White blood cell disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for White blood cell disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
White blood cell disorders US Medical PG Question 1: A 69-year-old Caucasian man presents for a routine health maintenance examination. He feels well. He has no significant past medical history. He takes aspirin for the occasional headaches that he has had for over several years. He exercises every day and does not smoke. His father was diagnosed with a hematologic malignancy at 79 years old. The patient’s vital signs are within normal limits. Physical examination shows no abnormalities. The laboratory test results are as follows:
Hemoglobin 14.5 g/dL
Leukocyte count 62,000/mm3
Platelet count 350,000/mm3
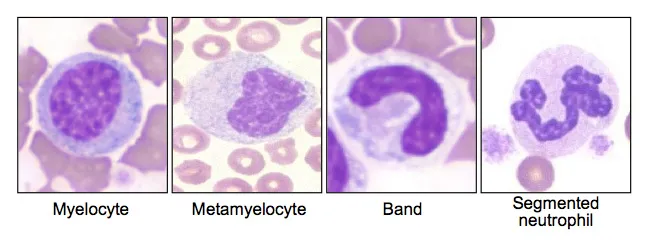
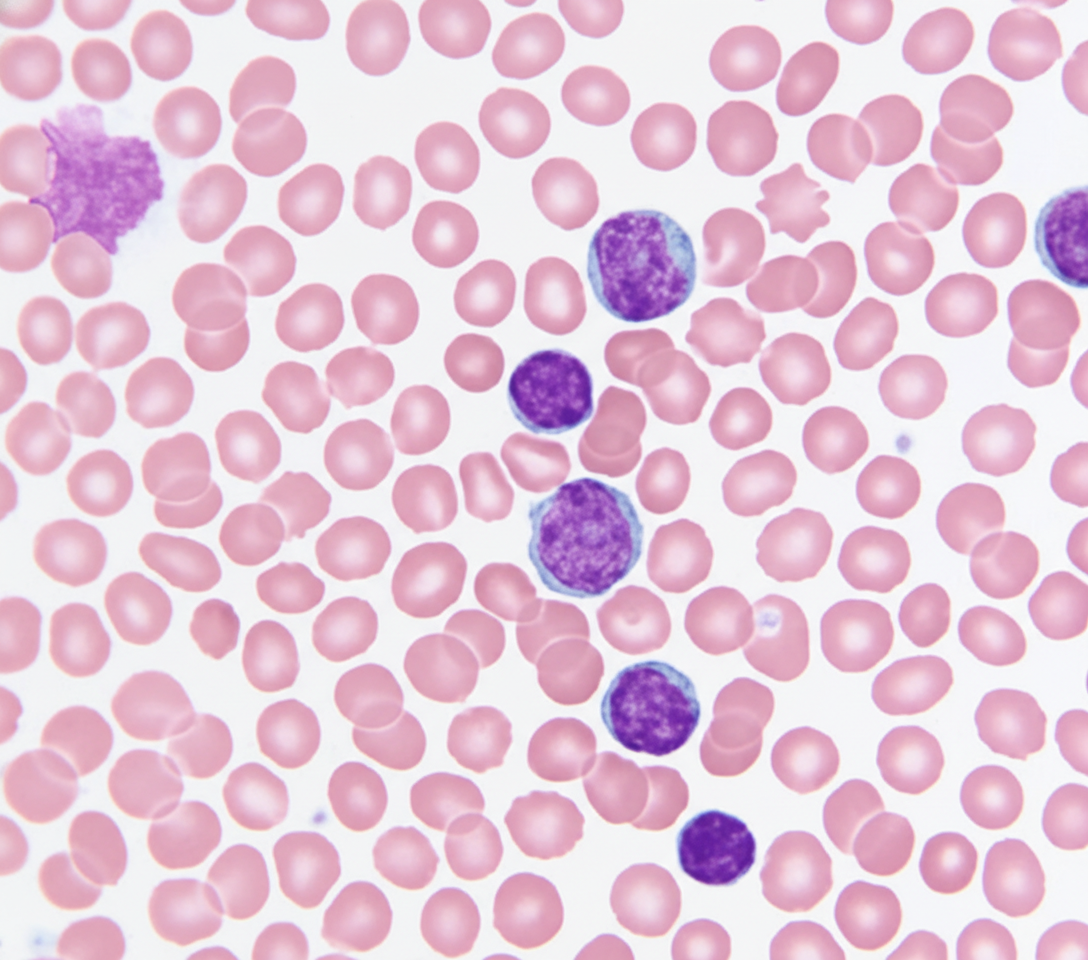
A peripheral blood smear is obtained (shown on the image). Which of the following best explains these findings?
