Cellular components of inflammation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cellular components of inflammation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cellular components of inflammation US Medical PG Question 1: A 45-year-old immigrant presents with unintentional weight loss, sleep hyperhidrosis, and a persistent cough. He says these symptoms have been present for quite some time. Upon imaging, many granulomas in the upper lobes are present. It is noted that these apical granulomas have centers of necrosis that appear cheese-like in appearance. Encircling the area of necrosis are large cells with cytoplasms pale in color. Of the following surface markers, which one is most closely associated with these cells?
- A. CD20
- B. CD3
- C. CD4
- D. CD14 (Correct Answer)
- E. CD8
Cellular components of inflammation Explanation: ***CD14***
- The description of **caseating granulomas** in the upper lobes with large cells having pale cytoplasm points towards **tuberculosis** and the presence of **epithelioid macrophages**.
- **CD14** is a surface marker commonly found on **monocytes** and **macrophages**, making it the most appropriate choice among the given options.
- Note: While epithelioid macrophages (the activated form seen in granulomas) may downregulate CD14 compared to circulating monocytes, CD14 remains the most closely associated macrophage marker among these choices. **CD68** would be the ideal marker for tissue macrophages, but it is not listed.
*CD20*
- **CD20** is a surface marker characteristic of **B lymphocytes**.
- While B cells might be present in inflammatory lesions, they are not the predominant cell type described as "large cells with pale cytoplasm" forming the granuloma.
*CD3*
- **CD3** is a pan T-cell marker, indicating the presence of all types of **T lymphocytes**.
- While T cells (specifically CD4+ T helper cells) are crucial in granuloma formation, the "large cells with pale cytoplasm" encasing the necrosis specifically refer to epithelioid macrophages, not T cells.
*CD4*
- **CD4** is a surface marker for **helper T lymphocytes**.
- **CD4+ T cells** play a critical role in orchestrating the immune response and granuloma formation in tuberculosis through IFN-γ secretion, but the description of the large cells with pale cytoplasm refers to macrophages, not lymphocytes.
*CD8*
- **CD8** is a surface marker for **cytotoxic T lymphocytes**.
- **CD8+ T cells** are also involved in the immune response to mycobacterial infection but are not the primary cell type described as forming the bulk of the granuloma's characteristic "large cells with pale cytoplasm."
Cellular components of inflammation US Medical PG Question 2: A 40-day-old child presents to a physician for the first time for a well-child visit. The mother is a 22-year-old college student who opted for a home birth. Upon examination, the child weighs 4.0 kg (8.8 lbs) and has intact reflexes. The umbilical cord is still attached and looks erythematous and indurated. A complete blood cell count reveals leukocytosis. Immunoglobulin levels are normal. A flow cytometry analysis is performed. Which of the following markers will most likely be deficient in this child?
- A. CD1a
- B. CD56
- C. CD3
- D. CD18 (Correct Answer)
- E. CD21
Cellular components of inflammation Explanation: ***CD18***
- The child's presentation with an **erythematous and indurated umbilical cord** that is still attached, along with **leukocytosis**, is highly suggestive of **Leukocyte Adhesion Deficiency Type 1 (LAD-1)**.
