Platelet disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Platelet disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Platelet disorders US Medical PG Question 1: A previously healthy 17-year-old boy is brought to the emergency department by his mother for further evaluation after elective removal of his wisdom teeth. During the procedure, the patient had persistent bleeding from the teeth's surrounding gums. Multiple gauze packs were applied with minimal effect. The patient has a history of easy bruising. The mother says her brother had similar problems when his wisdom teeth were removed, and that he also has a history of easy bruising and joint swelling. The patient takes no medications. His temperature is 37°C (98.6°F), pulse is 90/min, and blood pressure is 108/74 mm Hg. Laboratory studies show:
Hematocrit 35%
Leukocyte count 8,500/mm3
Platelet count 160,000/mm3
Prothrombin time 15 sec
Partial thromboplastin time 60 sec
Bleeding time 6 min
Fibrin split products negative
Serum
Urea nitrogen 20 mg/dL
Creatinine 1.0 mg/dL
Bilirubin
Total 1.0 mg/dL
Direct 0.5 mg/dL
Lactate dehydrogenase 90 U/L
Peripheral blood smear shows normal-sized platelets. Which of the following is the most likely diagnosis?
- A. Hemophilia
- B. Bernard-Soulier syndrome
- C. Glanzmann thrombasthenia
- D. Von Willebrand disease (Correct Answer)
- E. Immune thrombocytopenia
Platelet disorders Explanation: ***Von Willebrand disease***
- This patient presents with a **history of easy bruising** and **persistent bleeding after a surgical procedure**, along with a **prolonged bleeding time** and **prolonged PTT**. The family history of similar bleeding issues and joint swelling (which can represent hemarthroses) in his maternal uncle is also highly suggestive of an inherited bleeding disorder. These findings, particularly the prolonged bleeding time with normal platelet count and the prolonged PTT (due to Factor VIII deficiency), are classic for **von Willebrand disease (vWD)**.
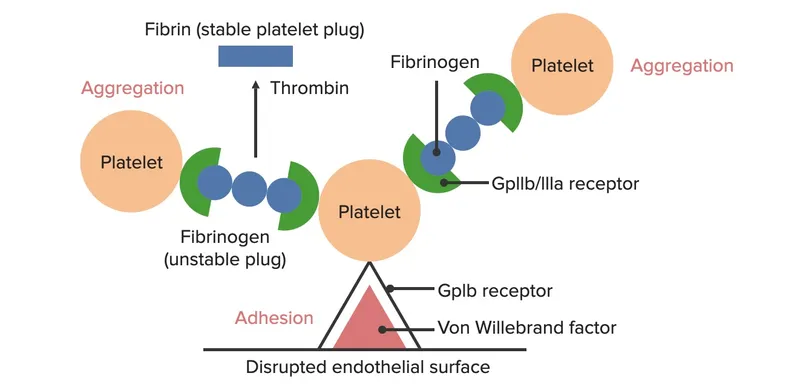
- Von Willebrand disease is the **most common inherited bleeding disorder**, characterized by a deficiency or dysfunction of **von Willebrand factor (vWF)**. vWF plays a dual role in hemostasis: it mediates platelet adhesion to the subendothelium (reflected by prolonged bleeding time) and also chaperones and protects **Factor VIII** from degradation, leading to a mild to moderate deficiency of Factor VIII (reflected by prolonged PTT).
*Hemophilia*
- Hemophilia A (Factor VIII deficiency) or Hemophilia B (Factor IX deficiency) would present with a **prolonged PTT** but a **normal bleeding time** and **platelet count**.
- While the patient has a prolonged PTT and family history of joint swelling (consistent with hemarthroses seen in hemophilia), his **prolonged bleeding time** is inconsistent with hemophilia alone.
*Bernard-Soulier syndrome*
- This syndrome is characterized by a defect in **platelet adhesion** due to a deficiency of **glycoprotein Ib (GP Ib)**, leading to **macrothrombocytopenia** (large platelets and reduced platelet count) and a **prolonged bleeding time**.
- The patient has a **normal platelet count** and **normal-sized platelets** on peripheral smear, which makes Bernard-Soulier syndrome less likely.
