Splenic pathology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Splenic pathology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Splenic pathology US Medical PG Question 1: A 32 year-old African American man with a past medical history of sickle cell anemia presents to his primary care physician for a routine check-up. He has no complaints. His physician notes that he likely has an increased susceptibility to infections with certain organisms. Which of the following patient groups has a similar pattern of increased susceptibility?
- A. Hemophilia B
- B. C5-9 complement deficiency
- C. T-cell deficiency
- D. Hemophilia A
- E. C3 complement deficiency (Correct Answer)
Splenic pathology Explanation: ***C3 complement deficiency***
- Patients with **sickle cell anemia** often experience **autosplenectomy** due to recurrent vaso-occlusive crises, leading to functional asplenia and impaired complement-mediated opsonization and clearance of encapsulated bacteria. A **C3 complement deficiency** directly impairs the entire complement cascade (both classical and alternative pathways), resulting in a similar defect in **opsonization** and clearance, particularly for **encapsulated bacteria**.
- Both conditions lead to an increased susceptibility to infections with encapsulated bacteria such as *Streptococcus pneumoniae*, *Haemophilus influenzae type b*, and *Neisseria meningitidis* due to the impaired ability to clear these pathogens from the bloodstream.
*Hemophilia B*
- This is an **X-linked recessive bleeding disorder** caused by a deficiency in coagulation factor IX.
- It results in **impaired clotting** and an increased risk of bleeding, not an increased susceptibility to specific infections.
*C5-9 complement deficiency*
- A deficiency in **C5-9 complement components** specifically impairs the formation of the **membrane attack complex (MAC)**.
- This primarily leads to an increased susceptibility to infections with **Neisseria species** (e.g., *N. meningitidis*, *N. gonorrhoeae*), as MAC is crucial for lysing these gram-negative bacteria. While C3 deficiency also increases susceptibility to *Neisseria*, C5-9 deficiency is more specifically and severely linked to this pathogen.
*T-cell deficiency*
- **T-cell deficiencies** (e.g., DiGeorge syndrome, HIV/AIDS) lead to impaired **cell-mediated immunity**.
- This results in increased susceptibility to **intracellular pathogens**, **viruses**, **fungi**, and **opportunistic infections** (e.g., *Pneumocystis jirovecii*, *Candida*, CMV), which is distinct from the encapsulated bacterial infections seen in sickle cell anemia.
*Hemophilia A*
- This is an **X-linked recessive bleeding disorder** caused by a deficiency in coagulation factor VIII.
- Similar to Hemophilia B, it primarily causes **bleeding abnormalities** due to dysfunctional secondary hemostasis, not a heightened susceptibility to infections.
Splenic pathology US Medical PG Question 2: A 60-year-old man presents to his physician as part of his routine annual medical check-up. He has no specific complaints but mentions that he has often experienced fatigue over the past few months. His past medical history is noncontributory. On physical examination, his temperature is 37.2°C (98.8°F), pulse rate is 84/min, blood pressure is 130/86 mm Hg, and respiratory rate is 18/min. On general examination, mild pallor is present. Palpation of the abdomen reveals splenomegaly, which extends 6.35 cm (2.5 in) below the left costal margin. There is no hepatomegaly. Laboratory studies show the following values:
Hemoglobin 9.7 g/dL
Total leukocyte count 30,000/mm3
Granulocytes 83%
Lymphocytes 10%
Eosinophils 5%
Basophils 1%
Monocytes 1%
Platelet count 700,000/mm3
The physician orders a bone marrow biopsy analysis of hematopoietic cells. The report shows the presence of a t(9;22)(q34; q11) translocation. Which of the following is the most likely diagnosis?
- A. Chronic myeloid leukemia (Correct Answer)
- B. Transient myeloproliferative disorder
- C. Chronic myelomonocytic leukemia
- D. Chronic neutrophilic leukemia
- E. Myelodysplastic syndrome/myeloproliferative neoplasm, unclassifiable
Splenic pathology Explanation: ***Chronic myeloid leukemia***
- The presence of **fatigue**, **splenomegaly**, **leukocytosis with a predominance of granulocytes**, **thrombocytosis**, and specifically the **t(9;22)(q34; q11) translocation (Philadelphia chromosome)** are classic findings for chronic myeloid leukemia (CML).