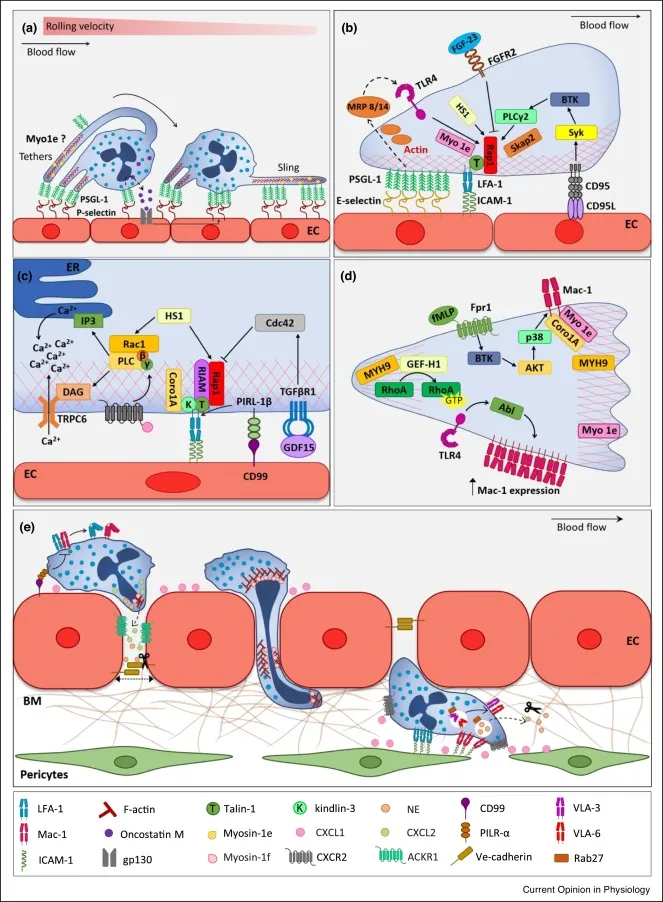
- LAD-1 is caused by a defect in the **integrin beta-2 subunit (CD18)**, which is crucial for leukocyte adhesion and extravasation to sites of infection.
*CD1a*
- **CD1a** is a marker for **Langerhans cells** and immature dendritic cells, which are involved in antigen presentation.
- A deficiency in CD1a is not typically associated with the recurrent bacterial infections and impaired umbilical cord separation seen in this case.
*CD56*
- **CD56** is a marker for **natural killer (NK) cells**, which are important for viral immunity and tumor surveillance.
- While NK cell deficiencies can lead to recurrent infections, the clinical picture here, with delayed umbilical cord detachment and bacterial infection, points more specifically to a defect in neutrophil function.
*CD3*
- **CD3** is a marker for **T lymphocytes**, which are central to cell-mediated immunity.
- Deficiencies in CD3 or T cells typically lead to severe combined immunodeficiency (SCID) with opportunistic infections, which usually present earlier and with more widespread symptoms than described.
*CD21*
- **CD21** (also known as the C3d receptor or CR2) is primarily found on **B lymphocytes** and follicular dendritic cells.
- It plays a role in B cell activation and memory, but a deficiency would not explain the specific constellation of symptoms, particularly the umbilical cord infection and leukocytosis.
Cellular components of inflammation US Medical PG Question 3: A researcher is studying the circulating factors that are released when immune cells are exposed to antigens. Specifically, she is studying a population of CD2+ cells that have been activated acutely. In order to determine which factors are secreted by these cells, she cultures the cells in media and collects the used media from these plates after several days. She then purifies a small factor from this media and uses it to stimulate various immune cell types. She finds that this factor primarily seems to increase the growth and prolong the survival of other CD2+ cells. Which of the following is most likely the factor that was purified by this researcher?
- A. Interleukin-2 (Correct Answer)
- B. Interleukin-3
- C. Interleukin-4
- D. Interleukin-5
- E. Interleukin-1
Cellular components of inflammation Explanation: ***Interleukin-2***
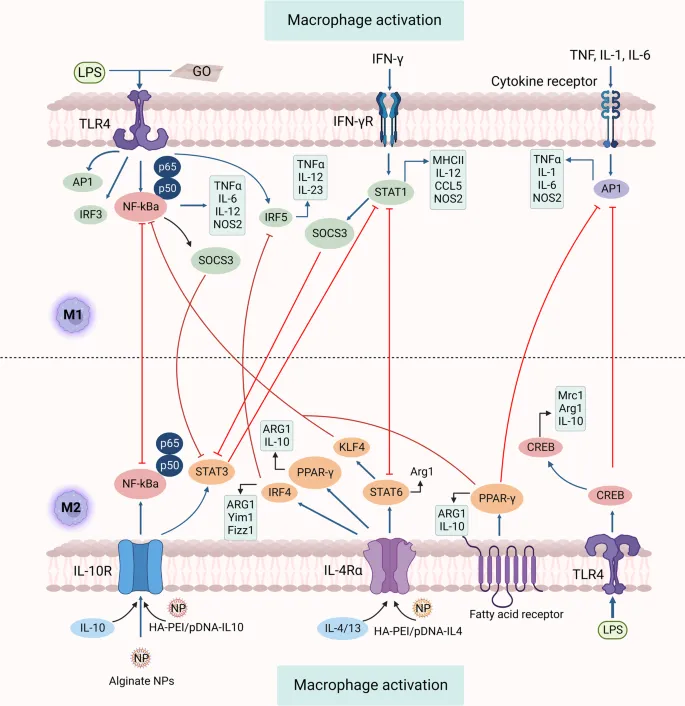
- **Interleukin-2 (IL-2)** is a crucial cytokine for the **growth**, **proliferation**, and **survival** of T lymphocytes, which are CD2+ cells.
