Acute inflammation mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute inflammation mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute inflammation mechanisms US Medical PG Question 1: A 24-year-old woman comes to the physician because of progressively worsening episodes of severe, crampy abdominal pain and nonbloody diarrhea for the past 3 years. Examination of the abdomen shows mild distension and generalized tenderness. There is a fistula draining stool in the perianal region. Immunohistochemistry shows dysfunction of the nucleotide oligomerization binding domain 2 (NOD2) protein. This dysfunction most likely causes overactivity of which of the following immunological proteins in this patient?
- A. Interferon-γ
- B. β-catenin
- C. IL-1β
- D. IL-10
- E. NF-κB (Correct Answer)
Acute inflammation mechanisms Explanation: ***NF-κB***
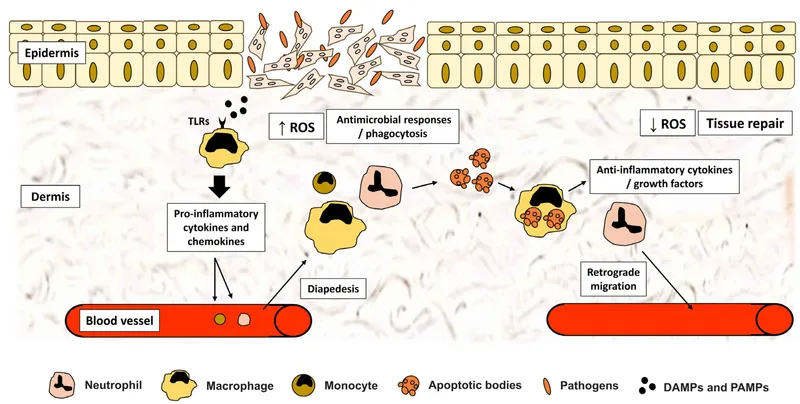
- **NOD2** is a pattern recognition receptor that normally detects bacterial products and regulates inflammatory responses. In **Crohn's disease**, loss-of-function **NOD2 mutations** lead to impaired bacterial sensing and clearance.
- This defective NOD2 function results in **compensatory overactivation of NF-κB** through alternative inflammatory pathways (particularly TLR signaling), causing excessive **pro-inflammatory cytokine** production.
- This **NF-κB hyperactivation** is a key driver of chronic inflammation in **Crohn's disease**, contributing to symptoms like fistulas, strictures, and transmural inflammation.
*Interferon-γ*
- **Interferon-γ** is an important pro-inflammatory cytokine in Crohn's disease and is part of the Th1-mediated immune response.
- However, its production is downstream of **NF-κB** activation and other inflammatory cascades. **NOD2 dysfunction** does not directly cause **IFN-γ** overactivity through the primary molecular pathway.
*β-catenin*
- **β-catenin** is a key component of the **Wnt signaling pathway** involved in cell adhesion, proliferation, and differentiation.
- It is not directly affected by **NOD2 dysfunction**. Dysregulation of **β-catenin** is more commonly associated with colorectal adenomas and cancer, not the inflammatory mechanisms of Crohn's disease.
*IL-1β*
- **IL-1β** is a potent pro-inflammatory cytokine that is indeed elevated in **Crohn's disease**.
- However, **IL-1β** is produced **downstream** of **NF-κB** activation. The primary molecular consequence of **NOD2 dysfunction** is the overactivity of **NF-κB**, which then drives production of various cytokines including **IL-1β**.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** essential for maintaining intestinal immune homeostasis and suppressing excessive inflammatory responses.
- In Crohn's disease, **IL-10** signaling is often **impaired or deficient** rather than overactive. The question asks about overactivity, making this the opposite of what occurs in the disease.
Acute inflammation mechanisms US Medical PG Question 2: An 18-year-old woman presents to the emergency department with a complaint of severe abdominal pain for the past 6 hours. She is anorexic and nauseous and has vomited twice since last night. She also states that her pain initially began in the epigastric region, then migrated to the right iliac fossa. Her vital signs include a respiratory rate of 14/min, blood pressure of 130/90 mm Hg, pulse of 110/min, and temperature of 38.5°C (101.3°F). On abdominal examination, there is superficial tenderness in her right iliac fossa, rebound tenderness, rigidity, and abdominal guarding. A complete blood count shows neutrophilic leukocytosis and a shift to the left. Laparoscopic surgery is performed and the inflamed appendix, which is partly covered by a yellow exudate, is excised. Microscopic examination of the appendix demonstrates a neutrophil infiltrate of the mucosal and muscular layers with extension into the lumen. Which of the following chemical mediators is responsible for pain in this patient?
