Autoimmune mechanisms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Autoimmune mechanisms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Autoimmune mechanisms US Medical PG Question 1: A 47-year-old woman comes to the physician because of progressive pain and stiffness in her hands and wrists for the past several months. Her hands are stiff in the morning; the stiffness improves as she starts her chores. Physical examination shows bilateral swelling and tenderness of the wrists, metacarpophalangeal joints, and proximal interphalangeal joints. Her range of motion is limited by pain. Laboratory studies show an increased erythrocyte sedimentation rate. This patient's condition is most likely associated with which of the following findings?
- A. IgM antibodies against the Fc region of IgG (Correct Answer)
- B. HLA-B27 protein on white blood cells
- C. HLA-A3 proteins on white blood cells
- D. HLA-DQ2 proteins on white blood cells
- E. IgG antibodies with a TNF-α binding domain on the Fc region
Autoimmune mechanisms Explanation: ***IgM antibodies against the Fc region of IgG***
- The patient's symptoms of symmetric **polyarthritis** affecting the **small joints of the hands and wrists**, morning stiffness that improves with activity, and elevated ESR are highly suggestive of **rheumatoid arthritis (RA)**.
- The finding described, **rheumatoid factor (RF)**, is an IgM antibody directed against the Fc portion of IgG and is a hallmark of RA.
*HLA-B27 protein on white blood cells*
- **HLA-B27** is strongly associated with **seronegative spondyloarthropathies**, such as **ankylosing spondylitis** and **reactive arthritis**.
- These conditions typically involve the **axial skeleton** (spine) and large joints, which differs from the presentation of small joint polyarthritis seen here.
*HLA-A3 proteins on white blood cells*
- **HLA-A3** is associated with **hereditary hemochromatosis**, a disorder of iron overload.
- While hemochromatosis can cause arthropathy, it typically affects the **second and third metacarpophalangeal joints** and does not present with the classic features of rheumatoid arthritis described.
*HLA-DQ2 proteins on white blood cells*
- **HLA-DQ2** is strongly associated with **celiac disease** and, to a lesser extent, type 1 diabetes.
- These conditions are not directly linked to the inflammatory polyarthritis presented by this patient.
*IgG antibodies with a TNF-α binding domain on the Fc region*
- This description refers to **therapeutic monoclonal antibodies** (biologics) used to treat inflammatory conditions like RA, such as **infliximab** or **adalimumab**, which are designed to bind TNF-α.
- These are **pharmacological interventions**, not diagnostic markers or naturally occurring antibodies in rheumatoid arthritis.
Autoimmune mechanisms US Medical PG Question 2: A 9-year-old boy is brought to your office due to nausea and vomiting. He had 4 episodes of non-bloody and non-bilious emesis over the last 24 hours. He denies any diarrhea or changes in his diet; however, his best friend at school recently had viral gastroenteritis and his mother is concerned that he has the same bug. She notes that he has been drinking more water than usual and wet his bed twice over the last two weeks. He is otherwise healthy and is not taking any medications. On physical exam his temperature is 99°F (37.2°C), blood pressure is 100/70 mmHg, pulse is 112/min, respirations are 26/min, and pulse oximetry is 99% on room air. He has lost 10 pounds since his previous visit 6 months ago. There is diffuse, mild abdominal tenderness to palpation. The most likely disease process responsible for this patient's symptoms is associated with which of the following?
- A. HLA-B8
- B. No association with HLA system
- C. HLA-DR2
- D. HLA-DR5
- E. HLA-DR3 (Correct Answer)
Autoimmune mechanisms Explanation: ***HLA-DR3***
- This patient's symptoms (nausea, vomiting, polydipsia, nocturia/enuresis, weight loss, tachypnea, abdominal tenderness) are highly suggestive of **new-onset Type 1 Diabetes Mellitus (T1DM)** with potential **diabetic ketoacidosis (DKA)**.
- T1DM has the **strongest genetic association** with **HLA-DR3** and **HLA-DR4** alleles, which are found in approximately 90% of patients with T1DM.