- Activated T cells, like the acute CD2+ cells in the scenario, are a primary source of IL-2, and IL-2 acts in an **autocrine** and **paracrine** fashion to stimulate other T cells.
*Interleukin-3*
- **Interleukin-3 (IL-3)** primarily stimulates the growth and differentiation of **hematopoietic stem cells** and progenitors, not specifically mature CD2+ cells.
- It plays a role in the development of various myeloid cell lineages and mast cells, and its main effect is not confined to T cells.
*Interleukin-4*
- **Interleukin-4 (IL-4)** is critical for the differentiation of naive T helper cells into **Th2 cells** and is a key cytokine for **B cell proliferation** and **antibody class switching** to IgE.
- While it has immunomodulatory effects on T cells, its primary role is not in promoting the generalized growth and survival of other CD2+ cells.
*Interleukin-5*
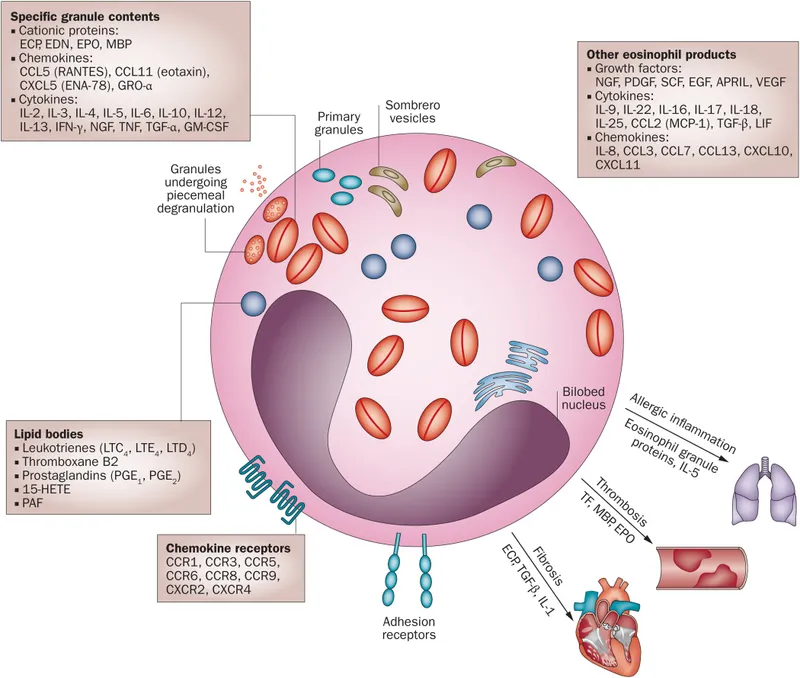
- **Interleukin-5 (IL-5)** is predominantly involved in the growth, differentiation, and activation of **eosinophils**.
- It also plays a role in B cell growth and IgA production, but its effects are not primarily on universal CD2+ cell growth and survival.
*Interleukin-1*
- **Interleukin-1 (IL-1)** is a **pro-inflammatory cytokine** produced by macrophages, monocytes, and other immune cells in response to infection or injury.
