Red blood cell disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Red blood cell disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Red blood cell disorders US Medical PG Question 1: A 25-year-old G2P1 woman at 12 weeks gestational age presents to the office to discuss the results of her routine prenatal screening labs, which were ordered during her 1st prenatal visit. She reports taking a daily prenatal vitamin but no other medications. She complains of mild fatigue and appears pale on exam. Her complete blood count (CBC) shows the following:
Hemoglobin (Hb) 9.5 g/dL
Hematocrit 29%
Mean corpuscular volume (MCV) 75 µm3
Which of the following are the most likely hematologic states of the patient and her fetus?
- A. Iron deficiency anemia in both the mother and the fetus
- B. Iron deficiency anemia in the mother; normal Hb levels in the fetus (Correct Answer)
- C. Pernicious anemia in the mother; normal Hb levels in the fetus
- D. Physiologic anemia in the mother; normal Hb levels in the fetus
- E. Folate deficiency anemia in both the mother and the fetus
Red blood cell disorders Explanation: ***Iron deficiency anemia in the mother; normal Hb levels in the fetus***
- The mother's lab values (Hb 9.5 g/dL, MCV 75 µm3) indicate **microcytic, hypochromic anemia**, consistent with **iron deficiency anemia**.
- The fetus prioritizes iron uptake, even in cases of severe maternal iron deficiency, meaning the **fetal hemoglobin levels** are typically normal unless maternal iron deficiency is profound and prolonged.
*Iron deficiency anemia in both the mother and the fetus*
- While the mother clearly has **iron deficiency anemia**, the fetus generally maintains **normal hemoglobin levels** by actively drawing iron from the mother, even at her expense.
- Fetal iron deficiency leading to anemia is rare unless maternal deficiency is extremely severe and prolonged, which is not indicated here.
*Pernicious anemia in the mother; normal Hb levels in the fetus*
- **Pernicious anemia** (vitamin B12 deficiency) typically presents as **macrocytic anemia** (high MCV), which contradicts the patient's MCV of 75 µm3 (microcytic).
- Although the fetus would likely have normal Hb levels in maternal pernicious anemia, the mother's lab findings do not support this diagnosis.
*Physiologic anemia in the mother; normal Hb levels in the fetus*
- **Physiologic anemia of pregnancy** is caused by a disproportionate increase in plasma volume compared to red blood cell mass, resulting in **dilutional anemia**, but usually with a **normal MCV**.
- The patient's **low MCV (75 µm3)** indicates a microcytic anemia, which is not characteristic of physiologic anemia of pregnancy.
*Folate deficiency anemia in both the mother and the fetus*
- **Folate deficiency anemia** is a type of **macrocytic anemia** (high MCV), which is inconsistent with the patient's MCV of 75 µm3.
- While severe maternal folate deficiency can affect the fetus, the maternal blood picture does not support this diagnosis.
Red blood cell disorders US Medical PG Question 2: A 37-year-old man, otherwise healthy, has a routine CBC done prior to donating blood for the first time. The results are as follows:
Hemoglobin 10.8 g/dL
Mean corpuscular volume (MCV) 82 μm3
Mean corpuscular hemoglobin concentration (MCHC) 42%
Reticulocyte count 3.2%
White blood cell count 8,700/mm3
Platelet count 325,000/mm3
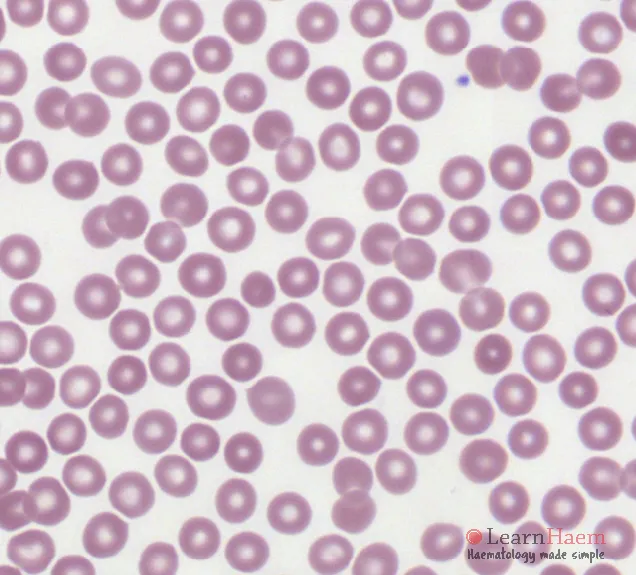
The patient is afebrile and his vital signs are within normal limits. On physical examination, his spleen is just palpable. A peripheral blood smear is shown in the exhibit (see image). A direct antiglobulin test (DAT) is negative. Which of the following best describes the etiology of this patient’s most likely diagnosis?
