Chronic inflammation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chronic inflammation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chronic inflammation US Medical PG Question 1: A 25-year-old man presents to the emergency department after a motor vehicle accident. He was the unrestrained front seat driver in a head on collision. The patient is unresponsive and his medical history is unknown. His temperature is 99.5°F (37.5°C), blood pressure is 67/38 mmHg, pulse is 190/min, respirations are 33/min, and oxygen saturation is 98% on room air. The patient is started on IV fluids, blood products, and norepinephrine. A FAST exam is performed and a pelvic binder is placed. One hour later, his temperature is 98.3°F (36.8°C), blood pressure is 119/66 mmHg, pulse is 110/min, respirations are 15/min, and oxygen saturation is 97% on room air. The patient is currently responsive. Management of the patient's pelvic fracture is scheduled by the orthopedic service. While the patient is waiting in the emergency department he suddenly complains of feeling hot, aches, and a headache. The patient's temperature is currently 101°F (38.3°C). He has not been given any pain medications and his past medical history is still unknown. Which of the following is the most likely diagnosis?
- A. Acute hemolytic transfusion reaction
- B. Febrile non-hemolytic transfusion reaction (Correct Answer)
- C. Sympathetic response to pain
- D. Minor blood group incompatibility
- E. Leukoagglutination reaction
Chronic inflammation Explanation: ***Febrile non-hemolytic transfusion reaction***
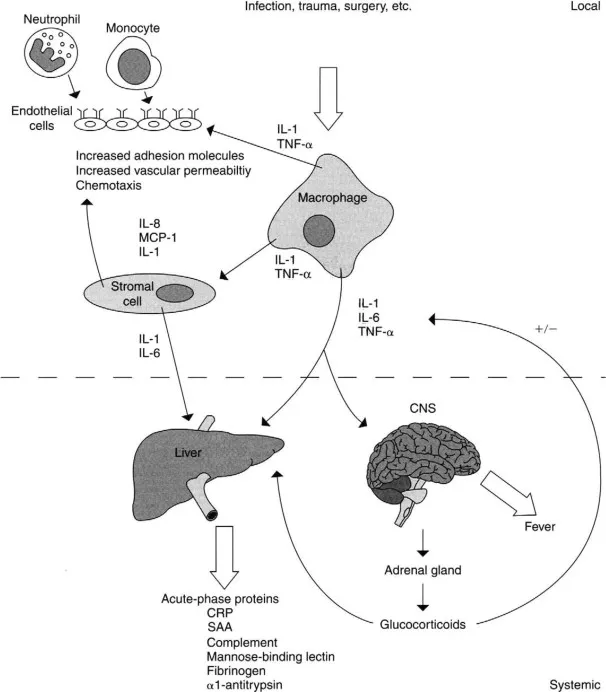
- This reaction is characterized by a **fever** and other constitutional symptoms (chills, headache, malaise) developing **within 4 hours of transfusion**, without evidence of hemolysis. The patient's symptoms and temperature rise after blood product administration fit this description.
- It is typically caused by antibodies in the recipient's plasma reacting with **leukocyte antigens** present on donor white blood cells or by **cytokines** released from donor leukocytes during storage.
*Acute hemolytic transfusion reaction*
- This reaction typically presents with more severe symptoms such as **hypotension**, **hemoglobinuria**, flank pain, and diffuse bleeding, indicating widespread intravascular hemolysis due to **ABO incompatibility**.
- Although the patient received blood products, his symptoms (feeling hot, aches, headache, mild fever) are not indicative of the severe, life-threatening nature of an acute hemolytic reaction.
*Sympathetic response to pain*
- While pain can cause a sympathetic response (tachycardia, hypertension), it typically does **not cause a fever** as seen in this patient.
- The patient's initial presentation included signs of shock, and after resuscitation, his vital signs normalized before the new symptoms appeared, suggesting a new process rather than ongoing pain alone.
*Minor blood group incompatibility*
- Reactions to minor blood group incompatibilities are usually **milder and delayed** compared to ABO incompatibilities.
- They often involve **extravascular hemolysis**, which might not present with the acute febrile reaction seen here, and are less common a cause of immediate febrile reactions.
*Leukoagglutination reaction*
- This is an older term for what is now often considered a type of **febrile non-hemolytic transfusion reaction (FNHTR)** caused by recipient antibodies to donor leukocyte antigens leading to leukocyte clumping.
