Resolution of acute inflammation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Resolution of acute inflammation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
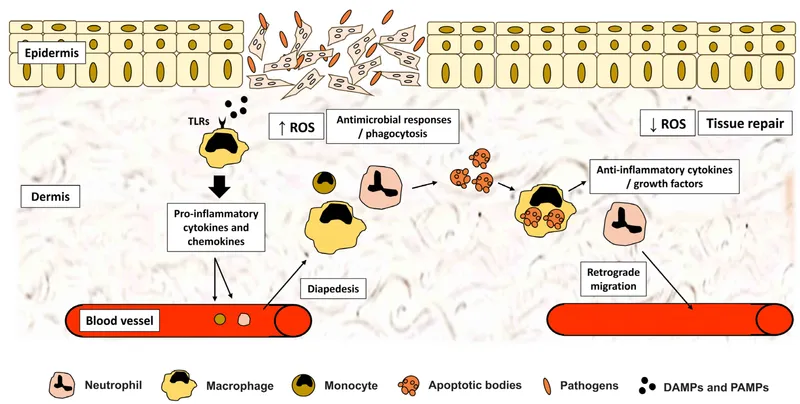
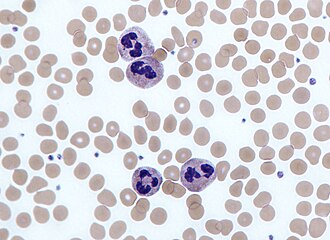
Resolution of acute inflammation US Medical PG Question 1: A 14-year-old girl presents with pain in the right lower quadrant of her abdomen. She describes the pain as sudden, severe, colicky, and associated with nausea and vomiting. Physical exam reveals tachycardia and severe tenderness to palpation with rebound in the right iliac region. Emergency laparotomy is performed which reveals an inflamed appendix. A presurgical blood cell count shows an increase in the number of cells having a multilobed nucleus and multiple cytoplasmic granules as shown in the image below. Which of the following is the main function of these cells?
- A. Blood clotting
- B. Transplant rejection
- C. Allergic reaction
- D. Phagocytosis (Correct Answer)
- E. Antigen presentation
Resolution of acute inflammation Explanation: ***Correct: Phagocytosis***
- The **multilobed nucleus** and **multiple cytoplasmic granules** are characteristic features of **neutrophils**, the most abundant white blood cells in acute inflammation.
- Neutrophils are the **primary phagocytic cells** in bacterial infections, engulfing and destroying bacteria and cellular debris.
- In acute appendicitis, neutrophilia (increased neutrophil count) is a hallmark finding, reflecting the body's response to bacterial infection.
- The cytoplasmic granules contain enzymes (e.g., myeloperoxidase, lysozyme) used to kill phagocytosed organisms.
*Incorrect: Blood clotting*
- This function is performed by **platelets** (thrombocytes) and clotting factors in the coagulation cascade.
- Platelets are anucleate cell fragments, not cells with multilobed nuclei.
*Incorrect: Transplant rejection*
- Primarily mediated by **T lymphocytes** (CD8+ cytotoxic T cells and CD4+ helper T cells) in cell-mediated immunity.
- This is an adaptive immune response, not the innate response characterized by neutrophil infiltration.
*Incorrect: Allergic reaction*
- Allergic reactions involve **mast cells** (releasing histamine) and **eosinophils** (which have bilobed nuclei, not multilobed).
- Eosinophils are associated with parasitic infections and allergic responses, not acute bacterial infections.
*Incorrect: Antigen presentation*
- Primarily performed by professional **antigen-presenting cells** (dendritic cells, macrophages, and B cells).
- These cells process and present antigens via MHC molecules to activate T cells.
- Neutrophils are **not efficient antigen-presenting cells**; their primary role is immediate pathogen destruction through phagocytosis.