- A. Immune-mediated hemolysis
- B. Inherited membrane abnormality of red cells (Correct Answer)
- C. Bone marrow hypocellularity
- D. Microangiopathic process
- E. Oxidant hemolysis
Red blood cell disorders Explanation: ***Inherited membrane abnormality of red cells***
- The findings of **anemia** (Hb 10.8 g/dL), **elevated MCHC** (42%), **reticulocytosis** (3.2%), and palpable **splenomegaly** with a **negative DAT** strongly suggest **hereditary spherocytosis**.
- This condition is caused by defects in red cell membrane proteins (e.g., **spectrin, ankyrin, band 3**) leading to **spherocytes** and increased red cell destruction, primarily in the spleen.
*Immune-mediated hemolysis*
- This would typically be indicated by a **positive direct antiglobulin test (DAT)** which detects antibodies or complement components on the surface of red blood cells, but the DAT is negative in this case.
- While spherocytes can be seen in immune hemolytic anemia, the negative DAT rules out this etiology as the primary cause.
*Bone marrow hypocellularity*
- **Bone marrow hypocellularity** (e.g., in aplastic anemia) would result in **pancytopenia** (low red cells, white cells, and platelets) and a **low reticulocyte count**, indicating impaired bone marrow production, which is not seen here as the reticulocyte count is elevated.
- The presence of **splenomegaly** and **spherocytes** on the peripheral smear points away from bone marrow failure.
*Microangiopathic process*
- A **microangiopathic process** (e.g., TTP, HUS) is characterized by the presence of **schistocytes** (fragmented red cells) on the peripheral smear, often alongside **thrombocytopenia** and organ damage, none of which are explicitly mentioned or supported by the provided data.
- The presence of **spherocytes** and **elevated MCHC** does not fit with a microangiopathic process.
*Oxidant hemolysis*
- **Oxidant hemolysis** (e.g., G6PD deficiency) often presents with **Heinz bodies** (precipitated denatured hemoglobin) and **bite cells** on the peripheral smear, particularly after exposure to oxidative stressors.
- While it can cause hemolysis, the classic findings of **hereditary spherocytosis** (elevated MCHC, spherocytes, splenomegaly, negative DAT) are more specific to a membrane defect rather than oxidant injury.
Red blood cell disorders US Medical PG Question 3: A 34-year-old female with a past medical history of a gastric sleeve operation for morbid obesity presents for pre-surgical clearance prior to a knee arthroplasty. Work-up reveals a hemoglobin of 8.7 g/dL, hematocrit of 26.1%, and MCV of 106 fL. With concern for folate deficiency, she is started on high dose folate supplementation, and her follow-up labs are as follows: hemoglobin of 10.1 g/dL, hematocrit of 28.5%, and MCV of 96 fL. Given her history of gastric sleeve surgery and associated malabsorption risks, she is at long-term risk for which complication?
- A. Peripheral neuropathy (Correct Answer)
- B. Macular degeneration
- C. Hypothyroidism
- D. Microcytic anemia
- E. Neural tube defects
Red blood cell disorders Explanation: ***Peripheral neuropathy***
- Gastric sleeve surgery can lead to **vitamin B12 deficiency** due to the removal of the fundus, which produces **intrinsic factor** necessary for B12 absorption.
- **Vitamin B12 deficiency** is a known cause of **peripheral neuropathy**, manifesting as numbness, tingling, and weakness.