- While related to FNHTR, the term "febrile non-hemolytic transfusion reaction" is the more encompassing and appropriate diagnosis given the typical symptom complex of fever, chills, and headache.
Chronic inflammation US Medical PG Question 2: A 7-year-old boy is brought to the physician because of a 5-day history of fever, malaise, and joint pain. He had a sore throat 4 weeks ago that resolved without treatment. His temperature is 38.6°C (101.5°F) and blood pressure is 84/62 mm Hg. Physical examination shows several firm, painless nodules under the skin near his elbows and the dorsal aspect of both wrists. Cardiopulmonary examination shows bilateral basilar crackles and a blowing, holosystolic murmur heard best at the cardiac apex. Both knee joints are warm. Laboratory studies show an erythrocyte sedimentation rate of 129 mm/h. The immune response seen in this patient is most likely due to the presence of which of the following?
- A. M protein (Correct Answer)
- B. CAMP factor
- C. TSST-1
- D. IgA protease
- E. Hyaluronic acid capsule
Chronic inflammation Explanation: ***M protein***
- The constellation of symptoms (recent sore throat, fever, joint pain, subcutaneous nodules, and a new heart murmur) is highly suggestive of **acute rheumatic fever (ARF)**, which is triggered by a preceding infection with **Group A Streptococcus (GAS)**.
- The **M protein** is a major virulence factor of GAS that elicits a strong immune response, and antibodies directed against it can cross-react with host tissues (molecular mimicry), leading to the inflammatory damage seen in ARF.
*CAMP factor*
- **CAMP factor** is a virulence factor produced by *Streptococcus agalactiae* (Group B Streptococcus), not Group A Streptococcus, which is responsible for ARF.
- Group B Streptococcus is primarily associated with neonatal infections and does not cause rheumatic fever.
*TSST-1*
- **Toxic Shock Syndrome Toxin-1 (TSST-1)** is a superantigen produced by *Staphylococcus aureus* and is responsible for **toxic shock syndrome**, not acute rheumatic fever.
- Toxic shock syndrome presents with abrupt onset of fever, hypotension, diffuse rash, and multi-organ dysfunction, which differs from the patient's presentation.
*IgA protease*
- **IgA protease** is an enzyme produced by several bacterial species, including *Neisseria meningitidis*, *Haemophilus influenzae*, and *Streptococcus pneumoniae*, that cleaves IgA antibodies.
- While it contributes to bacterial colonization of mucous membranes, it is not the primary virulence factor responsible for the immune response leading to acute rheumatic fever.
*Hyaluronic acid capsule*
- The **hyaluronic acid capsule** of *Streptococcus pyogenes* (GAS) is a virulence factor that helps in evading phagocytosis by mimicking host connective tissue.
- While it prevents immune detection and aids in colonization, it does not directly elicit the cross-reactive immune response responsible for the tissue damage in acute rheumatic fever; that role is attributed primarily to the M protein.
Chronic inflammation US Medical PG Question 3: A 3-year-old recent immigrant is diagnosed with primary tuberculosis. Her body produces T cells that do not have IL-12 receptors on their surface, and she is noted to have impaired development of Th1 T-helper cells. Which of the following cytokines would benefit this patient?
- A. IL-4
- B. IL-22
- C. TGF-beta
- D. IL-17
- E. Interferon-gamma (Correct Answer)
Chronic inflammation Explanation: ***Interferon-gamma***
- This patient has an impaired **Th1 response**, which is crucial for controlling intracellular infections like **tuberculosis** by activating macrophages.
- **Interferon-gamma** is the primary cytokine produced by **Th1 cells** that activates macrophages, leading to enhanced phagocytosis and killing of intracellular pathogens.
*IL-4*
- **IL-4** is a key cytokine produced by **Th2 cells**, which primarily drive **humoral immunity** and allergic responses, not cellular immunity against intracellular bacteria.
- Its administration would promote a **Th2 response**, which is not beneficial for combating **tuberculosis** and might even suppress the desirable Th1 response.
*IL-22*
- **IL-22** is mainly involved in **epithelial cell proliferation**, host defense at mucosal surfaces, and tissue repair.
- While it has a role in host defense against certain pathogens, it is not the primary cytokine required to compensate for a deficient **Th1 response** in **tuberculosis**.
*TGF-beta*
- **TGF-beta** is a pleiotropic cytokine with roles in cell growth, differentiation, and immune regulation, often acting as an **immunosuppressant** or driving **Treg differentiation**.