Resolution of acute inflammation US Medical PG Question 2: A researcher is studying the interactions between foreign antigens and human immune cells. She has isolated a line of lymphocytes that is known to bind antigen-presenting cells. From this cell line, she has isolated a cell surface protein that binds to class I major histocompatibility complex molecules. The continued activation, proliferation and survival of this specific cell line requires which of the following signaling molecules?
- A. Interleukin 1
- B. Interleukin 4
- C. Interleukin 2 (Correct Answer)
- D. Interleukin 8
- E. Interleukin 6
Resolution of acute inflammation Explanation: ***Interleukin 2***
- The description of the lymphocyte binding the **constant portion of MHC class I** and requiring a signaling molecule for activation, proliferation, and survival points to a **T cell**.
- **Interleukin-2 (IL-2)** is a crucial cytokine for the proliferation, differentiation, and survival of T lymphocytes, acting in an autocrine or paracrine fashion after T cell activation.
*Interleukin 1*
- **Interleukin-1 (IL-1)** is primarily involved in inflammation and fever, produced by macrophages and other innate immune cells.
- While it can act as a costimulator for T cells, it is not the primary cytokine required for their sustained proliferation and survival after initial activation.
*Interleukin 4*
- **Interleukin-4 (IL-4)** is a key cytokine in humoral immunity, promoting B cell proliferation and differentiation, and inducing IgE class switching.
- It also plays a role in the differentiation of naive T cells into **Th2 cells**, but it is not the main cytokine for general T cell proliferation and survival.
*Interleukin 8*
- **Interleukin-8 (IL-8)**, also known as CXCL8, is a chemokine primarily responsible for attracting and activating neutrophils to sites of infection or inflammation.
- It does not have a direct role in the sustained proliferation and survival of activated lymphocytes.
*Interleukin 6*
- **Interleukin-6 (IL-6)** is a pleiotropic cytokine involved in acute phase reactions, hematopoiesis, and the immune response, particularly B cell differentiation and antibody production.
- Although it can influence T cell responses, it is not the primary growth factor for activated T lymphocytes as IL-2 is.
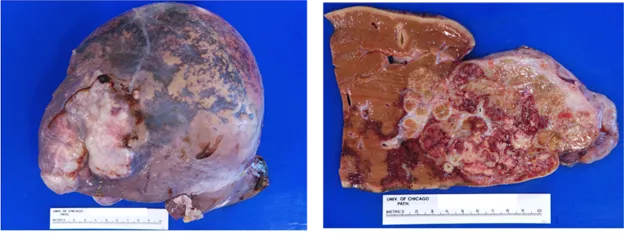
Resolution of acute inflammation US Medical PG Question 3: A 32-year-old man who recently emigrated from Somalia comes to the physician because of a 4-week history of fever, cough, and chest pain. He has had a 5-kg (11-lb) weight loss over the last 3 months despite no changes in appetite. His temperature is 38.1°C (100.6°F). Physical examination shows enlarged cervical lymph nodes. The lungs are clear to auscultation. The results of an interferon-γ release assay are positive. An x-ray of the chest shows bilateral mediastinal lymphadenopathy. A transbronchial needle aspiration biopsy of a mediastinal lymph node is performed; a photomicrograph of the specimen is shown. The structure indicated by the arrow is most likely comprised of which of the following types of cells?
- A. Natural killer cells
- B. B cells
- C. Fibroblasts
- D. Neutrophils
- E. Macrophages (Correct Answer)
Resolution of acute inflammation Explanation: ***Macrophages***
- The photomicrograph shows a **granuloma**, characterized by collections of **epithelioid histiocytes** (modified macrophages) and **multinucleated giant cells**, which are essentially fused macrophages.
- This morphology, coupled with the clinical picture of fever, cough, weight loss, positive interferon-γ release assay, and mediastinal lymphadenopathy in a patient from an endemic area, is highly suggestive of **tuberculosis**, a classic granulomatous disease.
*Natural killer cells*
- Natural killer cells are part of the innate immune system and are primarily involved in **killing virally infected cells** and **tumor cells**.