*Macular degeneration*
- This condition is primarily associated with **aging**, **genetics**, and **environmental factors** like smoking, rather than micronutrient deficiencies post-gastric sleeve.
- While certain vitamins (e.g., A, C, E) and minerals can influence macular health, there's no direct strong causal link between bariatric surgery malabsorption and increased risk of **macular degeneration**.
*Hypothyroidism*
- Hypothyroidism is most commonly caused by **autoimmune conditions** like Hashimoto's thyroiditis or **iodine deficiency**.
- While bariatric surgery can influence overall metabolic health, it does not directly lead to an increased risk of primary hypothyroidism.
*Microcytic anemia*
- **Microcytic anemia** is characterized by **small red blood cells (low MCV)**, typically caused by **iron deficiency** or **thalassemia**.
- The patient initially presented with **macrocytic anemia (MCV 106 fL)**, which improved with folate, but the underlying risk remains for macrocytic rather than microcytic anemia from malabsorption of B12 or folate.
*Neural tube defects*
- **Neural tube defects** are congenital anomalies that occur during early fetal development, primarily linked to **folate deficiency during pregnancy**.
- While the patient had a folate deficiency, this complication is relevant to **fetal development** and not a long-term risk for the adult patient herself after surgery.
Red blood cell disorders US Medical PG Question 4: A 32-year-old woman complains of fatigue and pallor. She says symptoms that started several months ago and have been becoming more serious with time. She reports that she has been exercising regularly and has been adhering to a strict vegan diet. The patient has no significant past medical history and takes no current medications. She denies any smoking history, alcohol use, or recreational drug use. She is tachycardic, but otherwise, her physical examination is unremarkable. A complete blood count (CBC) shows anemia with a low MCV (mean corpuscular volume), and a peripheral blood smear shows small erythrocytes. Which of the following is the most likely diagnosis in this patient?
- A. Pernicious anemia
- B. Iron deficiency anemia (Correct Answer)
- C. Glucose-6-phosphate dehydrogenase deficiency
- D. Hemolytic anemia
- E. Lead poisoning
Red blood cell disorders Explanation: ***Iron deficiency anemia***
- The patient's **vegan diet** makes her susceptible to **iron deficiency**, as primary dietary iron sources are from animal products.
- **Microcytic anemia** (low MCV and small erythrocytes) is a classic presentation of iron deficiency, further supported by symptoms like **fatigue** and **pallor**.
*Pernicious anemia*
- This is a type of **macrocytic anemia** (high MCV) caused by **vitamin B12 deficiency**, often due to an **autoimmune attack on parietal cells** leading to intrinsic factor deficiency.
- The patient in this case presents with **microcytic anemia**, which rules out pernicious anemia.
*Glucose-6-phosphate dehydrogenase deficiency*
- This is an **X-linked recessive disorder** that causes episodes of **hemolytic anemia** (rapid destruction of red blood cells) upon exposure to certain drugs, infections, or fava beans.
- It would typically present with signs of hemolysis and **normocytic/macrocytic anemia**, not microcytic.
*Hemolytic anemia*
- This refers to conditions where **red blood cells are destroyed prematurely**, leading to anemia. While it causes anemia, it typically presents with **normocytic** or **macrocytic** red blood cells, rather than the microcytic presentation seen here.
- Common signs include **jaundice**, **splenomegaly**, and elevated **reticulocyte count**, none of which are mentioned.
*Lead poisoning*
- Lead poisoning can cause a **microcytic anemia** by interfering with **heme synthesis**.
- However, it is typically associated with other symptoms such as **abdominal pain**, **neuropathy**, or **cognitive dysfunction**, and the patient's history doesn't suggest lead exposure.
Red blood cell disorders US Medical PG Question 5: A 35-year-old woman is involved in a car accident and presents with an open fracture of the left femur and severe bleeding from the left femoral artery. No past medical history or current medications. Her blood pressure is 90/60 mm Hg, pulse is 110/min, and respirations are 21/min. On physical examination, the patient is lethargic, confused, and poorly responds to commands. Peripheral pulses are 1+ in the left lower extremity below the level of the knee and 2+ elsewhere. When she arrives at the hospital, a stat hemoglobin level shows 6 g/dL. Which of the following is most correct about the patient’s condition?