*Glanzmann thrombasthenia*
- This is a disorder of **platelet aggregation** due to a deficiency in **glycoprotein IIb/IIIa (GP IIb/IIIa)**, resulting in a **prolonged bleeding time** despite a normal platelet count and morphology.
- However, Glanzmann thrombasthenia typically presents with a **normal PTT**, whereas this patient has a **prolonged PTT**, making it less likely.
*Immune thrombocytopenia*
- **Immune thrombocytopenia (ITP)** is characterized by an **isolated low platelet count** (thrombocytopenia) and a **prolonged bleeding time**, with other coagulation parameters (PT, PTT) being normal.
- The patient has a **normal platelet count** (160,000/mm3) and a **prolonged PTT**, which is inconsistent with ITP.
Platelet disorders US Medical PG Question 2: A 38-year-old woman comes to the physician for a follow-up examination. She was diagnosed with immune thrombocytopenic purpura at the age of 37 years and has been treated with glucocorticoids and intravenous immune globulin. She has visited the emergency department 3 times in the past 4 months for nose bleeds, which required cauterization. Her platelet counts on her previous visits were 18,320/mm3, 17,500/mm3, and 19,100/mm3. Current medications include dexamethasone and a multivitamin. She has no children. Her immunizations are up-to-date. Vital signs are within normal limits. Examination shows petechiae on the bilateral lower extremities. Cardiopulmonary examination shows no abnormalities. The abdomen is soft and nontender; there is no organomegaly. Her hemoglobin concentration is 13.3 g/dL, leukocyte count is 8,100/mm3, and platelet count is 13,000/mm3. Her blood type is A negative. Serology for hepatitis C and HIV is negative. Which of the following is the most appropriate next step in management?
- A. Schedule splenectomy
- B. Romiplostim therapy (Correct Answer)
- C. Rituximab therapy
- D. Observation and follow-up
- E. Danazol therapy
Platelet disorders Explanation: ***Romiplostim therapy***
- This patient has **chronic ITP refractory to corticosteroids and IVIG**, with persistent severe thrombocytopenia (platelet count 13,000/mm3) and recurrent bleeding (nosebleeds, petechiae).
- **Romiplostim** is a **thrombopoietin receptor agonist (TPO-RA)** that stimulates platelet production, making it an appropriate second-line treatment in this setting to increase platelet count and reduce bleeding risk.
*Schedule splenectomy*
- While splenectomy can be effective for refractory ITP, it is typically considered after failure of **pharmacological second-line therapies**, such as TPO-RAs or rituximab.
- The patient has not yet tried other non-surgical options that might increase platelet production with less invasive risk.
*Rituximab therapy*
- **Rituximab**, an **anti-CD20 antibody**, is another second-line treatment for ITP, reducing autoantibody production.
- It is a viable option, but TPO-RAs like romiplostim are often preferred or considered alongside rituximab as highly effective options for chronic, refractory ITP.
*Observation and follow-up*
- Given the patient's **persistent severe thrombocytopenia** (platelet count 13,000/mm3) and **recurrent bleeding episodes** requiring intervention, observation is not appropriate.
- There is a high risk of spontaneous bleeding, and active management is required to prevent life-threatening hemorrhage.
*Danazol therapy*
- **Danazol**, an attenuated androgen, has been used in ITP but is generally **less effective** than and has more side effects than other second-line agents like TPO-RAs or rituximab.
- It is not a preferred treatment for patients with severe refractory ITP and recurrent bleeding.
Platelet disorders US Medical PG Question 3: A 13-year-old girl is brought to the pediatrician due to a 4-month history of heavy vaginal bleeding during menstrual periods. She endorses episodes of bleeding gums after brushing her teeth and experienced prolonged bleeding after tonsillectomy 6 years ago. Her mother states that she bled significantly during childbirth and that the girl’s older brother has similar symptoms including easy bruising. Vitals were stable and physical exam was not revealing. Laboratory studies show:
Platelet count: 72,000/mm^3
Bleeding time: 14 min
Prothrombin time: 12 secs (INR = 1)
Partial thromboplastin time: 40 secs
Blood smear demonstrates increased megakaryocytes and enlarged platelets. Platelets do not aggregate to ristocetin. Which of the following is the most likely diagnosis?
