Non-Hodgkin lymphomas US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Non-Hodgkin lymphomas. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Non-Hodgkin lymphomas US Medical PG Question 1: A 69-year-old Caucasian man presents for a routine health maintenance examination. He feels well. He has no significant past medical history. He takes aspirin for the occasional headaches that he has had for over several years. He exercises every day and does not smoke. His father was diagnosed with a hematologic malignancy at 79 years old. The patient’s vital signs are within normal limits. Physical examination shows no abnormalities. The laboratory test results are as follows:
Hemoglobin 14.5 g/dL
Leukocyte count 62,000/mm3
Platelet count 350,000/mm3
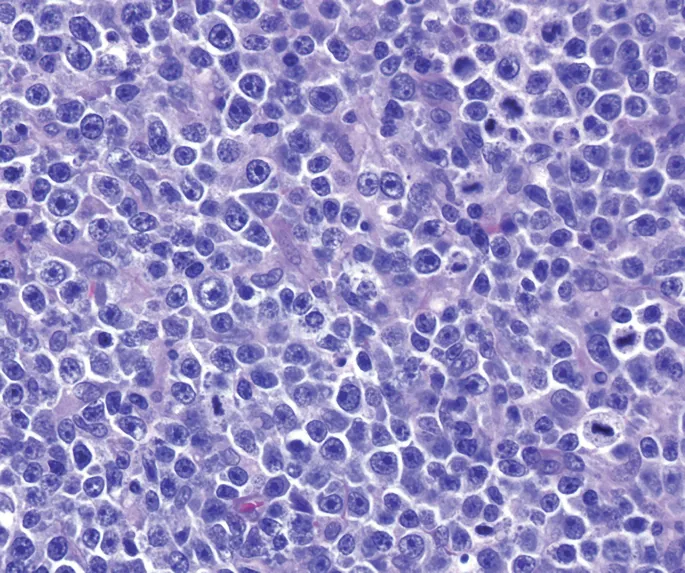
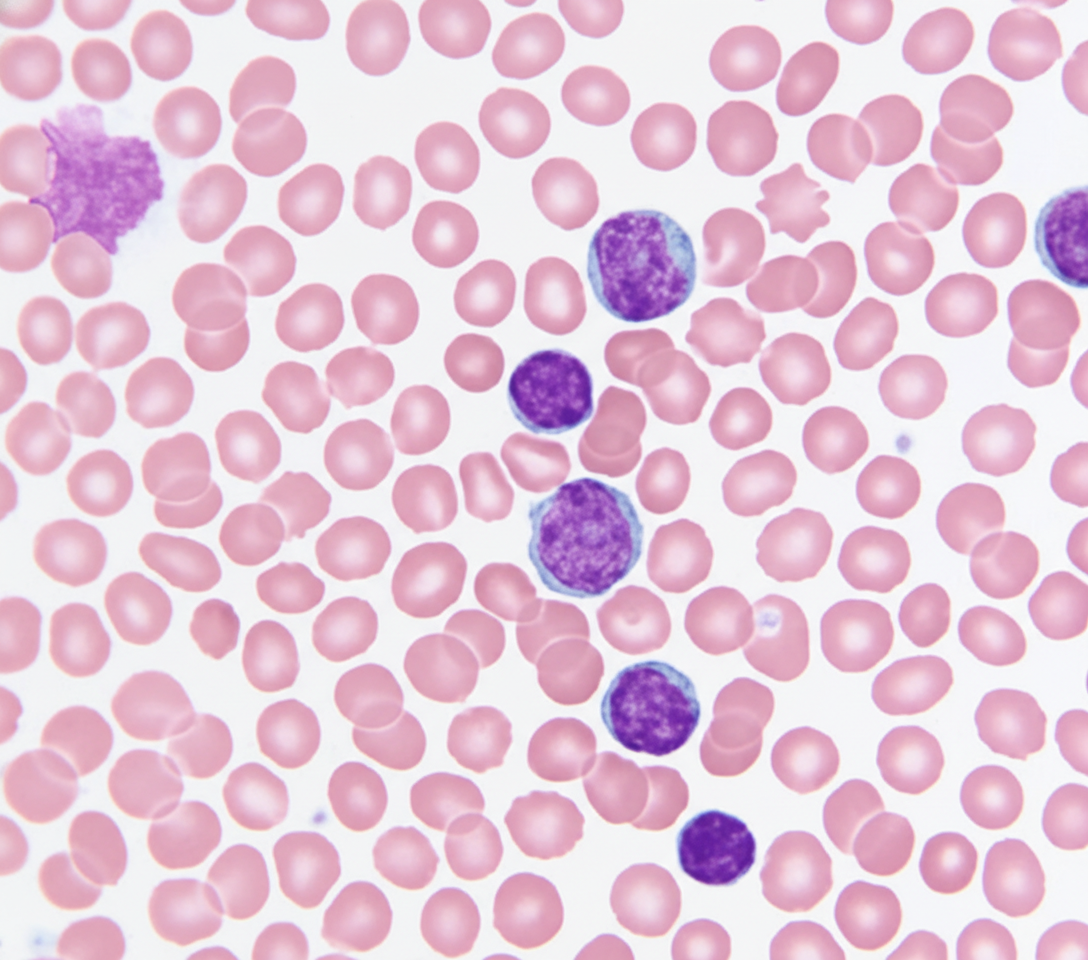
A peripheral blood smear is obtained (shown on the image). Which of the following best explains these findings?