- It would not directly compensate for a lack of **Th1 cell function** needed to activate macrophages against **tuberculosis**.
*IL-17*
- **IL-17** is the signature cytokine of **Th17 cells**, which are important for host defense against **extracellular bacteria** and fungi, primarily by recruiting neutrophils.
- While it plays a role in some immune responses, it is not the crucial cytokine to boost in a patient with impaired **Th1 development** against **intracellular M. tuberculosis**.
Chronic inflammation US Medical PG Question 4: A 42-year-old woman presents complaining of pain in her hands. She reports that the pain is in both hands, and that it is usually worse in the morning. She reports that her hands are also stiff in the morning, but that this gradually improves throughout the morning. She notes, however, that her symptoms seem to be getting worse over the last three months. What is the most likely pathogenesis of her disease process?
- A. Production of antibodies against smooth muscle
- B. Anti-neutrophil cytoplasmic antibody production
- C. Production of antibodies against antibodies (Correct Answer)
- D. Type 1 hypersensitivity reaction
- E. Repetitive microtrauma
Chronic inflammation Explanation: ***Production of antibodies against antibodies***
- The patient's symptoms of **bilateral hand pain and morning stiffness** improving with activity, worsening over three months, are classic for **Rheumatoid Arthritis (RA)**.
- RA is characterized by the production of **rheumatoid factor (RF)**, an antibody (typically IgM) directed against the Fc portion of IgG, which is essentially an antibody against an antibody.
*Production of antibodies against smooth muscle*
- This describes the presence of **anti-smooth muscle antibodies (ASMA)**, which are characteristic of **Autoimmune Hepatitis type 1**.
- Autoimmune hepatitis primarily affects the liver, leading to symptoms like fatigue, jaundice, and elevated liver enzymes, not primarily joint pain.
*Anti-neutrophil cytoplasmic antibody production*
- This refers to **ANCA (anti-neutrophil cytoplasmic antibodies)**, which are associated with various forms of **vasculitis**, such as Granulomatosis with Polyangiitis (Wegener's), Microscopic Polyangiitis, and Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss).
- While vasculitis can cause systemic symptoms, the patient's presentation of symmetric, inflammatory arthritis is not typical for primary ANCA-associated vasculitis.
*Type 1 hypersensitivity reaction*
- A **type I hypersensitivity reaction** involves IgE-mediated mast cell degranulation, leading to immediate allergic reactions like asthma, anaphylaxis, or hives.
- This mechanism is completely unrelated to the pathogenesis of an autoimmune, chronic inflammatory arthritis like Rheumatoid Arthritis.
*Repetitive microtrauma*
- Repetitive microtrauma is more consistent with **osteoarthritis** or **occupational overuse injuries**.
- Osteoarthritis typically presents with pain that worsens with activity and improves with rest, **morning stiffness lasting less than 30 minutes**, and often affects weight-bearing joints or specific joints due to trauma or wear and tear, rather than the inflammatory pattern described.
Chronic inflammation US Medical PG Question 5: A 55-year-old homeless man is presented to the emergency department by a group of volunteers after they found him coughing up blood during 1 of the beneficiary dinners they offer every week. His medical history is unknown as he recently immigrated from Bangladesh. He says that he has been coughing constantly for the past 3 months with occasional blood in his sputum. He also sweats a lot at nights and for the past 2 days, he has been thirsty with increased frequency of urination and feeling hungrier than usual. The respiratory rate is 30/min and the temperature is 38.6°C (101.5°F). He looks emaciated and has a fruity smell to his breath. The breath sounds are reduced over the apex of the right lung. The remainder of the physical exam is unremarkable. Biochemical tests are ordered, including a hemoglobin A1c (HbA1c) (8.5%) and chest radiography reveals cavitations in the apical region of the right lung. Which of the following immune cells is most critical in orchestrating the formation and maintenance of the granulomatous structure that led to these cavitations?
- A. B lymphocytes
- B. Treg lymphocytes
- C. Epithelioid cells
- D. Th1 lymphocytes (Correct Answer)
- E. Th2 lymphocytes
Chronic inflammation Explanation: ***Th1 lymphocytes***
- The clinical picture strongly suggests **reactivation of tuberculosis** due to the cavitary lung lesions, constitutional symptoms, and likely immunocompromise from undiagnosed diabetes (HbA1c 8.5%).
- **Th1 lymphocytes** are crucial for the cell-mediated immune response against **intracellular pathogens** like *Mycobacterium tuberculosis*, producing **interferon-gamma** which activates macrophages to form granulomas and contain the infection, thus preventing dissemination and contributing to cavitation.
