Plasma cell disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Plasma cell disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Plasma cell disorders US Medical PG Question 1: A 72-year-old African American man presents with progressive fatigue, difficulty breathing on exertion, and lower extremity swelling for 3 months. The patient was seen at the emergency department 2 times before. The first time was because of back pain, and the second was because of fever and cough. He took medications at the emergency room, but he refused to do further tests recommended to him. He does not smoke or drink alcohol. His family history is irrelevant. His vital signs include a blood pressure of 110/80 mm Hg, temperature of 37.2°C (98.9°F), and regular radial pulse of 90/min. On physical examination, the patient looks pale, and his tongue is enlarged. Jugular veins become distended on inspiration. Pitting ankle edema is present on both sides. Bilateral basal crackles are audible on the chest auscultation. Hepatomegaly is present on abdominal palpation. Chest X-ray shows osteolytic lesions of the ribs. ECG shows low voltage waves and echocardiogram shows a speckled appearance of the myocardium with diastolic dysfunction and normal appearance of the pericardium. Which of the following best describes the mechanism of this patient’s illness?
- A. Thickening of the parietal pericardium with dystrophic calcification
- B. Calcification of the aortic valve orifice with obstruction of the left ventricular outflow tract
- C. Concentric hypertrophy of the myocytes with thickening of the interventricular septum
- D. Diastolic cardiac dysfunction with reciprocal variation in ventricular filling with respiration
- E. Deposition of an extracellular fibrillar protein that stains positive for Congo red in the myocardium (Correct Answer)
Plasma cell disorders Explanation: - ***Deposition of an extracellular fibrillar protein that stains positive for Congo red in the myocardium***
- The patient's presentation with **progressive fatigue, dyspnea, edema, enlarged tongue, jugular venous distention with inspiration** (Kussmaul's sign), **basal crackles, hepatomegaly, osteolytic lesions, low voltage on ECG, and a speckled appearance of the myocardium on echocardiogram with diastolic dysfunction** is highly suggestive of **amyloidosis**.
- **Amyloidosis** involves the deposition of misfolded, insoluble **fibrillar proteins** in various tissues, including the heart, leading to restrictive cardiomyopathy. These amyloid deposits typically stain **positive with Congo red** and demonstrate **apple-green birefringence** under polarized light.
- *Thickening of the parietal pericardium with dystrophic calcification*
- This description is characteristic of **constrictive pericarditis**, which can cause symptoms similar to restrictive cardiomyopathy (e.g., Kussmaul's sign, edema).
- However, the echocardiogram in this patient shows a **speckled appearance of the myocardium** and a **normal pericardium**, ruling out constrictive pericarditis.
- *Calcification of the aortic valve orifice with obstruction of the left ventricular outflow tract*
- This describes **aortic stenosis**, which would lead to signs of left ventricular outflow obstruction, such as a systolic murmur and possibly left ventricular hypertrophy.
- While it can cause dyspnea and fatigue, it does not typically explain the **speckled myocardium**, **enlarged tongue**, or **osteolytic lesions** seen in this patient.
- *Concentric hypertrophy of the myocytes with thickening of the interventricular septum*
- This is characteristic of **hypertensive heart disease** or **hypertrophic cardiomyopathy**.
- While these conditions can cause diastolic dysfunction, they typically do not present with **osteolytic lesions**, **enlarged tongue**, or the **speckled appearance of the myocardium** on echocardiography that is seen in amyloidosis.
- *Diastolic cardiac dysfunction with reciprocal variation in ventricular filling with respiration*
- While **diastolic cardiac dysfunction** is present, this option is too general and describes a physiological consequence rather than the underlying mechanism for the constellation of symptoms.
- **Reciprocal variation in ventricular filling with respiration** can be seen in both restrictive cardiomyopathy and constrictive pericarditis but does not explain the specific findings of **osteolytic lesions** or **enlarged tongue**, which point towards a systemic infiltrative disease like amyloidosis.
Plasma cell disorders US Medical PG Question 2: A 61-year-old woman presents to her primary care physician for a routine check-up. Physical examination demonstrates asymmetric peripheral neuropathy in her feet. The patient has no previous relevant history and denies any symptoms of diabetes. Routine blood work shows normal results, and she is referred to a hematologist. Subsequent serum protein electrophoresis demonstrates a slightly elevated gamma globulin level, and monoclonal gammopathy of undetermined significance is diagnosed. Which of the following diseases is most likely to develop over the course of this patient’s condition?