- A. Acute lymphoid leukemia
- B. Hairy cell leukemia
- C. Adult T cell leukemia
- D. Chronic lymphocytic leukemia (Correct Answer)
- E. Acute myeloid leukemia
Non-Hodgkin lymphomas Explanation: ***Chronic lymphocytic leukemia***
- The image displays characteristic **smudge cells** (also known as **basket cells**) and mature-looking lymphocytes with scant cytoplasm and condensed chromatin, which are hallmarks of CLL.
- The patient's age (69 years), elevated leukocyte count (62,000/mm³), and the presence of these particular cells on peripheral smear in an otherwise asymptomatic individual are all highly suggestive of CLL.
*Acute lymphoid leukemia*
- This condition is characterized by a proliferation of **blasts** (immature lymphocytes) in the bone marrow and peripheral blood, which are not depicted in the provided image.
- While it can present with a high leukocyte count, the cellular morphology would show a predominance of immature cells rather than the mature-appearing lymphocytes and smudge cells seen here.
*Hairy cell leukemia*
- This leukemia is characterized by lymphocytes with **fine cytoplasmic projections** (hairy cells) and typically leads to **pancytopenia**, particularly leukopenia, rather than the marked leukocytosis seen in this patient.
- The morphology in the image does not show these cytoplasmic projections.
*Adult T cell leukemia*
- This form of leukemia is caused by the **human T-lymphotropic virus type 1 (HTLV-1)** and is more prevalent in specific endemic regions (e.g., Japan, Caribbean).
- It usually presents with **atypical pleomorphic T-cells** with convoluted nuclei, often accompanied by skin lesions, hypercalcemia, and lymphadenopathy, none of which are mentioned or depicted.
*Acute myeloid leukemia*
- AML is characterized by an overgrowth of **myeloblasts** (immature myeloid cells) in the bone marrow and peripheral blood, often containing **Auer rods**.
- The cells in the image are clearly lymphoid in origin and do not show features of myeloblasts or Auer rods.
Non-Hodgkin lymphomas US Medical PG Question 2: A 55-year-old man presents with severe fatigue and fever. His past medical history is significant for a recent history of mononucleosis from which he fully recovered 8 weeks ago. On physical examination, the patient seems pale. A chest radiograph shows multiple enlarged mediastinal lymph nodes. A biopsy of one of the enlarged mediastinal lymph nodes is performed and shows the presence of multinucleated cells with an 'owl-eye' appearance in a hypocellular background. Which of the following is the most likely diagnosis in this patient?
- A. Extranodal marginal zone lymphoma
- B. Classical Hodgkin lymphoma (Correct Answer)
- C. Diffuse large B cell lymphoma
- D. Nodular lymphocyte-predominant lymphoma
- E. Follicular lymphoma
Non-Hodgkin lymphomas Explanation: ***Classical Hodgkin lymphoma***
- The presence of **Reed-Sternberg cells** with their characteristic **'owl-eye' appearance** in a hypocellular background is pathognomonic for **Classical Hodgkin lymphoma**.
- The patient's presentation with **fatigue**, **fever**, **pale appearance**, and **enlarged mediastinal lymph nodes** is highly suggestive of this diagnosis, particularly given the recent **mononucleosis**, which is associated with Epstein-Barr virus (EBV) and can precede Hodgkin lymphoma development.
*Extranodal marginal zone lymphoma*
- This lymphoma typically arises in **mucosa-associated lymphoid tissue (MALT)**, often in the stomach in association with *H. pylori* infection.
- It is characterized by **small B cells** and **lymphoplasmacytic differentiation**, not Reed-Sternberg cells.
*Diffuse large B cell lymphoma*
- This is an **aggressive non-Hodgkin lymphoma** characterized by a proliferation of **large B cells**.