- It primarily mediates **acute phase responses**, fever, and activates endothelial cells, but its main function is not to promote the growth and survival of T lymphocytes.
Cellular components of inflammation US Medical PG Question 4: A 25-year-old G1P0 female of Middle Eastern descent gives birth to a male infant at 38 weeks' gestation. The child is in the 15th percentile for both height and weight. Over the course of the first six months of the child's life, he develops multiple severe skin and mucosal infections characterized by dramatically elevated white blood cell counts. The patient also demonstrates mental retardation soon after birth. A thorough hematologic analysis via flow cytometry reveals that the child's neutrophils lack Sialyl-Lewis X. Which of the following processes is likely deficient in this patient?
- A. Chemoattraction
- B. Diapedesis
- C. Transmigration through the extracellular matrix
- D. Rolling (Correct Answer)
- E. Tight adhesion
Cellular components of inflammation Explanation: ***Rolling***
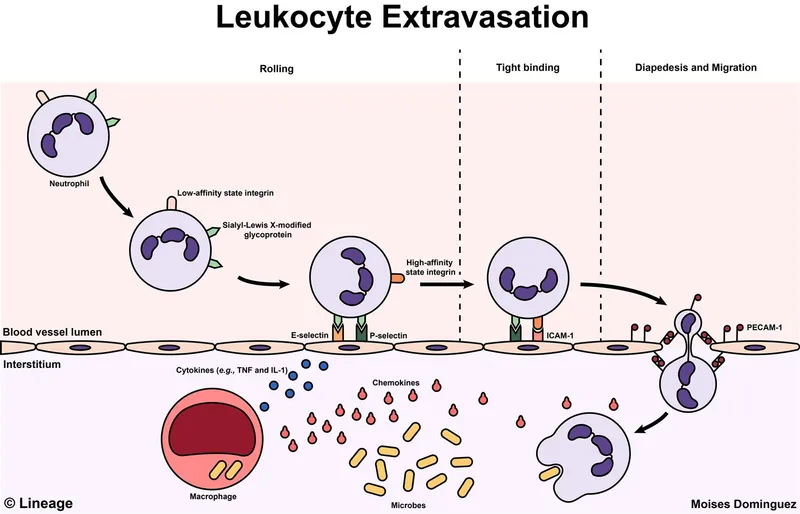
- The absence of **Sialyl-Lewis X** on neutrophils impairs their ability to bind to **P-selectin** and **E-selectin** on endothelial cells, which is crucial for the initial rolling phase of leukocyte extravasation.
- This deficiency is characteristic of **Leukocyte Adhesion Deficiency Type 2 (LAD2)**, also known as **congenital disorder of glycosylation IIc (CDGIIc)**, leading to recurrent infections and developmental delays due to impaired leukocyte trafficking to sites of infection.
*Chemoattraction*
- **Chemoattraction** involves leukocytes moving along a chemical gradient towards inflammatory signals, which occurs after initial rolling and adhesion.
- While essential for reaching the site of infection, the primary defect here is in the initial binding and rolling, rather than the ability to respond to chemokines once bound.
*Diapedesis*
- **Diapedesis**, or transmigration, is the process where leukocytes squeeze between endothelial cells into the tissue.
- This step occurs after stable adhesion, and while it would eventually be inhibited by preceding adhesion defects, it is not the primary process directly affected by the lack of Sialyl-Lewis X.
*Transmigration through the extracellular matrix*
- **Transmigration through the extracellular matrix (ECM)** is the final step where leukocytes move once they are in the tissue, navigating the ECM to reach the infectious agent.
- This process is dependent on successful extravasation and is distinct from the initial adhesion and rolling mechanisms affected by Sialyl-Lewis X deficiency.
*Tight adhesion*
- **Tight adhesion** involves firm binding between leukocyte integrins and endothelial cell adhesion molecules (e.g., ICAM-1) and occurs after rolling.