- A. Acute myelocytic leukemia
- B. Chronic myelocytic leukemia
- C. Multiple myeloma (Correct Answer)
- D. Waldenström macroglobulinemia
- E. Chronic lymphocytic leukemia
Plasma cell disorders Explanation: ***Multiple myeloma***
- This patient has **monoclonal gammopathy of undetermined significance (MGUS)**, confirmed by the asymmetric peripheral neuropathy, elevated gamma globulin, and monoclonal gammopathy. MGUS has a 1% annual risk of progressing to **multiple myeloma**.
- **Peripheral neuropathy** is a common initial presentation of MGUS, and its progression to multiple myeloma involves the proliferation of **plasma cells** in the bone marrow, leading to end-organ damage.
*Acute myelocytic leukemia*
- This is a **myeloid malignancy** characterized by rapid proliferation of abnormal myeloid blasts in the bone marrow, not typically preceded by MGUS or presenting with peripheral neuropathy.
- It usually presents with symptoms like **fatigue**, **bleeding**, and **infections**, unrelated to the monoclonal gammopathy.
*Chronic myelocytic leukemia*
- This is a **myeloproliferative disorder** associated with the **Philadelphia chromosome (BCR-ABL1 fusion gene)**, which is distinct from conditions involving plasma cell dyscrasias like MGUS.
- It classically presents with **splenomegaly** and a high white blood cell count with a myeloid shift.
*Waldenström macroglobulinemia*
- This is a **lymphoplasmacytic lymphoma** involving IgM monoclonal gammopathy, which can cause neuropathy similar to MGUS. However, MGUS with IgG or IgA is more common and has a higher progression risk to multiple myeloma than to Waldenström macroglobulinemia.
- While it involves **monoclonal gammopathy**, the clinical picture of MGUS with its specific progression risk profile is more indicative of eventual multiple myeloma.
*Chronic lymphocytic leukemia*
- This is a **lymphoid malignancy** characterized by the accumulation of mature but functionally incompetent lymphocytes, particularly B-cells.
- It is not typically preceded by MGUS and usually presents with **lymphadenopathy**, **splenomegaly**, and **lymphocytosis**.
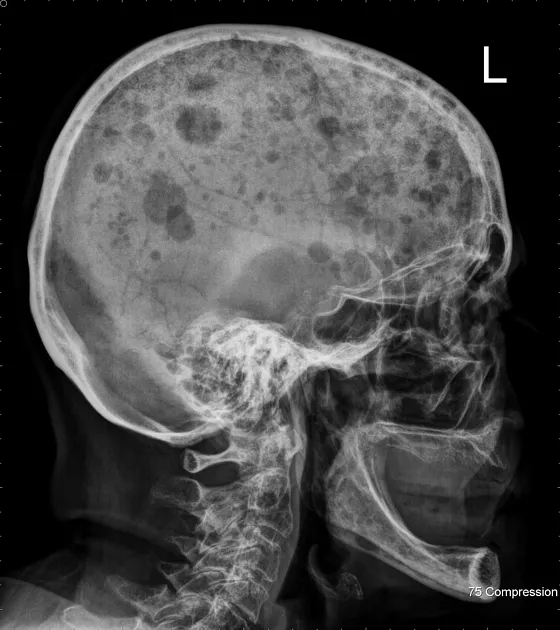
Plasma cell disorders US Medical PG Question 3: A 70-year-old man comes to the physician because of progressive fatigue and lower back pain for the past 4 months. The back pain worsened significantly after he had a minor fall while doing yard work the previous day. For the past year, he has had a feeling of incomplete emptying of his bladder after voiding. His vital signs are within normal limits. Examination shows bilateral paravertebral muscle spasm, severe tenderness over the second lumbar vertebra, and mild tenderness over the lower thoracic vertebrae. Neurologic examination shows no abnormalities. His hemoglobin is 10.5 g/dl, alkaline phosphatase is 110 U/L, and serum calcium is 11.1 mg/dl. An x-ray of the skull is shown. Which of the following is the most appropriate next step in diagnosis?