- A. Glanzmann thrombasthenia
- B. Idiopathic thrombocytopenic purpura (ITP)
- C. Bernard-Soulier syndrome (Correct Answer)
- D. Aspirin or NSAID use
- E. von Willebrand disease (vWD)
Platelet disorders Explanation: ***Bernard-Soulier syndrome***
- The patient presents with **thrombocytopenia** (platelet count 72,000/mm^3), **prolonged bleeding time** (14 min), and **enlarged platelets** and **megakaryocytes** on blood smear.
- The key diagnostic feature is the **failure of platelets to aggregate to ristocetin**, indicating a defect in the GPIb-IX-V receptor complex which mediates platelet adhesion to von Willebrand factor. This clinical picture in a patient with a family history of bleeding is classic for Bernard-Soulier syndrome.
*Glanzmann thrombasthenia*
- This condition is characterized by a defect in the **GPIIb/IIIa receptor**, which is crucial for platelet aggregation; however, patients with Glanzmann thrombasthenia typically have a **normal platelet count** and **normal platelet morphology**.
- Platelets in Glanzmann thrombasthenia would fail to aggregate to ADP, collagen, and epinephrine, but aggregation to **ristocetin** would generally be normal (unless very high concentrations are used), making it less likely given the specific finding of failed ristocetin aggregation and thrombocytopenia.
*Idiopathic thrombocytopenic purpura (ITP)*
- ITP causes isolated **thrombocytopenia** (low platelet count) and **increased megakaryocytes** in the bone marrow, but platelets are typically of **normal size** or may be **larger than normal** but not giant platelets.
- While ITP would cause a prolonged bleeding time, it would not typically show **enlarged platelets** on blood smear, nor would the platelets specifically fail to aggregate to ristocetin due to a receptor defect.
*Aspirin or NSAID use*
- Aspirin and NSAIDs inhibit **cyclooxygenase**, leading to impaired platelet aggregation and a **prolonged bleeding time**, but they do not cause **thrombocytopenia** or changes in **platelet morphology** like enlarged platelets or increased megakaryocytes.
- Platelet aggregation to ristocetin would be normal in the context of aspirin or NSAID use, as the GP Ib-IX-V and GP IIb/IIIa complexes are unaffected.
*von Willebrand disease (vWD)*
- vWD involves a deficiency or defect in **von Willebrand factor**, leading to impaired platelet adhesion and sometimes reduced factor VIII levels, which causes a **prolonged bleeding time**; however, platelet count and morphology are typically **normal**.
- While vWD can show decreased ristocetin-induced platelet aggregation, it does **not present with thrombocytopenia** or **enlarged platelets/megakaryocytes** as seen in this patient.
Platelet disorders US Medical PG Question 4: A 23-year-old woman presents to the emergency department with a 3-day history of fever and headache. She says that the symptoms started suddenly after she woke up 3 days ago, though she has been feeling increasingly fatigued over the last 5 months. On presentation, her temperature is 102°F (38.9°C), blood pressure is 117/74 mmHg, pulse is 106/min, and respirations are 14/min. Physical exam reveals diffuse petechiae and conjunctival pallor and selected laboratory results are shown as follows:
Bleeding time: 11 minutes
Platelet count: 68,000/mm^3
Lactate dehydrogenase: 105 U/L
Which of the following would also most likely be true for this patient?
- A. Increased serum von Willebrand factor multimers (Correct Answer)
- B. Large platelets on peripheral blood smear
- C. Immune production of anti-platelet antibodies
- D. Decreased platelet aggregation on platelet function studies
- E. Increased prothrombin time and partial thromboplastin time
Platelet disorders Explanation: ***Increased serum von Willebrand factor multimers***
- This patient's presentation with **fever**, **thrombocytopenia** (platelet count 68,000/mm^3), **fatigue**, and **petechiae** suggests **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is characterized by a deficiency of **ADAMTS13**, which normally cleaves large **von Willebrand factor (vWF) multimers**. Without ADAMTS13 activity, these large multimers accumulate, leading to widespread platelet adhesion and microthrombi formation.