- The HLA-DR3/DR4 heterozygous genotype confers the highest risk for developing T1DM.
*HLA-B8*
- While **HLA-B8** is in linkage disequilibrium with HLA-DR3 and can be found in patients with T1DM, it is **not the primary susceptibility marker**.
- The question asks for the disease association, and **HLA-DR3 and HLA-DR4 are the direct primary markers** for T1DM, making HLA-DR3 the best answer.
- HLA-B8 is also associated with other autoimmune conditions like celiac disease and myasthenia gravis.
*No association with HLA system*
- This is **incorrect** - Type 1 Diabetes Mellitus has one of the **strongest and most well-established HLA associations** among autoimmune diseases.
- The genetic component accounts for approximately 50% of disease susceptibility, with HLA genes contributing the majority of this genetic risk.
*HLA-DR2*
- **HLA-DR2** (particularly DRB1*15:01-DQB1*06:02) is actually a **protective allele** that decreases the risk of developing T1DM.
- Its presence is negatively associated with disease development and is rarely found in patients with T1DM.
*HLA-DR5*
- **HLA-DR5** is **not a primary genetic marker** for Type 1 Diabetes Mellitus susceptibility.
- The dominant susceptibility alleles remain HLA-DR3 and HLA-DR4, which have the strongest evidence-based associations.
Autoimmune mechanisms US Medical PG Question 3: A 42-year-old woman presents complaining of pain in her hands. She reports that the pain is in both hands, and that it is usually worse in the morning. She reports that her hands are also stiff in the morning, but that this gradually improves throughout the morning. She notes, however, that her symptoms seem to be getting worse over the last three months. What is the most likely pathogenesis of her disease process?
- A. Production of antibodies against smooth muscle
- B. Anti-neutrophil cytoplasmic antibody production
- C. Production of antibodies against antibodies (Correct Answer)
- D. Type 1 hypersensitivity reaction
- E. Repetitive microtrauma
Autoimmune mechanisms Explanation: ***Production of antibodies against antibodies***
- The patient's symptoms of **bilateral hand pain and morning stiffness** improving with activity, worsening over three months, are classic for **Rheumatoid Arthritis (RA)**.
- RA is characterized by the production of **rheumatoid factor (RF)**, an antibody (typically IgM) directed against the Fc portion of IgG, which is essentially an antibody against an antibody.
*Production of antibodies against smooth muscle*
- This describes the presence of **anti-smooth muscle antibodies (ASMA)**, which are characteristic of **Autoimmune Hepatitis type 1**.
- Autoimmune hepatitis primarily affects the liver, leading to symptoms like fatigue, jaundice, and elevated liver enzymes, not primarily joint pain.
*Anti-neutrophil cytoplasmic antibody production*
- This refers to **ANCA (anti-neutrophil cytoplasmic antibodies)**, which are associated with various forms of **vasculitis**, such as Granulomatosis with Polyangiitis (Wegener's), Microscopic Polyangiitis, and Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss).
- While vasculitis can cause systemic symptoms, the patient's presentation of symmetric, inflammatory arthritis is not typical for primary ANCA-associated vasculitis.
*Type 1 hypersensitivity reaction*
- A **type I hypersensitivity reaction** involves IgE-mediated mast cell degranulation, leading to immediate allergic reactions like asthma, anaphylaxis, or hives.
- This mechanism is completely unrelated to the pathogenesis of an autoimmune, chronic inflammatory arthritis like Rheumatoid Arthritis.
*Repetitive microtrauma*
- Repetitive microtrauma is more consistent with **osteoarthritis** or **occupational overuse injuries**.
- Osteoarthritis typically presents with pain that worsens with activity and improves with rest, **morning stiffness lasting less than 30 minutes**, and often affects weight-bearing joints or specific joints due to trauma or wear and tear, rather than the inflammatory pattern described.