- A. Bone marrow biopsy
- B. Bone scan
- C. Serum vitamin D levels
- D. Prostate biopsy
- E. Serum protein electrophoresis (Correct Answer)
Plasma cell disorders Explanation: ***Serum protein electrophoresis***
- The patient's symptoms (fatigue, back pain with minor fall causing vertebral tenderness), laboratory findings (**anemia**, **hypercalcemia**), and especially the skull X-ray showing **numerous lytic lesions** (also known as "punched-out" lesions) are highly suggestive of **multiple myeloma**.
- **Serum protein electrophoresis** (SPEP) is the most appropriate next step as it is crucial for identifying and quantifying the **monoclonal protein (M-spike)** produced by plasma cells, which is diagnostic for multiple myeloma.
*Bone marrow biopsy*
- While a bone marrow biopsy is used to confirm the diagnosis of multiple myeloma by identifying **clonal plasma cells**, it is typically done after initial screening tests like SPEP strongly suggest the diagnosis.
- SPEP is a less invasive and often the first definitive diagnostic step before proceeding to bone marrow biopsy.
*Bone scan*
- **Bone scans (technetium-99m scintigraphy)** are generally not useful for detecting the purely **lytic lesions** characteristic of multiple myeloma, as these lesions do not involve increased osteoblastic activity (bone formation) which is necessary for tracer uptake.
- X-rays and MRI are more effective for visualizing lytic lesions in multiple myeloma.
*Serum vitamin D levels*
- While vitamin D levels are important for bone health, measuring them is not a primary diagnostic step in a suspected case of multiple myeloma.
- The patient's symptoms and signs point strongly towards a neoplastic process, not a primary vitamin D deficiency.
*Prostate biopsy*
- The patient's age and urinary symptoms (incomplete bladder emptying) could raise suspicion for **prostatic enlargement** (benign prostatic hyperplasia or prostate cancer). However, the prominent lytic bone lesions, hypercalcemia, and anemia point more definitively towards a systemic hematologic malignancy like multiple myeloma rather than metastatic prostate cancer.
- While prostate cancer can cause blastic bone metastases, the X-ray shows classic lytic lesions, which are less typical of prostate cancer metastases and more characteristic of multiple myeloma.
Plasma cell disorders US Medical PG Question 4: A 61-year-old man presents to the emergency department with new-onset dizziness. He reports associated symptoms of confusion, headaches, and loss of coordination. The patient’s wife also mentions he has had recent frequent nosebleeds. Physical examination demonstrates a double vision. Routine blood work is significant for a slightly reduced platelet count. A noncontrast CT of the head is normal. A serum protein electrophoresis is performed and shows an elevated IgM spike. The consulting hematologist strongly suspects Waldenström’s macroglobulinemia. Which of the following is the best course of treatment for this patient?
- A. Plasmapheresis (Correct Answer)
- B. Vincristine
- C. Cyclophosphamide
- D. Rituximab
- E. Prednisone
Plasma cell disorders Explanation: ***Plasmapheresis***
- This patient presents with symptoms of **hyperviscosity syndrome** (dizziness, confusion, headaches, loss of coordination, double vision, nosebleeds) due to high levels of IgM, which is characteristic of Waldenström's macroglobulinemia.
- **Plasmapheresis** is the most effective initial treatment to rapidly reduce the IgM level and relieve these acute neurological and hemorrhagic symptoms by removing the excess globulins from the plasma.
*Vincristine*
- **Vincristine** is a chemotherapy agent used in the treatment of Waldenström's macroglobulinemia, but it is typically used as part of a multi-drug regimen for long-term disease control, not for acute management of hyperviscosity.
- Its mechanism involves inhibiting microtubule formation, which is a slower process and would not provide immediate relief for the crisis.
*Cyclophosphamide*
- **Cyclophosphamide** is an alkylating agent, often part of chemotherapy regimens for Waldenström's macroglobulinemia, especially for long-term disease control to reduce IgM production.
- Like vincristine, it works by damaging DNA in cancer cells, a process that is too slow to address the immediate, life-threatening symptoms of hyperviscosity syndrome.
*Rituximab*
- **Rituximab** is an anti-CD20 monoclonal antibody that targets B-cells, often used in Waldenström's macroglobulinemia to reduce the malignant B-cell clone and subsequent IgM production.