*Large platelets on peripheral blood smear*
- The presence of **large platelets** (macrocytosis) on a peripheral blood smear is typically associated with conditions where platelet production is increased or dysplastic, such as in **Immune Thrombocytopenic Purpura (ITP)** or myelodysplastic syndromes.
- In TTP, platelets are consumed rapidly in the microvasculature, and the morphology of remaining platelets isn't typically characterized by uniformly large size, although some megakaryocyte fragments might be seen.
*Immune production of anti-platelet antibodies*
- **Immune Thrombocytopenic Purpura (ITP)** is characterized by the production of autoantibodies against platelets, leading to their destruction.
- While ITP can cause thrombocytopenia and petechiae, the presence of **fever** and the systemic nature of symptoms (fatigue, potential renal/neurological involvement not explicitly ruled out) in this case point more strongly towards TTP.
*Decreased platelet aggregation on peripheral blood smear*
- Platelet aggregation tests evaluate platelet function. While there is a functional defect leading to microthrombi in TTP, the problem is related to inappropriate activation by large vWF multimers, not an inherent inability of platelets to aggregate in response to standard stimuli in vitro.
- **Decreased platelet aggregation** is more characteristic of intrinsic platelet disorders or the effect of antiplatelet medications.
*Increased prothrombin time and partial thromboplastin time*
- **Activated partial thromboplastin time (aPTT)** and **prothrombin time (PT)** measure the integrity of the coagulation cascade.
- In TTP, the primary defect is in platelet adhesion and aggregation due to vWF abnormalities, not in the coagulation cascade. Therefore, these coagulation times are typically **normal** in TTP, distinguishing it from conditions like **Disseminated Intravascular Coagulation (DIC)**.
Platelet disorders US Medical PG Question 5: A 3-year-old girl is brought to her pediatrician because of a nosebleed that will not stop. Her parents say that she started having a nosebleed about 1 hour prior to presentation. Since then they have not been able to stop the bleeding. Her past medical history is remarkable for asthma, and she has a cousin who has been diagnosed with hemophilia. Physical exam reveals diffuse petechiae and purpura. A panel of bleeding tests are obtained with the following results:
Bleeding time: 11 minutes
Prothrombin time: 14 seconds
Partial thromboplastin time: 32 seconds
Platelet count: 195,000/mm^3
Peripheral blood smear shows normal cell morphology. Which of the following characteristics is most likely true about this patient?
- A. Mutation in glycoprotein IIb/IIIa (Correct Answer)
- B. Mutation in glycoprotein Ib
- C. Production of anti platelet antibodies
- D. Production of antibodies against ADAMTS13
- E. Decreased levels of von Willebrand factor
Platelet disorders Explanation: ***Mutation in glycoprotein IIb/IIIa***
- The patient's symptoms (nosebleed, petechiae, purpura) and laboratory findings (prolonged **bleeding time**, normal platelet count, normal PT/PTT) are characteristic of **Glanzmann's thrombasthenia**, which is caused by a qualitative defect in **glycoprotein IIb/IIIa**.
- **Glycoprotein IIb/IIIa** is crucial for platelet aggregation, and a mutation in this protein prevents platelets from forming a stable clot.
*Mutation in glycoprotein Ib*
- A mutation in **glycoprotein Ib** leads to **Bernard-Soulier syndrome**, characterized by prolonged bleeding time, normal platelet count, and **abnormally large platelets** on peripheral smear, which are not seen here.
- Glycoprotein Ib is involved in platelet adhesion to von Willebrand factor, not aggregation.
*Production of anti platelet antibodies*
- This describes **Immune Thrombocytopenic Purpura (ITP)**, which would typically present with a **low platelet count**, not a normal count as seen in this patient.
- While ITP can cause petechiae and bleeding, the normal platelet count rules it out.
*Production of antibodies against ADAMTS13*
- This condition is **Thrombotic Thrombocytopenic Purpura (TTP)**, characterized by a **low platelet count**, microangiopathic hemolytic anemia, renal failure, neurological symptoms, and fever, none of which fully align with this patient's presentation.
