Chemical mediators of inflammation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chemical mediators of inflammation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chemical mediators of inflammation US Medical PG Question 1: A 6-year-old boy is presented to a pediatric clinic by his mother with complaints of fever, malaise, and cough for the past 2 days. He frequently complains of a sore throat and has difficulty eating solid foods. The mother mentions that, initially, the boy’s fever was low-grade and intermittent but later became high grade and continuous. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The past medical history is noncontributory. The boy takes a multivitamin every day. The mother reports that he does well in school and is helpful around the house. The boy’s vital signs include blood pressure 110/65 mm Hg, heart rate 110/min, respiratory rate 32/min, and temperature 38.3°C (101.0°F). On physical examination, the boy appears uncomfortable and has difficulty breathing. His heart is mildly tachycardic with a regular rhythm and his lungs are clear to auscultation bilaterally. Oropharyngeal examination shows that his palatine tonsils are covered with pus and that there is erythema of the surrounding mucosa. Which of the following mediators is responsible for this patient’s elevated temperature?
- A. Leukotriene D4
- B. Prostaglandin F2
- C. Prostaglandin E2 (Correct Answer)
- D. Thromboxane A2
- E. Prostaglandin I2
Chemical mediators of inflammation Explanation: ***Prostaglandin E2***
- **Prostaglandin E2 (PGE2)** is a key mediator of fever, acting directly on the **hypothalamus** to reset the body's thermoregulatory set point.
- In response to infection and inflammation, immune cells release **pyrogens** (like IL-1, TNF-alpha), which stimulate PGE2 synthesis in the brain, leading to increased body temperature.
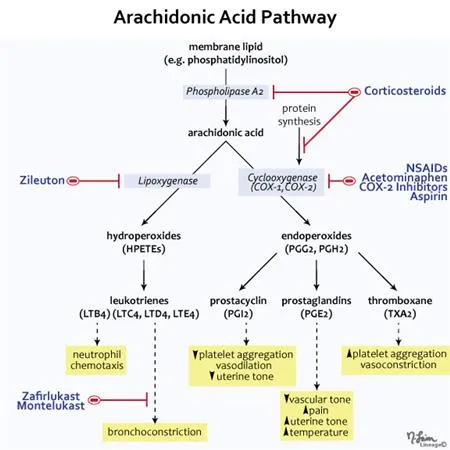
*Leukotriene D4*
- **Leukotriene D4 (LTD4)** is a potent mediator of **bronchoconstriction** and increased **vascular permeability**, particularly in allergic reactions and asthma.
- While it plays a role in inflammation, it does not directly cause fever by altering the hypothalamic set point.
*Prostaglandin F2*
- **Prostaglandin F2 (PGF2)** has various physiological roles, including **uterine contraction** and **bronchoconstriction**, and is important for reproductive functions.
- It is not primarily involved in mediating the febrile response to infection.
*Thromboxane A2*
- **Thromboxane A2 (TXA2)** is predominantly involved in **platelet aggregation** and **vasoconstriction**, playing a crucial role in hemostasis and thrombosis.
- While it is a product of the arachidonic acid pathway, it does not directly contribute to fever.
*Prostaglandin I2*
- **Prostaglandin I2 (PGI2)**, also known as **prostacyclin**, is a potent **vasodilator** and inhibitor of **platelet aggregation**, protecting the vascular endothelium.
- It typically counteracts the effects of TXA2 and is not a mediator of fever.
Chemical mediators of inflammation US Medical PG Question 2: A 34-year-old man comes to the physician because of palpitations, shortness of breath, diarrhea, and abdominal cramps for 2 months. Physical examination shows cutaneous flushing of the face. Auscultation of the chest shows bilateral wheezing. A 24-hour urine collection shows increased 5-hydroxyindoleacetic acid (5-HIAA) concentration. A contrast-enhanced CT scan of the abdomen shows an intestinal tumor with extensive metastasis to the liver. A diagnosis of an inoperable disease is made and the patient is started on treatment with octreotide. Six weeks later, the patient's symptoms have improved except for his abdominal pain and frequent loose stools. The physician suggests enrolling the patient in a trial to test additional treatment with a new drug that has been shown to improve symptoms in other patients with the same condition. The expected beneficial effect of this new drug is most likely caused by inhibition of which of the following?