Autoimmune mechanisms US Medical PG Question 4: A 32-year-old man presents to the clinic with a dull low back pain radiating to the buttocks. He first noted it about 2 years ago and it has progressed since then. He notes that it is worse in the morning and improves later in the day after physical activity. The patient also reports morning stiffness lasting up to 30 minutes and blurred vision, which started about 7 months ago. The patient's vital signs include: blood pressure 130/80 mm Hg, heart rate 88/min, respiratory rate 16/min, and temperature 36.8°C (98.2°F). Physical examination reveals tenderness over the sacroiliac joints and limitation of the lumbar spine movements in the sagittal plane. The patient's X-ray is shown in the picture below. Which of the following HLA variants is associated with this patient's condition?
- A. HLA-B27 (Correct Answer)
- B. HLA-DQ2
- C. HLA-DR3
- D. HLA-B47
- E. HLA-DR4
Autoimmune mechanisms Explanation: ***HLA-B27***
- The clinical presentation of **dull low back pain**, morning stiffness improving with activity, and **blurred vision** (suggestive of uveitis) points to a spondyloarthropathy, most commonly **ankylosing spondylitis**.
- **HLA-B27** is a strong genetic risk factor and is present in a high percentage of patients with ankylosing spondylitis and other spondyloarthropathies, making it the most likely associated HLA variant.
*HLA-DQ2*
- **HLA-DQ2** is primarily associated with **celiac disease**, an autoimmune disorder affecting the small intestine, and has no direct linkage to spondyloarthropathies.
- The patient's symptoms are musculoskeletal and ocular, not gastrointestinal, which rules out celiac disease.
*HLA-DR3*
- **HLA-DR3** is associated with various autoimmune conditions such as **Type 1 Diabetes**, **Graves' disease**, and **Sjogren's syndrome**, none of which align with the patient's symptoms.
- There is no known direct association between HLA-DR3 and spondyloarthropathies or uveitis.
*HLA-B47*
- **HLA-B47** is primarily associated with **21-hydroxylase deficiency**, a form of congenital adrenal hyperplasia, and it has no relevance to the patient's musculoskeletal and ocular symptoms.
- This genetic marker is not linked to inflammatory joint diseases or uveitis.
*HLA-DR4*
- **HLA-DR4** is a significant genetic marker for **rheumatoid arthritis** and certain other autoimmune disorders.
- The patient's symptoms (back pain improving with activity, sacroiliac tenderness, uveitis) are not typical for rheumatoid arthritis, which usually affects peripheral joints and worsens with activity.
Autoimmune mechanisms US Medical PG Question 5: A 55-year-old man with a history of fatigue and exertional dyspnea presents to the urgent care clinic following an acute upper respiratory illness. On physical examination, his pulses are bounding, his complexion is very pale, and scleral icterus is apparent. The spleen is moderately enlarged. Oxygen saturation is 79% at rest, with a new oxygen requirement of 9 L by a non-rebreather mask. Laboratory analysis results show a hemoglobin level of 6.8 g/dL. Of the following options, which hypersensitivity reaction does this condition represent?