*B lymphocytes*
- **B lymphocytes** primarily mediate **humoral immunity** by producing antibodies, which are less critical for controlling intracellular bacterial infections like tuberculosis.
- While antibodies can play a role in modulating inflammation, they are not the primary cells involved in the **granuloma formation** and containment of *M. tuberculosis* within the lungs.
*Treg lymphocytes*
- **Treg lymphocytes** (regulatory T cells) primarily function to **suppress immune responses** to prevent autoimmunity and limit tissue damage.
- While they can modulate the immune response in tuberculosis, their main role is not in the initial formation of **cavities** or primary defense against the pathogen, but rather in regulating the overall inflammatory process.
*Epithelioid cells*
- **Epithelioid cells** are **activated macrophages** that form the core of granulomas, but they are not lymphocytes; they are derived from monocytes.
- They are a crucial component of the **granulomatous structure** itself, but their differentiation and activation are largely driven by cytokines produced by **Th1 lymphocytes**.
*Th2 lymphocytes*
- **Th2 lymphocytes** are primarily involved in immunity against **extracellular parasites** and in allergic reactions, mediating humoral responses through cytokines like **IL-4, IL-5, and IL-13**.
- An effective immune response against *Mycobacterium tuberculosis* is dominated by a **Th1 cellular response**, and a prominent Th2 response is generally considered detrimental or insufficient in controlling the infection.
Chronic inflammation US Medical PG Question 6: A 31-year-old woman scrapes her finger on an exposed nail and sustains a minor laceration. Five minutes later, her finger is red, swollen, and painful. She has no past medical history and does not take any medications. She drinks socially with her friends and does not smoke. The inflammatory cell type most likely to be prominent in this patient's finger has which of the following characteristics?
- A. Segmented nuclei (Correct Answer)
- B. Dramatically expanded endoplasmic reticulum
- C. Large cell with amoeboid movement
- D. Multiple peripheral processes
- E. Dark histamine containing granules
Chronic inflammation Explanation: ***Segmented nuclei***
- This scenario describes **acute inflammation** following a minor injury, with classic signs of **redness, swelling, and pain** within minutes.
- **Neutrophils** are the primary inflammatory cells in acute inflammation and are characterized by their **segmented (multi-lobed) nuclei.**
*Dramatically expanded endoplasmic reticulum*
- An expanded endoplasmic reticulum is characteristic of cells highly active in protein synthesis and secretion, such as **plasma cells** producing antibodies.
- Plasma cells are typically involved in **chronic inflammation** and adaptive immune responses, not rapid acute inflammation.
*Large cell with amoeboid movement*
- This describes **macrophages**, which are phagocytic cells important in both acute and chronic inflammation, and in cleaning up debris.
- While macrophages are present, **neutrophils** are the predominant early responders in acute bacterial infections and tissue injury.
*Multiple peripheral processes*
- This description is characteristic of **dendritic cells**, which are antigen-presenting cells that initiate adaptive immune responses.
- Dendritic cells play a role in linking innate and adaptive immunity but are not the primary inflammatory cell type in the immediate acute response.
*Dark histamine containing granules*
- This description applies to **mast cells** and **basophils**, which release histamine and other mediators in allergic reactions and acute inflammation.
- While mast cells are involved in the immediate response by releasing mediators, **neutrophils** are the main cellular players migrating to the site of injury.
Chronic inflammation US Medical PG Question 7: A 34-year-old woman comes to the physician because of a 6-week history of fever and productive cough with blood-tinged sputum. She has also had a 4-kg (8.8-lb) weight loss during the same time period. Examination shows enlarged cervical lymph nodes. An x-ray of the chest shows a 2.5-cm pulmonary nodule in the right upper lobe. A biopsy specimen of the lung nodule shows caseating granulomas with surrounding multinucleated giant cells. Which of the following is the most likely underlying cause of this patient's pulmonary nodule?
- A. Combined type III/IV hypersensitivity reaction
- B. IgE-mediated mast cell activation
- C. Immune complex deposition
- D. Antibody-mediated cytotoxic reaction
- E. Delayed T cell-mediated reaction (Correct Answer)
Chronic inflammation Explanation: ***Delayed T cell-mediated reaction***
- The presence of **caseating granulomas** with **multinucleated giant cells** is characteristic of tuberculosis, which is mediated by a **Type IV hypersensitivity reaction**.