- The **bcr-abl fusion gene** resulting from the t(9;22) translocation leads to uncontrolled tyrosine kinase activity, driving the myeloproliferation seen in CML.
*Transient myeloproliferative disorder*
- This is a condition seen almost exclusively in **neonates with Down syndrome** and typically resolves spontaneously.
- The patient's age (60 years) and the specific translocation rule out this diagnosis.
*Chronic myelomonocytic leukemia*
- This is characterized by **monocytosis** (absolute monocyte count > 1 x 10^9/L and monocytes > 10% of WBCs) and features of both myelodysplastic and myeloproliferative disorders.
- While there is leukocytosis, monocytes are only 1% of the differential, and the t(9;22) translocation is not characteristic of CMML.
*Chronic neutrophilic leukemia*
- This is a rare myeloproliferative neoplasm characterized by **sustained peripheral blood neutrophilia** and often mutations in the **CSF3R gene**.
- While the patient has neutrophilia, the presence of the t(9;22) translocation is not associated with CNL.
*Myelodysplastic syndrome/myeloproliferative neoplasm, unclassifiable*
- This is a diagnosis of exclusion category used when a patient has features of both MDS and MPN but does not fit into a specific, well-defined entity.
- Given the clear presence of the **Philadelphia chromosome**, the diagnostic criteria for **CML** are met, making a diagnosis of "unclassifiable" inappropriate.
Splenic pathology US Medical PG Question 3: A 9-year-old boy is brought to the physician by his parents because of right-sided shoulder pain for 1 day. He has not had chills or sweating. Over the past year, he was treated twice in the emergency department for painful swelling of his hands and feet. He emigrated with his family from Kenya 2 years ago. His temperature is 37.4°C (99.3°F), pulse is 96/min, and blood pressure is 123/82 mm Hg. Physical examination shows no tenderness, erythema, or joint swelling of the shoulder. Laboratory studies show:
Hemoglobin 7 g/dL
Mean corpuscular volume 88 μm
Reticulocyte count 9%
Leukocyte count 12,000/mm3
A peripheral blood smear is most likely to show which of the following abnormalities?
- A. Ring-shaped inclusions in erythrocytes
- B. Erythrocytes with no central pallor
- C. Teardrop-shaped erythrocytes
- D. Fragmentation of erythrocytes
- E. Nuclear remnants in erythrocytes (Correct Answer)
Splenic pathology Explanation: ***Nuclear remnants in erythrocytes***
- This patient's history of **recurrent painful swelling** of hands and feet, emigration from Kenya, and current shoulder pain, combined with **anemia** (hemoglobin 7 g/dL) and **elevated reticulocyte count (9%)**, strongly suggests **sickle cell disease**.
- Complications such as **vaso-occlusive crises** can cause bone pain. **Nuclear remnants (Howell-Jolly bodies)** in erythrocytes are characteristic of **functional asplenia**, a common complication of sickle cell disease due to splenic infarction.
*Ring-shaped inclusions in erythrocytes*
- **Ring-shaped inclusions** are primarily associated with parasitic infections like **malaria** (ring forms of *Plasmodium* parasites within red blood cells).
- While the patient is from Kenya, the clinical picture here is not typical for an acute malaria presentation (no fever/chills), and other findings point more strongly to sickle cell disease complications.
*Erythrocytes with no central pallor*
- **Erythrocytes with no central pallor** (spherocytes) are characteristic of **hereditary spherocytosis** or **autoimmune hemolytic anemia**.
- While both can cause anemia and an elevated reticulocyte count, the history of recurrent painful swelling of hands and feet strongly points away from these disorders.