- A. IgG and complement C3b
- B. Bradykinin and prostaglandin (Correct Answer)
- C. 5- hydroperoxyeicosatetraenoic acid (5-HPETE) and leukotriene A4
- D. Serotonin and histamine
- E. Tumor necrosis factor and interleukin-1
Acute inflammation mechanisms Explanation: ***Bradykinin and prostaglandin***
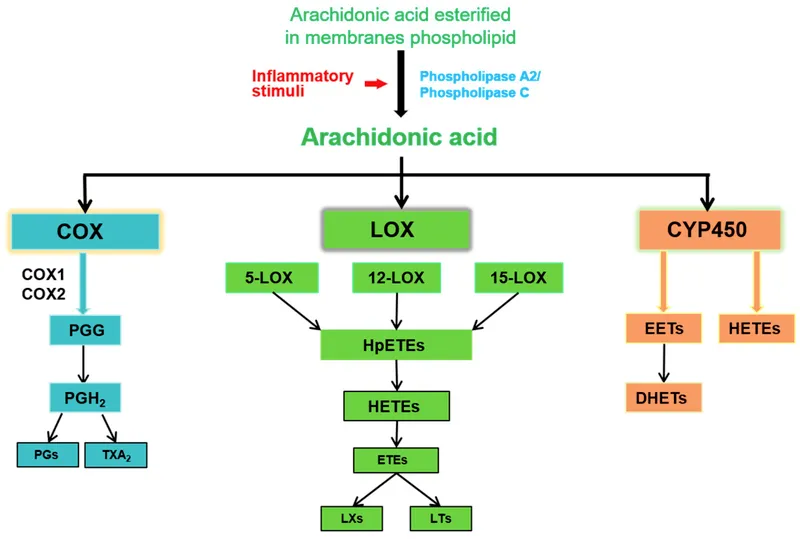
- **Bradykinin** and **prostaglandins** are key inflammatory mediators that directly stimulate **nociceptors**, leading to the sensation of pain. Prostaglandins are also responsible for inducing fever.
- The patient's symptoms, including **severe abdominal pain**, fever, and local tenderness, are consistent with acute inflammation (appendicitis), where these mediators play a central role.
*IgG and complement C3b*
- **IgG** is an antibody involved in the adaptive immune response, primarily responsible for pathogen neutralization and opsonization.
- **Complement C3b** is a component of the complement system involved in opsonization and forming the membrane attack complex, but neither directly mediates pain.
*5- hydroperoxyeicosatetraenoic acid (5-HPETE) and leukotriene A4*
- **5-HPETE** is an unstable intermediate in the lipoxygenase pathway, leading to the formation of leukotrienes.
- **Leukotriene A4** is a precursor to other leukotrienes (e.g., LTB4, LTC4, LTD4) that are potent **chemotactic agents** and **bronchoconstrictors**, but they are not primary pain mediators.
*Serotonin and histamine*
- **Serotonin** is primarily involved in smooth muscle contraction, vasoconstriction, and neurotransmission; while it can modulate pain, it is not a direct primary mediator in acute appendicitis.
- **Histamine** is released by mast cells and basophils, causing vasodilation and increased vascular permeability (contributing to edema), but its role in direct pain mediation in this context is less significant than bradykinin or prostaglandins.
*Tumor necrosis factor and interleukin-1*
- **Tumor necrosis factor (TNF)** and **interleukin-1 (IL-1)** are **pro-inflammatory cytokines** that are crucial in initiating and amplifying the inflammatory response.
- While they contribute to fever and systemic symptoms of inflammation, their primary role is in cell signaling and immune cell activation rather than direct pain sensation.
Acute inflammation mechanisms US Medical PG Question 3: A 24-year-old woman presents to the emergency department because she started experiencing dyspnea and urticaria after dinner. Her symptoms began approximately 15 minutes after eating a new type of shellfish that she has never had before. On physical exam her breathing is labored, and pulmonary auscultation reveals wheezing bilaterally. Given this presentation, she is immediately started on intramuscular epinephrine for treatment of her symptoms. If part of this patient's symptoms were related to the systemic release of certain complement components, which of the following is another function of the responsible component?