- A. Acute lymphoid leukemia
- B. Hairy cell leukemia
- C. Adult T cell leukemia
- D. Chronic lymphocytic leukemia (Correct Answer)
- E. Acute myeloid leukemia
White blood cell disorders Explanation: ***Chronic lymphocytic leukemia***
- The image displays characteristic **smudge cells** (also known as **basket cells**) and mature-looking lymphocytes with scant cytoplasm and condensed chromatin, which are hallmarks of CLL.
- The patient's age (69 years), elevated leukocyte count (62,000/mm³), and the presence of these particular cells on peripheral smear in an otherwise asymptomatic individual are all highly suggestive of CLL.
*Acute lymphoid leukemia*
- This condition is characterized by a proliferation of **blasts** (immature lymphocytes) in the bone marrow and peripheral blood, which are not depicted in the provided image.
- While it can present with a high leukocyte count, the cellular morphology would show a predominance of immature cells rather than the mature-appearing lymphocytes and smudge cells seen here.
*Hairy cell leukemia*
- This leukemia is characterized by lymphocytes with **fine cytoplasmic projections** (hairy cells) and typically leads to **pancytopenia**, particularly leukopenia, rather than the marked leukocytosis seen in this patient.
- The morphology in the image does not show these cytoplasmic projections.
*Adult T cell leukemia*
- This form of leukemia is caused by the **human T-lymphotropic virus type 1 (HTLV-1)** and is more prevalent in specific endemic regions (e.g., Japan, Caribbean).
- It usually presents with **atypical pleomorphic T-cells** with convoluted nuclei, often accompanied by skin lesions, hypercalcemia, and lymphadenopathy, none of which are mentioned or depicted.
*Acute myeloid leukemia*
- AML is characterized by an overgrowth of **myeloblasts** (immature myeloid cells) in the bone marrow and peripheral blood, often containing **Auer rods**.
- The cells in the image are clearly lymphoid in origin and do not show features of myeloblasts or Auer rods.
White blood cell disorders US Medical PG Question 2: A 61-year-old woman presents to her primary care physician for a routine check-up. Physical examination demonstrates asymmetric peripheral neuropathy in her feet. The patient has no previous relevant history and denies any symptoms of diabetes. Routine blood work shows normal results, and she is referred to a hematologist. Subsequent serum protein electrophoresis demonstrates a slightly elevated gamma globulin level, and monoclonal gammopathy of undetermined significance is diagnosed. Which of the following diseases is most likely to develop over the course of this patient’s condition?
- A. Acute myelocytic leukemia
- B. Chronic myelocytic leukemia
- C. Multiple myeloma (Correct Answer)
- D. Waldenström macroglobulinemia
- E. Chronic lymphocytic leukemia
White blood cell disorders Explanation: ***Multiple myeloma***
- This patient has **monoclonal gammopathy of undetermined significance (MGUS)**, confirmed by the asymmetric peripheral neuropathy, elevated gamma globulin, and monoclonal gammopathy. MGUS has a 1% annual risk of progressing to **multiple myeloma**.
- **Peripheral neuropathy** is a common initial presentation of MGUS, and its progression to multiple myeloma involves the proliferation of **plasma cells** in the bone marrow, leading to end-organ damage.
*Acute myelocytic leukemia*
- This is a **myeloid malignancy** characterized by rapid proliferation of abnormal myeloid blasts in the bone marrow, not typically preceded by MGUS or presenting with peripheral neuropathy.
- It usually presents with symptoms like **fatigue**, **bleeding**, and **infections**, unrelated to the monoclonal gammopathy.
*Chronic myelocytic leukemia*
- This is a **myeloproliferative disorder** associated with the **Philadelphia chromosome (BCR-ABL1 fusion gene)**, which is distinct from conditions involving plasma cell dyscrasias like MGUS.
- It classically presents with **splenomegaly** and a high white blood cell count with a myeloid shift.
*Waldenström macroglobulinemia*
- This is a **lymphoplasmacytic lymphoma** involving IgM monoclonal gammopathy, which can cause neuropathy similar to MGUS. However, MGUS with IgG or IgA is more common and has a higher progression risk to multiple myeloma than to Waldenström macroglobulinemia.