*Teardrop-shaped erythrocytes*
- **Teardrop-shaped erythrocytes (dacryocytes)** are typically seen in **myelofibrosis** and other myeloproliferative neoplasms, or severe marrow infiltration.
- This finding is not consistent with the clinical presentation of sickle cell disease.
*Fragmentation of erythrocytes*
- **Fragmentation of erythrocytes (schistocytes)** indicates **microangiopathic hemolytic anemia (MAHA)**, seen in conditions like thrombotic thrombocytopenic purpura (TTP), hemolytic-uremic syndrome (HUS), or disseminated intravascular coagulation (DIC).
- While sickle cell crises can involve microvascular occlusion, the primary red cell abnormality in sickle cell disease isn't schistocyte formation as a hallmark feature.
Splenic pathology US Medical PG Question 4: A 66-year-old woman is brought to the emergency department because of fever, chills, night sweats, and progressive shortness of breath for 1 week. She also reports generalized fatigue and nausea. She has type 2 diabetes mellitus and hypothyroidism. Current medications include metformin, sitagliptin, and levothyroxine. She appears ill. Her temperature is 38.7°C (101.7°F), pulse is 104/min, and blood pressure is 160/90 mm Hg. Examination shows pale conjunctivae and small nontender hemorrhagic macules over her palms and soles. Crackles are heard at both lung bases. A grade 2/6 mid-diastolic murmur is heard best at the third left intercostal space and is accentuated by leaning forward. The spleen is palpated 1–2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10.6 g/dL
Leukocyte count 18,300/mm3
Erythrocyte sedimentation rate 48 mm/h
Urine
Protein 1+
Blood 2+
RBCs 20-30/hpf
WBCs 0-2/hpf
An echocardiography shows multiple vegetations on the aortic valve. Blood cultures grow S. gallolyticus. She is treated with ampicillin and gentamicin for 2 weeks and her symptoms resolve. A repeat echocardiography at 3 weeks shows mild aortic regurgitation with no vegetations. Which of the following is the most appropriate next step in management?
- A. Esophagogastroduodenoscopy
- B. CT scan of the abdomen and pelvis
- C. Colonoscopy (Correct Answer)
- D. Warfarin therapy
- E. Implantable defibrillator
Splenic pathology Explanation: ***Colonoscopy***
- The isolation of **_S. gallolyticus_** (formerly _S. bovis_ biotype I) in blood cultures, especially in the context of infective endocarditis, is highly associated with **colorectal neoplasms** (adenomas or carcinomas).
- Therefore, a **colonoscopy** is essential to screen for underlying gastrointestinal malignancy, even after the infection has been successfully treated.
*Esophagogastroduodenoscopy*
- While _S. gallolyticus_ can originate from the GI tract, its strong association is specifically with **colorectal pathology**, not primarily upper GI sources.
- An EGD would not be the initial, most appropriate next step given the specific microorganism.
*CT scan of the abdomen and pelvis*
- A CT scan can detect abdominal masses but is **less sensitive** than colonoscopy for detecting adenomatous polyps or early-stage colorectal cancer.
- It would also not provide a tissue diagnosis, which is crucial for characterizing any detected lesions.
*Warfarin therapy*
- Warfarin is an anticoagulant used to prevent thromboembolic events, but there is **no indication for chronic anticoagulation** in this patient at this stage.
- Her endocarditis has resolved, and the mild aortic regurgitation alone does not necessitate warfarin.
*Implantable defibrillator*
- An implantable defibrillator is used to prevent sudden cardiac death in patients at high risk of **ventricular arrhythmias**.
- There is no information in the clinical scenario suggestive of such a risk, and her cardiac issue (mild aortic regurgitation post-endocarditis) does not warrant this intervention.