- A. Histidine decarboxylase
- B. Plasma kallikrein
- C. Vasoactive intestinal peptide
- D. Tryptophan hydroxylase (Correct Answer)
- E. Dopamine β-hydroxylase
Chemical mediators of inflammation Explanation: ***Tryptophan hydroxylase***
- This patient presents with symptoms consistent with **carcinoid syndrome** from an intestinal neuroendocrine tumor with liver metastases. The increased urinary **5-HIAA** confirms serotonin overproduction.
- While existing treatment with **octreotide** (a somatostatin analog) controls most symptoms, persistent abdominal pain and diarrhea suggest continued serotonin effects. A new drug targeting **tryptophan hydroxylase** would inhibit the rate-limiting step in serotonin synthesis, thus reducing serotonin levels.
*Histidine decarboxylase*
- This enzyme converts **histidine to histamine**. While histamine can contribute to flushing in some carcinoid tumors, it is not the primary mediator of the systemic symptoms in this case.
- The main issue here is serotonin overproduction, not histamine.
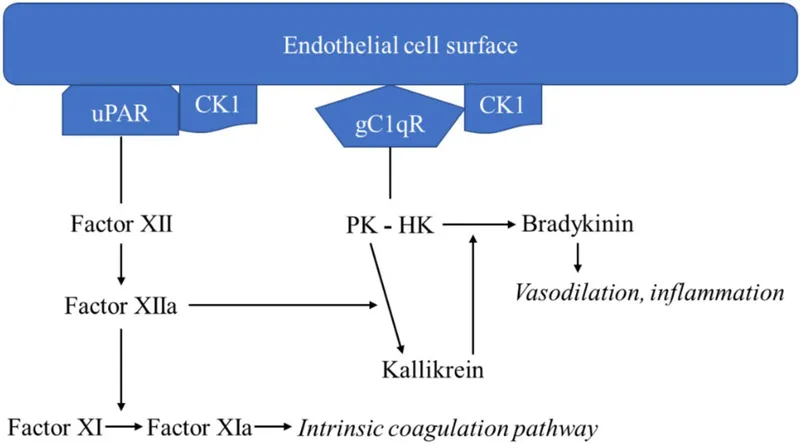
*Plasma kallikrein*
- **Plasma kallikrein** is involved in the kinin-kallikrein system, which produces **bradykinin**, a potent vasodilator. While bradykinin can cause flushing, it is not primarily responsible for the GI symptoms or serotonin overproduction seen in carcinoid syndrome.
- Inhibiting plasma kallikrein would not address the fundamental problem of excess serotonin.
*Vasoactive intestinal peptide*
- **VIP (Vasoactive Intestinal Peptide)** is a neuroendocrine peptide that can cause watery diarrhea and flushing, often associated with **VIPomas**.
- However, the patient's elevated **5-HIAA** strongly points towards serotonin overproduction from a carcinoid tumor, not a VIPoma.
*Dopamine β-hydroxylase*
- This enzyme converts **dopamine to norepinephrine**. This pathway is relevant to catecholamine synthesis, not serotonin.
- This enzyme would be targeted in conditions involving excess catecholamines (e.g., pheochromocytoma), which is not the case here.
Chemical mediators of inflammation US Medical PG Question 3: An investigator is studying the effect of different cytokines on the growth and differentiation of B cells. The investigator isolates a population of B cells from the germinal center of a lymph node. After exposure to a particular cytokine, these B cells begin to produce an antibody that prevents attachment of pathogens to mucous membranes but does not fix complement. Which of the following cytokines is most likely responsible for the observed changes in B-cell function?
- A. Interleukin-5 (Correct Answer)
- B. Interleukin-6
- C. Interleukin-8
- D. Interleukin-2
- E. Interleukin-4
Chemical mediators of inflammation Explanation: ***Interleukin-5***
- The antibody described (prevents pathogen attachment to mucous membranes, does not fix complement) is characteristic of **IgA**.
- **IL-5** plays a crucial role in promoting **IgA secretion** by differentiated B cells and supports B cell growth and differentiation in mucosal immunity.
- IL-5 works synergistically with **TGF-β** (the primary cytokine for IgA class switching) to enhance IgA production, particularly in mucosal-associated lymphoid tissue.
