoconstriction**, and is important for reproductive functions.
- It is not primarily involved in mediating the febrile response to infection.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is predominantly involved in **platelet aggregation** and **vasoconstriction**, playing a crucial role in hemostasis and thrombosis.
- While it is a product of the arachidonic acid pathway, it does not directly contribute to fever.
*Prostaglandin I2*
- **Prostaglandin I2 (PGI2)**, also known as **prostacyclin**, is a potent **vasodilator** and inhibitor of **platelet aggregation**, protecting the vascular endothelium.
- It typically counteracts the effects of TXA2 and is not a mediator of fever.
Systemic effects of inflammation US Medical PG Question 2: A 60-year-old rock musician presents to the office because he has been feeling increasingly tired for the past 6 months. He has a history of intravenous drug use and alcohol abuse. He states that he feels quite tired, but he otherwise has no complaints. Physical examination is noncontributory. His laboratory values are normal other than moderately elevated liver enzymes. Which of the following additional tests should you order first?
- A. Hepatitis C virus antibodies (Correct Answer)
- B. Hepatitis B surface antigen
- C. Hepatitis E virus-specific IgM antibodies
- D. Hepatitis D virus-specific IgG antibody
- E. Hepatitis A virus-specific IgM antibodies
Systemic effects of inflammation Explanation: ***Hepatitis C virus antibodies***
- The patient's history of **intravenous drug use** and **chronic fatigue** with **elevated liver enzymes** strongly suggests chronic viral hepatitis, with hepatitis C being the most common blood-borne infection in persons with IVDU history.
- **Hepatitis C** is the **most prevalent chronic viral hepatitis** in the United States among persons with history of injection drug use, with transmission efficiency via needle sharing being very high.
- Hepatitis C often has a **long asymptomatic phase** (decades) before symptoms like fatigue and liver damage become apparent, making antibody testing the appropriate initial screen.
- While both HBV and HCV should ultimately be screened in this patient, **HCV prevalence is significantly higher** in the IVDU population, making it the priority initial test.
*Hepatitis B surface antigen*
- While **hepatitis B** can also be transmitted via intravenous drug use and cause chronic liver disease, **hepatitis C is more prevalent** in persons with IVDU history in the United States.
- **HBsAg** is used to detect active hepatitis B infection and should also be ordered, but given resource constraints and the clinical context, **anti-HCV is the higher-yield initial test**.
- Many IVDU patients have been vaccinated against HBV, further reducing its likelihood compared to HCV (for which no vaccine exists).
*Hepatitis E virus-specific IgM antibodies*
- **Hepatitis E** is typically transmitted via the **fecal-oral route** (contaminated water) and usually causes **acute, self-limiting hepatitis**, not chronic insidious fatigue and liver enzyme elevation in a Western patient.
- **IgM antibodies** would indicate an acute infection, which is less likely given the 6-month duration of symptoms.
- HEV rarely causes chronic infection except in immunocompromised patients.
*Hepatitis D virus-specific IgG antibody*
- **Hepatitis D** requires an existing **hepatitis B infection** to replicate (it's a satellite virus), meaning you would first need to confirm chronic hepatitis B before testing for HDV.
- While HDV can cause severe liver disease and is transmitted via blood exposure, it's not the initial test to pursue without evidence of HBV co-infection.
*Hepatitis A virus-specific IgM antibodies*
- **Hepatitis A** is transmitted via the **fecal-oral route** and causes an **acute, self-limiting infection** with complete resolution, rarely leading to chronic liver disease or persistent fatigue over 6 months.
- **IgM antibodies** are indicative of acute infection, which contradicts the chronic nature of the patient's symptoms.
- HAV does not cause chronic hepatitis.
Systemic effects of inflammation US Medical PG Question 3: A 68-year-old man of Mediterranean descent comes to the clinic with complaints of fatigue for the past month. He reports that it is increasingly difficult for him to complete his after-dinner walks as he would get breathless and tired around 10 minutes. He endorses dizziness and an upper respiratory infection last week for which he “took a lot of aspirin.” Past medical history is significant for malaria 10 years ago (for which he was adequately treated with anti-malarial medications) and aortic stenosis status post prosthetic valve replacement 5 months ago. When asked if he has had similar episodes before, he claims, “Never! I’ve been as healthy as a horse until my heart surgery.” Physical examination is significant for mild scleral icterus bilaterally and a faint systolic murmur. Which of the following images represents a potential peripheral smear in this patient?