- A. Type III–immune complex-mediated hypersensitivity reaction
- B. Type I–anaphylactic hypersensitivity reaction
- C. Type IV–cell-mediated (delayed) hypersensitivity reaction
- D. Type II–cytotoxic hypersensitivity reaction (Correct Answer)
- E. Type II and III–mixed cytotoxic and immune complex hypersensitivity reaction
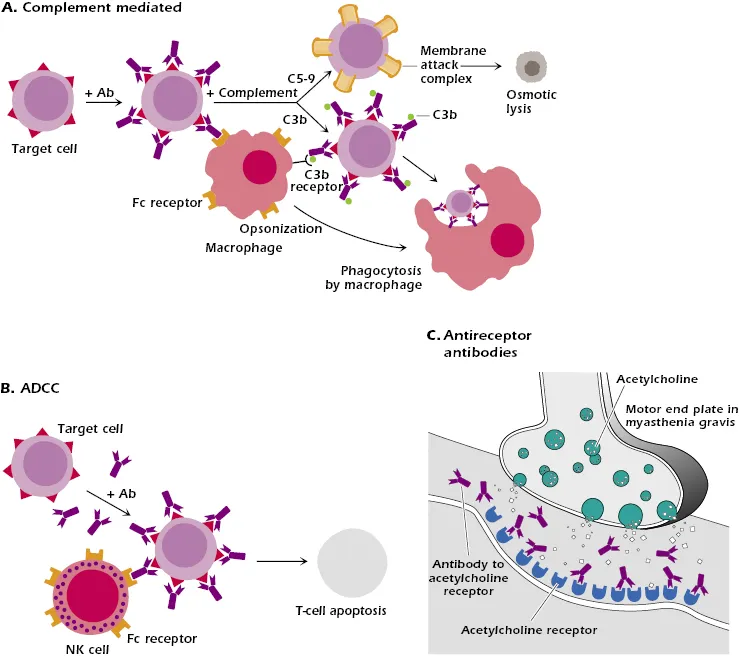
Autoimmune mechanisms Explanation: ***Type II–cytotoxic hypersensitivity reaction***
- The patient's symptoms, including **fatigue**, **exertional dyspnea**, **pale complexion**, **scleral icterus**, and **splenomegaly**, along with a **low hemoglobin** of 6.8 g/dL, strongly suggest **hemolytic anemia**.
- Following an **upper respiratory illness**, this presentation is consistent with **autoimmune hemolytic anemia (AIHA)**, where antibodies (mainly IgG or IgM) mistakenly target and destroy red blood cells, which is a classic example of a **Type II hypersensitivity reaction**.
*Type III–immune complex-mediated hypersensitivity reaction*
- This reaction involves the formation of **immune complexes** that deposit in tissues, leading to inflammation and damage, as seen in conditions like **serum sickness** or **lupus nephritis**.
- The patient's primary symptoms of **hemolysis** and **anemia** are not characteristic of immune complex deposition.
*Type I–anaphylactic hypersensitivity reaction*
- This type involves **IgE-mediated mast cell degranulation**, leading to rapid onset symptoms like **urticaria**, **angioedema**, **bronchospasm**, and **hypotension**.
- The patient's presentation of gradual onset fatigue, anemia, and icterus does not align with the acute, systemic allergic reaction seen in Type I hypersensitivity.
*Type IV–cell-mediated (delayed) hypersensitivity reaction*
- This reaction is mediated by **T cells** and **macrophages**, with a delayed onset (24-72 hours), as seen in **contact dermatitis** or **tuberculosis skin tests**.
- The patient's rapid development of severe anemia and an acute hemolytic picture is not consistent with a T-cell-mediated delayed reaction.
*Type II and III–mixed cytotoxic and immune complex hypersensitivity reaction*
- While some autoimmune conditions can involve elements of both Type II and Type III reactions, the overwhelming clinical picture in this patient points to direct **antibody-mediated destruction of red blood cells (Type II)**.
- There are no specific features mentioned, such as vasculitis or nephritis, that would strongly suggest **immune complex deposition** in addition to the prominent hemolytic anemia.
Autoimmune mechanisms US Medical PG Question 6: A 53-year-old woman presents to her primary care physician with joint pain. She reports a 6-month history of progressive pain in her hands that is worse around her knuckles. The pain is symmetric bilaterally and seems to improve after she starts working in the morning at her job in a local grocery store. She has also lost 10 pounds over the past 6 months despite no changes in her diet or exercise regimen. Her past medical history is notable for seasonal allergies, hypertension, and intermittent constipation. She takes losartan and a laxative as needed. She had adolescent idiopathic scoliosis as a child and underwent a spinal fusion at the age of 14. She does not smoke or drink alcohol. Her temperature is 98.6°F (37°C), blood pressure is 135/75 mmHg, pulse is 92/min, and respirations are 16/min. On examination, she appears well and is appropriately interactive. Strength is 5/5 and sensation to light touch is intact in the bilateral upper and lower extremities. An examination of her hands demonstrates symmetric swelling of the metacarpophalangeal joints bilaterally. This patient's condition is most strongly characterized by which of the following?