- Among the options provided, **IL-5 has the strongest association with IgA production**.
*Interleukin-4*
- **IL-4** is the primary cytokine driving class switching to **IgE** (and IgG4), not IgA.
- IL-4 is central to **allergic responses** and type 2 immunity, promoting B cells to produce IgE antibodies against allergens and parasites.
- It does not play a significant role in IgA production or mucosal immunity.
*Interleukin-6*
- **IL-6** is a pleiotropic cytokine involved in acute phase reactions, inflammation, and promoting B cell **differentiation into plasma cells**.
- While it supports general B cell maturation and antibody secretion, it is not specifically associated with **IgA production** or class switching.
*Interleukin-8*
- **IL-8** (CXCL8) is a **chemokine** that primarily recruits and activates neutrophils during inflammation.
- It has no direct role in B cell class switching or antibody production.
*Interleukin-2*
- **IL-2** is essential for T cell proliferation and differentiation, enhancing **cell-mediated immunity**.
- While it can indirectly affect B cell responses through T cell help, it is not directly responsible for promoting **IgA production** or class switching.
Chemical mediators of inflammation US Medical PG Question 4: A 55-year-old woman with diabetes presents to the emergency department due to swelling of her left leg, fever, and chills for the past 2 days. The woman’s maximum recorded temperature at home was 38.3°C (101.0°F). Her left leg is red and swollen from her ankle to the calf, with an ill-defined edge. Her vital signs include: blood pressure 120/78 mm Hg, pulse rate 94/min, temperature 38.3°C (101.0°F), and respiratory rate 16/min. On physical examination, her left leg shows marked tenderness and warmth compared with her right leg. The left inguinal lymph node is enlarged to 3 x 3 cm. Which of the following chemical mediators is the most likely cause of the woman’s fever?
- A. Bradykinin
- B. Histamine
- C. PGE2 (Correct Answer)
- D. Arachidonic acid
- E. LTB4
Chemical mediators of inflammation Explanation: ***PGE2***
- **Prostaglandin E2 (PGE2)** is a potent **pyrogen** that acts on the **hypothalamus** to reset the body's thermoregulatory set point, leading to fever.
- In infections like **cellulitis**, inflammatory mediators stimulate the production of PGE2, causing the systemic symptom of fever.
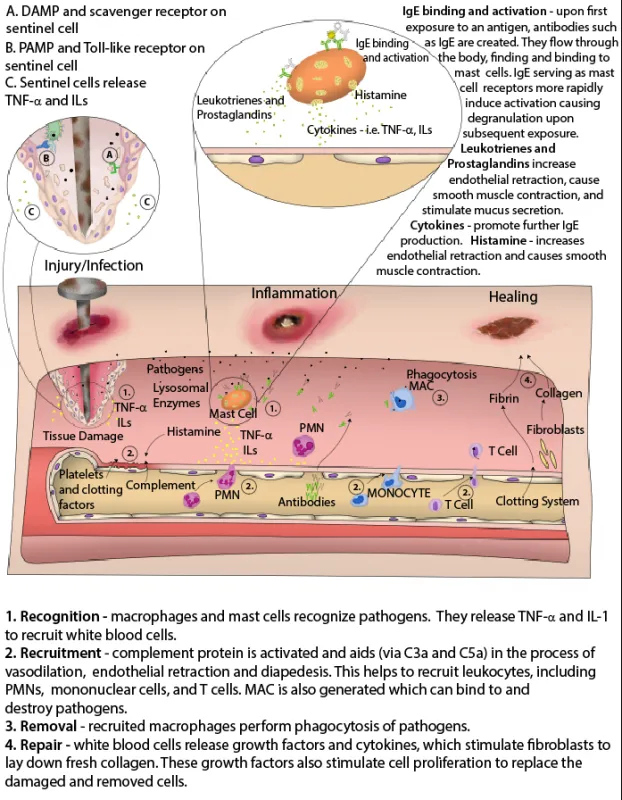
*Bradykinin*
- **Bradykinin** primarily mediates **pain** and **vasodilation** at the site of inflammation.
- While it contributes to local signs of inflammation, it is not a direct mediator of systemic fever.
*Histamine*
- **Histamine** is a key mediator in immediate **hypersensitivity reactions** and local inflammation, causing **vasodilation** and increased **vascular permeability**.