- A. B
- B. E
- C. C
- D. D
- E. A (Correct Answer)
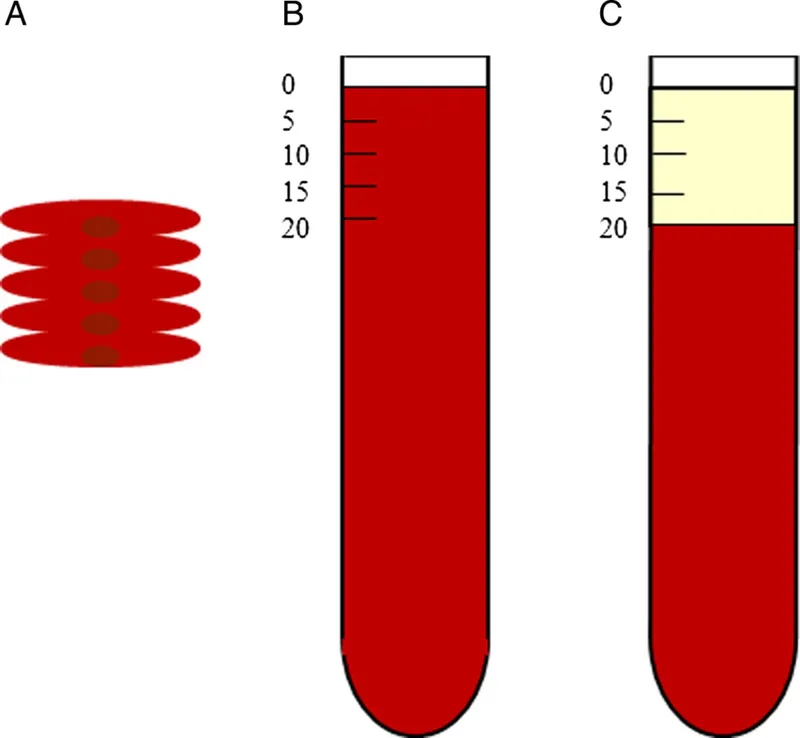
Systemic effects of inflammation Explanation: ***A***
- Image A depicts **bite cells** and **Heinz bodies**, which are characteristic findings in **hemolysis** caused by **G6PD deficiency**. This patient's Mediterranean descent, recent aspirin use (an oxidant drug), and symptoms of fatigue, dyspnea, dizziness, and scleral icterus are highly suggestive of an acute hemolytic crisis in G6PD deficiency patients.
- **G6PD deficiency** is an X-linked recessive disorder prevalent in Mediterranean populations, where certain medications (like aspirin, sulfonamides, antimalarials) or infections can trigger episodes of acute hemolytic anemia due to oxidative stress.
*B*
- Image B shows **sickle cells**, which are characteristic of **sickle cell anemia**. While individuals with sickle cell disease can experience fatigue and anemia, there are no specific clinical elements in the vignette that point to sickle cell disease (e.g., pain crises, vaso-occlusion, or chronic hemolytic anemia from birth).
- The patient's presentation with an acute episode triggered by aspirin is less typical for a first presentation of sickle cell anemia at this age, and his prior malaria exposure is not directly linked to sickle cell disease as the cause of this acute presentation.
*E*
- Image E illustrates **schistocytes** (fragmented red blood cells) and potentially an occasional spherocyte, which are hallmarks of **microangiopathic hemolytic anemia (MAHA)**, often seen in conditions like **thrombotic thrombocytopenic purpura (TTP)**, **hemolytic uremic syndrome (HUS)**, or **disseminated intravascular coagulation (DIC)**.
- While the patient has a prosthetic valve (which can cause hemolytic anemia through mechanical stress, leading to schistocytes), the primary trigger for this acute episode appears to be G6PD deficiency, given the history of aspirin use and Mediterranean descent.
*C*
- Image C displays **spherocytes**, which are small, dense red blood cells lacking central pallor, commonly seen in **hereditary spherocytosis** or **autoimmune hemolytic anemia (AIHA)**.