- While it can present with B symptoms and lymphadenopathy, the presence of **Reed-Sternberg cells** on biopsy rules out DLBCL.
*Nodular lymphocyte-predominant lymphoma*
- This is a rare type of Hodgkin lymphoma characterized by **lymphocyte-predominant (LP) cells** (popcorn cells), which are different from the classic Reed-Sternberg cells.
- It typically presents with **peripheral lymphadenopathy** and has a more indolent course than classical Hodgkin lymphoma.
*Follicular lymphoma*
- Follicular lymphoma is an **indolent non-Hodgkin lymphoma** characterized by a **follicular growth pattern** and composed of centrocytes and centroblasts.
- It does not feature the **Reed-Sternberg cells** with an 'owl-eye' appearance.
Non-Hodgkin lymphomas US Medical PG Question 3: A medical research study is beginning to evaluate the positive predictive value of a novel blood test for non-Hodgkin’s lymphoma. The diagnostic arm contains 700 patients with NHL, of which 400 tested positive for the novel blood test. In the control arm, 700 age-matched control patients are enrolled and 0 are found positive for the novel test. What is the PPV of this test?
- A. 400 / (400 + 0) (Correct Answer)
- B. 700 / (700 + 300)
- C. 400 / (400 + 300)
- D. 700 / (700 + 0)
- E. 700 / (400 + 400)
Non-Hodgkin lymphomas Explanation: ***400 / (400 + 0) = 1.0 or 100%***
- The **positive predictive value (PPV)** is calculated as **True Positives / (True Positives + False Positives)**.
- In this scenario, **True Positives (TP)** are the 400 patients with NHL who tested positive, and **False Positives (FP)** are 0, as no control patients tested positive.
- This gives a PPV of 400/400 = **1.0 or 100%**, indicating that all patients who tested positive actually had the disease.
*700 / (700 + 300)*
- This calculation does not align with the formula for PPV based on the given data.
- The denominator `(700+300)` suggests an incorrect combination of various patient groups.
*400 / (400 + 300)*
- The denominator `(400+300)` incorrectly includes 300, which is the number of **False Negatives** (patients with NHL who tested negative), not False Positives.
- PPV focuses on the proportion of true positives among all positive tests, not all diseased individuals.
*700 / (700 + 0)*
- This calculation incorrectly uses the total number of patients with NHL (700) as the numerator, rather than the number of positive test results in that group.
- The numerator should be the **True Positives** (400), not the total number of diseased individuals.
*700 / (400 + 400)*
- This calculation uses incorrect values for both the numerator and denominator, not corresponding to the PPV formula.
- The numerator 700 represents the total number of patients with the disease, not those who tested positive, and the denominator incorrectly sums up values that don't represent the proper PPV calculation.
Non-Hodgkin lymphomas US Medical PG Question 4: A 29-year-old man comes to the physician because of a 3-month history of fatigue, weight loss, and multiple painless swellings on his neck and axilla. He reports that his swellings become painful after he drinks alcohol. Physical examination shows nontender cervical and axillary lymphadenopathy. A lymph node biopsy specimen shows giant binucleate cells. Which of the following is the most likely diagnosis?
- A. Diffuse large B-cell lymphoma
- B. Acute retroviral syndrome
- C. Hodgkin lymphoma (Correct Answer)
- D. Acute lymphocytic leukemia
- E. Adult T-cell lymphoma
Non-Hodgkin lymphomas Explanation: ***Hodgkin lymphoma***
- The presence of **fatigue, weight loss, and painless lymphadenopathy** (B symptoms) in a young man is highly suggestive of Hodgkin lymphoma.
- The **lymph node biopsy showing giant binucleate cells** (Reed-Sternberg cells) is pathognomonic for Hodgkin lymphoma, and **alcohol-induced lymph node pain** is a classic, though uncommon, symptom.
*Diffuse large B-cell lymphoma*
- This is an **aggressive non-Hodgkin lymphoma** that can present with rapidly enlarging lymph nodes and B symptoms.
- However, the characteristic **Reed-Sternberg cells** found on biopsy are not seen in diffuse large B-cell lymphoma.
*Acute retroviral syndrome*
- This syndrome typically presents with **flu-like symptoms, fever, sore throat, and generalized lymphadenopathy** within weeks of HIV infection.
- It is usually **self-limiting** and does not feature the specific histopathology of giant binucleate cells on lymph node biopsy.
*Acute lymphocytic leukemia*
- This is a **hematologic malignancy** characterized by the proliferation of immature lymphoid cells.
- It often presents with symptoms of **bone marrow failure** (anemia, bleeding, infections) and can have lymphadenopathy, but the diagnostic lymph node biopsy features are not consistent with Reed-Sternberg cells.