- While it involves **monoclonal gammopathy**, the clinical picture of MGUS with its specific progression risk profile is more indicative of eventual multiple myeloma.
*Chronic lymphocytic leukemia*
- This is a **lymphoid malignancy** characterized by the accumulation of mature but functionally incompetent lymphocytes, particularly B-cells.
- It is not typically preceded by MGUS and usually presents with **lymphadenopathy**, **splenomegaly**, and **lymphocytosis**.
White blood cell disorders US Medical PG Question 3: A 64-year-old woman comes to the physician for her routine health maintenance examination. She feels well. She had cervical cancer and received radiotherapy 8 years ago. Her vital signs are within normal limits. On percussion, the spleen size is 15 cm. Otherwise, the physical examination shows no abnormalities. The laboratory test results are as follows:
Hemoglobin 10 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 65,000/mm3
Platelet count 500,000/mm3
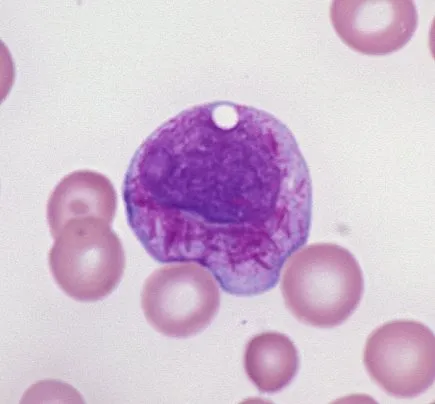
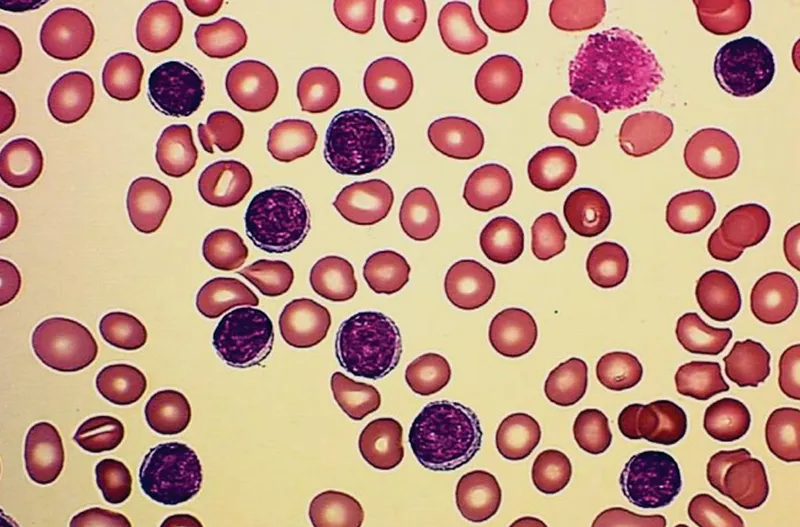
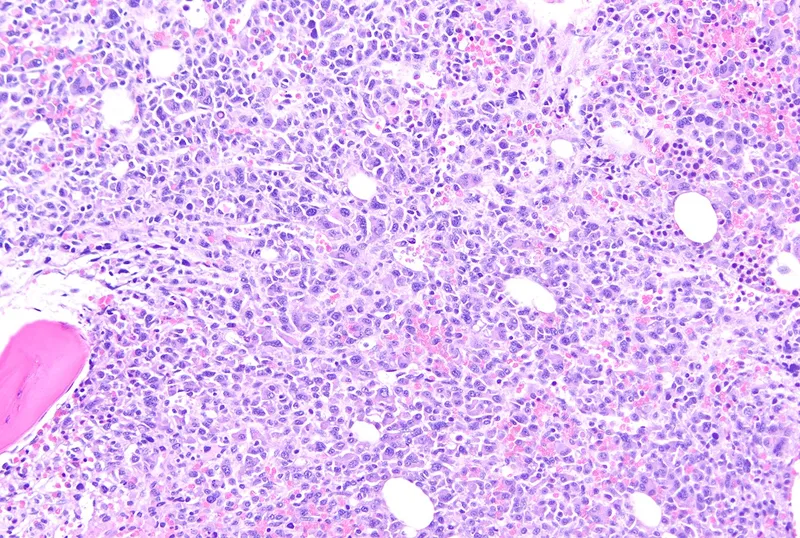
Two images of the peripheral blood smear are shown on the image. Which of the following is the most appropriate next step in management?