- Although the patient's symptoms suggest hemolysis, the trigger (aspirin) and his ethnic background make G6PD deficiency a more likely diagnosis than hereditary spherocytosis or AIHA, which would typically present differently or have other specific findings.
*D*
- Image D demonstrates **acanthocytes (spur cells)**, which are red blood cells with irregular, spiny projections, typically associated with severe **liver disease** (e.g., cirrhosis, alcoholic liver disease), **abetalipoproteinemia**, or **hypothyroidism**.
- There are no clinical features in the vignette to suggest any of these underlying conditions, and acanthocytes are not characteristic of the acute hemolytic anemia described.
Systemic effects of inflammation US Medical PG Question 4: A 53-year-old diabetic man with cellulitis of the right lower limb presents to the emergency department because of symptoms of fever and chills. His pulse is 122/min, the blood pressure is 76/50 mm Hg, the respirations are 26/min, and the temperature is 40.0°C (104.0°F). His urine output is < 0.5mL/kg/h. He has warm peripheral extremities. The hemodynamic status of the patient is not improving in spite of the initiation of adequate fluid resuscitation. He is admitted to the hospital. Which of the following is the most likely laboratory profile?
- A. WBC count: 11,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 0.9 mmol/L
- B. WBC count: 1234/mm3; high CVP; blood culture: gram-negative bacteremia; blood lactate level: 1.6 mmol/L
- C. WBC count: 16,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 2.2 mmol/L (Correct Answer)
- D. WBC count: 6670/mm3; low CVP; blood culture: gram-positive bacteremia; blood lactate level: 1.1 mmol/L
- E. WBC count: 8880/mm3; high CVP; blood culture: gram-positive bacteremia; blood lactate level: 2.1 mmol/L
Systemic effects of inflammation Explanation: ***WBC count: 16,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 2.2 mmol/L***
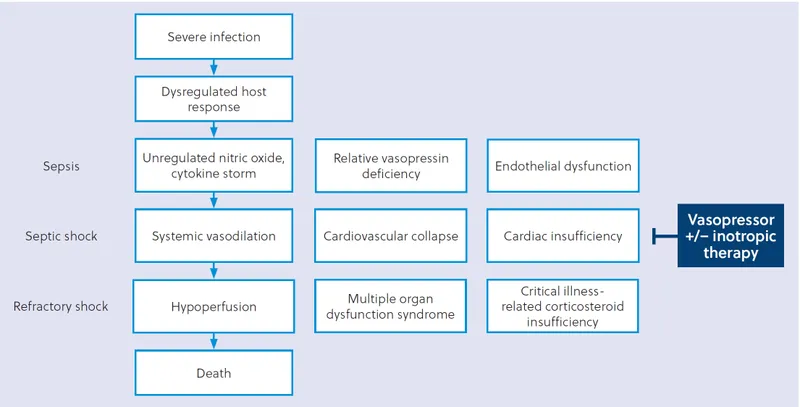
- This profile aligns with **septic shock** driven by gram-negative bacteria, presenting with **tachycardia**, **hypotension**, **fever**, and **poor urine output** despite fluid resuscitation.
- A **high WBC count** (leukocytosis), **low CVP** (due to vasodilation and relative hypovolemia), **gram-negative bacteremia** (common in severe sepsis), and **elevated lactate** (indicating tissue hypoperfusion) are characteristic findings.
*WBC count: 11,670/mm3; low CVP; blood culture: gram-negative bacteremia; blood lactate level: 0.9 mmol/L*
- While most components suggest sepsis (WBC count and low CVP), a **lactate level of 0.9 mmol/L** is within the normal range, contradicting the severe hypoperfusion and shock observed in the patient.
- The patient's presentation with **hypotension** unresponsive to fluids and **oliguria** strongly indicates significant tissue hypoperfusion, which would typically result in a higher lactate.
*WBC count: 1234/mm3; high CVP; blood culture: gram-negative bacteremia; blood lactate level: 1.6 mmol/L*
- A **WBC count of 1234/mm3 (leukopenia)** is an atypical response for severe infection and sepsis; often, sepsis presents with leukocytosis.
- A **high CVP** indicates fluid overload or cardiac dysfunction, which is not consistent with the initial low blood pressure and the need for fluid resuscitation seen in distributive shock.