- This reaction involves **T cells** and **macrophages** forming granulomas to wall off persistent intracellular pathogens.
*Combined type III/IV hypersensitivity reaction*
- While granulomas can sometimes involve aspects of **Type III hypersensitivity** (immune complex deposition), **caseating granulomas** are primarily a feature of **Type IV (delayed T cell-mediated) hypersensitivity**.
- **Type III reactions** are more typically associated with vasculitis or glomerulonephritis, which are not the primary features here.
*IgE-mediated mast cell activation*
- This describes a **Type I hypersensitivity reaction**, responsible for immediate allergic reactions like asthma or anaphylaxis.
- The patient's symptoms (fever, weight loss, productive cough, granulomas) are not consistent with an **IgE-mediated response**.
*Immune complex deposition*
- This is characteristic of a **Type III hypersensitivity reaction**, where antigen-antibody complexes deposit in tissues, leading to inflammation and damage.
- While Type III reactions can cause inflammation, they typically don't manifest as **caseating granulomas** and the chronic, progressive symptoms described.
*Antibody-mediated cytotoxic reaction*
- This describes a **Type II hypersensitivity reaction**, where antibodies directly bind to antigens on cell surfaces, leading to cell lysis (e.g., autoimmune hemolytic anemia).
- The clinical picture of **granulomatous inflammation** is not consistent with a direct **antibody-mediated cytotoxic reaction**.
Chronic inflammation US Medical PG Question 8: A 12-year-old child is exposed to pollen while playing outside. The allergen stimulates TH2 cells of his immune system to secrete a factor that leads to B-cell class switching to IgE. What factor is secreted by the TH2 cell?
- A. IL-4 (Correct Answer)
- B. IL-22
- C. TGF-beta
- D. IL-17
- E. IFN-gamma
Chronic inflammation Explanation: ***IL-4***
- **Interleukin-4 (IL-4)** is a key cytokine produced by **TH2 cells** that promotes **B-cell class switching to IgE**, central to allergic reactions.
- It also stimulates the differentiation of naive T cells into **TH2 cells**, further amplifying the **allergic response**.
*IL-22*
- **IL-22** is primarily involved in maintaining **epithelial barrier integrity** and promoting **tissue repair**, especially in the gut and skin.
- It does not play a direct role in **IgE class switching** or the pathogenesis of type I hypersensitivity.
*TGF-beta*
- **TGF-beta (Transforming Growth Factor-beta)** is a pleiotropic cytokine involved in **cell growth**, differentiation, apoptosis, and immune regulation, particularly promoting **Treg cell development** and IgA class switching.
- It primarily suppresses rather than promotes **allergic reactions** and IgE production.
*IL-17*
- **IL-17** is a cytokine predominantly produced by **TH17 cells** and is crucial in protection against **extracellular bacteria and fungi**.
- It is associated with **autoimmune diseases** and inflammation but not directly with IgE-mediated allergic responses.
*IFN-gamma*
- **Interferon-gamma (IFN-gamma)** is a critical **TH1 cytokine** that activates macrophages, enhances natural killer cell activity, and promotes the cell-mediated immune response.
- It typically **inhibits TH2 responses** and IgE production, thus working against the development of allergic reactions.
Chronic inflammation US Medical PG Question 9: A 37-year-old man presents to his primary care physician because he has had constipation for the last several weeks. He has also been feeling lethargic and complains that this winter has been particularly cold. He also complains that he has been gaining weight despite no change in his normal activities. He reveals that two months prior to presentation he had what felt like the flu for which he took Tylenol and did not seek medical attention. Several days after this he developed anterior neck pain. Which of the following findings would most likely be seen on biopsy of this patient's abnormality?
- A. Focal hyperplasia
- B. Germinal follicles
- C. Scalloped clear areas
- D. Fibrous tissue
- E. Granulomatous inflammation (Correct Answer)
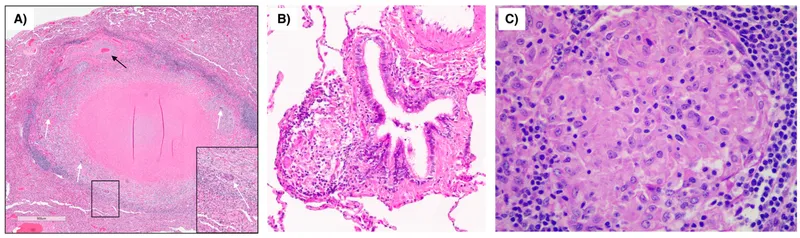
Chronic inflammation Explanation: ***Granulomatous inflammation***
- The patient's presentation with **constipation**, **lethargy**, **cold intolerance**, and **weight gain** after a flu-like illness followed by **anterior neck pain** is highly suggestive of **subacute granulomatous thyroiditis (de Quervain thyroiditis)**.