- A. Phlebotomy
- B. Rituximab
- C. Watchful waiting
- D. Allogeneic stem cell transplantation
- E. Dasatinib (Correct Answer)
White blood cell disorders Explanation: ***Dasatinib***
- The patient's presentation with **anemia**, **marked leukocytosis (65,000/mm³) with predominantly myeloid cells**, **thrombocytosis (500,000/mm³)**, and **splenomegaly (15 cm)** is highly suggestive of **Chronic Myeloid Leukemia (CML)**. The peripheral smear showing **myelocytes, metamyelocytes, and basophils** (indicated by arrows on the image) further supports this diagnosis.
- **Dasatinib** is a second-generation **tyrosine kinase inhibitor (TKI)** that targets the **BCR-ABL fusion protein**, which is the hallmark of CML. TKIs are the first-line treatment for CML.
*Phlebotomy*
- This is primarily used for **polycythemia vera** to reduce red blood cell mass and hematocrit.
- It is not indicated for CML, which is characterized by an overproduction of myeloid cells, not primarily red blood cells.
*Rituximab*
- **Rituximab** is a monoclonal antibody targeting the **CD20 antigen** on B-lymphocytes.
- It is used in the treatment of **B-cell non-Hodgkin lymphoma** and some autoimmune diseases, not CML.
*Watchful waiting*
- Given the patient's clear signs of **CML (leukocytosis, thrombocytosis, splenomegaly, and characteristic peripheral smear)**, active treatment is indicated, not watchful waiting.
- CML, if left untreated, progresses from the chronic phase to accelerated phase and then to **blast crisis**, which is rapidly fatal.
*Allogeneic stem cell transplantation*
- **Allogeneic stem cell transplantation** is a potentially curative treatment for CML.
- However, it is typically reserved for patients who have **failed TKI therapy** or have high-risk features, as **TKIs are the initial first-line treatment** due to their effectiveness and lower toxicity compared to transplantation.
White blood cell disorders US Medical PG Question 4: A 72-year-old man goes to his primary care provider for a checkup after some blood work showed lymphocytosis 3 months ago. He says he has been feeling a bit more tired lately but doesn’t complain of any other symptoms. Past medical history is significant for hypertension and hyperlipidemia. He takes lisinopril, hydrochlorothiazide, and atorvastatin. Additionally, his right hip was replaced three years ago due to osteoarthritis. Family history is noncontributory. He drinks socially and does not smoke. Today, he has a heart rate of 95/min, respiratory rate of 17/min, blood pressure of 135/85 mm Hg, and temperature of 36.8°C (98.2°F). On physical exam, he looks well. His heartbeat has a regular rate and rhythm and lungs that are clear to auscultation bilaterally. Additionally, he has mild lymphadenopathy of his cervical lymph nodes. A complete blood count with differential shows the following:
Leukocyte count 5,000/mm3
Red blood cell count 3.1 million/mm3
Hemoglobin 11.0 g/dL
MCV 95 um3
MCH 29 pg/cell
Platelet count 150,000/mm3
Neutrophils 40%
Lymphocytes 40%
Monocytes 5%
A specimen is sent for flow cytometry that shows a population that is CD 5, 19, 20, 23 positive. Which of the following is the most likely diagnosis?
- A. Chronic lymphocytic leukemia (Correct Answer)
- B. Immune thrombocytopenic purpura
- C. Aplastic anemia
- D. Acute lymphoblastic leukemia
- E. Tuberculosis
White blood cell disorders Explanation: ***Chronic lymphocytic leukemia***
- The patient presents with mild **lymphadenopathy**, a **history of lymphocytosis**, and a **flow cytometry** showing cells positive for **CD5, CD19, CD20, and CD23**, which is pathognomonic for **CLL**.
- While the total leukocyte count is within normal limits due to the absolute neutrophil decrease, the persistent lymphocytosis and characteristic immunophenotype are highly indicative of CLL.
*Immune thrombocytopenic purpura*
- This condition is characterized by **isolated thrombocytopenia** caused by autoantibody-mediated platelet destruction, which is not supported by the patient's normal platelet count (150,000/mm3).
- While it can cause fatigue, it doesn't explain the lymphocytosis or the specific **CD marker profile**.
*Aplastic anemia*
- Aplastic anemia involves **pancytopenia** (decreased red blood cells, white blood cells, and platelets) due to bone marrow failure, which is not consistent with the patient's normal-range leukocyte and platelet counts.