*WBC count: 6670/mm3; low central venous pressure (CVP); blood culture: gram-positive bacteremia; blood lactate level: 1.1 mmol/L*
- A **WBC count of 6670/mm3** is within the normal range and does not reflect an adequate inflammatory response to severe infection and shock.
- A **normal lactate level (1.1 mmol/L)** does not support the clinical picture of shock and tissue hypoperfusion despite the presence of gram-positive bacteremia.
*WBC count: 8880/mm3; high CVP; blood culture: gram-positive bacteremia; blood lactate level: 2.1 mmol/L*
- A **WBC count of 8880/mm3** is normal, which is unlikely in a severe sepsis presentation.
- A **high CVP** is not consistent with the distributive shock state where there is often relative hypovolemia and vasodilation leading to low CVP.
Systemic effects of inflammation US Medical PG Question 5: A 70-year-old woman is on hospital day 2 in the medical intensive care unit. She was admitted from the emergency department for a 2-day history of shortness of breath and fever. In the emergency department, her temperature is 39.4°C (103.0°F), the pulse is 120/min, the blood pressure is 94/54 mm Hg, the respiratory rate is 36/min, and oxygen saturation was 82% while on 4L of oxygen via a non-rebreather mask. Chest X-ray shows a right lower lobe consolidation. She was intubated, sedated, and started on broad-spectrum antibiotics for sepsis of pulmonary origin and intravenous norepinephrine for blood pressure support. Since then, her clinical condition has been stable, though her vasopressor and oxygen requirements have not improved. Today, her physician is called to the bedside because her nurse noted some slow bleeding from her intravenous line sites and around her urinary catheter. Which of the following most likely represents the results of coagulation studies for this patient?
- A. D-dimer: negative, fibrinogen level: low, platelet count: low
- B. D-dimer: elevated, fibrinogen level: normal, platelet count: normal
- C. D-dimer: elevated, fibrinogen level: low, platelet count: low (Correct Answer)
- D. D-dimer: negative, fibrinogen level: elevated, platelet count: elevated
- E. D-dimer: negative, fibrinogen level: normal, platelet count: normal
Systemic effects of inflammation Explanation: ***D-dimer: elevated, fibrinogen level: low, platelet count: low***
- The patient's presentation with **sepsis** requiring intubation and vasopressors, along with diffuse **bleeding from IV sites and urinary catheter**, strongly suggests **disseminated intravascular coagulation (DIC)**.
- In DIC, widespread activation of the coagulation cascade leads to consumption of **platelets** and **clotting factors (including fibrinogen)**, resulting in thrombocytopenia and hypofibrinogenemia. The breakdown of clots produces **elevated D-dimer** levels.
*D-dimer: negative, fibrinogen level: low, platelet count: low*
- A **negative D-dimer** would contradict the diagnosis of DIC, as D-dimer is a product of fibrin degradation and is almost always elevated in DIC due to extensive clot formation and subsequent fibrinolysis.
- While low fibrinogen and platelet count are characteristic of DIC, the negative D-dimer makes this option unlikely in the context of active bleeding from multiple sites.
*D-dimer: elevated, fibrinogen level: normal, platelet count: normal*
- While an **elevated D-dimer** is consistent with fibrinolysis occurring in DIC, normal **fibrinogen** and **platelet counts** would argue against the consumptive coagulopathy that defines DIC.
- The presence of diffuse bleeding in a patient with sepsis usually indicates significant depletion of clotting factors and platelets.
*D-dimer: negative, fibrinogen level: elevated, platelet count: elevated*
- This profile suggests an **inflammatory state** or a hypercoagulable state without significant fibrinolysis or consumption of clotting factors.
- A **negative D-dimer** and **elevated fibrinogen/platelets** contradict the signs and symptoms of DIC with active bleeding.
*D-dimer: negative, fibrinogen level: normal, platelet count: normal*
- This result would be inconsistent with **DIC** and the patient's clinical picture of widespread bleeding.
- In DIC, there is active coagulation and fibrinolysis, leading to consumption of platelets and fibrinogen and production of D-dimers.