Splenic pathology US Medical PG Question 5: A 55-year-old man comes to the physician for a routine health visit. He feels well except for occasional left-sided abdominal discomfort and left shoulder pain. He has smoked 1 pack of cigarettes daily for 20 years. He does not drink alcohol. His pulse is 85/min and his blood pressure is 130/70 mmHg. Examination shows a soft, nontender abdomen. The spleen is palpated 5 cm below the costal margin. There is no lymphadenopathy present. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 12.2 g/dL
Hematocrit 36 %
Leukocyte count 34,000/mm3
Platelet count 450,000/mm3
Cytogenetic testing of his blood cells is pending. Further evaluation of this patient is most likely to show which of the following findings?
- A. Autoimmune hemolytic anemia
- B. Elevated serum β2 microglobulin
- C. Elevated serum calcium
- D. Decreased basophil count
- E. Low leukocyte alkaline phosphatase score (Correct Answer)
Splenic pathology Explanation: ***Low leukocyte alkaline phosphatase score***
- The patient's presentation with **splenomegaly**, **leukocytosis** (34,000/mm³), and a normal hemoglobin/platelet count, strongly suggests a **myeloproliferative neoplasm**, specifically **chronic myeloid leukemia (CML)**.
- A **low leukocyte alkaline phosphatase (LAP) score** is a classic diagnostic feature of CML, as the neutrophils in CML have decreased LAP activity.
*Autoimmune hemolytic anemia*
- This condition is characterized by **anemia** and signs of **hemolysis**, such as elevated reticulocytes and lactate dehydrogenase, which are not described.
- While anemia is present, the primary issue indicated by the high leukocyte count and splenomegaly is a myeloproliferative disorder, not solely autoimmune hemolysis.
*Elevated serum β2 microglobulin*
- Elevated **β2 microglobulin** is a marker of **lymphocytic proliferation** and is commonly seen in conditions like **multiple myeloma** or **lymphoma**.
- The patient's dominant features of **marked leukocytosis** and **splenomegaly** are more consistent with a myeloid disorder than a lymphoid one.
*Elevated serum calcium*
- **Hypercalcemia** is a common complication of **multiple myeloma** or certain **carcinomas** due to bone destruction or paraneoplastic syndromes.
- The patient's symptoms and lab findings (especially high leukocyte count and splenomegaly) do not point to these conditions.
*Decreased basophil count*
- In conditions like **CML**, an **elevated basophil count** is often observed, which contradicts the option of a decreased basophil count.
- Other myeloproliferative neoplasms can also have varying basophil counts, but a decrease is not a hallmark.
Splenic pathology US Medical PG Question 6: A 40-year-old man presents to the office with complaints of epigastric discomfort for the past 6 months. He adds that the discomfort is not that bothersome as it does not interfere with his daily activities. He does not have any other complaints at the moment. The past medical history is insignificant. He is a non-smoker and does not consume alcohol. He recently came back from a trip to South America where he visited a relative who owned a sheep farm. On physical examination, he has a poorly palpable epigastric non-tender mass with no organomegaly. The hepatitis B and C serology are negative. The liver CT scan and MRI are shown. What is the most likely diagnosis?
- A. Echinococcosis (Correct Answer)
- B. Liver abscess
- C. Hepatocellular carcinoma
- D. Tuberculosis
- E. Hemangioma
Splenic pathology Explanation: ***Echinococcosis (Correct Answer)***
- The patient's history of travel to **South America** and contact with a **sheep farm** is highly suggestive of exposure to *Echinococcus granulosus*, the causative agent of hydatid disease.
- The **CT scan image** shows a large, well-defined cyst with a **calcified wall** and internal septations, consistent with the characteristic appearance of a **hydatid cyst** in the liver.
- This presentation is classic for **hepatic echinococcosis**: chronic indolent course, epidemiological exposure, and pathognomonic imaging findings.
*Liver abscess (Incorrect)*
- Liver abscesses typically present with more acute symptoms such as **fever, chills, and significant pain**, which are absent in this case.
- Imaging usually reveals a **hypo-dense lesion** with a rim of enhancement, possibly gas formation, and less commonly a calcified wall.
*Hepatocellular carcinoma (Incorrect)*
- This patient lacks typical risk factors for HCC, such as **chronic hepatitis B or C infection** (serology is negative) or cirrhosis.