- A. HLA-DR2
- B. HLA-B8
- C. HLA-DR3
- D. HLA-B27
- E. HLA-DR4 (Correct Answer)
Autoimmune mechanisms Explanation: ***HLA-DR4***
- The patient's symptoms, including **symmetric polyarthritis** of the **small joints** (knuckles), morning stiffness that improves with activity, and weight loss, are highly suggestive of **rheumatoid arthritis (RA)**.
- **HLA-DR4** is the **MHC class II allele most strongly associated with rheumatoid arthritis** and is found in the majority of patients with seropositive RA.
*HLA-DR2*
- **HLA-DR2** is associated with other autoimmune diseases such as **multiple sclerosis**, **narcolepsy**, and **Goodpasture's syndrome**, but not typically with rheumatoid arthritis.
- There is no clinical evidence in the patient's presentation to suggest these conditions.
*HLA-B8*
- **HLA-B8** is primarily associated with diseases like **myasthenia gravis**, **celiac disease**, and **Dermatitis herpetiformis**.
- It does not have a strong association with rheumatoid arthritis.
*HLA-DR3*
- **HLA-DR3** is linked with diseases such as **celiac disease**, **Type 1 diabetes mellitus**, and **systemic lupus erythematosus**.
- While autoimmune, these conditions do not align with the patient's specific pattern of joint and systemic symptoms.
*HLA-B27*
- **HLA-B27** is strongly associated with **spondyloarthropathies**, such as **ankylosing spondylitis** and **reactive arthritis**.
- This patient's symptoms of symmetric small joint polyarthritis are inconsistent with spondyloarthropathies, which typically affect the spine and larger joints.
Autoimmune mechanisms US Medical PG Question 7: A 7-year-old boy presents to an urgent care clinic from his friend’s birthday party after experiencing trouble breathing. His father explains that the patient had eaten peanut butter at the party, and soon after, he developed facial flushing and began scratching his face and neck. This has never happened before but his father says that they have avoided peanuts and peanut butter in the past because they were worried about their son having an allergic reaction. The patient has no significant medical history and takes no medications. His blood pressure is 94/62 mm Hg, heart rate is 125/min, and respiratory rate is 22/min. On physical examination, his lips are edematous and he has severe audible stridor. Of the following, which type of hypersensitivity reaction is this patient experiencing?
- A. Type II hypersensitivity reaction
- B. Type III hypersensitivity reaction
- C. Type I hypersensitivity reaction (Correct Answer)
- D. Type IV hypersensitivity reaction
- E. Combined type I and type III hypersensitivity reactions
Autoimmune mechanisms Explanation: ***Type I hypersensitivity reaction***
- This patient is experiencing **anaphylaxis** due to **peanut exposure**, a classic example of a **Type I hypersensitivity reaction**. This involves **IgE-mediated mast cell and basophil degranulation**, releasing histamines and other inflammatory mediators.
- The symptoms like **facial flushing, itching, angioedema (edematous lips), stridor (upper airway obstruction), tachycardia**, and potentially **hypotension** (blood pressure 94/62 mmHg in a child suggests relative hypotension) are all consistent with a severe systemic allergic reaction.
*Type II hypersensitivity reaction*
- Type II hypersensitivity involves **antibody-mediated cytotoxicity**, where **IgG or IgM antibodies** bind to antigens on cell surfaces, leading to cell destruction.
- This type of reaction typically manifests as **hemolytic anemia, thrombocytopenia**, or **Goodpasture syndrome**, which are distinct from the patient's acute allergic presentation.
*Type III hypersensitivity reaction*
- Type III hypersensitivity is characterized by the formation of **immune complexes** (antigen-antibody complexes) that deposit in tissues, leading to inflammation and tissue damage.
- Conditions like **serum sickness, lupus nephritis**, or **Arthus reaction** are examples of Type III reactions and do not fit the acute, IgE-mediated symptoms seen in this patient.