- A. This patient’s laboratory findings will likely demonstrate a normocytic anemia (Correct Answer)
- B. Hemoglobin concentration will be significantly decreased immediately after the acute bleeding begins
- C. This patient will likely be diagnosed with iron deficiency anemia
- D. Hematocrit is expected to accurately reflect the degree of blood loss immediately after acute hemorrhage
- E. Her reticulocyte count is expected to be elevated at this time
Red blood cell disorders Explanation: ***This patient's laboratory findings will likely demonstrate a normocytic anemia***
- In cases of **acute blood loss**, both plasma and red blood cells are lost proportionally, leading to **normocytic, normochromic anemia** as the body has not yet had time to alter red blood cell production
- The MCV (mean corpuscular volume) remains **normal (80-100 fL)** until chronic compensatory mechanisms develop
- This distinguishes acute hemorrhage from chronic blood loss, which can eventually lead to **microcytic anemia** due to iron depletion
*Hematocrit is expected to accurately reflect the degree of blood loss immediately after acute hemorrhage*
- **Immediately after acute hemorrhage**, both red blood cells and plasma are lost proportionally, so the **hematocrit initially remains relatively unchanged** despite significant blood volume loss
- The hematocrit **drops hours later** as fluid shifts from the interstitial space into the vascular compartment to restore blood volume, diluting the remaining red blood cells
- This patient's low hemoglobin at hospital arrival reflects this compensatory hemodilution process
*Hemoglobin concentration will be significantly decreased immediately after the acute bleeding begins*
- While the patient is actively bleeding, the **hemoglobin concentration may not immediately decrease** because red blood cells and plasma are lost together in proportion
- The apparent drop in hemoglobin becomes more pronounced as the body **replenishes plasma volume** through fluid shifts or after **intravenous fluid administration**, diluting the remaining red cell mass
- The hemoglobin of 6 g/dL at hospital arrival reflects fluid shifts that have already occurred
*Her reticulocyte count is expected to be elevated at this time*
- The bone marrow requires **3-5 days to mount a reticulocytosis** in response to acute blood loss and increased erythropoietin production
- At hospital arrival shortly after the accident, the **reticulocyte count will be normal** as insufficient time has passed for bone marrow response
- An elevated reticulocyte count would be expected **several days after the hemorrhage**, not acutely
*This patient will likely be diagnosed with iron deficiency anemia*
- **Iron deficiency anemia** is a **chronic condition** characterized by **microcytic, hypochromic red blood cells** due to prolonged iron loss or inadequate dietary intake
- Acute blood loss, as seen in this trauma case, causes **normocytic anemia** with normal MCV and MCH
- Iron deficiency could develop weeks to months later if iron stores become depleted without supplementation
Red blood cell disorders US Medical PG Question 6: A 62-year-old man, a retired oil pipeline engineer, presents to his primary care physician with complaints of headaches, fatigue, and constant ringing in his ears. Recurrently he has developed pruritus, usually after a hot shower. He also noted a constant burning sensation in his fingers and toes, independent of physical activity. On examination, he has a red face and his blood pressure levels are 147/89 mm Hg. A CBC revealed that his Hb is 19.0 g/dL and Hct is 59%. Because of his condition, his physician prescribes him 81 mg of aspirin to be taken daily in addition to therapeutic phlebotomy. Which of the statements below is true about this patient’s condition?
- A. Warfarin and phlebotomy are the preferred course of treatment.
- B. The patient has a decreased risk of developing myelofibrosis.
- C. Serum erythropoietin is expected to be high.
- D. Arterial oxygen saturation is usually higher than normal values in this condition.
- E. Mutation of the JAK2 gene is commonly seen in this condition. (Correct Answer)
Red blood cell disorders Explanation: ***Mutation of the JAK2 gene is commonly seen in this condition.***
* The patient's symptoms (headaches, fatigue, tinnitus, pruritus after hot showers, erythromelalgia, facial plethora, hypertension, and elevated hemoglobin/hematocrit) are highly suggestive of **polycythemia vera (PV)**.