- Although LAD2 may indirectly affect tight adhesion by preventing sufficient rolling and subsequent integrin activation, the direct defect in Sialyl-Lewis X impacts the initial weak interactions (rolling) rather than the strong, stable adhesive bonds.
Cellular components of inflammation US Medical PG Question 5: A 30-year-old man is admitted to the hospital with a presumed pneumonia and started on antibiotics. Two days later, the patient shows no improvement. Blood cultures reveal yeast with pseudophyphae. Which of the following cell types is most likely deficient or dysfunctional in this patient?
- A. Eosinophils
- B. Macrophages
- C. Neutrophils (Correct Answer)
- D. T-cells
- E. B-cells
Cellular components of inflammation Explanation: ***Neutrophils***
- The presence of **yeast with pseudohyphae** in blood cultures, particularly *Candida*, indicates a fungal infection.
- **Neutrophils** are crucial for the host defense against *Candida* and other fungal pathogens, so their deficiency or dysfunction would predispose to candidemia.
- Neutropenia or neutrophil dysfunction (e.g., chronic granulomatous disease) significantly increases risk of invasive candidiasis.
*Eosinophils*
- **Eosinophils** are primarily involved in defense against **parasitic infections** and in allergic reactions.
- They play a minimal role in the immune response to systemic fungal infections like candidemia.
*Macrophages*
- **Macrophages** are phagocytic cells that contribute to antifungal immunity, particularly in tissue surveillance and chronic infection control.
- However, **neutrophils** are the primary and most critical defense against acute *Candida* bloodstream infections.
- Macrophage deficiency alone does not typically predispose to candidemia as severely as neutrophil deficiency.
*T-cells*
- **T-cells** are important for cell-mediated immunity, particularly against **intracellular pathogens** and viral infections.
- While they play a role in modulating antifungal responses, their deficiency typically leads to infections with *Pneumocystis jirovecii* or severe mucocutaneous candidiasis, rather than disseminated candidemia.
*B-cells*
- **B-cells** are responsible for **humoral immunity** through antibody production, which is primarily effective against extracellular bacteria and toxins.
- They are not the primary line of defense against fungal infections such as candidemia.
Cellular components of inflammation US Medical PG Question 6: Two days after being admitted for acute myocardial infarction, a 61-year-old man has sharp, substernal chest pain that worsens with inspiration and improves when leaning forward. Cardiac examination shows a scratchy sound best heard over the left sternal border. Histopathological examination of the infarcted myocardial tissue is most likely to show which of the following findings?
- A. Neutrophilic infiltration
- B. Collagenous scar tissue
- C. Normal myocardium
- D. Coagulative necrosis (Correct Answer)
- E. Granulation tissue with macrophages
Cellular components of inflammation Explanation: ***Coagulative necrosis***
- The patient's clinical presentation (sharp, substernal chest pain, worsening with inspiration, improving while leaning forward, and a scratchy pericardial friction rub) indicates **post-MI fibrinous pericarditis**, a common complication occurring 2-4 days after myocardial infarction.
- At **day 2 post-MI**, the infarcted myocardium demonstrates **coagulative necrosis** as the primary and most characteristic histopathological finding, representing irreversible ischemic cell death with preserved tissue architecture.
- While neutrophilic infiltration is also present at this timepoint, coagulative necrosis of the cardiomyocytes themselves is the defining pathological feature that distinguishes irreversible myocardial injury.
*Neutrophilic infiltration*
- **Neutrophilic infiltration** is indeed present at day 2 post-MI (peaks at days 1-3) as part of the acute inflammatory response to clear necrotic debris.
- However, neutrophils represent the **reactive inflammatory response** rather than the primary pathological change in the infarcted cardiomyocytes themselves.
- The question asks about the most characteristic histopathological finding, which is the **coagulative necrosis** of the myocardial cells, not the secondary inflammatory infiltrate.
*Collagenous scar tissue*
- **Collagenous scar tissue** forms much later during the remodeling phase, typically **7 weeks or more** after MI, representing the final stage of healing.
- At day 2, the tissue is still in the acute phase of coagulative necrosis and early inflammation, far too early for mature fibrous scar formation.