- While effective for disease control, its therapeutic effects take weeks to materialize and would not provide rapid relief for acute hyperviscosity.
*Prednisone*
- **Prednisone** is a corticosteroid that can be used in some hematologic malignancies to reduce inflammation or induce apoptosis in certain cell types.
- However, in Waldenström's macroglobulinemia, corticosteroids alone are not effective in rapidly reducing the large IgM burden causing hyperviscosity, and their role is often supportive or part of combination chemotherapy.
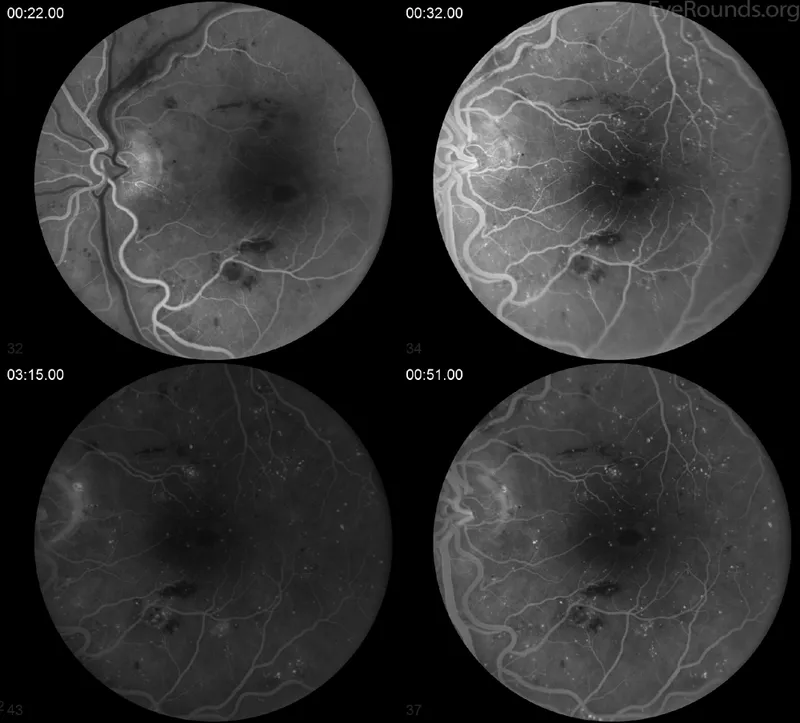
Plasma cell disorders US Medical PG Question 5: A 69-year-old woman comes to the physician because of a 3-week history of headache and worsening vision. Ophthalmologic examination shows a visual acuity of 20/120 in the right eye and 20/80 in the left eye. Physical examination shows no other abnormalities. Laboratory studies show a hemoglobin of 14.2 g/dL and total serum calcium of 9.9 mg/dL. A photomicrograph of a peripheral blood smear is shown. Serum electrophoresis shows increased concentration of a pentameric immunoglobulin. Which of the following is the most likely diagnosis?
- A. Multiple myeloma
- B. Hyper IgM syndrome
- C. Waldenstrom macroglobulinemia (Correct Answer)
- D. Essential thrombocythemia
- E. Giant cell arteritis
Plasma cell disorders Explanation: ***Waldenstrom macroglobulinemia***
- This condition is characterized by the overproduction of **monoclonal IgM** (a pentameric immunoglobulin), which can lead to **hyperviscosity syndrome**.
- Symptoms like **headache** and **worsening vision** in an elderly patient, combined with increased IgM, are classic presentations of hyperviscosity associated with Waldenstrom macroglobulinemia.
*Multiple myeloma*
- This plasma cell disorder typically involves the overproduction of **IgG or IgA**, not IgM.
- While it can cause headaches and vision problems, it's often accompanied by **bone pain**, **hypercalcemia**, **renal failure**, and recurrent infections, which are not described here.
*Hyper IgM syndrome*
- This is a rare **primary immunodeficiency** characterized by normal or increased IgM levels but decreased levels of IgG, IgA, and IgE, leading to recurrent infections.
- It usually presents in childhood and is not associated with the **hyperviscosity symptoms** seen in this patient.
*Essential thrombocythemia*
- This is a **myeloproliferative neoplasm** characterized by an elevated platelet count, which increases the risk of thrombosis or hemorrhage.
- It does not involve immunoglobulin overproduction or present with symptoms indicative of **hyperviscosity syndrome**.