- HCC imaging typically shows an **enhancing mass** that washes out on delayed phases, without the calcified, multi-loculated appearance seen here.
*Tuberculosis (Incorrect)*
- Hepatic tuberculosis typically presents with fever, weight loss, and multiple **small, hypo-dense lesions** on imaging, often with an associated pulmonary or extra-pulmonary focus.
- The single, large, calcified cystic lesion seen on imaging is not characteristic of hepatic tuberculosis.
*Hemangioma (Incorrect)*
- Hepatic hemangiomas are benign vascular tumors that often present as **incidental findings** and are typically asymptomatic.
- On CT scans, they show characteristic **peripheral nodular enhancement** that fills in centripetally on delayed phases, which is different from the calcified cyst observed.
Splenic pathology US Medical PG Question 7: A 3-year-old boy is brought to the physician because of a 5-day history of yellowing of his eyes and skin. He has had generalized fatigue and mild shortness of breath over the past 2 months. Examination shows pale conjunctivae and scleral jaundice. The spleen is palpated 4 cm below the left costal margin. Laboratory studies show a hemoglobin concentration of 8.5 g/dL and a mean corpuscular volume of 76 μm3. A peripheral blood smear shows round erythrocytes that lack central pallor. Which of the following is the most likely cause of the splenomegaly seen in this child?
- A. Metabolite accumulation
- B. Work hypertrophy (Correct Answer)
- C. Neoplastic infiltration
- D. Reticuloendothelial hyperplasia
- E. Extramedullary hematopoiesis
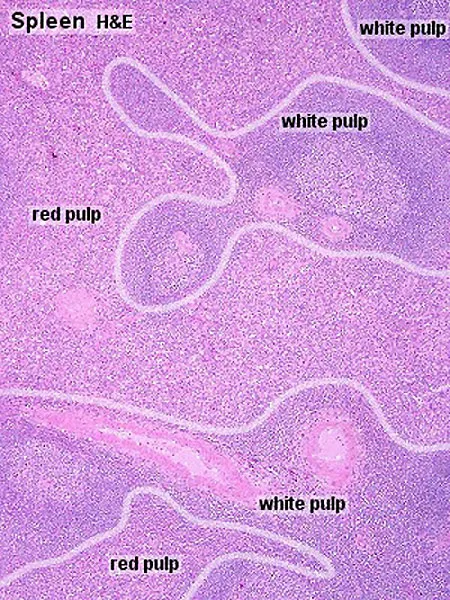
Splenic pathology Explanation: ***Work hypertrophy***
- The patient's presentation is consistent with **hereditary spherocytosis**, characterized by **hemolytic anemia**, jaundice, and **splenomegaly**.
- **Work hypertrophy** of the spleen's red pulp occurs due to its increased function in removing abnormal, rigid spherocytes from circulation, leading to its enlargement.
*Metabolite accumulation*
- This typically occurs in **lysosomal storage diseases** where defective enzymes lead to the buildup of specific metabolites within splenic macrophages.
- Conditions like **Gaucher disease** or **Niemann-Pick disease** cause splenomegaly through this mechanism, but do not present with spherocytes and hemolytic anemia.
*Neoplastic infiltration*
- This type of splenomegaly results from the infiltration of the spleen by **malignant cells**, such as in **leukemias** or **lymphomas**.
- While neoplastic infiltration can cause anemia, it is generally associated with different peripheral smear findings and systemic symptoms, not hereditary spherocytosis.
*Reticuloendothelial hyperplasia*
- While related to increased splenic activity, **reticuloendothelial hyperplasia** is a broader term encompassing the proliferation of macrophages and other immune cells in response to chronic infections or certain immune disorders.
- In hemolytic anemia, the primary driver of splenic enlargement is the excessive workload of removing red blood cells, which is best described as **work hypertrophy**.
*Extramedullary hematopoiesis*
- This refers to blood cell production occurring outside the bone marrow, often in the spleen or liver, as a compensatory mechanism in severe **bone marrow failure** or chronic hemolytic states.