- A. Chemotaxis (Correct Answer)
- B. Direct cytolysis
- C. Inhibition of kallikrein activation
- D. Clearance of immune complexes
- E. Opsonization of pathogens
Acute inflammation mechanisms Explanation: **Chemotaxis**
- The patient's symptoms are consistent with **anaphylaxis**, an IgE-mediated hypersensitivity reaction that causes mast cell degranulation.
- During anaphylaxis, mast cells release mediators that can activate the **complement system**, producing anaphylatoxins like C3a and C5a. **C5a** is a potent **chemotactic factor** for neutrophils and macrophages, attracting them to the site of inflammation.
*Direct cytolysis*
- **Direct cytolysis** is primarily mediated by the **membrane attack complex (MAC)**, formed by C5b-C9.
- While complement activation occurs in anaphylaxis, the immediate severe symptoms like urticaria and bronchospasm are predominantly due to mast cell degranulation and the release of histamine and other mediators, not direct cell lysis by MAC which occurs in later stages or different contexts.
*Inhibition of kallikrein activation*
- **Kallikrein activation** is inhibited by **C1 esterase inhibitor (C1-INH)**.
- A deficiency in C1-INH leads to conditions like **hereditary angioedema**, which is distinct from the type I hypersensitivity reaction (anaphylaxis) described in the patient.
*Clearance of immune complexes*
- **Clearance of immune complexes** is a function primarily associated with **C3b** binding to immune complexes, allowing their uptake by phagocytes or transport to the liver and spleen.
- While immune complexes are involved in other types of hypersensitivity reactions, they are not the primary mechanism or a direct complement component involved in the acute allergic reaction due to shellfish.
*Opsonization of pathogens*
- **Opsonization** is the process by which pathogens are tagged for phagocytosis, chiefly performed by **C3b** and antibodies.
- While complement plays a role in host defense, opsonization is not the function of the complement components (C3a, C5a) primarily responsible for the anaphylactoid reactions seen in this patient's presentation.
Acute inflammation mechanisms US Medical PG Question 4: A 4-year-old Caucasian boy is brought by his mother to the pediatrician with a red and swollen elbow. He was playing outside a few days prior to presentation when he fell and lightly scraped his elbow on the sidewalk. He was born at 34 weeks' gestation and was in the neonatal ICU for 2 days. His temperature is 102.1°F (38.9°C), blood pressure is 105/65 mmHg, pulse is 110/min, and respirations are 20/min. On exam, he has a swollen, erythematous, fluctuant, and exquisitely tender mass on his right elbow. There is expressible purulence coming from his wound. A peripheral blood smear in this patient would most likely reveal which of the following findings?
- A. Absence of dark blue cytoplasmic staining upon nitroblue tetrazolium administration
- B. Neutrophils with peroxidase-negative granules
- C. Neutrophils with pale cytoplasm without granules
- D. Neutrophils with abundant peroxidase-positive granules (Correct Answer)
- E. Macrocytic erythrocytes and acanthocytes
Acute inflammation mechanisms Explanation: ***Neutrophils with abundant peroxidase-positive granules***
- This patient presents with a **typical acute bacterial skin and soft tissue infection** (abscess) following minor trauma. This is a **normal, age-appropriate scenario** in a healthy child.
- In response to acute bacterial infection, the peripheral blood smear would show **normal, mature neutrophils with abundant peroxidase-positive (myeloperoxidase-positive) granules**. This is the **standard appearance of healthy, functioning neutrophils** responding to infection.
- Additional findings might include **leukocytosis** with a **left shift** (increased band forms), but the neutrophils themselves would have normal morphology with prominent azurophilic (primary) and specific (secondary) granules that stain positive for peroxidase.
- This is the expected finding in any patient with an acute bacterial infection and a normal immune system.
*Absence of dark blue cytoplasmic staining upon nitroblue tetrazolium administration*
- The **nitroblue tetrazolium (NBT) test** is a specialized diagnostic test for **Chronic Granulomatous Disease (CGD)**, where neutrophils cannot produce a respiratory burst due to defective NADPH oxidase.
- However, this patient shows **no clinical evidence of CGD**: this is a **first-time infection** (not recurrent), occurring after **significant environmental exposure** (playing outside, scraping elbow on sidewalk), and the infection is responding as expected to inflammation.
- Additionally, NBT testing is a **functional assay**, not a routine finding on peripheral blood smear examination.