*Type IV hypersensitivity reaction*
- Type IV hypersensitivity is a **delayed-type hypersensitivity** reaction mediated by **T-cells**, not antibodies. It takes 24-72 hours to develop.
- Examples include **contact dermatitis (e.g., poison ivy)**, **tuberculin skin test reactions**, or **graft rejection**, which are much slower and have different mechanisms than the immediate anaphylactic response described.
*Combined type I and type III hypersensitivity reactions*
- While some complex immune conditions might involve multiple types of hypersensitivity over time, the patient's acute, rapid-onset symptoms after peanut ingestion are overwhelmingly characteristic of a **primary Type I hypersensitivity reaction**.
- There is no clinical evidence in this presentation to suggest the involvement of **immune complex deposition** (Type III) in addition to the immediate IgE-mediated response.
Autoimmune mechanisms US Medical PG Question 8: A 31-year-old woman presents to her primary care provider to discuss the results from a previous urine analysis. She has no new complaints and feels well. Past medical history is significant for systemic lupus erythematosus. She was diagnosed 5 years ago and takes hydroxychloroquine every day and prednisone when her condition flares. Her previous urine analysis shows elevated protein levels (4+) and blood (3+). The urine sediment contained red blood cells (6 RBCs/high-power field). The treating physician would like to perform a renal biopsy to rule out lupus nephritis. What type of hypersensitivity is suggestive of lupus nephritis?
- A. Type IV, mediated by IgG and IgM antibodies
- B. Type IV, mediated by CD4+ T cells
- C. Type III, mediated by IgG antibodies (Correct Answer)
- D. Type I, mediated by IgE antibodies
- E. Type II, mediated by IgG and IgM antibodies
Autoimmune mechanisms Explanation: ***Type III, mediated by IgG antibodies***
- Lupus nephritis is a classic example of a **Type III hypersensitivity reaction**, characterized by the formation of **immune complexes** (combinations of antibodies and antigens) in the circulation.
- These circulating **autoantibody-antigen complexes** deposit in the glomeruli of the kidneys, activating complement and initiating an inflammatory response that damages renal tissue.
*Type IV, mediated by IgG and IgM antibodies*
- **Type IV hypersensitivity** is a **delayed-type reaction** mediated by T cells, not antibodies.
- IgG and IgM antibodies are involved in Type II and Type III hypersensitivity, not Type IV.
*Type IV, mediated by CD4+ T cells*
- While **Type IV hypersensitivity** is indeed mediated by **CD4+ T cells** (and CD8+ T cells), lupus nephritis is primarily an **immune complex-mediated (Type III)** disease.
- T cells do play a role in the pathogenesis of SLE, but the direct kidney damage in lupus nephritis is driven by antibody-antigen complex deposition.
*Type I, mediated by IgE antibodies*
- **Type I hypersensitivity** is an **immediate allergic reaction** mediated by **IgE antibodies** binding to mast cells and basophils, leading to histamine release.
- This type of reaction is responsible for conditions like asthma, allergies, and anaphylaxis, and is not involved in lupus nephritis.
*Type II, mediated by IgG and IgM antibodies*
- **Type II hypersensitivity** involves **antibodies directly targeting antigens on cell surfaces or extracellular matrix components**, leading to cell lysis or dysfunction.
- While IgG and IgM are involved, the defining feature is direct binding to fixed tissue antigens rather than deposition of circulating immune complexes as seen in lupus nephritis.
Autoimmune mechanisms US Medical PG Question 9: A 12-year-old child is exposed to pollen while playing outside. The allergen stimulates TH2 cells of his immune system to secrete a factor that leads to B-cell class switching to IgE. What factor is secreted by the TH2 cell?
- A. IL-4 (Correct Answer)
- B. IL-22
- C. TGF-beta
- D. IL-17
- E. IFN-gamma
Autoimmune mechanisms Explanation: ***IL-4***
- **Interleukin-4 (IL-4)** is a key cytokine produced by **TH2 cells** that promotes **B-cell class switching to IgE**, central to allergic reactions.