Systemic effects of inflammation US Medical PG Question 6: A 28-year-old man presents to the office with complaints of malaise, anorexia, and vomiting for the past 2 weeks. He also says that his urine is dark. The past medical history is unremarkable. The temperature is 36.8°C (98.2°F), the pulse is 72/min, the blood pressure is 118/63 mm Hg, and the respiratory rate is 15/min. The physical examination reveals a slightly enlarged, tender liver. No edema or spider angiomata are noted. Laboratory testing showed the following:
HBsAg Positive
IgM anti-HBc < 1:1,000
Anti-HBs Negative
HBeAg Positive
Anti-HBe Negative
HBV DNA 2.65 × 10⁹ IU/L
Alpha-fetoprotein 125 ng/mL
What is the most likely cause of this patient's condition?
- A. Acute HBV infection
- B. Passive immunity
- C. Acute resolving infection
- D. Resolved HBV infection (innate immunity)
- E. Acute exacerbation of chronic HBV infection (Correct Answer)
Systemic effects of inflammation Explanation: ***Acute exacerbation of chronic HBV infection***
- The combination of **HBsAg positive** (indicating extant infection) and **IgM anti-HBc < 1:1,000** (a low titer consistent with chronic infection, not acute) points towards a pre-existing chronic hepatitis B infection.
- The elevated **HBV DNA (2.65 × 109 IU/L)**, along with clinical symptoms like malaise, anorexia, vomiting, dark urine, and a tender liver, suggests an **acute exacerbation** of this chronic condition.
*Acute HBV infection*
- An acute HBV infection would typically present with a **high titer of IgM anti-HBc** and often **HBeAg positive** initially, but this patient's low IgM anti-HBc titer rules out a new acute infection.
- While symptoms align with acute hepatitis, the serology (low IgM anti-HBc) is not characteristic of primary acute infection.
*Passive immunity*
- Passive immunity would be characterized by the presence of **Anti-HBs without HBsAg**, which is not seen here.
- This scenario usually occurs after receiving hepatitis B immunoglobulin or transplacental transfer of antibodies.
*Acute resolving infection*
- A resolving acute infection would typically show a **decrease in HBsAg** and the **presence of Anti-HBs**, neither of which are observed in this patient.
- The **high viral load (HBV DNA)** and persistent HBsAg also contradict a resolving infection.
*Resolved HBV infection (innate immunity)*
- A resolved HBV infection is defined by the **absence of HBsAg** and the **presence of Anti-HBs**, along with anti-HBc.
- This patient still has **HBsAg present** and **Anti-HBs negative**, ruling out a resolved infection.
Systemic effects of inflammation US Medical PG Question 7: A 3-day-old female newborn is brought to the emergency department because of fever, poor feeding, and irritability for 6 hours. She was delivered at home at 39 weeks' gestation and delivery was uncomplicated. The mother had no prenatal care. Her temperature is 39.8°C (103.6°F), pulse is 172/min, respirations are 58/min, and blood pressure is 74/45 mm Hg. She appears lethargic. Physical examination shows expiratory grunting and nasal flaring. Serum studies show elevated levels of interleukin-6. Which of the following is the most likely effect of this laboratory finding?
- A. Decreased synthesis of hepcidin
- B. Decreased expression of MHC class II
- C. Increased release of fibrinogen (Correct Answer)
- D. Increased classical activation of macrophages
- E. Increased production of IgE
Systemic effects of inflammation Explanation: ***Increased release of fibrinogen***
- **Interleukin-6 (IL-6)** is a major **pro-inflammatory cytokine** that stimulates the liver to produce **acute phase reactants**, including **fibrinogen**.
- This increase in fibrinogen is part of the body's non-specific immune response to infection and inflammation, leading to elevated inflammatory markers like **ESR**.
*Decreased synthesis of hepcidin*
- **Hepcidin** synthesis is *increased* by IL-6, not decreased, as part of the body's response to inflammation to limit iron availability to pathogens.
- High levels of hepcidin lead to **anemia of chronic disease** by inhibiting iron absorption and release from macrophages.
*Decreased expression of MHC class II*
- IL-6 generally *enhances* immune responses, and while it doesn't directly increase MHC class II expression on antigen-presenting cells, reduced expression is not a typical effect.
- **MHC class II** expression is primarily regulated by cytokines like **interferon-gamma** and helps present antigens to T-helper cells.
*Increased classical activation of macrophages*
- **Classical activation of macrophages** (M1 polarization) is primarily driven by **interferon-gamma (IFN-γ)** and **TNF-α**, often in response to pathogen signals.