*Neutrophils with peroxidase-negative granules*
- **Myeloperoxidase deficiency** is a rare neutrophil disorder where granules lack myeloperoxidase enzyme.
- There is **no clinical indication** for this diagnosis in a child with a straightforward post-traumatic bacterial infection.
- Most patients with myeloperoxidase deficiency are **asymptomatic** or have only mild infection susceptibility.
*Neutrophils with pale cytoplasm without granules*
- **Hypogranular or agranular neutrophils** are seen in **Chediak-Higashi syndrome** (which includes oculocutaneous albinism and neurologic abnormalities) or **myelodysplastic syndromes**.
- This patient has an **acute infection with normal inflammatory response**, making these conditions extremely unlikely.
- Chediak-Higashi syndrome would present with additional features like partial albinism and easy bruising.
*Macrocytic erythrocytes and acanthocytes*
- **Macrocytic erythrocytes** suggest vitamin B12/folate deficiency, liver disease, or hypothyroidism.
- **Acanthocytes** (spur cells) are associated with severe liver disease, abetalipoproteinemia, or neuroacanthocytosis.
- These red blood cell abnormalities are **completely unrelated** to this patient's presentation of acute bacterial skin infection.
Acute inflammation mechanisms US Medical PG Question 5: A 32-year-old female with Crohn's disease diagnosed in her early 20s comes to your office for a follow-up appointment. She is complaining of headaches and fatigue. Which of the following arterial blood gas findings might you expect?
- A. High PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)
- B. Low PaO2, low O2 saturation (SaO2), low O2 content (CaO2)
- C. Normal PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)
- D. Normal PaO2, normal O2 saturation (SaO2), low O2 content (CaO2) (Correct Answer)
- E. Low PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)
Acute inflammation mechanisms Explanation: ***Normal PaO2, normal O2 saturation (SaO2), low O2 content (CaO2)***
- Patients with **Crohn's disease** are prone to developing **iron deficiency anemia** due to chronic inflammation, malabsorption, and blood loss, leading to reduced hemoglobin levels.
- While PaO2 and SaO2 measure oxygen *tension* and *percentage saturation* of available hemoglobin, respectively, **O2 content (CaO2)** directly reflects the *total amount* of oxygen delivered to tissues, which is primarily dependent on hemoglobin concentration. Therefore, with anemia, CaO2 will be low despite normal PaO2 and SaO2 because there is less hemoglobin to carry oxygen.
*High PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)*
- High PaO2 would indicate **hyperoxygenation**, which is not an expected complication of Crohn's disease or its associated anemia.
- Normal O2 content is inconsistent with the presence of anemia, which significantly reduces the body's total oxygen-carrying capacity.
*Low PaO2, low O2 saturation (SaO2), low O2 content (CaO2)*
- Low PaO2 and SaO2 suggest a primary **respiratory problem** or severe hypoxemia, which is not directly linked to Crohn's disease or the typical presentation of iron deficiency anemia.
- While low O2 content is correct for anemia, the accompanying low PaO2 and SaO2 indicate a different underlying pathology for oxygen transport issues.
*Normal PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)*
- This finding would indicate **normal oxygenation** and oxygen-carrying capacity, which is contrary to the clinical scenario of a patient with Crohn's likely complicated by anemia.
- The patient's symptoms of headaches and fatigue are consistent with poor tissue oxygenation, which would not occur if all these parameters were normal.
*Low PaO2, normal O2 saturation (SaO2), normal O2 content (CaO2)*
- A low PaO2 with a normal SaO2 is physiologically unlikely unless there is a **left shift of the oxygen dissociation curve** with adequate hemoglobin, which doesn't fit the expected anemic state.
- Normal O2 content would rule out the presence of anemia as a cause for the symptoms, which is a common complication in Crohn's disease.
Acute inflammation mechanisms US Medical PG Question 6: A 2-year-old boy has a history of recurrent bacterial infections, especially of his skin. When he has an infection, pus does not form. His mother reports that, when he was born, his umbilical cord took 5 weeks to detach. He is ultimately diagnosed with a defect in a molecule in the pathway that results in neutrophil extravasation. Which of the following correctly pairs the defective molecule with the step of extravasation that molecule affects?