*Normal myocardium*
- The patient has sustained an **acute myocardial infarction** with irreversible injury to cardiac tissue.
- Histopathological examination of the infarcted region would show clear abnormalities, not **normal myocardium**.
*Granulation tissue with macrophages*
- **Granulation tissue** with fibroblasts, new capillaries, and macrophages begins forming during the proliferative phase, typically starting around **days 5-7** post-MI.
- At day 2, it is too early for granulation tissue formation; the tissue is still dominated by coagulative necrosis and acute neutrophilic inflammation.
Cellular components of inflammation US Medical PG Question 7: A 37-year-old man presents to his primary care physician because he has had constipation for the last several weeks. He has also been feeling lethargic and complains that this winter has been particularly cold. He also complains that he has been gaining weight despite no change in his normal activities. He reveals that two months prior to presentation he had what felt like the flu for which he took Tylenol and did not seek medical attention. Several days after this he developed anterior neck pain. Which of the following findings would most likely be seen on biopsy of this patient's abnormality?
- A. Focal hyperplasia
- B. Germinal follicles
- C. Scalloped clear areas
- D. Fibrous tissue
- E. Granulomatous inflammation (Correct Answer)
Cellular components of inflammation Explanation: ***Granulomatous inflammation***
- The patient's presentation with **constipation**, **lethargy**, **cold intolerance**, and **weight gain** after a flu-like illness followed by **anterior neck pain** is highly suggestive of **subacute granulomatous thyroiditis (de Quervain thyroiditis)**.
- A biopsy of the thyroid in cases of de Quervain thyroiditis typically reveals **granulomatous inflammation** with scattered **giant cells** and lymphocytes, reflecting the destructive inflammatory process.
*Focal hyperplasia*
- **Focal hyperplasia** is characterized by an increase in the number of thyroid follicular cells and is seen in conditions like **Graves' disease** or **multinodular goiter**, particularly when the gland is overstimulated.
- This finding would not be expected in subacute granulomatous thyroiditis, where the primary pathology is destruction rather than proliferation.
*Germinal follicles*
- **Germinal follicles** are characteristic of chronic lymphocytic thyroiditis (**Hashimoto's thyroiditis**), an autoimmune condition where the thyroid gland is infiltrated by lymphocytes, plasma cells, and macrophages.
- While Hashimoto's can cause hypothyroidism, the preceding flu-like illness and acute neck pain make de Quervain thyroiditis a more likely diagnosis.
*Scalloped clear areas*
- **Scalloped clear areas** at the colloid-epithelial interface, also known as **colloid resorption vacuoles**, are a histological feature of **hyperactive thyroid follicles**, typically seen in conditions causing hyperthyroidism like **Graves' disease**.
- The patient's symptoms of lethargy, cold intolerance, and weight gain indicate hypothyroidism, which can follow the initial hyperthyroid phase of de Quervain thyroiditis but are not indicative of active hyperfunction on biopsy at this stage.
*Fibrous tissue*
- An increased amount of **fibrous tissue** is characteristic of **Riedel's thyroiditis**, a rare condition characterized by dense fibrosis that replaces normal thyroid parenchyma and can extend into surrounding neck structures.
- This patient's presentation with a preceding febrile illness and neck pain is not typical for Riedel's thyroiditis, which usually presents as a hard, fixed mass without an antecedent viral infection.
Cellular components of inflammation US Medical PG Question 8: A 4-year-old Caucasian boy is brought by his mother to the pediatrician with a red and swollen elbow. He was playing outside a few days prior to presentation when he fell and lightly scraped his elbow on the sidewalk. He was born at 34 weeks' gestation and was in the neonatal ICU for 2 days. His temperature is 102.1°F (38.9°C), blood pressure is 105/65 mmHg, pulse is 110/min, and respirations are 20/min. On exam, he has a swollen, erythematous, fluctuant, and exquisitely tender mass on his right elbow. There is expressible purulence coming from his wound. A peripheral blood smear in this patient would most likely reveal which of the following findings?