- While it can contribute to splenomegaly in some chronic hemolytic anemias (e.g., thalassemia major), the primary cause of splenomegaly in hereditary spherocytosis is the *increased destruction* of abnormal RBCs by the spleen.
Splenic pathology US Medical PG Question 8: A 45-year-old woman presents to the emergency department after sustaining a gunshot wound to her shoulder. During the course of the physical exam, the physician notes her spleen is palpable 10 cm below the left costal margin. Additionally, radiography of her shoulder showed several 'punched-out' areas of lytic bone. While this was considered an incidental finding at the time, she was referred to her primary care physician for further workup. Subsequent biopsy of the spleen demonstrated that this patient’s splenomegaly was caused by an infiltrative process. Which of the following processes would most likely result in splenomegaly in this patient?
- A. Multiple myeloma (Correct Answer)
- B. Budd-Chiari syndrome
- C. Infectious mononucleosis
- D. Myelofibrosis
- E. Beta-thalassemia
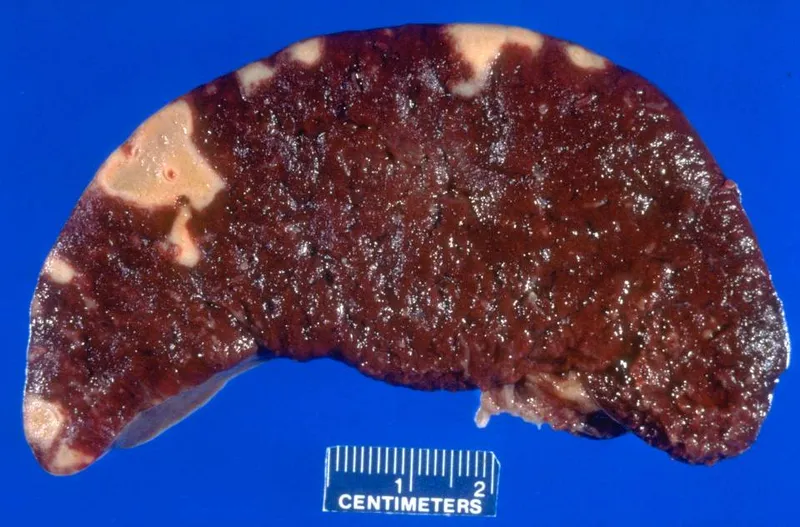
Splenic pathology Explanation: ***Multiple myeloma***
- **Multiple myeloma** is characterized by malignant plasma cell proliferation in the bone marrow, causing classic **"punched-out" lytic bone lesions** due to osteoclast-activating factors secreted by malignant plasma cells.
- While splenomegaly is less common than in other hematologic malignancies, **plasma cell infiltration of the spleen** can occur, causing splenomegaly with an **infiltrative process on biopsy**.
- The combination of **pathognomonic punched-out lytic bone lesions** + **infiltrative splenomegaly** is diagnostic of multiple myeloma with splenic involvement.
- Additional features typically include **anemia**, **hypercalcemia**, **renal insufficiency**, and elevated serum protein with monoclonal spike on electrophoresis.
*Myelofibrosis*
- **Myelofibrosis** is a myeloproliferative neoplasm causing **massive splenomegaly** due to extramedullary hematopoiesis and does cause infiltrative changes in the spleen.
- However, bone changes in myelofibrosis typically show **osteosclerosis** (increased bone density) or mixed sclerotic/lytic patterns, NOT the classic discrete "punched-out" lytic lesions described.
- The punched-out lytic lesions are the key distinguishing feature pointing to multiple myeloma, not myelofibrosis.
*Budd-Chiari syndrome*
- **Budd-Chiari syndrome** involves hepatic venous outflow obstruction, leading to **hepatomegaly**, **ascites**, and congestive splenomegaly due to portal hypertension.
- Splenomegaly is due to **passive congestion**, not an infiltrative process, and would not show infiltrative changes on biopsy.
- Does not cause lytic bone lesions.