- While IL-6 can contribute to the overall inflammatory environment, it is not the primary cytokine for classical macrophage activation; rather, it often promotes alternative (M2) phenotypes or has pleiotropic effects.
*Increased production of IgE*
- **IgE production** is primarily associated with **allergic reactions** and **parasitic infections**, driven by cytokines like **IL-4** and **IL-13**.
- IL-6 is not directly involved in stimulating IgE synthesis; its main roles are in inflammation, hematopoiesis, and the acute phase response.
Systemic effects of inflammation US Medical PG Question 8: A 46-year-old male was found unconscious in the field and brought to the emergency department by EMS. The patient was intubated in transit and given a 2 liter bolus of normal saline. On arrival, the patient's blood pressure is 80/60 mmHg and temperature is 37.5°C. Jugular veins are flat and capillary refill time is 4 seconds.
Vascular parameters are measured and are as follows:
Cardiac index - Low
Pulmonary capillary wedge pressure (PCWP) - Low
Systemic vascular resistance - High
Which of the following is the most likely diagnosis?
- A. Septic shock
- B. Anaphylactic shock
- C. Cardiogenic shock
- D. Hypovolemic shock (Correct Answer)
- E. Neurogenic shock
Systemic effects of inflammation Explanation: ***Hypovolemic shock***
- The patient presents with **hypotension**, **flat jugular veins**, **prolonged capillary refill**, and a **low cardiac index** and **low pulmonary capillary wedge pressure (PCWP)**, all indicative of inadequate intravascular volume.
- The **high systemic vascular resistance** is a compensatory mechanism to maintain blood pressure in the setting of decreased circulating volume.
*Septic shock*
- Septic shock typically presents with **vasodilation**, leading to a **low systemic vascular resistance**, which contradicts the findings in this patient.
- While patients can be hypotensive, the vascular parameters, especially SVR, do not align with septic shock.
*Anaphylactic shock*
- This type of shock is characterized by widespread **vasodilation** and increased capillary permeability, leading to a **low systemic vascular resistance** and often significant **edema** or **urticaria**, none of which are suggested here.
- While it can cause hypotension and low PCWP due to fluid shifts, the high SVR makes it less likely.
*Cardiogenic shock*
- Cardiogenic shock is characterized by **pump failure**, leading to a **low cardiac index** but a **high PCWP** due to fluid backup in the pulmonary circulation.
- This directly contrasts the patient's low PCWP.
*Neurogenic shock*
- Neurogenic shock involves a loss of **sympathetic tone**, resulting in widespread **vasodilation** and a **low systemic vascular resistance**, often accompanied by **bradycardia**.
- The high SVR in this patient rules out neurogenic shock.
Systemic effects of inflammation US Medical PG Question 9: A 73-year-old man comes to the physician because of progressive fatigue and shortness of breath on exertion for 3 weeks. He has swelling of his legs. He has not had nausea or vomiting. His symptoms began shortly after he returned from a trip to Cambodia. He occasionally takes ibuprofen for chronic back pain. He has a history of arterial hypertension and osteoarthritis of both knees. He had an episode of pneumonia 4 months ago. His current medications include lisinopril and hydrochlorothiazide. He has no history of drinking or smoking. His temperature is 37°C (98.6°F), pulse is 101/min, and blood pressure is 135/76 mm Hg. Examination shows pitting edema of the upper and lower extremities. Laboratory studies show:
Hemoglobin 14.1 g/dL
Leukocyte count 6,800/mm3
Platelet count 216,000/mm3
Serum
Urea nitrogen 26 mg/dL
Creatinine 2.9 mg/dL
Albumin 1.6 g/dL
Urine
Blood negative
Protein 4+
Glucose negative
Renal biopsy with Congo red stain shows apple-green birefringence under polarized light. Further evaluation of this patient is most likely to show which of the following findings?
- A. Positive interferon-γ release assay
- B. Dilated bronchi on chest CT
- C. Elevated anti-citrullinated peptide antibodies
- D. Positive HLA-B27 test
- E. Rouleaux formation on peripheral smear (Correct Answer)
Systemic effects of inflammation Explanation: ***Rouleaux formation on peripheral smear***
- The renal biopsy showing **apple-green birefringence** with Congo red stain is pathognomonic for **amyloidosis**.