- The patient's presentation with lymphocytosis and lymphadenopathy further makes this diagnosis unlikely.
*Acute lymphoblastic leukemia*
- **ALL** typically presents with symptoms related to **bone marrow failure** (anemia, thrombocytopenia, infections) and often very **high blast counts** in the peripheral blood and bone marrow.
- While it involves lymphocytes, the specific **CD5/19/20/23 co-expression** is characteristic of CLL, and ALL usually involves more aggressive symptoms and a different immunophenotype.
*Tuberculosis*
- **Tuberculosis** is an infectious disease that can cause **lymphadenopathy** and systemic symptoms like fatigue, but it is typically associated with a **caseating granulomatous inflammation** and is diagnosed via cultures or PCR rather than flow cytometry.
- It would not explain the specific **B-cell lymphocytosis** with the described immunophenotype.
White blood cell disorders US Medical PG Question 5: A 39-year-old man presents to the emergency department with the complaint of ‘cola-colored’ urine that he noticed this morning. Additionally, he complains of malaise and reports that he has not been able to be productive at work since last week. Lab results revealed a hemoglobin of 6.7 g/dL, leukocyte total count of 1,000 cells/mm3, and a reticulocyte count of 6%. Coomb test is negative and flow cytometry shows CD55/CD59-negative red blood cells. Concerned about the results of his complete blood count, his physician explains the diagnosis to the patient. Which of the following sets of events best describes the mechanism underlying the development of neutropenia?
- A. ↑ release of neutrophils in the bone marrow, ↑ destruction of neutrophils, and ↑ activation of neutrophil adhesion molecules
- B. ↓ activation of neutrophil adhesion molecules and ↓ production of neutrophils in the bone marrow
- C. ↑ activation of neutrophil adhesion molecules, ↓ destruction of neutrophils, and ↓ production of neutrophils in the bone marrow
- D. ↑ activation of neutrophil adhesion molecules, ↓ release of neutrophils in the bone marrow, and ↑ destruction of neutrophils
- E. ↓ production of neutrophils in the bone marrow, ↑ destruction of neutrophils, and ↑ activation of neutrophil adhesion molecules (Correct Answer)
White blood cell disorders Explanation: ***↓ production of neutrophils in the bone marrow, ↑ destruction of neutrophils, and ↑ activation of neutrophil adhesion molecules***
- **Paroxysmal nocturnal hemoglobinuria (PNH)**, indicated by the **CD55/CD59-negative red blood cells** and **cola-colored urine (hemoglobinuria)**, is characterized by a defect in **hematopoietic stem cells** in the **bone marrow**, leading to the **decreased production of all myeloid cell lines**, including neutrophils.
- The deficiency of **glycosylphosphatidylinositol-anchored proteins (GPI-APs)**, specifically **CD55** and **CD59**, on the surface of neutrophils in PNH makes them susceptible to **complement-mediated destruction**, and their increased activation of adhesion molecules can paradoxically lead to their sequestration or increased clearance.
*↑ release of neutrophils in the bone marrow, ↑ destruction of neutrophils, and ↑ activation of neutrophil adhesion molecules*
- **Neutropenia** (low leukocyte count) is due to a **decreased production** and/or **increased destruction**, not increased release, of neutrophils from the bone marrow.
- While increased destruction and activation of adhesion molecules can contribute to neutropenia, the initial step in PNH is impaired production.
*↓ activation of neutrophil adhesion molecules and ↓ production of neutrophils in the bone marrow*
- While **decreased production of neutrophils** in the bone marrow correctly describes a component of neutropenia in PNH, **decreased activation of neutrophil adhesion molecules** is not a feature; instead, there is often paradoxically increased activation leading to sequestration.
- Reduced adhesion molecule activation would typically lead to impaired margination and increased circulating neutrophils (leukocytosis) in the setting of inflammation, not neutropenia.
*↑ activation of neutrophil adhesion molecules, ↓ destruction of neutrophils, and ↓ production of neutrophils in the bone marrow*
- In PNH, the neutrophils are actually highly susceptible to **complement-mediated destruction** due to the lack of complement-inhibiting proteins like CD55 and CD59, hence there is **increased destruction**, not decreased.
- While **decreased production** and **increased activation of adhesion molecules** may contribute, the statement incorrectly suggests decreased destruction.