*Beta-thalassemia*
- **Beta-thalassemia** can cause splenomegaly due to extramedullary hematopoiesis and hemolysis, with bone changes from marrow expansion.
- Bone changes show **widened medullary spaces** and "hair-on-end" appearance on skull X-ray, NOT discrete punched-out lytic lesions.
- The primary features are severe **microcytic anemia** and abnormal hemoglobin patterns, not plasma cell infiltration.
*Infectious mononucleosis*
- **Infectious mononucleosis** (EBV infection) causes acute splenomegaly due to **lymphoid hyperplasia** and immune response.
- This is a **self-limiting viral illness** that does not cause punched-out lytic bone lesions or chronic infiltrative splenomegaly.
- Biopsy would show reactive lymphoid hyperplasia, not malignant infiltration.
Splenic pathology US Medical PG Question 9: A 64-year-old man comes to the emergency department complaining of fatigue and abdominal distension. He has a remote history of intravenous drug use. Vital signs include a normal temperature, blood pressure of 120/80 mm Hg, and a pulse of 75/min. Physical examination reveals jaundice and a firm liver. Abdominal ultrasonography shows liver surface nodularity, moderate splenomegaly, and increased diameter of the portal vein. Complete blood count of the patient is shown:
Hemoglobin 14 g/dL
Mean corpuscular volume 90/μm3
Mean corpuscular hemoglobin 30 pg/cell
Mean corpuscular hemoglobin concentration 34%
Leukocyte count 7,000/mm3
Platelet count 50,000/mm3
Which of the following best represents the mechanism of low platelet count in this patient?
- A. Platelet sequestration (Correct Answer)
- B. Dilutional effect
- C. Bone marrow-based disorder
- D. Increased platelet clearance
- E. Genetic disorder
Splenic pathology Explanation: ***Platelet sequestration***
- The patient's history of IV drug use, jaundice, abdominal distension, firm liver, splenomegaly, and increased portal vein diameter are highly suggestive of **portal hypertension** due to **cirrhosis**, which often leads to **splenomegaly**.
- An enlarged spleen (splenomegaly) sequesters a disproportionately high percentage of the body's platelets, leading to **thrombocytopenia**, even if total platelet production is normal.
- **Splenic sequestration** is the **primary mechanism** of thrombocytopenia in cirrhosis with portal hypertension; up to **90% of platelets** can be sequestered in an enlarged spleen.
- Additionally, the diseased liver produces less **thrombopoietin (TPO)**, which contributes to reduced platelet production, but sequestration remains the dominant mechanism.
*Dilutional effect*
- A dilutional effect on platelet count typically occurs with **massive transfusions** of packed red blood cells and crystalloids, which is not indicated in this patient's presentation.
- While fluid overload can dilute blood components, the patient's symptoms point specifically to a **liver pathology** and related complications, not simply volume expansion.
*Bone marrow-based disorder*
- A primary bone marrow disorder would likely affect other cell lines as well, but the patient's hemoglobin and leukocyte counts are within normal limits, making a general **bone marrow suppression** less likely.
- Furthermore, the strong evidence of **cirrhosis and portal hypertension** provides a more direct and common explanation for isolated thrombocytopenia in this context.
*Increased platelet clearance*
- While increased platelet clearance can cause thrombocytopenia (e.g., in immune thrombocytopenia or thrombotic microangiopathies), there are no signs of increased destruction or consumption in this case.
- Conditions involving increased clearance usually present with other features like petechiae, purpura, or schistocytes, which are not mentioned.
- The clinical picture is most consistent with **sequestration** rather than **destruction**.
*Genetic disorder*
- Genetic disorders causing thrombocytopenia typically present much earlier in life or have a family history, which does not fit this patient's age and clinical presentation.
- The patient's history of **IV drug use** and the findings of advanced liver disease indicate an **acquired condition**, not a congenital one.