- They are not the primary cellular component forming the characteristic structure of a granuloma.
*B cells*
- B cells are responsible for **antibody production** and antigen presentation.
- While B cells may be present in the periphery of a granuloma, they do not form the core epithelioid and giant cell components.
*Fibroblasts*
- Fibroblasts produce **collagen** and the extracellular matrix, playing a role in **scar formation** and the fibrotic wall that can surround chronic granulomas.
- They do not constitute the primary cellular components of the inflammatory core of a granuloma.
*Neutrophils*
- Neutrophils are typically associated with **acute inflammation** and bacterial infections, characterized by pus formation.
- They are not the predominant cell type in the organized structure of a **granuloma** found in tuberculosis.
Resolution of acute inflammation US Medical PG Question 4: A 21-year-old male presents to the emergency department after losing his footing and falling 20 feet off a construction scaffold. He hit his left side on a railing on the way down before landing on his left arm. He denies loss of consciousness during the event or feelings of lightheadedness. He has no significant past medical or surgical history and does not take any regular medications. Evaluation in the trauma bay revealed mild lacerations to the upper and lower extremities, pain to palpation in the distal left forearm, and bruising to the upper left quadrant of the abdomen as well as the lower left thorax. Free fluid was found in the abdomen by ultrasound, fluids were started, and he was rushed to the operating room for an exploratory laparotomy. A heavily lacerated spleen was discovered and removed. No other sources of bleeding were found. Further workup determined he suffered a non-displaced left distal radius fracture and non-displaced 9th and 10th rib fractures. Which of the following should be administered to this patient?
- A. Total parenteral nutrition (TPN)
- B. Prophylactic ceftriaxone
- C. Pneumococcal vaccine (Correct Answer)
- D. Nothing by mouth (NPO)
- E. Open reduction internal fixation
Resolution of acute inflammation Explanation: ***Pneumococcal vaccine***
- The patient underwent a **splenectomy**, which renders him **immunocompromised** and highly susceptible to infections by **encapsulated bacteria**, particularly *Streptococcus pneumoniae*, *Haemophilus influenzae*, and *Neisseria meningitidis*.
- **Prompt vaccination** against pneumococcus (as well as Hib and meningococcus) is the **most critical intervention** post-splenectomy to prevent life-threatening **overwhelming post-splenectomy infection (OPSI)**.
- Vaccination should ideally be given **at least 14 days before splenectomy** when possible, but in emergency splenectomy cases like this, should be administered **before discharge** or as soon as the patient is stable.
*Total parenteral nutrition (TPN)*
- There is no indication in the clinical scenario to suggest this patient has **malabsorption, intestinal failure**, or is unable to tolerate **enteral feedings**.
- **Enteral nutrition** is generally preferred over TPN due to its fewer complications and role in maintaining gut integrity, assuming the gut is functional.
- This patient had a splenectomy without bowel injury and should be able to resume oral intake once stable post-operatively.
*Prophylactic ceftriaxone*
- While **prophylactic antibiotics** (typically **penicillin V or amoxicillin**) are actually recommended post-splenectomy for at least 2 years (and sometimes lifelong), **vaccination is the most important and primary intervention** that must be addressed first.
- Daily prophylactic antibiotics are part of post-splenectomy care, but **vaccination provides more comprehensive and durable protection** against encapsulated organisms.
- In the context of this question asking what "should be administered," vaccination takes priority as the most critical immediate intervention.
*Nothing by mouth (NPO)*
- While initial NPO status is common immediately after surgery, there is no information to suggest a prolonged need for NPO status.
- The patient had an **exploratory laparotomy** and **splenectomy**, but no other injuries were found (specifically no bowel injury) that would contraindicate eventual transition to oral intake.
*Open reduction internal fixation*
- The patient sustained a **non-displaced left distal radius fracture** and **non-displaced 9th and 10th rib fractures**.
- **Non-displaced fractures** are typically managed conservatively with immobilization (e.g., casting for the radius fracture), and surgery like ORIF is not indicated for such injuries.