*↑ activation of neutrophil adhesion molecules, ↓ release of neutrophils in the bone marrow, and ↑ destruction of neutrophils*
- Although there is **increased destruction** and **increased activation of neutrophil adhesion molecules**, the primary issue is **decreased production** of neutrophils from the bone marrow, not specifically decreased release of adequately produced cells.
- The underlying **hematopoietic stem cell defect** results in a failure to generate sufficient neutrophils in the first place.
White blood cell disorders US Medical PG Question 6: A 30-year-old man is admitted to the hospital with a presumed pneumonia and started on antibiotics. Two days later, the patient shows no improvement. Blood cultures reveal yeast with pseudophyphae. Which of the following cell types is most likely deficient or dysfunctional in this patient?
- A. Eosinophils
- B. Macrophages
- C. Neutrophils (Correct Answer)
- D. T-cells
- E. B-cells
White blood cell disorders Explanation: ***Neutrophils***
- The presence of **yeast with pseudohyphae** in blood cultures, particularly *Candida*, indicates a fungal infection.
- **Neutrophils** are crucial for the host defense against *Candida* and other fungal pathogens, so their deficiency or dysfunction would predispose to candidemia.
- Neutropenia or neutrophil dysfunction (e.g., chronic granulomatous disease) significantly increases risk of invasive candidiasis.
*Eosinophils*
- **Eosinophils** are primarily involved in defense against **parasitic infections** and in allergic reactions.
- They play a minimal role in the immune response to systemic fungal infections like candidemia.
*Macrophages*
- **Macrophages** are phagocytic cells that contribute to antifungal immunity, particularly in tissue surveillance and chronic infection control.
- However, **neutrophils** are the primary and most critical defense against acute *Candida* bloodstream infections.
- Macrophage deficiency alone does not typically predispose to candidemia as severely as neutrophil deficiency.
*T-cells*
- **T-cells** are important for cell-mediated immunity, particularly against **intracellular pathogens** and viral infections.
- While they play a role in modulating antifungal responses, their deficiency typically leads to infections with *Pneumocystis jirovecii* or severe mucocutaneous candidiasis, rather than disseminated candidemia.
*B-cells*
- **B-cells** are responsible for **humoral immunity** through antibody production, which is primarily effective against extracellular bacteria and toxins.
- They are not the primary line of defense against fungal infections such as candidemia.
White blood cell disorders US Medical PG Question 7: A 59-year-old man presents to his primary care physician for fatigue. In general, he has been in good health; however, he recently has experienced some weight loss, abdominal pain, and general fatigue. He has a past medical history of anxiety, diabetes, a fracture of his foot sustained when he tripped, and a recent cold that caused him to miss work for a week. His current medications include metformin, insulin, buspirone, vitamin D, calcium, and sodium docusate. His temperature is 99.5°F (37.5°C), blood pressure is 150/100 mmHg, pulse is 90/min, respirations are 18/min, and oxygen saturation is 98% on room air. Physical exam reveals a calm gentleman. A mild systolic murmur is heard in the left upper sternal region. The rest of the physical exam is within normal limits. Laboratory values are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 66,500/mm^3 with normal differential
Platelet count: 177,000/mm^3
Leukocyte alkaline phosphatase: elevated
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
BUN: 20 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.9 mEq/L
AST: 12 U/L
ALT: 10 U/L
Which of the following is the most likely diagnosis?
- A. Chronic myeloid leukemia
- B. Acute lymphoblastic leukemia
- C. Multiple myeloma
- D. Leukemoid reaction (Correct Answer)
- E. Chronic lymphocytic leukemia
White blood cell disorders Explanation: ***Leukemoid reaction***
- The **highly elevated leukocyte count** (66,500/mm^3) with **normal differential** and **elevated leukocyte alkaline phosphatase (LAP)** are classic features of a leukemoid reaction.
- This condition is a reactive increase in white blood cells, often triggered by **severe infections, inflammation, or malignancy**, rather than a primary hematologic malignancy.
- The patient's **recent cold/infection** provides a clear trigger for this reactive process.
*Chronic myeloid leukemia*
- While CML also presents with marked leukocytosis, it is typically characterized by a **low or normal LAP score** and a left shift with immature myeloid forms (e.g., myelocytes, metamyelocytes).
- The patient's **normal differential** and **elevated LAP score** argue strongly against CML.
*Acute lymphoblastic leukemia*
- ALL is characterized by the presence of a large number of **lymphoblasts** (immature lymphocytes) in the blood and bone marrow, which is not suggested by the normal differential.