*Adult T-cell lymphoma*
- This rare lymphoma is associated with **human T-lymphotropic virus type 1 (HTLV-1) infection** and is more common in endemic regions.
- It can present with lymphadenopathy, skin lesions, and hypercalcemia, but the histopathology would show **pleomorphic T-cells**, not Reed-Sternberg cells.
Non-Hodgkin lymphomas US Medical PG Question 5: A 65-year-old man presents with painless swelling of the neck over the past week. He also has noted severe night sweats, which require a change of clothes and bed linens the next day. His medical history is significant for long-standing hypertension. He received a kidney transplant 6 years ago. His current medications include amlodipine, metoprolol, furosemide, aspirin, tacrolimus, and mycophenolate. His family history is significant for his sister, who died last year from lymphoma. A review of systems is positive for a 6-kg (13.2-lb) unintentional weight loss over the past 2 months. His vital signs include: temperature 37.8°C (100.0°F) and blood pressure 120/75 mm Hg. On physical examination, there are multiple painless lymph nodes, averaging 2 cm in diameter, palpable in the anterior and posterior triangles of the neck bilaterally. Axillary and inguinal lymphadenopathy is palpated on the right side. Abdominal examination is significant for a spleen of 16 cm below the costal margin on percussion. Laboratory studies are significant for the following:
Hemoglobin 9 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 12,000/mm3
Platelet count 130,000/mm3
Creatinine 1.1 mg/dL
Lactate dehydrogenase (LDH) 1,000 U/L
A peripheral blood smear is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Multiple myeloma
- B. Non-Hodgkin’s lymphoma (NHL) (Correct Answer)
- C. Drug-induced lymphadenopathy
- D. Chronic lymphocytic leukemia (CLL)
- E. Cytomegalovirus infection
Non-Hodgkin lymphomas Explanation: ***Non-Hodgkin’s lymphoma (NHL)***
- This patient presents with **B symptoms** (**unintentional weight loss**, **night sweats**, fever), diffuse **lymphadenopathy**, and **splenomegaly**, which are classic signs of lymphoma. Elevated **LDH** and a history of kidney transplant requiring immunosuppression (tacrolimus, mycophenolate) significantly increase the risk of **post-transplant lymphoproliferative disorder (PTLD)**, a type of NHL.
- The **anemia**, **thrombocytopenia**, and **leukocytosis** (with an otherwise unremarkable peripheral smear) are consistent with bone marrow involvement or chronic disease in lymphoma.
*Multiple myeloma*
- Multiple myeloma is a plasma cell dyscrasia characterized by **bone pain**, **renal failure**, **hypercalcemia**, and **anemia**. While anemia and potential renal impairment are present, the widespread lymphadenopathy and splenomegaly are not typical features.
- The elevated LDH and presence of B symptoms are more indicative of lymphoma than multiple myeloma.
*Drug-induced lymphadenopathy*
- While some medications can cause lymphadenopathy, it is typically less severe, often without systemic B symptoms, and usually resolves upon discontinuation of the causative drug.
- The combination of severe B symptoms, impressive splenomegaly, and significantly elevated LDH points to a more aggressive underlying malignancy rather than a drug reaction.
*Chronic lymphocytic leukemia (CLL)*
- CLL is characterized by a persistent **lymphocytosis** (often >5,000 mature lymphocytes/µL) on peripheral smear, which is not described here ("unremarkable").
- While CLL can cause lymphadenopathy and splenomegaly, the rapid onset of severe B symptoms and the extremely high LDH are more suggestive of an aggressive lymphoma rather than indolent CLL.
*Cytomegalovirus infection*
- CMV infection can cause lymphadenopathy, fever, and fatigue, particularly in immunocompromised patients. However, the degree of **weight loss**, **splenomegaly**, and elevated **LDH** seen here are uncharacteristic of CMV infection and point towards a more serious underlying malignancy.
- CMV typically presents with a more acute, mononucleosis-like illness and often lymphocytosis with atypical lymphocytes on peripheral smear.
Non-Hodgkin lymphomas US Medical PG Question 6: A 7-year-old boy presents to his primary care physician for a general checkup. The patient has been feeling poorly for the past several weeks and has been losing weight. He states that he often feels weak and too tired to play with his friends. He is no longer interested in many recreational activities he used to be interested in. The patient's parents state that a few of their child's friends have been sick lately. His temperature is 102°F (38.9°C), blood pressure is 77/48 mmHg, pulse is 110/min, respirations are 24/min, and oxygen saturation is 98% on room air. On exam, you note a fatigued appearing child who has lost 10 pounds since his last appointment. Left upper quadrant tenderness and a mass is noted on abdominal exam. Which of the following best describes the most likely diagnosis?