- It does not directly induce fever by acting on the thermoregulatory center.
*Arachidonic acid*
- **Arachidonic acid** is a **precursor** molecule derived from membrane phospholipids, which is metabolized to various inflammatory mediators like prostaglandins and leukotrienes.
- It is not a direct chemical mediator of fever itself; rather, its downstream products such as PGE2 are.
*LTB4*
- **Leukotriene B4 (LTB4)** is a potent **chemotactic agent** for neutrophils, playing a role in immune cell recruitment to the site of inflammation.
- While involved in inflammation, LTB4 does not directly cause fever.
Chemical mediators of inflammation US Medical PG Question 5: A researcher is studying the circulating factors that are released when immune cells are exposed to antigens. Specifically, she is studying a population of CD2+ cells that have been activated acutely. In order to determine which factors are secreted by these cells, she cultures the cells in media and collects the used media from these plates after several days. She then purifies a small factor from this media and uses it to stimulate various immune cell types. She finds that this factor primarily seems to increase the growth and prolong the survival of other CD2+ cells. Which of the following is most likely the factor that was purified by this researcher?
- A. Interleukin-2 (Correct Answer)
- B. Interleukin-3
- C. Interleukin-4
- D. Interleukin-5
- E. Interleukin-1
Chemical mediators of inflammation Explanation: ***Interleukin-2***
- **Interleukin-2 (IL-2)** is a crucial cytokine for the **growth**, **proliferation**, and **survival** of T lymphocytes, which are CD2+ cells.
- Activated T cells, like the acute CD2+ cells in the scenario, are a primary source of IL-2, and IL-2 acts in an **autocrine** and **paracrine** fashion to stimulate other T cells.
*Interleukin-3*
- **Interleukin-3 (IL-3)** primarily stimulates the growth and differentiation of **hematopoietic stem cells** and progenitors, not specifically mature CD2+ cells.
- It plays a role in the development of various myeloid cell lineages and mast cells, and its main effect is not confined to T cells.
*Interleukin-4*
- **Interleukin-4 (IL-4)** is critical for the differentiation of naive T helper cells into **Th2 cells** and is a key cytokine for **B cell proliferation** and **antibody class switching** to IgE.
- While it has immunomodulatory effects on T cells, its primary role is not in promoting the generalized growth and survival of other CD2+ cells.
*Interleukin-5*
- **Interleukin-5 (IL-5)** is predominantly involved in the growth, differentiation, and activation of **eosinophils**.
- It also plays a role in B cell growth and IgA production, but its effects are not primarily on universal CD2+ cell growth and survival.
*Interleukin-1*
- **Interleukin-1 (IL-1)** is a **pro-inflammatory cytokine** produced by macrophages, monocytes, and other immune cells in response to infection or injury.
- It primarily mediates **acute phase responses**, fever, and activates endothelial cells, but its main function is not to promote the growth and survival of T lymphocytes.
Chemical mediators of inflammation US Medical PG Question 6: A father brings his 3-year-old son to the pediatrician because he is concerned about his health. He states that throughout his son's life he has had recurrent infections despite proper treatment and hygiene. Upon reviewing the patient's chart, the pediatrician notices that the child has been infected multiple times with S. aureus, Aspergillus, and E. coli. Which of the following would confirm the most likely cause of this patient's symptoms?