* Over 95% of patients with PV have a **JAK2 V617F mutation**, leading to constitutive activation of the JAK-STAT pathway, resulting in uncontrolled erythrocyte production.
*Warfarin and phlebotomy are the preferred course of treatment.*
* While **phlebotomy** is a cornerstone of PV management to reduce hematocrit and prevent thrombotic events, **warfarin** is generally not indicated for primary thromboprophylaxis in PV.
* **Low-dose aspirin** is preferred for reducing thrombotic risk, as indicated by the physician's prescription, along with phlebotomy.
*The patient has a decreased risk of developing myelofibrosis.*
* Polycythemia vera is a **myeloproliferative neoplasm**, and a significant percentage of patients (10-15%) will progress to **post-polycythemia vera myelofibrosis** over time.
* This progression is a natural history of the disease rather than a decreased risk, occurring as the bone marrow becomes exhausted and fibrotic.
*Serum erythropoietin is expected to be high.*
* In polycythemia vera, the **erythroid progenitors** are hypersensitive to erythropoietin (EPO), and red blood cell production occurs independently of EPO.
* Consequently, the **serum erythropoietin level is typically low or undetectable** due to feedback inhibition from the high red blood cell mass.
*Arterial oxygen saturation is usually higher than normal values in this condition.*
* Arterial oxygen saturation is generally **normal** in polycythemia vera, differentiating it from secondary polycythemia caused by hypoxemia (where oxygen saturation would be low).
* The increased red blood cell mass in PV does not inherently lead to higher-than-normal arterial oxygen saturation; it leads to increased oxygen-carrying capacity.
Red blood cell disorders US Medical PG Question 7: A 4-year-old boy is brought to the physician for the evaluation of fatigue since he returned from visiting family in South Africa one week ago. The day after he returned, he had fever, chills, and diffuse joint pain for 3 days. His symptoms improved with acetaminophen. He was born at term and has been healthy. His immunizations are up-to-date. His temperature is 37.6°C (99.68°F), pulse is 100/min, and blood pressure is 100/60 mm Hg. Examination shows conjunctival pallor. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.8 g/dL
Mean corpuscular volume 68 μm3
Red cell distribution width 14% (N = 13%–15%)
Hemoglobin A2 6% (N < 3.5%)
A peripheral smear shows microcytic, hypochromic erythrocytes, some of which have a darkly stained center and peripheral rim, separated by a pale ring. Which of the following is the most appropriate next step in the management of this patient?
- A. Oral pyridoxine
- B. Iron supplementation
- C. Reassurance (Correct Answer)
- D. Folic acid therapy
- E. Oral succimer
Red blood cell disorders Explanation: ***Reassurance***
- The patient's presentation with **microcytic anemia**, elevated **Hemoglobin A2 (6%)**, and **target cells** on peripheral smear is highly suggestive of **beta-thalassemia trait** (minor). This genetic condition is more common in individuals with Mediterranean, African, Middle Eastern, or South Asian ancestry.
- Beta-thalassemia trait is a **benign condition** that does not typically require specific medical intervention. The mild anemia does not usually cause significant symptoms or complications, and patients can live normal lives without treatment.
- The elevated HbA2 is the key diagnostic finding that distinguishes thalassemia trait from iron deficiency anemia.
*Oral pyridoxine*
- **Pyridoxine (Vitamin B6)** supplementation is indicated for **sideroblastic anemia**, which can also cause microcytic anemia.
- However, sideroblastic anemia typically presents with **ring sideroblasts** in the bone marrow and does not have the characteristic elevated HbA2 seen in beta-thalassemia trait.
*Iron supplementation*
- **Iron deficiency anemia** is a common cause of microcytic hypochromic anemia, but it would present with **low ferritin** and **low or normal HbA2** (not elevated).
- In this case, iron supplementation would not be appropriate and could potentially be harmful due to the risk of **iron overload** in thalassemia syndromes, even in the trait form.
- The elevated HbA2 and normal RDW help distinguish thalassemia trait from iron deficiency.