- The clinical presentation of **nephrotic syndrome** (massive proteinuria, hypoalbuminemia, edema) with renal amyloidosis in an elderly patient is most commonly due to **AL (light chain) amyloidosis** caused by plasma cell dyscrasia.
- AL amyloidosis is associated with **monoclonal gammopathy** which causes increased serum protein viscosity, leading to **rouleaux formation** (stacking of RBCs like coins) on peripheral blood smear.
- Further workup would typically show serum/urine protein electrophoresis with monoclonal protein and possibly bone marrow plasmacytosis.
*Positive interferon-γ release assay*
- This test diagnoses **latent or active tuberculosis**.
- While TB can cause **AA (secondary) amyloidosis** through chronic inflammation, and the patient traveled to an endemic area, the renal-limited presentation without active systemic infection makes AL amyloidosis more likely.
- AA amyloidosis typically presents with chronic inflammatory conditions lasting months to years.
*Dilated bronchi on chest CT*
- **Bronchiectasis** causes chronic inflammation and can lead to **AA amyloidosis**.
- However, a single episode of pneumonia 4 months ago is insufficient to cause the chronic inflammation needed for AA amyloidosis.
- This finding would not directly relate to the amyloid deposition causing current symptoms.
*Elevated anti-citrullinated peptide antibodies*
- These antibodies are highly specific for **rheumatoid arthritis**, which can cause AA amyloidosis.
- However, the patient has **osteoarthritis** (degenerative joint disease), not inflammatory arthritis.
- There are no clinical features suggesting RA (no joint inflammation, no morning stiffness).
*Positive HLA-B27 test*
- **HLA-B27** is associated with **seronegative spondyloarthropathies** which can rarely cause AA amyloidosis.
- The patient's back pain is attributed to chronic mechanical issues, not inflammatory spondyloarthropathy.
- This finding is unrelated to the renal amyloidosis presentation.
Systemic effects of inflammation US Medical PG Question 10: A 45-year-old immigrant presents with unintentional weight loss, sleep hyperhidrosis, and a persistent cough. He says these symptoms have been present for quite some time. Upon imaging, many granulomas in the upper lobes are present. It is noted that these apical granulomas have centers of necrosis that appear cheese-like in appearance. Encircling the area of necrosis are large cells with cytoplasms pale in color. Of the following surface markers, which one is most closely associated with these cells?
- A. CD20
- B. CD3
- C. CD4
- D. CD14 (Correct Answer)
- E. CD8
Systemic effects of inflammation Explanation: ***CD14***
- The description of **caseating granulomas** in the upper lobes with large cells having pale cytoplasm points towards **tuberculosis** and the presence of **epithelioid macrophages**.
- **CD14** is a surface marker commonly found on **monocytes** and **macrophages**, making it the most appropriate choice among the given options.
- Note: While epithelioid macrophages (the activated form seen in granulomas) may downregulate CD14 compared to circulating monocytes, CD14 remains the most closely associated macrophage marker among these choices. **CD68** would be the ideal marker for tissue macrophages, but it is not listed.
*CD20*
- **CD20** is a surface marker characteristic of **B lymphocytes**.
- While B cells might be present in inflammatory lesions, they are not the predominant cell type described as "large cells with pale cytoplasm" forming the granuloma.
*CD3*
- **CD3** is a pan T-cell marker, indicating the presence of all types of **T lymphocytes**.
- While T cells (specifically CD4+ T helper cells) are crucial in granuloma formation, the "large cells with pale cytoplasm" encasing the necrosis specifically refer to epithelioid macrophages, not T cells.
*CD4*
- **CD4** is a surface marker for **helper T lymphocytes**.
- **CD4+ T cells** play a critical role in orchestrating the immune response and granuloma formation in tuberculosis through IFN-γ secretion, but the description of the large cells with pale cytoplasm refers to macrophages, not lymphocytes.
*CD8*
- **CD8** is a surface marker for **cytotoxic T lymphocytes**.
- **CD8+ T cells** are also involved in the immune response to mycobacterial infection but are not the primary cell type described as forming the bulk of the granuloma's characteristic "large cells with pale cytoplasm."
More Systemic effects of inflammation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.