- A. Absence of dark blue cytoplasmic staining upon nitroblue tetrazolium administration
- B. Neutrophils with peroxidase-negative granules
- C. Neutrophils with pale cytoplasm without granules
- D. Neutrophils with abundant peroxidase-positive granules (Correct Answer)
- E. Macrocytic erythrocytes and acanthocytes
Cellular components of inflammation Explanation: ***Neutrophils with abundant peroxidase-positive granules***
- This patient presents with a **typical acute bacterial skin and soft tissue infection** (abscess) following minor trauma. This is a **normal, age-appropriate scenario** in a healthy child.
- In response to acute bacterial infection, the peripheral blood smear would show **normal, mature neutrophils with abundant peroxidase-positive (myeloperoxidase-positive) granules**. This is the **standard appearance of healthy, functioning neutrophils** responding to infection.
- Additional findings might include **leukocytosis** with a **left shift** (increased band forms), but the neutrophils themselves would have normal morphology with prominent azurophilic (primary) and specific (secondary) granules that stain positive for peroxidase.
- This is the expected finding in any patient with an acute bacterial infection and a normal immune system.
*Absence of dark blue cytoplasmic staining upon nitroblue tetrazolium administration*
- The **nitroblue tetrazolium (NBT) test** is a specialized diagnostic test for **Chronic Granulomatous Disease (CGD)**, where neutrophils cannot produce a respiratory burst due to defective NADPH oxidase.
- However, this patient shows **no clinical evidence of CGD**: this is a **first-time infection** (not recurrent), occurring after **significant environmental exposure** (playing outside, scraping elbow on sidewalk), and the infection is responding as expected to inflammation.
- Additionally, NBT testing is a **functional assay**, not a routine finding on peripheral blood smear examination.
*Neutrophils with peroxidase-negative granules*
- **Myeloperoxidase deficiency** is a rare neutrophil disorder where granules lack myeloperoxidase enzyme.
- There is **no clinical indication** for this diagnosis in a child with a straightforward post-traumatic bacterial infection.
- Most patients with myeloperoxidase deficiency are **asymptomatic** or have only mild infection susceptibility.
*Neutrophils with pale cytoplasm without granules*
- **Hypogranular or agranular neutrophils** are seen in **Chediak-Higashi syndrome** (which includes oculocutaneous albinism and neurologic abnormalities) or **myelodysplastic syndromes**.
- This patient has an **acute infection with normal inflammatory response**, making these conditions extremely unlikely.
- Chediak-Higashi syndrome would present with additional features like partial albinism and easy bruising.
*Macrocytic erythrocytes and acanthocytes*
- **Macrocytic erythrocytes** suggest vitamin B12/folate deficiency, liver disease, or hypothyroidism.
- **Acanthocytes** (spur cells) are associated with severe liver disease, abetalipoproteinemia, or neuroacanthocytosis.
- These red blood cell abnormalities are **completely unrelated** to this patient's presentation of acute bacterial skin infection.
Cellular components of inflammation US Medical PG Question 9: A 32-year-old man who recently emigrated from Somalia comes to the physician because of a 4-week history of fever, cough, and chest pain. He has had a 5-kg (11-lb) weight loss over the last 3 months despite no changes in appetite. His temperature is 38.1°C (100.6°F). Physical examination shows enlarged cervical lymph nodes. The lungs are clear to auscultation. The results of an interferon-γ release assay are positive. An x-ray of the chest shows bilateral mediastinal lymphadenopathy. A transbronchial needle aspiration biopsy of a mediastinal lymph node is performed; a photomicrograph of the specimen is shown. The structure indicated by the arrow is most likely comprised of which of the following types of cells?
- A. Natural killer cells
- B. B cells
- C. Fibroblasts
- D. Neutrophils
- E. Macrophages (Correct Answer)
Cellular components of inflammation Explanation: ***Macrophages***
- The photomicrograph shows a **granuloma**, characterized by collections of **epithelioid histiocytes** (modified macrophages) and **multinucleated giant cells**, which are essentially fused macrophages.