- A. E-selectin; transmigration
- B. LFA-1 (integrin); tight adhesion (Correct Answer)
- C. ICAM-1; margination
- D. E-selectin; tight adhesion
- E. PECAM-1; transmigration
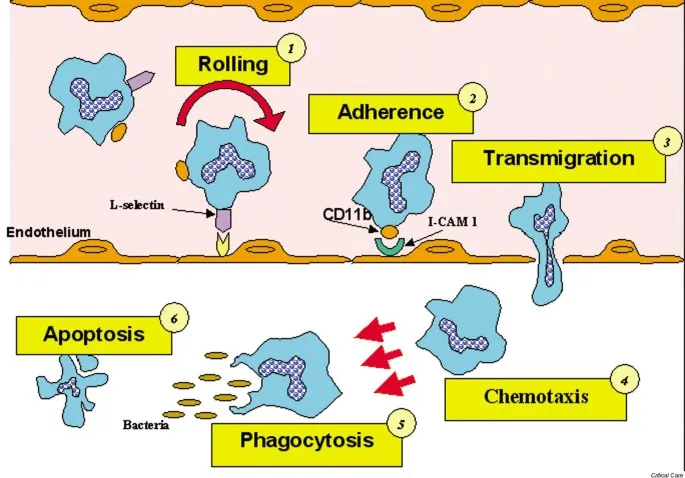
Acute inflammation mechanisms Explanation: ***LFA-1 (integrin); tight adhesion***
- This patient's symptoms (recurrent bacterial infections, lack of pus formation, and delayed umbilical cord separation) are classic for **Leukocyte Adhesion Deficiency type 1 (LAD-1)**.
- **LAD-1** is caused by a defect in the **CD18 subunit** of **β2 integrins**, including **LFA-1** and **Mac-1**, which are crucial for the **tight adhesion** of neutrophils to endothelial cells.
*E-selectin; transmigration*
- **E-selectin** mediates the initial **rolling** of leukocytes along the endothelial surface, not transmigration.
- A defect in E-selectin would impair rolling, but the primary defect in LAD-1 is in tight adhesion.
*ICAM-1; margination*
- **ICAM-1** (Intercellular Adhesion Molecule-1) is an endothelial ligand that binds to integrins on leukocytes, facilitating **tight adhesion** and transmigration, not margination.
- **Margination** refers to the movement of leukocytes to the periphery of the blood vessel lumen.
*E-selectin; tight adhesion*
- **E-selectin** is involved in the initial **rolling** phase of extravasation by binding to sialyl Lewis X on leukocytes.
- It does not primarily mediate **tight adhesion**, which is facilitated by integrins binding to ICAM-1.
*PECAM-1; transmigration*
- **PECAM-1** (Platelet Endothelial Cell Adhesion Molecule-1) is primarily involved in **transmigration** (diapedesis), where leukocytes pass between endothelial cells.
- While important for extravasation, the characteristic findings of LAD-1 point to a defect earlier in the pathway, specifically tight adhesion.
Acute inflammation mechanisms US Medical PG Question 7: Researchers are investigating the mechanism of cell apoptosis and host defense in mice. They have observed that mice with certain gene deletions are not able to fight the induced viral infection. They identify a cell that is able to destroy target cells infected with viruses by exocytosis of granule contents, which induces the activation of caspases. Which type of cell is responsible for this process?
- A. CD8+ lymphocytes (Correct Answer)
- B. CD4+ lymphocytes
- C. Macrophages
- D. Neutrophils
- E. Eosinophils
Acute inflammation mechanisms Explanation: ***CD8+ lymphocytes***
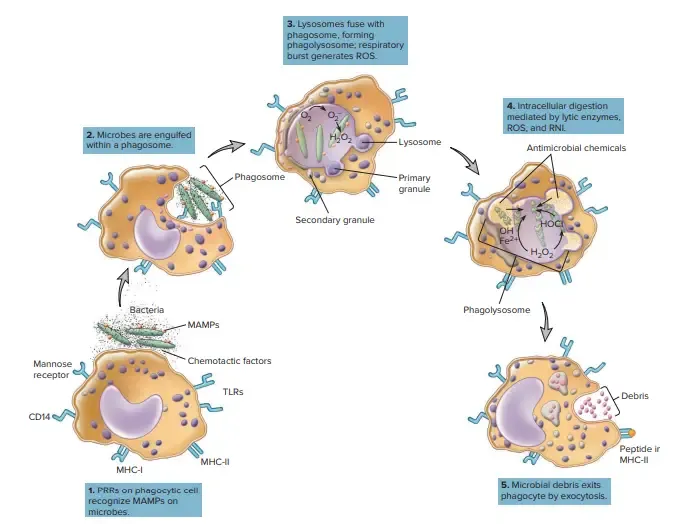
- **CD8+ lymphocytes**, or **cytotoxic T lymphocytes (CTLs)**, are specialized to recognize and kill **virus-infected cells** and cancer cells.