*Folic acid therapy*
- **Folic acid** is primarily used in the management of **macrocytic anemias** or in conditions with high red blood cell turnover, such as **hemolytic anemias** or major thalassemia syndromes requiring chronic transfusions.
- It is not indicated for beta-thalassemia trait, which is a microcytic anemia with normal red blood cell turnover and no significant hemolysis.
*Oral succimer*
- **Succimer** is a chelating agent used to treat **lead poisoning**, which can cause microcytic anemia with basophilic stippling.
- There are no clinical or laboratory findings in this patient (e.g., **basophilic stippling**, developmental delays, neurological symptoms, abdominal pain) to suggest lead poisoning.
Red blood cell disorders US Medical PG Question 8: A 33-year-old G2P2 woman presents with a history of fatigue and difficulty breathing upon exertion. She was not able to tolerate antenatal vitamin supplements due to nausea and constipation. Her vital signs include: temperature 37.0°C (98.6°F), blood pressure 112/64 mm Hg, and pulse 98/min. Physical examination reveals conjunctival pallor and spoon nails. Laboratory findings are significant for the following:
Hemoglobin 9.1 g/dL
Hematocrit 27.3%
Mean corpuscular volume (MCV) 73 μm3
Mean corpuscular hemoglobin (MCH) 21 pg/cell
Red cell distribution width (RDW) 17.5% (ref: 11.5–14.5%)
Serum ferritin 9 ng/mL
Which of the following would most likely be seen on a peripheral blood smear in this patient?
- A. Teardrop cells
- B. Degmacytes
- C. Basophilic stippling
- D. Echinocytes
- E. Anisopoikilocytosis (Correct Answer)
Red blood cell disorders Explanation: ***Anisopoikilocytosis***
- The patient's blood work (low **hemoglobin**, **hematocrit**, **MCV**, **MCH**, and **serum ferritin**) indicates **microcytic hypochromic anemia** due to **iron deficiency**. The elevated **RDW** suggests significant variation in red blood cell size (anisocytosis) and shape (poikilocytosis), making **anisopoikilocytosis** on the smear most likely.
- **Iron deficiency anemia** is characterized by the presence of red blood cells that vary widely in size and shape on a peripheral smear. In severe cases, a wide variety of abnormal shapes are observed (poikilocytosis), along with variations in size (anisocytosis).
*Teardrop cells*
- **Teardrop cells** (dacryocytes) are typically seen in conditions like **myelofibrosis**, **thalassemia**, or other types of **myelophthisic anemia**, which are not suggested by this patient’s presentation.
- While they can be seen in severe iron deficiency, the primary and most defining feature would be the overall variation in size and shape encapsulated by anisopoikilocytosis.
*Degmacytes*
- **Degmacytes**, also known as **bite cells**, are formed when phagocytes remove denatured hemoglobin (Heinz bodies) from red blood cells, which is characteristic of **G6PD deficiency** or other **oxidative hemolytic anemias**.
- This is not consistent with the patient's presentation of iron deficiency, which is a production problem rather than a premature destruction problem.
*Basophilic stippling*
- **Basophilic stippling** refers to the presence of small, dark blue granules in red blood cells that represent aggregated ribosomes and is typically associated with conditions such as **lead poisoning**, **thalassemia**, or **sideroblastic anemia**.
- These conditions are not indicated by the patient's symptoms or lab findings.
*Echinocytes*
- **Echinocytes**, or **burr cells**, are red blood cells with evenly spaced, spiny projections and are commonly seen in **uremia**, **pyruvate kinase deficiency**, or as an artifact of slide preparation.
- They are not a characteristic finding in iron deficiency anemia.