- Rib fractures are generally managed with pain control and pulmonary hygiene rather than surgical fixation.
Resolution of acute inflammation US Medical PG Question 5: A 48-year-old man is brought to the emergency department with a stab wound to his chest. The wound is treated in the emergency room. Three months later he develops a firm 4 x 3 cm nodular mass with intact epithelium over the site of the chest wound. On local examination, the scar is firm, non-tender, and there is no erythema. The mass is excised and microscopic examination reveals fibroblasts with plentiful collagen. Which of the following processes is most likely related to the series of events mentioned above?
- A. Development of a fibrosarcoma
- B. Foreign body response from suturing
- C. Staphylococcal wound infection
- D. Poor wound healing from diabetes mellitus
- E. Keloid scar formation (Correct Answer)
Resolution of acute inflammation Explanation: ***Keloid scar formation***
- A **keloid** is a raised, firm, nodular scar that extends beyond the original wound boundaries and is characterized by excessive collagen deposition from **fibroblasts**.
- The delayed presentation (3 months), firm nature, absence of inflammation (no erythema, non-tender), and microscopic findings of fibroblasts with plentiful collagen are classic features of a keloid.
*Development of a fibrosarcoma*
- A fibrosarcoma is a **malignant tumor** of fibroblasts, which would typically present with more aggressive growth, often pain, and possibly ulceration, none of which are described.
- While composed of fibroblasts, fibrosarcomas exhibit **cellular atypia**, mitotic activity, and invasion, which are not mentioned in the microscopic description.
*Foreign body response from suturing*
- A foreign body response usually involves a **granulomatous inflammation** around foreign material, such as suture remnants.
- The microscopic description of "fibroblasts with plentiful collagen" without mention of inflammatory cells or foreign bodies makes this less likely.
*Staphylococcal wound infection*
- A **bacterial infection** would typically present with signs of acute inflammation such as erythema, warmth, pain, and possibly pus, shortly after the wound.
- The mass is described as non-tender with no erythema, and the 3-month delay makes an active infection less probable.
*Poor wound healing from diabetes mellitus*
- Poor wound healing in diabetes often manifests as **delayed closure**, chronic ulcers, and increased susceptibility to infection, rather than an overgrowth of fibrous tissue in the form of a nodular mass.
- While diabetes can affect wound healing, the specific description of a firm, nodular mass with excessive collagen points away from typical diabetic wound complications.
Resolution of acute inflammation US Medical PG Question 6: A 2-year-old boy has a history of recurrent bacterial infections, especially of his skin. When he has an infection, pus does not form. His mother reports that, when he was born, his umbilical cord took 5 weeks to detach. He is ultimately diagnosed with a defect in a molecule in the pathway that results in neutrophil extravasation. Which of the following correctly pairs the defective molecule with the step of extravasation that molecule affects?
- A. E-selectin; transmigration
- B. LFA-1 (integrin); tight adhesion (Correct Answer)
- C. ICAM-1; margination
- D. E-selectin; tight adhesion
- E. PECAM-1; transmigration
Resolution of acute inflammation Explanation: ***LFA-1 (integrin); tight adhesion***
- This patient's symptoms (recurrent bacterial infections, lack of pus formation, and delayed umbilical cord separation) are classic for **Leukocyte Adhesion Deficiency type 1 (LAD-1)**.
- **LAD-1** is caused by a defect in the **CD18 subunit** of **β2 integrins**, including **LFA-1** and **Mac-1**, which are crucial for the **tight adhesion** of neutrophils to endothelial cells.
*E-selectin; transmigration*
- **E-selectin** mediates the initial **rolling** of leukocytes along the endothelial surface, not transmigration.
- A defect in E-selectin would impair rolling, but the primary defect in LAD-1 is in tight adhesion.
*ICAM-1; margination*
- **ICAM-1** (Intercellular Adhesion Molecule-1) is an endothelial ligand that binds to integrins on leukocytes, facilitating **tight adhesion** and transmigration, not margination.