- A biopsy of the thyroid in cases of de Quervain thyroiditis typically reveals **granulomatous inflammation** with scattered **giant cells** and lymphocytes, reflecting the destructive inflammatory process.
*Focal hyperplasia*
- **Focal hyperplasia** is characterized by an increase in the number of thyroid follicular cells and is seen in conditions like **Graves' disease** or **multinodular goiter**, particularly when the gland is overstimulated.
- This finding would not be expected in subacute granulomatous thyroiditis, where the primary pathology is destruction rather than proliferation.
*Germinal follicles*
- **Germinal follicles** are characteristic of chronic lymphocytic thyroiditis (**Hashimoto's thyroiditis**), an autoimmune condition where the thyroid gland is infiltrated by lymphocytes, plasma cells, and macrophages.
- While Hashimoto's can cause hypothyroidism, the preceding flu-like illness and acute neck pain make de Quervain thyroiditis a more likely diagnosis.
*Scalloped clear areas*
- **Scalloped clear areas** at the colloid-epithelial interface, also known as **colloid resorption vacuoles**, are a histological feature of **hyperactive thyroid follicles**, typically seen in conditions causing hyperthyroidism like **Graves' disease**.
- The patient's symptoms of lethargy, cold intolerance, and weight gain indicate hypothyroidism, which can follow the initial hyperthyroid phase of de Quervain thyroiditis but are not indicative of active hyperfunction on biopsy at this stage.
*Fibrous tissue*
- An increased amount of **fibrous tissue** is characteristic of **Riedel's thyroiditis**, a rare condition characterized by dense fibrosis that replaces normal thyroid parenchyma and can extend into surrounding neck structures.
- This patient's presentation with a preceding febrile illness and neck pain is not typical for Riedel's thyroiditis, which usually presents as a hard, fixed mass without an antecedent viral infection.
Chronic inflammation US Medical PG Question 10: A 45-year-old immigrant presents with unintentional weight loss, sleep hyperhidrosis, and a persistent cough. He says these symptoms have been present for quite some time. Upon imaging, many granulomas in the upper lobes are present. It is noted that these apical granulomas have centers of necrosis that appear cheese-like in appearance. Encircling the area of necrosis are large cells with cytoplasms pale in color. Of the following surface markers, which one is most closely associated with these cells?
- A. CD20
- B. CD3
- C. CD4
- D. CD14 (Correct Answer)
- E. CD8
Chronic inflammation Explanation: ***CD14***
- The description of **caseating granulomas** in the upper lobes with large cells having pale cytoplasm points towards **tuberculosis** and the presence of **epithelioid macrophages**.
- **CD14** is a surface marker commonly found on **monocytes** and **macrophages**, making it the most appropriate choice among the given options.
- Note: While epithelioid macrophages (the activated form seen in granulomas) may downregulate CD14 compared to circulating monocytes, CD14 remains the most closely associated macrophage marker among these choices. **CD68** would be the ideal marker for tissue macrophages, but it is not listed.
*CD20*
- **CD20** is a surface marker characteristic of **B lymphocytes**.
- While B cells might be present in inflammatory lesions, they are not the predominant cell type described as "large cells with pale cytoplasm" forming the granuloma.
*CD3*
- **CD3** is a pan T-cell marker, indicating the presence of all types of **T lymphocytes**.
- While T cells (specifically CD4+ T helper cells) are crucial in granuloma formation, the "large cells with pale cytoplasm" encasing the necrosis specifically refer to epithelioid macrophages, not T cells.
*CD4*
- **CD4** is a surface marker for **helper T lymphocytes**.
- **CD4+ T cells** play a critical role in orchestrating the immune response and granuloma formation in tuberculosis through IFN-γ secretion, but the description of the large cells with pale cytoplasm refers to macrophages, not lymphocytes.
*CD8*
- **CD8** is a surface marker for **cytotoxic T lymphocytes**.
- **CD8+ T cells** are also involved in the immune response to mycobacterial infection but are not the primary cell type described as forming the bulk of the granuloma's characteristic "large cells with pale cytoplasm."
More Chronic inflammation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.