- TTP usually has significant **thrombocytopenia** and normal bleeding time, despite symptoms of bleeding.
*Decreased levels of von Willebrand factor*
- **Von Willebrand disease (vWD)** would typically show a **prolonged bleeding time** and, depending on the type, may also have a prolonged PTT (due to low factor VIII).
- However, the diffuse petechiae and purpura with a normal platelet count and normal PT/PTT point more strongly towards a platelet function defect rather than a primary coagulation factor deficiency or vWD.
Platelet disorders US Medical PG Question 6: A 47-year-old woman presents for a routine wellness checkup. She complains of general fatigue and lethargy for the past 6 months. She does not have a significant past medical history and is currently not taking any medications. The patient reports that she drinks “socially” approx. 6 nights a week. She says she also enjoys a “nightcap,” which is 1–2 glasses of wine before bed every night. She denies any history of drug use or smoking. The patient is afebrile, and her vital signs are within normal limits. A physical examination reveals pallor of the mucous membranes. Her laboratory findings are significant for a mean corpuscular volume of 72 fL, leukocyte count of 5,300/mL, hemoglobin of 11.0 g/dL, and platelet count of 420,000/mL.
Which of the following is the most likely cause of this patient’s thrombocytosis?
- A. Iron deficiency anemia (Correct Answer)
- B. Essential thrombocytosis
- C. Aplastic anemia
- D. Chronic alcohol abuse
- E. Chronic myelogenous leukemia (CML)
Platelet disorders Explanation: ***Iron deficiency anemia***
- The patient presents with **microcytic anemia** (MCV 72 fL, Hb 11.0 g/dL) and **pallor**, which are classic signs of iron deficiency.
- **Iron deficiency** is a common cause of **secondary thrombocytosis**, as iron plays a role in platelet production and maturation.
*Essential thrombocytosis*
- This is a **myeloproliferative neoplasm** characterized by significantly elevated platelet counts, usually much higher than 420,000/mL (often > 600,000/mL).
- While it causes thrombocytosis, it typically doesn't present with microcytic anemia unless there's a co-existing iron deficiency, which is the primary finding here.
*Aplastic anemia*
- **Aplastic anemia** would present with **pancytopenia** (low red blood cells, white blood cells, and platelets), which is not consistent with the patient's elevated platelet count and normal leukocyte count.
- The patient's presentation of fatigue and pallor would likely be more severe due to significant anemia, and thrombocytosis would not be present.
*Chronic alcohol abuse*
- **Chronic alcohol abuse** typically causes **macrocytic anemia** (elevated MCV) due to folate deficiency or direct bone marrow toxicity, not microcytic anemia.
- While it can sometimes lead to thrombocytopenia, it is not a direct cause of robust thrombocytosis, especially in the context of microcytic anemia.
*Chronic myelogenous leukemia (CML)*
- CML is a **myeloproliferative neoplasm** characterized by the **Philadelphia chromosome (BCR-ABL1 fusion gene)**, leading to a significant increase in **granulocytes** (leukocytosis) and often thrombocytosis.
- Although thrombocytosis can occur, the primary hallmark is significant leukocytosis, which is not seen here (leukocyte count is normal), and the anemia would typically be normocytic or even macrocytic if folate deficient.
Platelet disorders US Medical PG Question 7: A previously healthy 38-year-old woman is brought to the emergency department by her husband because of left-sided weakness. As she was getting dressed this morning, she was suddenly unable to button up her shirt. When she showed her husband, he noticed that she seemed confused. She has a 3-year history of diabetes mellitus, for which she takes metformin. She had a knee operation 2 days ago. Her temperature is 38.9°C (102°F), pulse is 98/min, respirations are 17/min, and blood pressure is 138/85 mm Hg. She is confused and oriented only to person. Neurologic examination shows diminished muscle strength on the left side. There are scattered petechiae over the chest, arms, and legs. Laboratory studies show:
Hemoglobin 7.5 g/dL
Leukocyte count 10,500/mm3
Platelet count 40,000/mm3
Prothrombin time 15 seconds
Partial thromboplastin time 36 seconds
Serum
Bilirubin
Total 3.5 mg/dL
Direct 0.3 mg/dL
Urea nitrogen 35 mg/dL
Creatinine 2.5 mg/dL
Lactate dehydrogenase 1074 U/L
A peripheral smear shows numerous schistocytes. Further evaluation is most likely going to show which of the following findings?