- **Margination** refers to the movement of leukocytes to the periphery of the blood vessel lumen.
*E-selectin; tight adhesion*
- **E-selectin** is involved in the initial **rolling** phase of extravasation by binding to sialyl Lewis X on leukocytes.
- It does not primarily mediate **tight adhesion**, which is facilitated by integrins binding to ICAM-1.
*PECAM-1; transmigration*
- **PECAM-1** (Platelet Endothelial Cell Adhesion Molecule-1) is primarily involved in **transmigration** (diapedesis), where leukocytes pass between endothelial cells.
- While important for extravasation, the characteristic findings of LAD-1 point to a defect earlier in the pathway, specifically tight adhesion.
Resolution of acute inflammation US Medical PG Question 7: A 12-year-old girl is brought to the physician by her mother 2 hours after cutting her hand while playing in the yard. Examination of the right hand shows a 2-cm laceration on the thenar region of the palm with some surrounding tenderness and erythema. The right palm appears mildly swollen in comparison to the left. In response to this patient's injury, the endothelial cells lining the blood vessels of the affected area express increased numbers of cellular adhesion molecules. Which of the following mediators is most likely directly responsible for the described change?
- A. Interferon alpha
- B. Interleukin-10
- C. Interleukin-1 (Correct Answer)
- D. Interferon gamma
- E. Interleukin-6
Resolution of acute inflammation Explanation: ***Interleukin-1***
- **IL-1** is a potent **pro-inflammatory cytokine** that directly induces the expression of **cellular adhesion molecules** (CAMs) on endothelial cells.
- This action facilitates the **recruitment of leukocytes** to the site of injury, a crucial step in the inflammatory response observed with pain, tenderness, and swelling.
*Interferon alpha*
- **Interferon alpha (IFN-α)** is primarily an **antiviral cytokine** and has limited direct effects on the immediate upregulation of endothelial adhesion molecules in acute injury.
- It is more involved in the early immune response to viral infections by inhibiting viral replication and activating natural killer (NK) cells.
*Interleukin-10*
- **Interleukin-10 (IL-10)** is an **anti-inflammatory cytokine** that functions to suppress the immune response and downregulate the production of pro-inflammatory cytokines and adhesion molecules.
- Its role is to resolve inflammation, not to initiate or enhance the early stages of leukocyte recruitment in acute injury.
*Interferon gamma*
- **Interferon gamma (IFN-γ)** is a powerful **pro-inflammatory cytokine**, but its main role in inflammation is different from directly inducing immediate CAM expression.
- It **activates macrophages** and enhances antigen presentation, playing a more significant role in chronic inflammation and adaptive immunity rather than the initial endothelial activation in acute injury.
*Interleukin-6*
- **Interleukin-6 (IL-6)** is a major **pro-inflammatory cytokine**, but its primary function in acute inflammation is more related to the **acute phase response** (e.g., fever, CRP production) rather than direct and immediate upregulation of endothelial adhesion molecules.
- While it contributes to systemic inflammation, **IL-1** and **TNF-α** are more directly and immediately responsible for inducing CAM expression on endothelial cells.
Resolution of acute inflammation US Medical PG Question 8: A researcher is studying how arachidonic acid metabolites mediate the inflammatory response in rats. She has developed multiple enzyme inhibitors that specifically target individual proteins in the arachidonic acid pathway. She injects these inhibitors in rats who have been exposed to common bacterial pathogens and analyzes their downstream effects. In one of her experiments, she injects a leukotriene B4 inhibitor into a rat and observes an abnormal cell response. Which of the following interleukins would most closely restore the function of one of the missing products?
- A. Interleukin 2
- B. Interleukin 4
- C. Interleukin 1
- D. Interleukin 5
- E. Interleukin 8 (Correct Answer)
Resolution of acute inflammation Explanation: ***Interleukin 8***
- **Leukotriene B4 (LTB4)** is a potent **chemoattractant** and activator of neutrophils.