- It also stimulates the differentiation of naive T cells into **TH2 cells**, further amplifying the **allergic response**.
*IL-22*
- **IL-22** is primarily involved in maintaining **epithelial barrier integrity** and promoting **tissue repair**, especially in the gut and skin.
- It does not play a direct role in **IgE class switching** or the pathogenesis of type I hypersensitivity.
*TGF-beta*
- **TGF-beta (Transforming Growth Factor-beta)** is a pleiotropic cytokine involved in **cell growth**, differentiation, apoptosis, and immune regulation, particularly promoting **Treg cell development** and IgA class switching.
- It primarily suppresses rather than promotes **allergic reactions** and IgE production.
*IL-17*
- **IL-17** is a cytokine predominantly produced by **TH17 cells** and is crucial in protection against **extracellular bacteria and fungi**.
- It is associated with **autoimmune diseases** and inflammation but not directly with IgE-mediated allergic responses.
*IFN-gamma*
- **Interferon-gamma (IFN-gamma)** is a critical **TH1 cytokine** that activates macrophages, enhances natural killer cell activity, and promotes the cell-mediated immune response.
- It typically **inhibits TH2 responses** and IgE production, thus working against the development of allergic reactions.
Autoimmune mechanisms US Medical PG Question 10: A 33-year-old man comes into the urgent care clinic with an intensely itchy rash on the bilateral mid-lower extremities, with a fine linear demarcation approximately an inch above his socks. The rash is arranged in streaks of erythema with superimposed vesicular lesions. The patient states that he recently began hiking in the woods behind his house, but he denies any local chemical exposures to his lower extremities. His vital signs include: blood pressure of 127/76, heart rate of 82/min, and respiratory rate of 12/min. Of the following options, which is the mechanism of his reaction?
- A. Type III–immune complex-mediated hypersensitivity reaction
- B. Type IV–cell-mediated (delayed) hypersensitivity reaction (Correct Answer)
- C. Type II–cytotoxic hypersensitivity reaction
- D. Type I–anaphylactic hypersensitivity reaction
- E. Type III and IV–mixed immune complex and cell-mediated hypersensitivity reactions
Autoimmune mechanisms Explanation: **Type IV–cell-mediated (delayed) hypersensitivity reaction**
- The described rash with **erythema**, **vesicular lesions**, and a **linear demarcation** after hiking is classic for **allergic contact dermatitis**, often caused by plants like poison ivy, which is a **Type IV hypersensitivity reaction**.
- This reaction is **delayed**, usually appearing 24-72 hours after exposure, and is mediated by **T lymphocytes** and **macrophages** reacting to the antigen.
*Type III–immune complex-mediated hypersensitivity reaction*
- This type of reaction involves the formation of **immune complexes** (antigen-antibody), leading to inflammation and tissue damage.
- Clinically, it often presents as **vasculitis**, **serum sickness**, or conditions like **lupus nephritis**, which do not match the localized, vesicular rash described.
*Type II–cytotoxic hypersensitivity reaction*
- This reaction involves **antibodies** (IgG or IgM) binding to antigens on cell surfaces, leading to cell destruction or dysfunction.
- Examples include **hemolytic transfusion reactions** and **autoimmune hemolytic anemia**, which are distinct from allergic contact dermatitis.
*Type I–anaphylactic hypersensitivity reaction*
- This is an **immediate hypersensitivity** reaction mediated by **IgE antibodies** binding to mast cells, leading to histamine release.
- Symptoms typically include **urticaria**, **angioedema**, **bronchospasm**, and **anaphylaxis**, occurring rapidly after exposure.
*Type III and IV–mixed immune complex and cell-mediated hypersensitivity reactions*
- While some conditions can involve features of both Type III and Type IV, the clinical picture of **allergic contact dermatitis** is predominantly a **pure Type IV (delayed cell-mediated) reaction**.
- The primary mechanism of the described rash does not involve immune complex deposition.
More Autoimmune mechanisms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.