- A. Decreased ADAMTS13 activity in serum (Correct Answer)
- B. Enterohemorrhagic Escherichia coli on stool culture
- C. Elevated fibrin degradation products in serum
- D. Decreased megakaryocytes on bone marrow biopsy
- E. Positive direct Coombs test
Platelet disorders Explanation: **Decreased ADAMTS13 activity in serum**
- The patient's presentation with **neurological symptoms (confusion, left-sided weakness)**, **renal dysfunction (elevated BUN and creatinine)**, **thrombocytopenia (platelet count 40,000/mm³)**, **microangiopathic hemolytic anemia (schistocytes on smear, high LDH, low hemoglobin, elevated bilirubin)**, and **fever** constitutes the classic pentad of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is characterized by a severe deficiency (<10%) in **ADAMTS13 activity**, a metalloprotease responsible for cleaving large multimers of von Willebrand factor, leading to widespread platelet adhesion and microthrombi formation.
*Enterohemorrhagic Escherichia coli on stool culture*
- This is characteristic of **hemolytic-uremic syndrome (HUS)**, which typically presents with microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury, often following a diarrheal illness.
- However, the prominent neurological symptoms and absence of preceding diarrhea in this case make HUS less likely than TTP, though both fall under the umbrella of thrombotic microangiopathies.
*Elevated fibrin degradation products in serum*
- Elevated **fibrin degradation products (FDPs)** and **D-dimers** are hallmarks of **Disseminated Intravascular Coagulation (DIC)**, which involves systemic activation of coagulation leading to widespread microthrombi and consumption of clotting factors and platelets.
- While thrombocytopenia and schistocytes can be seen in DIC, the constellation of prominent neurological findings and severe ADAMTS13 deficiency points more specifically to TTP, and the normal PT/PTT values make DIC less probable as they are typically prolonged in DIC due to consumption of clotting factors.
*Decreased megakaryocytes on bone marrow biopsy*
- A decrease in megakaryocytes would indicate a problem with platelet production in the bone marrow, as seen in **aplastic anemia** or other bone marrow failures.
- In TTP, thrombocytopenia is due to increased peripheral consumption of platelets in thrombi, not decreased production; thus, megakaryocytes in the bone marrow would typically be normal or increased in response to the low platelet count.
*Positive direct Coombs test*
- A positive **direct Coombs test** indicates the presence of antibodies or complement on the surface of red blood cells, which is characteristic of **autoimmune hemolytic anemia**.
- While hemolytic anemia is present, the associated thrombocytopenia, neurological symptoms, and renal dysfunction, along with schistocytes, are not typical features of autoimmune hemolytic anemia in isolation.
Platelet disorders US Medical PG Question 8: A previously healthy 40-year-old woman comes to the physician because of a 3-day history of fever, headaches, and fatigue. She also reports a persistent tingling sensation in her right hand and numbness in her right arm that started this morning. Physical examination shows pallor, mild scleral icterus, and petechiae on her forearms and legs. On mental status examination, she appears confused and is only oriented to person. Laboratory studies show:
Hemoglobin 11.1 g/dL
Platelet count 39,500/mm3
Bleeding time 9 minutes
Prothrombin time 14 seconds
Partial thromboplastin time 35 seconds
Serum
Creatinine 1.7 mg/dL
Total bilirubin 2.1 mg/dL
A peripheral blood smear shows fragmented erythrocytes. Which of the following is the most likely underlying cause of this patient's condition?
- A. Antibodies against double-stranded DNA
- B. Mutation of the PIGA gene
- C. Antibodies against GpIIb/IIIa
- D. Antibodies against ADAMTS13 (Correct Answer)
- E. Absence of platelet GpIIb/IIIa receptors
Platelet disorders Explanation: ***Antibodies against ADAMTS13***
- This patient presents with a classic pentad of symptoms: **fever**, **neurologic symptoms** (confusion, tingling, numbness), **renal failure** (creatinine 1.7 mg/dL), **thrombocytopenia** (platelet count 39,500/mm3), and **microangiopathic hemolytic anemia** (pallor, scleral icterus, fragmented erythrocytes on smear). This constellation of findings is highly suggestive of **Thrombotic Thrombocytopenic Purpura (TTP)**.