*Giant cell arteritis*
- This condition is an **inflammatory vasculitis** that can cause headache and vision loss, similar to the patient's symptoms.
- However, it is typically associated with an **elevated erythrocyte sedimentation rate (ESR)** and C-reactive protein, and would not show increased pentameric immunoglobulin on serum electrophoresis.
Plasma cell disorders US Medical PG Question 6: A 73-year-old man comes to the physician because of progressive fatigue and shortness of breath on exertion for 3 weeks. He has swelling of his legs. He has not had nausea or vomiting. His symptoms began shortly after he returned from a trip to Cambodia. He occasionally takes ibuprofen for chronic back pain. He has a history of arterial hypertension and osteoarthritis of both knees. He had an episode of pneumonia 4 months ago. His current medications include lisinopril and hydrochlorothiazide. He has no history of drinking or smoking. His temperature is 37°C (98.6°F), pulse is 101/min, and blood pressure is 135/76 mm Hg. Examination shows pitting edema of the upper and lower extremities. Laboratory studies show:
Hemoglobin 14.1 g/dL
Leukocyte count 6,800/mm3
Platelet count 216,000/mm3
Serum
Urea nitrogen 26 mg/dL
Creatinine 2.9 mg/dL
Albumin 1.6 g/dL
Urine
Blood negative
Protein 4+
Glucose negative
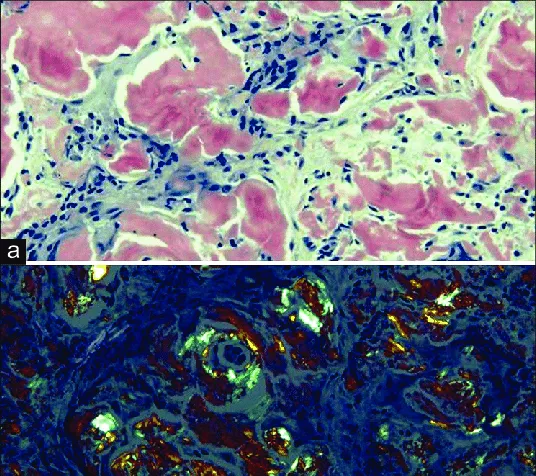
Renal biopsy with Congo red stain shows apple-green birefringence under polarized light. Further evaluation of this patient is most likely to show which of the following findings?
- A. Positive interferon-γ release assay
- B. Dilated bronchi on chest CT
- C. Elevated anti-citrullinated peptide antibodies
- D. Positive HLA-B27 test
- E. Rouleaux formation on peripheral smear (Correct Answer)
Plasma cell disorders Explanation: ***Rouleaux formation on peripheral smear***
- The renal biopsy showing **apple-green birefringence** with Congo red stain is pathognomonic for **amyloidosis**.
- The clinical presentation of **nephrotic syndrome** (massive proteinuria, hypoalbuminemia, edema) with renal amyloidosis in an elderly patient is most commonly due to **AL (light chain) amyloidosis** caused by plasma cell dyscrasia.
- AL amyloidosis is associated with **monoclonal gammopathy** which causes increased serum protein viscosity, leading to **rouleaux formation** (stacking of RBCs like coins) on peripheral blood smear.
- Further workup would typically show serum/urine protein electrophoresis with monoclonal protein and possibly bone marrow plasmacytosis.
*Positive interferon-γ release assay*
- This test diagnoses **latent or active tuberculosis**.
- While TB can cause **AA (secondary) amyloidosis** through chronic inflammation, and the patient traveled to an endemic area, the renal-limited presentation without active systemic infection makes AL amyloidosis more likely.
- AA amyloidosis typically presents with chronic inflammatory conditions lasting months to years.
*Dilated bronchi on chest CT*
- **Bronchiectasis** causes chronic inflammation and can lead to **AA amyloidosis**.
- However, a single episode of pneumonia 4 months ago is insufficient to cause the chronic inflammation needed for AA amyloidosis.
- This finding would not directly relate to the amyloid deposition causing current symptoms.
*Elevated anti-citrullinated peptide antibodies*
- These antibodies are highly specific for **rheumatoid arthritis**, which can cause AA amyloidosis.
- However, the patient has **osteoarthritis** (degenerative joint disease), not inflammatory arthritis.