- A. Increased IgM, Decreased IgG, IgA, and IgE
- B. Negative nitroblue-tetrazolium test (Correct Answer)
- C. Positive nitroblue-tetrazolium test
- D. Normal dihydrorhodamine (DHR) flow cytometry test
- E. Increased IgE and IgA, Decreased IgM
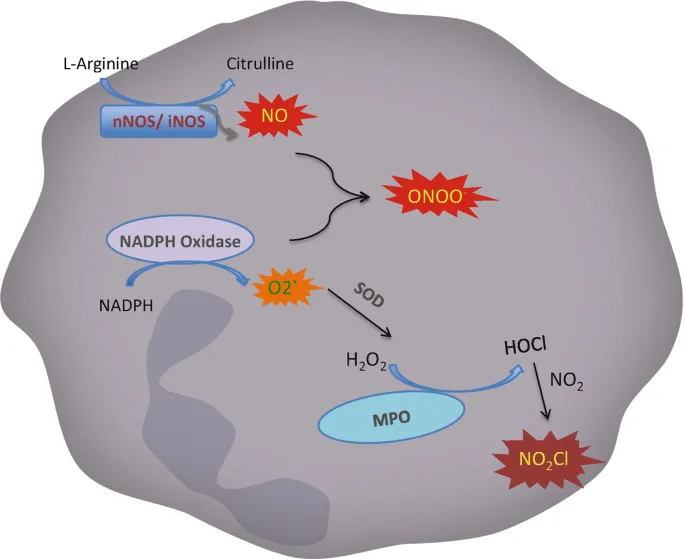
Chemical mediators of inflammation Explanation: ***Negative nitroblue-tetrazolium test***
- A **negative nitroblue-tetrazolium (NBT) test** indicates an inability of phagocytes to produce a respiratory burst, which is characteristic of **Chronic Granulomatous Disease (CGD)**.
- CGD patients suffer from recurrent infections with catalase-positive organisms such as *Staphylococcus aureus*, *Aspergillus*, and *E. coli*, consistent with the patient's history.
*Increased IgM, Decreased IgG, IgA, and IgE*
- This pattern of immunoglobulin levels is characteristic of **X-linked hyper-IgM syndrome**, where there is a defect in CD40L on T cells.
- While it also causes recurrent infections, the typical pathogens differ from those stated in the question, often including *Pneumocystis jirovecii*.
*Positive nitroblue-tetrazolium test*
- A **positive NBT test** indicates that phagocytes are capable of producing a respiratory burst and forming superoxide, thus ruling out CGD.
- This result would be expected in a healthy individual or someone with an immunodeficiency not affecting the phagocytic oxidative burst.
*Normal dihydrorhodamine (DHR) flow cytometry test*
- A **normal DHR flow cytometry test** indicates that neutrophils can produce reactive oxygen species (ROS) effectively, meaning the respiratory burst is intact.
- This result would rule out CGD, as CGD patients have an abnormal (decreased) DHR test.
*Increased IgE and IgA, Decreased IgM*
- This specific pattern of immunoglobulin abnormalities is not typically associated with a single, well-defined primary immunodeficiency that would present with the described infections.
- **Hyper-IgE syndrome (Job's syndrome)**, for example, features very high IgE levels but usually a normal IgM.
Chemical mediators of inflammation US Medical PG Question 7: A 7-year-old boy with asthma is brought to the physician because of a 1-month history of worsening shortness of breath and cough. The mother reports that the shortness of breath usually occurs when he is exercising with his older brother. His only medication is an albuterol inhaler that is taken as needed. The physician considers adding zafirlukast to his drug regimen. Which of the following is the most likely mechanism of action of this drug?
- A. Antagonism at muscarinic receptors
- B. Blockade of 5-lipoxygenase pathway
- C. Inhibition of mast cell degranulation
- D. Inhibition of phosphodiesterase
- E. Antagonism at leukotriene receptors (Correct Answer)
Chemical mediators of inflammation Explanation: ***Antagonism at leukotriene receptors***
- **Zafirlukast** is a **leukotriene receptor antagonist** (LTRA) that blocks the action of leukotrienes at their CysLT1 receptors.
- This action helps to reduce **bronchoconstriction**, airway edema, and inflammation, which are key features of asthma pathophysiology.
*Antagonism at muscarinic receptors*
- This is the mechanism of action for **anticholinergic bronchodilators** like **ipratropium** or **tiotropium**, which are not **zafirlukast**.
- These drugs primarily prevent **acetylcholine-induced bronchoconstriction** but do not target the leukotriene pathway.
*Blockade of 5-lipoxygenase pathway*
- This is the mechanism of **zileuton**, a **leukotriene synthesis inhibitor**, which prevents the formation of all leukotrienes.
- While it targets leukotrienes, it is distinct from **receptor antagonism**, which is how **zafirlukast** works.
*Inhibition of mast cell degranulation*
- This is the mechanism of **mast cell stabilizers** such as **cromolyn sodium** or **nedocromil**, which prevent the release of inflammatory mediators.
- This action differs from the direct receptor blockade provided by **zafirlukast**.