- TTP is primarily caused by a deficiency of the **ADAMTS13 enzyme**, often due to **autoantibodies** that inhibit its activity. ADAMTS13 is responsible for cleaving large **von Willebrand factor (vWF) multimers**, and its deficiency leads to the accumulation of these large multimers, promoting platelet aggregation and microthrombi formation.
*Antibodies against double-stranded DNA*
- Antibodies against double-stranded DNA (**anti-dsDNA antibodies**) are characteristic of **Systemic Lupus Erythematosus (SLE)**, which can present with various systemic symptoms.
- While SLE can cause thrombocytopenia and renal involvement, it typically does not cause the severe **microangiopathic hemolytic anemia** with schistocytes or the combination of symptoms seen in this patient to the extent of TTP.
*Mutation of the PIGA gene*
- A **mutation of the *PIGA* gene** is responsible for **Paroxysmal Nocturnal Hemoglobinuria (PNH)**, a clonal stem cell disorder characterized by hemolytic anemia, thrombosis, and bone marrow failure.
- While PNH involves hemolysis, it typically lacks the prominent neurological symptoms, severe thrombocytopenia with microangiopathic features, and renal failure seen in TTP.
*Antibodies against GpIIb/IIIa*
- **Antibodies against GpIIb/IIIa** (glycoprotein IIb/IIIa) receptors are the hallmark of **Immune Thrombocytopenic Purpura (ITP)**, causing accelerated platelet destruction.
- ITP primarily causes **isolated thrombocytopenia** and mucocutaneous bleeding, but it does not cause microangiopathic hemolytic anemia, renal failure, or neurological symptoms that are prominent in this patient.
*Absence of platelet GpIIb/IIIa receptors*
- The **absence of platelet GpIIb/IIIa receptors** is characteristic of **Glanzmann's thrombasthenia**, a rare inherited disorder of platelet function.
- Glanzmann's thrombasthenia leads to **mucocutaneous bleeding** due to impaired platelet aggregation, but it does not cause thrombocytopenia, hemolytic anemia, renal failure, or neurological symptoms.
Platelet disorders US Medical PG Question 9: A mother brings her 6-year-old daughter in to the pediatrician’s clinic for a wellness visit. The mother has a history of von Willebrand’s disease (vWD) and is concerned that her daughter may be affected as well. The mother tells you that she has noticed that her daughter bruises very easily, and her bruises typically are visible for a longer period of time than those of her brother. She denies any personal history of blood clots in her past, but she says that her mother has had to be treated for pulmonary embolism in the recent past. Her birth history is significant for preeclampsia, preterm birth at 32 weeks, a NICU stay of two and a half weeks, and retinopathy of prematurity. She currently eats a diet full of green vegetables, fruits, and french fries. Her vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 106/54 mm Hg; heart rate, 111/min; and respiratory, rate 23/min. On physical examination, her pulses are bounding, complexion is pale, scattered bruises throughout all extremities that are specifically scattered around the knees and elbows. After ordering a coagulation panel, which of the following would one expect to see in the lab panel of a patient with vWD?
- A. Elevated platelet count
- B. Prolonged PT
- C. Normal bleeding time
- D. Decreased factor IX
- E. Prolonged PTT (Correct Answer)
Platelet disorders Explanation: ***Prolonged PTT***
- **Von Willebrand factor (vWF)** stabilizes **Factor VIII**, and in vWD, reduced vWF levels lead to lower Factor VIII activity, which is reflected as a **prolonged PTT**.
- The coagulation cascade components associated with PTT (intrinsic and common pathways) are affected due to the impaired function or deficiency of vWF.
*Elevated platelet count*
- **Platelet count** is typically **normal** in vWD, as the disorder primarily affects platelet function and adhesion, not platelet production.
- Thrombocytosis is not characteristic of vWD and would suggest other primary hematologic conditions.