- There are no clinical features suggesting RA (no joint inflammation, no morning stiffness).
*Positive HLA-B27 test*
- **HLA-B27** is associated with **seronegative spondyloarthropathies** which can rarely cause AA amyloidosis.
- The patient's back pain is attributed to chronic mechanical issues, not inflammatory spondyloarthropathy.
- This finding is unrelated to the renal amyloidosis presentation.
Plasma cell disorders US Medical PG Question 7: A 67-year-old man presents to the emergency department with altered mental status. The patient is non-verbal at baseline, but his caretakers at the nursing home noticed he was particularly somnolent recently. The patient has a past medical history of diabetes and Alzheimer dementia. His temperature is 99.7°F (37.6°C), blood pressure is 157/98 mmHg, pulse is 150/min, respirations are 16/min, and oxygen saturation is 98% on room air. Laboratory values are obtained and shown below.
Hemoglobin: 9 g/dL
Hematocrit: 33%
Leukocyte count: 8,500/mm^3 with normal differential
Platelet count: 197,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 102 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 37 mg/dL
Glucose: 99 mg/dL
Creatinine: 2.4 mg/dL
Ca2+: 12.2 mg/dL
The patient has lost 20 pounds over the past month. His parathyroid hormone is within normal limits, and his urinary calcium is increased. Physical exam demonstrates discomfort when the patient's lower back and extremities are palpated. Which of the following is the most accurate diagnostic test for this patient's underlying diagnosis?
- A. Peripheral blood smear
- B. Urine protein levels
- C. Bone marrow biopsy (Correct Answer)
- D. Radiograph of the lumbar spine
- E. Urine, blood, and cerebrospinal fluid cultures
Plasma cell disorders Explanation: **Bone marrow biopsy**
- The patient presents with **hypercalcemia**, **elevated creatinine** (acute kidney injury), **anemia**, **weight loss**, and bony pain, which are classic features of **multiple myeloma**; a bone marrow biopsy is crucial for diagnosis and staging by identifying plasma cell infiltration.
- Identification of > **10% clonal plasma cells** in the bone marrow confirms the diagnosis of multiple myeloma in patients with myeloma-defining events (e.g., hypercalcemia, renal failure, anemia, bone lesions).
*Peripheral blood smear*
- While a peripheral blood smear might show **rouleaux formation** in multiple myeloma due to increased plasma proteins, it is not specific or diagnostic as rouleaux can be seen in other conditions like inflammation.
- It does not quantify the percentage of **clonal plasma cells**, which is essential for diagnosing multiple myeloma.
*Urine protein levels*
- **Urine protein electrophoresis (UPEP)** and **immunofixation** are important for detecting Bence-Jones proteinuria (clonal free light chains) which supports the diagnosis of multiple myeloma, but quantifying general urine protein levels (e.g., with a 24-hour collection) is not as specific or diagnostic.
- While **elevated urine protein** is expected in multiple myeloma due to light chain excretion, it doesn't provide definitive evidence of plasma cell dyscrasia or bone marrow involvement.
*Radiograph of the lumbar spine*
- **Skeletal surveys** (including radiographs) are used to identify **lytic bone lesions** characteristic of multiple myeloma, which contribute to pain and hypercalcemia.
- Although important for identifying bone involvement, radiographs are not the most accurate diagnostic test for the underlying disease itself, as they do not directly evaluate the presence of **clonal plasma cells**.
*Urine, blood, and cerebrospinal fluid cultures*
- These cultures are primarily used to diagnose **infections**, which can cause altered mental status and fever.
- While infection is a consideration, the constellation of hypercalcemia, renal failure, anemia, and bone pain points strongly toward multiple myeloma, making cultures less likely to reveal the primary underlying diagnosis.
Plasma cell disorders US Medical PG Question 8: A 60-year-old woman comes to the physician because of lower back pain, generalized weakness, and weight loss that has occurred over the past 6 weeks. She also says that her urine has appeared foamy recently. Physical examination shows focal midline tenderness of the lumbar spine and conjunctival pallor. Her temperature is 100.5°F (38°C). A photomicrograph of a bone marrow biopsy specimen is shown. Further evaluation of this patient is most likely to show which of the following findings?