*Inhibition of phosphodiesterase*
- This is the mechanism of **methylxanthines** like **theophylline**, which increase intracellular cAMP and lead to **bronchodilation**.
- This is a distinct pharmacological class and mechanism from **zafirlukast**.
Chemical mediators of inflammation US Medical PG Question 8: Two days after being admitted for acute myocardial infarction, a 61-year-old man has sharp, substernal chest pain that worsens with inspiration and improves when leaning forward. Cardiac examination shows a scratchy sound best heard over the left sternal border. Histopathological examination of the infarcted myocardial tissue is most likely to show which of the following findings?
- A. Neutrophilic infiltration
- B. Collagenous scar tissue
- C. Normal myocardium
- D. Coagulative necrosis (Correct Answer)
- E. Granulation tissue with macrophages
Chemical mediators of inflammation Explanation: ***Coagulative necrosis***
- The patient's clinical presentation (sharp, substernal chest pain, worsening with inspiration, improving while leaning forward, and a scratchy pericardial friction rub) indicates **post-MI fibrinous pericarditis**, a common complication occurring 2-4 days after myocardial infarction.
- At **day 2 post-MI**, the infarcted myocardium demonstrates **coagulative necrosis** as the primary and most characteristic histopathological finding, representing irreversible ischemic cell death with preserved tissue architecture.
- While neutrophilic infiltration is also present at this timepoint, coagulative necrosis of the cardiomyocytes themselves is the defining pathological feature that distinguishes irreversible myocardial injury.
*Neutrophilic infiltration*
- **Neutrophilic infiltration** is indeed present at day 2 post-MI (peaks at days 1-3) as part of the acute inflammatory response to clear necrotic debris.
- However, neutrophils represent the **reactive inflammatory response** rather than the primary pathological change in the infarcted cardiomyocytes themselves.
- The question asks about the most characteristic histopathological finding, which is the **coagulative necrosis** of the myocardial cells, not the secondary inflammatory infiltrate.
*Collagenous scar tissue*
- **Collagenous scar tissue** forms much later during the remodeling phase, typically **7 weeks or more** after MI, representing the final stage of healing.
- At day 2, the tissue is still in the acute phase of coagulative necrosis and early inflammation, far too early for mature fibrous scar formation.
*Normal myocardium*
- The patient has sustained an **acute myocardial infarction** with irreversible injury to cardiac tissue.
- Histopathological examination of the infarcted region would show clear abnormalities, not **normal myocardium**.
*Granulation tissue with macrophages*
- **Granulation tissue** with fibroblasts, new capillaries, and macrophages begins forming during the proliferative phase, typically starting around **days 5-7** post-MI.
- At day 2, it is too early for granulation tissue formation; the tissue is still dominated by coagulative necrosis and acute neutrophilic inflammation.
Chemical mediators of inflammation US Medical PG Question 9: A 4-year-old Caucasian boy is brought by his mother to the pediatrician with a red and swollen elbow. He was playing outside a few days prior to presentation when he fell and lightly scraped his elbow on the sidewalk. He was born at 34 weeks' gestation and was in the neonatal ICU for 2 days. His temperature is 102.1°F (38.9°C), blood pressure is 105/65 mmHg, pulse is 110/min, and respirations are 20/min. On exam, he has a swollen, erythematous, fluctuant, and exquisitely tender mass on his right elbow. There is expressible purulence coming from his wound. A peripheral blood smear in this patient would most likely reveal which of the following findings?
- A. Absence of dark blue cytoplasmic staining upon nitroblue tetrazolium administration
- B. Neutrophils with peroxidase-negative granules
- C. Neutrophils with pale cytoplasm without granules
- D. Neutrophils with abundant peroxidase-positive granules (Correct Answer)
- E. Macrocytic erythrocytes and acanthocytes
Chemical mediators of inflammation Explanation: ***Neutrophils with abundant peroxidase-positive granules***
- This patient presents with a **typical acute bacterial skin and soft tissue infection** (abscess) following minor trauma. This is a **normal, age-appropriate scenario** in a healthy child.
- In response to acute bacterial infection, the peripheral blood smear would show **normal, mature neutrophils with abundant peroxidase-positive (myeloperoxidase-positive) granules**. This is the **standard appearance of healthy, functioning neutrophils** responding to infection.