*Prolonged PT*
- The **prothrombin time (PT)** measures the extrinsic and common pathways of coagulation, which are typically **unaffected** in vWD.
- PT prolongation would suggest deficiencies in factors VII, X, V, or prothrombin.
*Normal bleeding time*
- **Bleeding time** is typically **prolonged** in vWD because vWF is crucial for platelet adhesion to the subendothelium and platelet plug formation.
- A normal bleeding time would argue against a platelet function disorder like vWD.
*Decreased factor IX*
- **Factor IX** deficiency is associated with **Hemophilia B**, a separate X-linked coagulopathy, and is not directly affected in vWD.
- While vWD involves coagulation factor deficiencies, the primary factor stabilized by vWF is Factor VIII, not Factor IX.
Platelet disorders US Medical PG Question 10: A 12-year-old boy, otherwise healthy, presents with frequent nosebleeds and lower extremity bruising. His mother reports that his symptoms started about 2 weeks ago and have not improved. The patient received the Tdap vaccine 2 weeks ago. He has no current medications. The review of systems is significant for the patient having a stomach ache after winning a hamburger eating competition 2 weeks ago. The vital signs include: temperature 37.0°C (98.6°F), blood pressure 110/75 mm Hg, pulse 95/min, respirations 15/min, and oxygen saturation 99% on room air. On physical exam, the patient is alert and cooperative. The cardiac exam is normal. The lungs are clear to auscultation bilaterally. The lower extremities findings are shown in the image. Laboratory results are pending. Which of the following best describes the pathogenesis of this patient’s condition?
- A. Shiga-toxin mediated damage to vascular endothelium, resulting in microthrombi formation
- B. Systemic activation of clotting cascade resulting in platelet and coagulation factor consumption
- C. IgG autoantibodies against platelet glycoproteins (Correct Answer)
- D. Deposition of IgA immune complexes
- E. Deficiency of ADAMTS13
Platelet disorders Explanation: ***IgG autoantibodies against platelet glycoproteins***
- The patient's symptoms of **nosebleeds** and **bruising** (petechiae/purpura on lower extremities) following a recent **infection/illness** (stomach ache) and/or **vaccination** (Tdap) are highly suggestive of **immune thrombocytopenia (ITP)**.
- ITP involves the production of **autoantibodies**, usually IgG, that target **platelet glycoproteins** (e.g., GP IIb/IIIa), leading to accelerated platelet destruction by macrophages in the spleen.
*Shiga-toxin mediated damage to vascular endothelium, resulting in microthrombi formation*
- This describes the pathogenesis of **hemolytic uremic syndrome (HUS)**, typically caused by E. coli O157:H7 infection, leading to **thrombocytopenia**, microangiopathic hemolytic anemia, and acute kidney injury.
- While the patient had a stomach ache, there's no mention of **bloody diarrhea**, renal symptoms, or anemia to suggest HUS.
*Systemic activation of clotting cascade resulting in platelet and coagulation factor consumption*
- This describes **disseminated intravascular coagulation (DIC)**, a severe condition characterized by widespread activation of the coagulation system, leading to both **thrombosis** and bleeding.
- DIC is usually associated with severe underlying conditions like **sepsis**, trauma, or malignancy, and would typically present with more systemic involvement and deranged coagulation studies, which are not described.
*Deposition of IgA immune complexes*
- This is characteristic of **IgA vasculitis (Henoch-Schönlein purpura)**, which presents with a classic tetrad of **palpable purpura**, arthritis/arthralgia, abdominal pain, and renal disease.
- While the patient has lower extremity bruising and a history of abdominal pain, the absence of **palpable purpura** and systemic features like arthritis or renal involvement makes IgA vasculitis less likely than ITP given the prominent bleeding symptoms.
*Deficiency of ADAMTS13*
- A deficiency in **ADAMTS13** (a metalloprotease that cleaves vWF multimers) is the hallmark of **thrombotic thrombocytopenic purpura (TTP)**.
- TTP presents with the classic pentad of **thrombocytopenia**, microangiopathic hemolytic anemia, renal failure, neurological symptoms, and fever, none of which are fully described in this patient.
More Platelet disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.