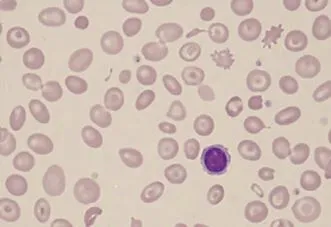
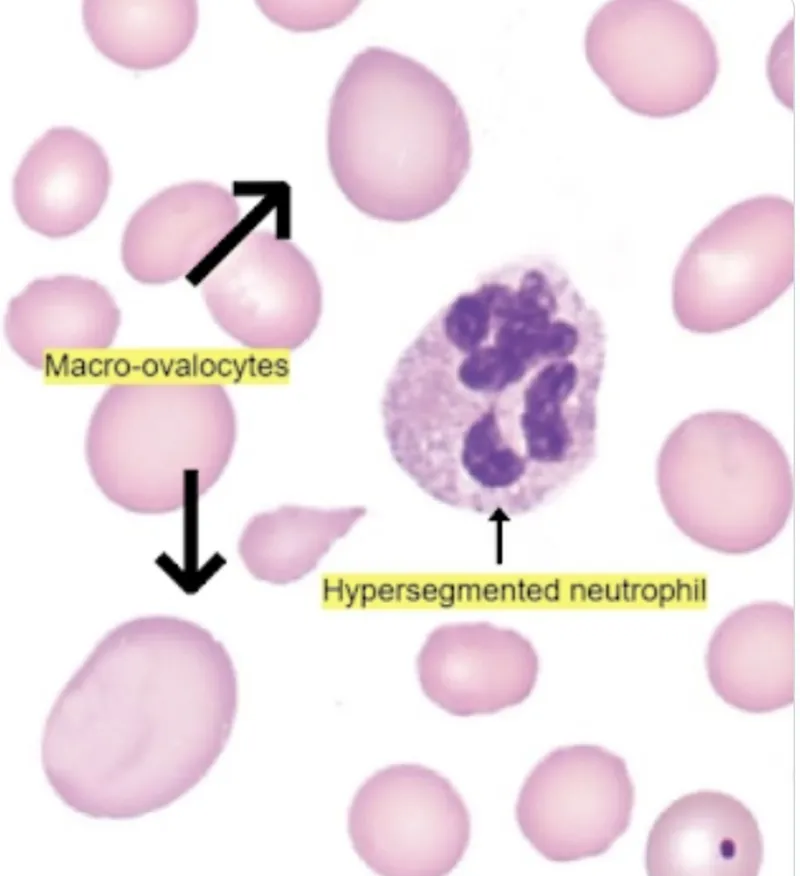
Red blood cell disorders US Medical PG Question 9: A 68-year-old man of Mediterranean descent comes to the clinic with complaints of fatigue for the past month. He reports that it is increasingly difficult for him to complete his after-dinner walks as he would get breathless and tired around 10 minutes. He endorses dizziness and an upper respiratory infection last week for which he “took a lot of aspirin.” Past medical history is significant for malaria 10 years ago (for which he was adequately treated with anti-malarial medications) and aortic stenosis status post prosthetic valve replacement 5 months ago. When asked if he has had similar episodes before, he claims, “Never! I’ve been as healthy as a horse until my heart surgery.” Physical examination is significant for mild scleral icterus bilaterally and a faint systolic murmur. Which of the following images represents a potential peripheral smear in this patient?
- A. B
- B. E
- C. C
- D. D
- E. A (Correct Answer)
Red blood cell disorders Explanation: ***A***
- Image A depicts **bite cells** and **Heinz bodies**, which are characteristic findings in **hemolysis** caused by **G6PD deficiency**. This patient's Mediterranean descent, recent aspirin use (an oxidant drug), and symptoms of fatigue, dyspnea, dizziness, and scleral icterus are highly suggestive of an acute hemolytic crisis in G6PD deficiency patients.
- **G6PD deficiency** is an X-linked recessive disorder prevalent in Mediterranean populations, where certain medications (like aspirin, sulfonamides, antimalarials) or infections can trigger episodes of acute hemolytic anemia due to oxidative stress.
*B*
- Image B shows **sickle cells**, which are characteristic of **sickle cell anemia**. While individuals with sickle cell disease can experience fatigue and anemia, there are no specific clinical elements in the vignette that point to sickle cell disease (e.g., pain crises, vaso-occlusion, or chronic hemolytic anemia from birth).