- This morphology, coupled with the clinical picture of fever, cough, weight loss, positive interferon-γ release assay, and mediastinal lymphadenopathy in a patient from an endemic area, is highly suggestive of **tuberculosis**, a classic granulomatous disease.
*Natural killer cells*
- Natural killer cells are part of the innate immune system and are primarily involved in **killing virally infected cells** and **tumor cells**.
- They are not the primary cellular component forming the characteristic structure of a granuloma.
*B cells*
- B cells are responsible for **antibody production** and antigen presentation.
- While B cells may be present in the periphery of a granuloma, they do not form the core epithelioid and giant cell components.
*Fibroblasts*
- Fibroblasts produce **collagen** and the extracellular matrix, playing a role in **scar formation** and the fibrotic wall that can surround chronic granulomas.
- They do not constitute the primary cellular components of the inflammatory core of a granuloma.
*Neutrophils*
- Neutrophils are typically associated with **acute inflammation** and bacterial infections, characterized by pus formation.
- They are not the predominant cell type in the organized structure of a **granuloma** found in tuberculosis.
Cellular components of inflammation US Medical PG Question 10: A 60-year-old man comes to the office because of an 8-month history of cough, night sweats, shortness of breath, and fatigue. He has also had a 9-kg (19.8-lb) weight loss during this time. He appears pale. Abdominal examination shows hepatosplenomegaly. His leukocyte count is 80,000/mm3 and his leukocyte alkaline phosphatase level is increased. A peripheral blood smear shows > 82% neutrophils with band forms and immature and mature neutrophil precursors. An x-ray of the chest shows a 9-mm right hilar nodule. Which of the following is the most likely cause of this patient's laboratory findings?
- A. Sarcoidosis
- B. Acute lymphoblastic leukemia
- C. Leukemoid reaction (Correct Answer)
- D. Tuberculosis
- E. Chronic myeloid leukemia
Cellular components of inflammation Explanation: ***Leukemoid reaction***
- The combination of **leukocytosis** (>50,000/mm³), **immature granulocytes**, and **elevated leukocyte alkaline phosphatase (LAP) score** in the presence of an underlying inflammatory or infectious process (such as the suspected lung lesion) strongly suggests a leukemoid reaction.
- A leukemoid reaction is a reactive **increase in white blood cells**, often in response to severe infection or malignancy, mimicking leukemia but distinct from it due to the high LAP score and lack of specific chromosomal translocations.
*Sarcoidosis*
- Sarcoidosis typically presents with **non-caseating granulomas**, often affecting the lungs and lymph nodes, but does not usually cause such a profound leukocytosis with immature forms.
- While a **hilar nodule** can be seen, the described hematological findings, especially the high LAP score and pronounced neutrophilia, are not characteristic of sarcoidosis.
*Acute lymphoblastic leukemia*
- This condition involves a proliferation of **lymphoblasts**, not mature or immature neutrophils; therefore, the peripheral smear would show a predominance of blasts and not mature neutrophil precursors.
- While it can cause leukocytosis, the specific cell types and the **elevated LAP score** (LAP is typically low in ALL) rule it out.
*Tuberculosis*
- Tuberculosis can cause fever, night sweats, weight loss, and lung findings, but it typically does not lead to a **leukocyte count of 80,000/mm³** with such a high proportion of immature neutrophils.
- While it can cause a **leukemoid reaction**, the LAP score and specific granulocyte morphology help differentiate it from other causes, and the primary diagnosis here is the reaction itself, which would be *caused* by something like TB.
*Chronic myeloid leukemia*
- CML also presents with marked leukocytosis and **immature myeloid cells** but is characterized by a **low leukocyte alkaline phosphatase (LAP) score** and the presence of the **Philadelphia chromosome (BCR-ABL1 fusion gene)**, which contradicts the elevated LAP score found in this patient.
- While hepatosplenomegaly and constitutional symptoms align, the LAP score is a key differentiating factor.
More Cellular components of inflammation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.