- It usually presents with symptoms of **bone marrow failure** (anemia, thrombocytopenia, infection) and often affects children, though it can occur in adults.
*Multiple myeloma*
- Multiple myeloma is a plasma cell malignancy characterized by **monoclonal gammopathy**, bone lesions, renal failure, and hypercalcemia; **marked leukocytosis is not a primary feature**.
- Although the patient has mildly elevated calcium, the absence of other myeloma features (renal dysfunction, anemia, bone pain) and the **very high WBC count with elevated LAP** make this diagnosis unlikely.
*Chronic lymphocytic leukemia*
- CLL is characterized by a **profound lymphocytosis** (elevated lymphocytes) with mature-appearing cells, which is not described by the "normal differential" of the leukocyte count.
- The elevated LAP would also be unusual in CLL, as CLL cells typically have low LAP activity.
White blood cell disorders US Medical PG Question 8: A 79-year-old woman who lives alone is brought to the emergency department by her neighbor because of worsening confusion over the last 2 days. Due to her level of confusion, she is unable to answer questions appropriately. She has had type 2 diabetes mellitus for 29 years for which she takes metformin. Vital signs include: blood pressure 111/72 mm Hg, temperature 38.5°C (101.3°F), and pulse 100/min. Her fingerstick blood glucose is 210 mg/dL. On physical examination, she is not oriented to time or place and mistakes the nursing assistant for her cousin. Laboratory results are shown:
Hemoglobin 13 g/dL
Leukocyte count 16,000/mm3
Segmented neutrophils 70%
Eosinophils 1%
Basophils 0.3%
Lymphocytes 25%
Monocytes 4%
Which of the following is the most likely diagnosis?
- A. Brief psychotic disorder
- B. Alzheimer's dementia
- C. Delirium (Correct Answer)
- D. Depression
- E. Delusional disorder
White blood cell disorders Explanation: **Delirium**
- The patient presents with **acute-onset confusion**, **disorientation** to time and place, and **misidentification of individuals**, all fluctuating symptoms characteristic of delirium.
- The presence of **fever** (38.5°C), **leukocytosis** (16,000/mm³ with neutrophilia), and **hyperglycemia** (210 mg/dL) suggests an underlying acute medical condition (e.g., infection) as a precipitating factor for delirium in a vulnerable elderly patient with diabetes.
*Brief psychotic disorder*
- This disorder is characterized by the sudden onset of **psychotic symptoms** (e.g., delusions, hallucinations, disorganized speech) lasting less than 1 month, but it is not typically associated with an acute medical illness or systemic signs like fever and leukocytosis.
- While the patient exhibits confusion, the clinical picture points more strongly to an acute organic cause rather than a primary psychiatric disorder.
*Alzheimer's dementia*
- Alzheimer's dementia typically manifests as a **gradual, progressive decline** in cognitive function over months to years, not an acute change in mental status over 2 days.
- Although advanced dementia can present with confusion and disorientation, the acute onset, fluctuating nature, and signs of an underlying infection make delirium more likely.
*Depression*
- Depression in the elderly can sometimes cause **cognitive slowing** or **"pseudodementia,"** but it does not typically present with acute disorientation, fever, or leukocytosis.
- The patient's presentation is more consistent with an acute confusional state rather than altered mood or anhedonia associated with depression.
*Delusional disorder*
- Delusional disorder involves **persistent, non-bizarre delusions** without other prominent psychotic symptoms or significant impairment in functioning, typically developing over a longer period.
- The patient's global confusion, disorientation, and acute medical signs are inconsistent with a primary delusional disorder.
White blood cell disorders US Medical PG Question 9: A 14-year-old boy presents with abdominal pain and diarrhea after returning from an East Asian vacation. Stool sample reveals the presence of red and white blood cells. Stool culture shows growth of immobile, non-lactose fermenting gram-negative rods. The attending physician explains to the medical students that the bacteria function by invading intestinal M-cells. The bacterium responsible for this patient's infection is:
- A. Shigella dysenteriae (Correct Answer)
- B. Salmonella enteritidis
- C. Helicobacter pylori
- D. Escherichia coli
- E. Vibrio cholerae
White blood cell disorders Explanation: ***Shigella dysenteriae***
- The combination of **abdominal pain**, **bloody diarrhea** (red and white blood cells in stool), **immobile, non-lactose fermenting gram-negative rods**, and **invasion of M-cells** is classic for *Shigella* infection.