- The patient's presentation with an acute episode triggered by aspirin is less typical for a first presentation of sickle cell anemia at this age, and his prior malaria exposure is not directly linked to sickle cell disease as the cause of this acute presentation.
*E*
- Image E illustrates **schistocytes** (fragmented red blood cells) and potentially an occasional spherocyte, which are hallmarks of **microangiopathic hemolytic anemia (MAHA)**, often seen in conditions like **thrombotic thrombocytopenic purpura (TTP)**, **hemolytic uremic syndrome (HUS)**, or **disseminated intravascular coagulation (DIC)**.
- While the patient has a prosthetic valve (which can cause hemolytic anemia through mechanical stress, leading to schistocytes), the primary trigger for this acute episode appears to be G6PD deficiency, given the history of aspirin use and Mediterranean descent.
*C*
- Image C displays **spherocytes**, which are small, dense red blood cells lacking central pallor, commonly seen in **hereditary spherocytosis** or **autoimmune hemolytic anemia (AIHA)**.
- Although the patient's symptoms suggest hemolysis, the trigger (aspirin) and his ethnic background make G6PD deficiency a more likely diagnosis than hereditary spherocytosis or AIHA, which would typically present differently or have other specific findings.
*D*
- Image D demonstrates **acanthocytes (spur cells)**, which are red blood cells with irregular, spiny projections, typically associated with severe **liver disease** (e.g., cirrhosis, alcoholic liver disease), **abetalipoproteinemia**, or **hypothyroidism**.
- There are no clinical features in the vignette to suggest any of these underlying conditions, and acanthocytes are not characteristic of the acute hemolytic anemia described.
Red blood cell disorders US Medical PG Question 10: A 43-year-old man comes to the physician for a 1-week history of swelling around his eyes and decreased urination. His pulse is 87/min, and blood pressure is 152/95 mm Hg. Physical examination shows 1+ periorbital and pretibial edema. Serum studies show a urea nitrogen concentration of 21 mg/dL and a creatinine concentration of 1.4 mg/dL. Urinalysis shows 3+ blood and 1+ protein. Further evaluation of this patient is most likely to show which of the following?
- A. Urinary rhomboid crystals
- B. Renal interstitial inflammation
- C. Hypoalbuminemia
- D. Detached renal tubular epithelial cells
- E. Red blood cell casts (Correct Answer)
Red blood cell disorders Explanation: ***Red blood cell casts***
- The patient's presentation with **periorbital and pretibial edema**, **hypertension**, elevated **creatinine**, **hematuria** (3+ blood), and mild **proteinuria** (1+ protein) is highly suggestive of **acute glomerulonephritis**.
- **Red blood cell casts** are pathognomonic for **glomerulonephritis**, indicating that red blood cells are leaking from the glomeruli and congealing in the renal tubules.
*Urinary rhomboid crystals*
- **Urinary rhomboid crystals** are typically associated with conditions like **uric acid nephrolithiasis** or gout, which are not suggested by the patient's symptoms or lab findings.
- Their presence would indicate a risk for **kidney stones**, not evidence of glomerular inflammation.
*Renal interstitial inflammation*
- **Renal interstitial inflammation** is characteristic of **acute interstitial nephritis**, which often presents with fever, rash, eosinophilia, and flank pain, usually due to drug reactions or infections.
- While kidney injury can occur, the primary findings of **hematuria** and **proteinuria** in this context strongly point away from an interstitial process as the initial diagnosis.
*Hypoalbuminemia*
- **Hypoalbuminemia** is a hallmark of **nephrotic syndrome**, characterized by severe proteinuria (>3.5 g/day), significant edema, and hyperlipidemia.
- This patient has only 1+ proteinuria, which is not severe enough to cause significant hypoalbuminemia or the full nephrotic picture.
*Detached renal tubular epithelial cells*
- **Detached renal tubular epithelial cells** and **tubular cell casts** are characteristic findings in **acute tubular necrosis (ATN)**, usually resulting from ischemia or nephrotoxins.
- While ATN can cause acute kidney injury, the prominent **hematuria** and **hypertension** in this case are more indicative of a glomerular process than tubular damage.
More Red blood cell disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.