- A. Myeloblasts with needle-shaped cytoplasmic inclusions
- B. Erythrocytes with cytoplasmic hemoglobin inclusions
- C. Neutrophils with hypersegmented nuclear lobes
- D. Grouped erythrocytes with stacked-coin appearance (Correct Answer)
- E. B-lymphocytes with radial cytoplasmic projections
Plasma cell disorders Explanation: ***Grouped erythrocytes with stacked-coin appearance***
- The patient's presentation of **lower back pain** (lytic bone lesions), **foamy urine** (proteinuria from Bence Jones proteins), **weight loss**, and **fever** strongly suggests **multiple myeloma**.
- Bone marrow biopsy would show **increased plasma cells**, and further evaluation with **peripheral blood smear** would reveal **rouleaux formation** (stacked-coin appearance of RBCs).
- Rouleaux formation occurs due to **increased serum proteins** (M-protein/paraprotein) that decrease the negative charge between erythrocytes, causing them to stack.
- This finding, combined with **anemia** (conjunctival pallor) and **hypercalcemia** symptoms, is characteristic of multiple myeloma.
*Myeloblasts with needle-shaped cytoplasmic inclusions*
- This describes **Auer rods**, which are pathognomonic for **acute myeloid leukemia (AML)**.
- AML typically presents with **bleeding**, **infections**, and **pancytopenia**, rather than bone pain and foamy urine.
- The patient's clinical picture points to a **plasma cell dyscrasia**, not myeloid leukemia.
*Erythrocytes with cytoplasmic hemoglobin inclusions*
- This finding (Howell-Jolly bodies, Heinz bodies, or other inclusions) suggests **hemolytic anemia**, **thalassemia**, or **asplenia**.
- These conditions do not explain the **bone pain**, **proteinuria**, or **plasma cell proliferation** seen in this case.
- The patient's symptoms are better explained by **multiple myeloma**, not hemoglobinopathy.
*Neutrophils with hypersegmented nuclear lobes*
- Hypersegmented neutrophils (≥5 lobes) are characteristic of **megaloblastic anemia** due to **vitamin B12** or **folate deficiency**.
- While this could cause weakness and anemia, it does not explain the **bone pain**, **fever**, **foamy urine**, or **lumbar spine tenderness**.
- The complete clinical picture is consistent with **multiple myeloma**, not nutritional deficiency.
*B-lymphocytes with radial cytoplasmic projections*
- This describes **hairy cell leukemia**, a rare B-cell neoplasm with characteristic "hairy" projections.
- Hairy cell leukemia presents with **splenomegaly** and **pancytopenia**, not the bone lesions and proteinuria seen here.
- The patient's presentation aligns with **plasma cell myeloma**, not B-cell lymphoproliferative disorder.
Plasma cell disorders US Medical PG Question 9: A 62-year-old retired professor comes to the clinic with the complaints of back pain and increasing fatigue over the last 4 months. For the past week, his back pain seems to have worsened. It radiates to his legs and is burning in nature, 6/10 in intensity. There is no associated tingling sensation. He has lost 4.0 kg (8.8 lb) in the past 2 months. There is no history of trauma. He has hypertension which is well controlled with medications. Physical examination is normal. Laboratory studies show normocytic normochromic anemia. Serum calcium is 12.2 mg/dL and Serum total proteins is 8.8 gm/dL. A serum protein electrophoresis shows a monoclonal spike. X-ray of the spine shows osteolytic lesions over L2–L5 and right femur. A bone marrow biopsy reveals plasmacytosis. Which of the following is the most preferred treatment option?
- A. Renal dialysis
- B. Palliative care
- C. Chemotherapy and autologous stem cell transplant (Correct Answer)
- D. Bisphosphonates
- E. Chemotherapy alone
Plasma cell disorders Explanation: ***Chemotherapy and autologous stem cell transplant***
- This patient presents with classic features of **multiple myeloma**, including bone pain with osteolytic lesions, hypercalcemia, normocytic anemia, elevated total protein with a monoclonal spike, and plasmacytosis in the bone marrow.
- In a relatively healthy patient with newly diagnosed multiple myeloma who is fit for intensive therapy (as suggested by the absence of significant comorbidities beyond controlled hypertension), **chemotherapy followed by autologous stem cell transplant (ASCT)** is the preferred treatment to achieve deeper and more durable remission.