- *Shigella* species, particularly *S. dysenteriae*, cause **dysentery** by directly invading and destroying the intestinal epithelium, often in M-cells, leading to inflammation and ulceration.
*Salmonella enteritidis*
- While *Salmonella enteritidis* is also a **non-lactose fermenting gram-negative rod** and can cause diarrhea, it is typically **motile** (unlike the immobile bacteria described) and invades enterocytes, not specifically M-cells for its primary pathogenic mechanism.
- While it can cause bloody diarrhea, the **immotility** and primary M-cell invasion point away from *Salmonella*.
*Helicobacter pylori*
- *Helicobacter pylori* is a **spiral-shaped, gram-negative bacterium** primarily associated with gastritis and peptic ulcers, not acute bloody diarrhea.
- It colonizes the stomach lining and is not characteristically an immobile, non-lactose fermenting rod found in diarrheal stool.
*Vibrio cholerae*
- *Vibrio cholerae* causes **profuse watery diarrhea** (cholera) and is characterized by a **comma-shaped gram-negative rod** that is highly motile.
- It does not cause bloody diarrhea or invade M-cells; its pathogenicity is due to the production of an enterotoxin.
*Escherichia coli*
- While *E. coli* is a **gram-negative rod** and some strains can cause diarrhea (e.g., EHEC, ETEC), most strains are **lactose fermenting**.
- Pathogenic *E. coli* strains have various mechanisms, but the specific combination of **immobile, non-lactose fermenting rods with M-cell invasion** leading to dysentery is not characteristic of common diarrheagenic *E. coli*.
White blood cell disorders US Medical PG Question 10: A 42-year-old man comes to his physician with a history of fever, non-bloody diarrhea, and headache for 10 days. He also complains of anorexia and abdominal pain. He returned from a trip to India 3 weeks ago. His temperature is 40.0°C (104.0°F), pulse is 65/min, respirations are 15/min, and blood pressure is 135/80 mm Hg. He has developed a blanchable rash on his chest and trunk. A photograph of the rash is shown. Examination of the heart, lungs, and abdomen show no abnormalities. Laboratory studies show:
Hemoglobin 15 g/dL
Mean corpuscular volume 95 μm3
White blood cell count 3400/mm3
Percent segmented neutrophils 40%
Which of the following is the most likely diagnosis?
- A. Leptospirosis
- B. Enteric fever (Correct Answer)
- C. Dengue fever
- D. Malaria
- E. Nontyphoidal salmonellosis
White blood cell disorders Explanation: ***Enteric fever***
- The constellation of **fever**, **non-bloody diarrhea**, **bradycardia** (pulse 65/min with 40°C fever), **leukopenia** (WBC 3400/mm³), **rose spots** (blanchable rash on chest/trunk), and recent travel to **India** (endemic area) is highly characteristic of enteric fever caused by *Salmonella Typhi* or *Paratyphi*.
- Abdominal pain, anorexia, and headache are also common symptoms, and the relatively low **neutrophil percentage** (40%) further supports the diagnosis of a bacterial infection with atypical white blood cell response.
*Leptospirosis*
- While leptospirosis can cause **fever** and **headache** and is found in tropical regions, it typically presents with **conjunctival suffusion**, **muscle pain**, and sometimes **jaundice** or **renal involvement**, none of which are detailed here.
- Exposure usually involves contact with contaminated water or soil, and **diarrhea** is less common than in enteric fever.
*Dengue fever*
- Dengue fever is characterized by **high fever**, severe **myalgia** and **arthralgia** ("breakbone fever"), and often a **maculopapular rash**, but **bradycardia** and **leukopenia** with low neutrophils are not typical features.
- **Hemorrhagic manifestations** are also a concern in severe dengue, which are not described.
*Malaria*
- Malaria presents with cyclical **fever** (often paroxysmal), **chills**, **sweats**, and frequently causes **anemia** and **thrombocytopenia**.
- While **leukopenia** can occur, the presence of **rose spots** and sustained fever with relative **bradycardia** point away from malaria as the primary diagnosis.
*Nontyphoidal salmonellosis*
- This typically causes **gastroenteritis** with **diarrhea**, **vomiting**, and **fever**, which is usually self-limiting.
- It would not typically present with **rose spots**, pronounced **bradycardia**, or a prolonged course with systemic symptoms suggestive of enteric fever.
More White blood cell disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.