- **Interleukin 8 (IL-8)**, also known as **CXCL8**, is a primary **chemoattractant** for neutrophils, functionally mimicking the role of LTB4 in recruiting these inflammatory cells to the site of infection.
*Interleukin 2*
- **IL-2** is primarily involved in the **growth, proliferation, and differentiation of T cells**, as well as the activation of B cells and natural killer cells.
- It does not have a significant role in **neutrophil chemotaxis**, which is the main function of LTB4.
*Interleukin 4*
- **IL-4** is crucial for **B cell activation** and class switching to IgE, and it's a key cytokine in the **Th2 immune response**.
- Its functions are related to **allergic reactions** and **parasitic infections**, not neutrophil recruitment.
*Interleukin 1*
- **IL-1** is a pro-inflammatory cytokine that mediates a wide range of immune responses, including **fever** and the activation of other immune cells.
- While it contributes to inflammation, it does not directly act as a **chemoattractant for neutrophils** in the same manner as LTB4 or IL-8.
*Interleukin 5*
- **IL-5** is primarily involved in the **growth and differentiation of eosinophils** and B cell IgA production.
- It plays a significant role in **allergic reactions** and defense against parasites, not neutrophil chemotaxis.
Resolution of acute inflammation US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Resolution of acute inflammation Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Resolution of acute inflammation US Medical PG Question 10: An immunology expert is explaining the functions of macrophages to biology students. He describes a hypothetical case scenario as follows: a potentially harmful gram-negative bacillus encounters a macrophage in the tissues. The Toll-like receptor (TLR) on the macrophage recognizes the bacterial lipopolysaccharide (LPS). The macrophage is activated by the binding of TLR with bacterial LPS and by interferon-γ (IFN-γ). Which of the following cytokines is most likely to be secreted by the activated macrophage?
- A. Interleukin-4 (IL-4)
- B. Interleukin-1 receptor antagonist (IL-1RA)
- C. Interleukin-10 (IL-10)
- D. Interleukin-2 (IL-2)
- E. Interleukin-12 (IL-12) (Correct Answer)
Resolution of acute inflammation Explanation: ***Interleukin-12 (IL-12)***
- Macrophage activation by **LPS (a PAMP recognized by TLR4)** and **IFN-γ (a macrophage-activating cytokine)** leads to the secretion of pro-inflammatory cytokines, with **IL-12** being a key mediator.
- **IL-12** is crucial for promoting **Th1 differentiation** and enhancing **NK cell activity**, thus linking innate and adaptive immunity against intracellular pathogens and tumor cells.
*Interleukin-4 (IL-4)*
- **IL-4** is primarily secreted by **Th2 cells, mast cells, and basophils**, and is involved in **allergic responses** and humoral immunity.
- It promotes **Th2 differentiation** and IgE production, which is not the primary response to a Gram-negative bacterial encounter as described.
*Interleukin-1 receptor antagonist (IL-1RA)*
- **IL-1RA** is an **anti-inflammatory cytokine** that blocks the effects of IL-1α and IL-1β, thereby downregulating inflammatory responses.
- While it can be produced by macrophages, initial activation by LPS and IFN-γ would trigger pro-inflammatory mediators before the release of antagonists to temper the response.
*Interleukin-10 (IL-10)*
- **IL-10** is a potent **anti-inflammatory cytokine** that suppresses the immune response, particularly by inhibiting cytokine production by macrophages and Th1 cells.
- Macrophage activation in response to a pathogen initially leads to pro-inflammatory cytokine secretion, with IL-10 typically arising later to resolve the inflammation.
*Interleukin-2 (IL-2)*
- **IL-2** is predominantly produced by **T lymphocytes**, especially **Th1 cells**, upon activation.
- Its main roles include **T cell proliferation**, differentiation, and maintenance of regulatory T cells, rather than being a primary cytokine secreted by activated macrophages in this context.
More Resolution of acute inflammation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.