- Additional findings might include **leukocytosis** with a **left shift** (increased band forms), but the neutrophils themselves would have normal morphology with prominent azurophilic (primary) and specific (secondary) granules that stain positive for peroxidase.
- This is the expected finding in any patient with an acute bacterial infection and a normal immune system.
*Absence of dark blue cytoplasmic staining upon nitroblue tetrazolium administration*
- The **nitroblue tetrazolium (NBT) test** is a specialized diagnostic test for **Chronic Granulomatous Disease (CGD)**, where neutrophils cannot produce a respiratory burst due to defective NADPH oxidase.
- However, this patient shows **no clinical evidence of CGD**: this is a **first-time infection** (not recurrent), occurring after **significant environmental exposure** (playing outside, scraping elbow on sidewalk), and the infection is responding as expected to inflammation.
- Additionally, NBT testing is a **functional assay**, not a routine finding on peripheral blood smear examination.
*Neutrophils with peroxidase-negative granules*
- **Myeloperoxidase deficiency** is a rare neutrophil disorder where granules lack myeloperoxidase enzyme.
- There is **no clinical indication** for this diagnosis in a child with a straightforward post-traumatic bacterial infection.
- Most patients with myeloperoxidase deficiency are **asymptomatic** or have only mild infection susceptibility.
*Neutrophils with pale cytoplasm without granules*
- **Hypogranular or agranular neutrophils** are seen in **Chediak-Higashi syndrome** (which includes oculocutaneous albinism and neurologic abnormalities) or **myelodysplastic syndromes**.
- This patient has an **acute infection with normal inflammatory response**, making these conditions extremely unlikely.
- Chediak-Higashi syndrome would present with additional features like partial albinism and easy bruising.
*Macrocytic erythrocytes and acanthocytes*
- **Macrocytic erythrocytes** suggest vitamin B12/folate deficiency, liver disease, or hypothyroidism.
- **Acanthocytes** (spur cells) are associated with severe liver disease, abetalipoproteinemia, or neuroacanthocytosis.
- These red blood cell abnormalities are **completely unrelated** to this patient's presentation of acute bacterial skin infection.
Chemical mediators of inflammation US Medical PG Question 10: A 32-year-old man who recently emigrated from Somalia comes to the physician because of a 4-week history of fever, cough, and chest pain. He has had a 5-kg (11-lb) weight loss over the last 3 months despite no changes in appetite. His temperature is 38.1°C (100.6°F). Physical examination shows enlarged cervical lymph nodes. The lungs are clear to auscultation. The results of an interferon-γ release assay are positive. An x-ray of the chest shows bilateral mediastinal lymphadenopathy. A transbronchial needle aspiration biopsy of a mediastinal lymph node is performed; a photomicrograph of the specimen is shown. The structure indicated by the arrow is most likely comprised of which of the following types of cells?
- A. Natural killer cells
- B. B cells
- C. Fibroblasts
- D. Neutrophils
- E. Macrophages (Correct Answer)
Chemical mediators of inflammation Explanation: ***Macrophages***
- The photomicrograph shows a **granuloma**, characterized by collections of **epithelioid histiocytes** (modified macrophages) and **multinucleated giant cells**, which are essentially fused macrophages.
- This morphology, coupled with the clinical picture of fever, cough, weight loss, positive interferon-γ release assay, and mediastinal lymphadenopathy in a patient from an endemic area, is highly suggestive of **tuberculosis**, a classic granulomatous disease.
*Natural killer cells*
- Natural killer cells are part of the innate immune system and are primarily involved in **killing virally infected cells** and **tumor cells**.
- They are not the primary cellular component forming the characteristic structure of a granuloma.
*B cells*
- B cells are responsible for **antibody production** and antigen presentation.
- While B cells may be present in the periphery of a granuloma, they do not form the core epithelioid and giant cell components.
*Fibroblasts*
- Fibroblasts produce **collagen** and the extracellular matrix, playing a role in **scar formation** and the fibrotic wall that can surround chronic granulomas.
- They do not constitute the primary cellular components of the inflammatory core of a granuloma.
*Neutrophils*
- Neutrophils are typically associated with **acute inflammation** and bacterial infections, characterized by pus formation.
- They are not the predominant cell type in the organized structure of a **granuloma** found in tuberculosis.
More Chemical mediators of inflammation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.