- They achieve this by releasing cytotoxic granules containing **perforin** and **granzymes**, which enter the target cell and activate **caspases**, leading to **apoptosis**.
- Note: **Natural killer (NK) cells** also use a similar granule-mediated mechanism, but CD8+ T cells provide **antigen-specific** recognition via MHC class I.
*CD4+ lymphocytes*
- **CD4+ lymphocytes**, or **helper T cells**, primarily coordinate immune responses by secreting **cytokines** and activating other immune cells, rather than directly killing infected cells.
- They are crucial for both humoral and cell-mediated immunity but do not typically induce apoptosis via granule exocytosis.
*Macrophages*
- **Macrophages** are phagocytic cells that engulf and digest pathogens, cellular debris, and foreign substances.
- While they can present antigens and participate in immune responses, their primary role in antiviral defense is **phagocytosing infected cells** and presenting antigens, not inducing apoptosis via granule exocytosis.
*Neutrophils*
- **Neutrophils** are key components of the innate immune system, primarily involved in fighting bacterial infections through **phagocytosis**, degranulation, and formation of **neutrophil extracellular traps (NETs)**.
- They are not specialized for detecting and inducing apoptosis in virus-infected cells.
*Eosinophils*
- **Eosinophils** are primarily involved in the immune response against **parasitic infections** and allergic reactions.
- They release granules containing toxic proteins against parasites and contribute to inflammation, but they do not directly kill virus-infected cells via caspase activation.
Acute inflammation mechanisms US Medical PG Question 8: A 3-year-old female is found to have unusual susceptibility to infections by catalase-producing organisms. This patient likely has a problem with the function of which of the following cell types?
- A. Natural killer cells
- B. Eosinophils
- C. B cells
- D. T cells
- E. Neutrophils (Correct Answer)
Acute inflammation mechanisms Explanation: ***Neutrophils***
- Catalase-producing organisms, such as *Staphylococcus aureus* or *Aspergillus*, are typically cleared by **phagocytic cells**, specifically **neutrophils**, which use the **respiratory burst** to produce reactive oxygen species.
- A defect in neutrophil function, particularly in the **NADPH oxidase enzyme complex** responsible for the respiratory burst, leads to **chronic granulomatous disease (CGD)**, characterized by increased susceptibility to infections by these specific pathogens.
*Natural killer cells*
- **Natural killer (NK) cells** are primarily involved in the anti-viral and anti-tumor immune responses, recognizing and **killing infected or malignant cells**.
- They do not play a primary role in clearing bacterial or fungal infections, especially those caused by catalase-producing organisms.
*Eosinophils*
- **Eosinophils** are primarily involved in defense against **parasitic infections** and in mediating **allergic reactions**.
- Their role in clearing common bacterial or fungal infections is limited.
*B cells*
- **B cells** are responsible for **humoral immunity**, producing **antibodies** that neutralize pathogens and toxins or opsonize them for phagocytosis.
- While antibodies can aid in the clearance of many pathogens, a primary deficiency in B cell function (e.g., agammaglobulinemia) would lead to broad susceptibility to encapsulated bacteria, not specifically catalase-positive organisms.
*T cells*
- **T cells** are central to **cell-mediated immunity**, recognizing and eliminating intracellular pathogens or directly killing infected cells.
- Deficiencies in T cell function (e.g., SCID) lead to severe immunodeficiency with susceptibility to opportunistic infections, but do not specifically point to problems with catalase-producing organisms as the hallmark.
Acute inflammation mechanisms US Medical PG Question 9: Two days after being admitted for acute myocardial infarction, a 61-year-old man has sharp, substernal chest pain that worsens with inspiration and improves when leaning forward. Cardiac examination shows a scratchy sound best heard over the left sternal border. Histopathological examination of the infarcted myocardial tissue is most likely to show which of the following findings?