*Renal dialysis*
- While **renal impairment** can occur in multiple myeloma due to myeloma kidney, it is not described in this patient, and **dialysis** is a supportive measure for end-stage kidney disease, not the primary treatment for the underlying malignancy.
- The patient's symptoms are primarily related to bone involvement and systemic effects of myeloma, not severe renal failure.
*Palliative care*
- **Palliative care** focuses on symptom relief and quality of life, which is essential at any stage of a serious illness, but it is not the initial primary therapeutic intervention for a newly diagnosed, symptomatic, and treatable cancer like multiple myeloma in a patient who could benefit from curative or remission-inducing therapy.
- The goal at this stage is disease control and prolonging survival.
*Bisphosphonates*
- **Bisphosphonates** (e.g., zoledronic acid) are an important adjunctive therapy in multiple myeloma to manage and prevent **skeletal-related events** by inhibiting osteoclast activity, but they do not treat the underlying plasma cell malignancy itself.
- They would be used in conjunction with chemotherapy, not as a standalone primary treatment.
*Chemotherapy alone*
- While **chemotherapy** (often a combination of proteasome inhibitors, immunomodulatory drugs, and dexamethasone) is central to treating multiple myeloma, **chemotherapy alone** without subsequent ASCT is typically reserved for patients who are not candidates for transplantation due to age, comorbidities, or frailty.
- For transplant-eligible patients, ASCT after induction chemotherapy significantly improves progression-free survival and overall survival compared to chemotherapy alone.
Plasma cell disorders US Medical PG Question 10: A previously healthy 68-year-old woman is brought to the emergency department because of a 3-day history of nausea, anorexia, polyuria, and confusion. Her only medication is acetaminophen, which she takes daily for back pain that started 6 weeks ago. Physical examination shows conjunctival pallor. She is oriented to person but not to time or place. Laboratory studies show a hemoglobin concentration of 9.3 g/dL, a serum calcium concentration of 13.8 mg/dL, and a serum creatinine concentration of 2.1 mg/dL. Her erythrocyte sedimentation rate is 65 mm/h. Which of the following is the most likely underlying cause of this patient's condition?
- A. Overproliferation of plasma cells (Correct Answer)
- B. Decreased renal excretion of calcium
- C. Excessive intake of calcium
- D. Ectopic release of PTHrP
- E. Excess PTH secretion from parathyroid glands
Plasma cell disorders Explanation: ***Overproliferation of plasma cells***
- The patient's symptoms (nausea, anorexia, polyuria, confusion, back pain, anemia, hypercalcemia, acute kidney injury, and elevated ESR) are classic features of **multiple myeloma** (CRAB — Calcium elevation, Renal insufficiency, Anemia, Bone lesions).
- Multiple myeloma is characterized by the **malignant proliferation of plasma cells** in the bone marrow, leading to skeletal destruction (causing back pain and hypercalcemia), renal damage, and anemia.
*Decreased renal excretion of calcium*
- While **renal insufficiency** (creatinine 2.1 mg/dL) contributes to hypercalcemia by impairing calcium excretion, it is typically a **consequence** of the underlying disease rather than the primary cause of hypercalcemia, especially with such a high calcium level.
- The elevated calcium itself can worsen kidney function, creating a **vicious cycle**, but an underlying cause for hypercalcemia is still needed.
*Excessive intake of calcium*
- This typically occurs with **calcium and vitamin D supplementation** (milk-alkali syndrome) and is not suggested by the patient's history, as her only medication is acetaminophen.
- Her current symptoms are too severe and multi-systemic to be explained solely by dietary calcium excess without other contributing factors.
*Ectopic release of PTHrP*
- **Parathyroid hormone-related peptide (PTHrP)** is secreted by various solid tumors (e.g., squamous cell carcinoma of the lung, renal cell carcinoma) and causes humoral hypercalcemia of malignancy.
- While it causes hypercalcemia, the prominent **bone pain and anemia** in this patient are more characteristic of multiple myeloma than a solid tumor secreting PTHrP.
*Excess PTH secretion from parathyroid glands*
- This describes **primary hyperparathyroidism**, which causes hypercalcemia and can lead to bone pain and renal stones.
- However, primary hyperparathyroidism is typically associated with **normal or elevated PTH levels**, and it does not usually cause the degree of anemia or elevated ESR seen in this case.
More Plasma cell disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.