Splenic pathology US Medical PG Question 10: A 62-year-old man comes to the physician because of easy bruising and recurrent nosebleeds over the past 4 months. During the same time period, the patient has felt weak and has had a 10-kg (22-lb) weight loss. Physical examination shows mucosal pallor and bruising on the upper and lower extremities in various stages of healing. The spleen is palpated 4 cm below the left costal margin. Laboratory studies show anemia and thrombocytopenia. A photomicrograph of a peripheral blood smear is shown. Histologic examination of a bone marrow biopsy in this patient is most likely to show which of the following findings?
- A. Neoplastic granulocytes with low leukocyte alkaline phosphatase score
- B. Neoplastic lymphocytes that stain positive for tartrate-resistant acid phosphatase (Correct Answer)
- C. Neoplastic myeloid cells that stain positive for myeloperoxidase
- D. Neoplastic lymphoid cells that stain positive for terminal deoxynucleotidyl transferase activity
- E. Dysplastic erythroid cells that stain positive for iron
Splenic pathology Explanation: ***Neoplastic lymphocytes that stain positive for tartrate-resistant acid phosphatase***
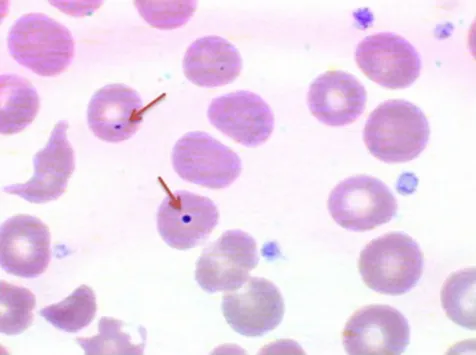
- The patient's symptoms of **easy bruising, recurrent nosebleeds, weakness, weight loss, mucosal pallor, and thrombocytopenia**, along with **splenomegaly**, are highly suggestive of a **hematologic malignancy**. The peripheral blood smear shows **lymphocytes with characteristic cytoplasmic projections ("hairy cells")**.
- **Hairy cell leukemia (HCL)** is a **B-cell lymphoma** characterized by the proliferation of these specific lymphocytes. These cells are known to stain positively for **tartrate-resistant acid phosphatase (TRAP)**, a diagnostic hallmark of this condition.
*Neoplastic granulocytes with low leukocyte alkaline phosphatase score*
- This description is characteristic of **chronic myeloid leukemia (CML)**, which typically presents with **markedly elevated white blood cell counts** (granulocytosis) and a low leukocyte alkaline phosphatase (LAP) score.
- The patient's presentation of **pancytopenia** (anemia, thrombocytopenia) and lack of **marked leukocytosis** makes CML less likely.
*Neoplastic myeloid cells that stain positive for myeloperoxidase*
- **Myeloperoxidase (MPO)** positivity is a key feature of **acute myeloid leukemia (AML)**, specifically distinguishing myeloid blasts from lymphoid blasts.
- While AML can cause **pancytopenia** and **splenomegaly**, the specific morphology of **hairy cells** in the peripheral smear and the absence of overt blasts point away from AML.
*Neoplastic lymphoid cells that stain positive for terminal deoxynucleotidyl transferase activity*
- **Terminal deoxynucleotidyl transferase (TdT)** is an enzyme found in immature lymphocytes and is a marker for **acute lymphoblastic leukemia (ALL)** and some lymphomas.
- The patient's age (62 years old) makes ALL less common than in children, and the clinical picture, particularly the **massive splenomegaly without significant lymphadenopathy** often seen in ALL, is more characteristic of hairy cell leukemia.
*Dysplastic erythroid cells that stain positive for iron*
- This finding is suggestive of **myelodysplastic syndromes (MDS)**, particularly refractory anemia with ring sideroblasts, where there is ineffective erythropoiesis and iron deposition in mitochondria of erythroid precursors (ring sideroblasts).
- While MDS can lead to **anemia** and **thrombocytopenia**, the distinctive morphology of **hairy cells** in the peripheral smear and the prominent **splenomegaly** are not typical features of MDS.
More Splenic pathology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.