- A. Neutrophilic infiltration
- B. Collagenous scar tissue
- C. Normal myocardium
- D. Coagulative necrosis (Correct Answer)
- E. Granulation tissue with macrophages
Acute inflammation mechanisms Explanation: ***Coagulative necrosis***
- The patient's clinical presentation (sharp, substernal chest pain, worsening with inspiration, improving while leaning forward, and a scratchy pericardial friction rub) indicates **post-MI fibrinous pericarditis**, a common complication occurring 2-4 days after myocardial infarction.
- At **day 2 post-MI**, the infarcted myocardium demonstrates **coagulative necrosis** as the primary and most characteristic histopathological finding, representing irreversible ischemic cell death with preserved tissue architecture.
- While neutrophilic infiltration is also present at this timepoint, coagulative necrosis of the cardiomyocytes themselves is the defining pathological feature that distinguishes irreversible myocardial injury.
*Neutrophilic infiltration*
- **Neutrophilic infiltration** is indeed present at day 2 post-MI (peaks at days 1-3) as part of the acute inflammatory response to clear necrotic debris.
- However, neutrophils represent the **reactive inflammatory response** rather than the primary pathological change in the infarcted cardiomyocytes themselves.
- The question asks about the most characteristic histopathological finding, which is the **coagulative necrosis** of the myocardial cells, not the secondary inflammatory infiltrate.
*Collagenous scar tissue*
- **Collagenous scar tissue** forms much later during the remodeling phase, typically **7 weeks or more** after MI, representing the final stage of healing.
- At day 2, the tissue is still in the acute phase of coagulative necrosis and early inflammation, far too early for mature fibrous scar formation.
*Normal myocardium*
- The patient has sustained an **acute myocardial infarction** with irreversible injury to cardiac tissue.
- Histopathological examination of the infarcted region would show clear abnormalities, not **normal myocardium**.
*Granulation tissue with macrophages*
- **Granulation tissue** with fibroblasts, new capillaries, and macrophages begins forming during the proliferative phase, typically starting around **days 5-7** post-MI.
- At day 2, it is too early for granulation tissue formation; the tissue is still dominated by coagulative necrosis and acute neutrophilic inflammation.
Acute inflammation mechanisms US Medical PG Question 10: A 22-year-old man is rushed to the emergency room with constant, severe right lower abdominal pain that started 7 hours ago in the periumbilical region and later shifted to the right lower quadrant with a gradual increase in intensity. The patient's blood pressure is 110/80 mm Hg, the heart rate is 76/min, the respiratory rate is 17/min, and the temperature is 37.5℃ (99.5℉). The physical examination shows tenderness, muscle guarding, and rebound over the right lower quadrant of the abdomen. Abdominal sonography shows a dilated appendix with a periappendiceal fluid collection. He is diagnosed with acute appendicitis and undergoes a laparoscopic appendectomy. Histopathologic examination of the removed appendix shows transmural acute inflammation with abundant neutrophils infiltrating the appendiceal wall. Which of the following substances is responsible for attracting these neutrophils to the inflamed tissue?
- A. IL-10
- B. IL-7
- C. IL-8 (Correct Answer)
- D. CCL-11
- E. CXCL-9
Acute inflammation mechanisms Explanation: ***IL-8***
- **IL-8 (CXCL8)** is a potent **chemoattractant** for **neutrophils**, which are the primary inflammatory cells seen in acute appendicitis and are responsible for the "marked cells" in the histopathology of acute inflammation.
- It is produced by macrophages, endothelial cells, and epithelial cells at the site of infection and inflammation, guiding neutrophils to the affected tissue.
*IL-10*
- **IL-10** is an **anti-inflammatory cytokine** that inhibits the production of pro-inflammatory cytokines and suppresses immune responses.
- It would **reduce** the inflammatory cell infiltrate rather than attracting it.
*IL-7*
- **IL-7** is a cytokine important for the **development and survival of lymphocytes**, particularly T cells and B cells, in the bone marrow and thymus.
- It does not act as a primary chemoattractant for neutrophils in acute inflammation like appendicitis.
*CCL-11*
- **CCL-11 (eotaxin-1)** is a **chemoattractant** specifically for **eosinophils**, which are prominent in allergic reactions and parasitic infections.
- Eosinophils are not the predominant cells in acute bacterial inflammation like appendicitis.
*CXCL-9*
- **CXCL-9 (MIG)** is a chemokine that primarily attracts **T lymphocytes** and **natural killer (NK) cells**.
- It is involved in chronic inflammatory and immune responses, not the acute neutrophilic-dominated inflammation of appendicitis.
More Acute inflammation mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.