- A. Smudge cells on peripheral smear
- B. TdT positive cells (Correct Answer)
- C. Infection sensitive to oseltamivir
- D. Auer rods on peripheral smear
- E. Parental mistreatment of the child
Non-Hodgkin lymphomas Explanation: ***TdT positive cells***
- This patient's symptoms, including **fever**, **weight loss**, **fatigue**, and **splenomegaly** (left upper quadrant tenderness and mass), are highly suggestive of **Acute Lymphoblastic Leukemia (ALL)**.
- **Terminal deoxynucleotidyl transferase (TdT)** is a DNA polymerase found in immature lymphocytes (blasts) and is a key marker for diagnosing ALL.
- ALL is the **most common childhood malignancy**, particularly prevalent in children aged 2-10 years.
*Smudge cells on peripheral smear*
- **Smudge cells** are characteristic of **Chronic Lymphocytic Leukemia (CLL)**, which predominantly affects older adults and is rare in children.
- The clinical picture of rapid decline and significant systemic symptoms in a child is inconsistent with CLL.
*Infection sensitive to oseltamivir*
- Oseltamivir is an **antiviral medication for influenza**, and while the child has a fever, the profound **weight loss**, **fatigue**, and **abdominal mass** point towards a hematologic malignancy, not a typical viral infection.
- Viral infections rarely present with such a significant abdominal mass or sustained constitutional symptoms for several weeks.
*Auer rods on peripheral smear*
- **Auer rods** are cytoplasmic inclusions pathognomonic for **Acute Myeloid Leukemia (AML)**.
- While AML can occur in children, **ALL is far more common in this age group** (85% of childhood leukemias), and the presentation is highly classic for ALL, making TdT positivity the best diagnostic marker.
*Parental mistreatment of the child*
- While some symptoms (weight loss, fatigue) could potentially be seen in neglect, the presence of **fever**, **splenomegaly** (abdominal mass), and **hypotension** points strongly to a severe underlying medical condition.
- Objective signs of systemic illness necessitate a thorough medical workup rather than suspicion of abuse.
Non-Hodgkin lymphomas US Medical PG Question 7: An 82-year-old man presents with painless swelling of the neck for the past week. He reports no recent fever, night sweats, or weight loss. He has no significant medical history, and his only medication is daily aspirin. His temperature is 36.8℃ (98.2℉). On physical examination, there are several non-tender lymph nodes, each averaging 2 cm in diameter, which are palpable in the right anterior cervical triangle. No other palpable lymphadenopathy is noted. The remainder of the physical exam is unremarkable. Laboratory studies show the following:
Hemoglobin 10 g/dL
Leukocyte count 8000/mm3 with a normal differential
Platelet count 250,000/mm3
Erythrocyte sedimentation rate
30 mm/h
An excisional biopsy of a cervical lymph node reveals the presence of Reed-Sternberg (RS) cells. Computed tomography (CT) scans and positron emission tomography (PET) scans reveal no mediastinal mass or signs of additional disease. Which of the following aspects most strongly indicates a good prognosis for this patient?
- A. Erythrocyte sedimentation rate (ESR)
- B. Leukocyte count and differential
- C. Absence of B symptoms
- D. Stage of the disease (Correct Answer)
- E. Hemoglobin level
Non-Hodgkin lymphomas Explanation: ***Stage of the disease***
- The **stage of Hodgkin lymphoma** is the most significant prognostic factor, with **earlier stages (I and II)** having a much better prognosis than advanced stages (III and IV). The prompt indicates **no mediastinal mass or additional disease**, suggesting an early stage.
- Absence of widespread disease in CT and PET scans is a critical indicator of **localized disease**, which is associated with higher cure rates.
*Absence of B symptoms*
- While the **absence of B symptoms** (fever, night sweats, weight loss) is a favorable prognostic indicator, it is secondary to the overall disease stage in predicting long-term outcomes in Hodgkin lymphoma.
- The patient's lack of B symptoms is positive, but the *extent of disease spread* (stage) remains the primary determinant of prognosis.
*Erythrocyte sedimentation rate (ESR)*
- An **elevated ESR** (30 mm/h in this case) is a known adverse prognostic factor in Hodgkin lymphoma, indicating systemic inflammation.
- While important, it is a **secondary indicator** and does not outweigh the significance of disease stage in determining prognosis.
*Hemoglobin level*
- A **hemoglobin level below 10.5 g/dL** is an adverse prognostic factor in Hodgkin lymphoma according to the International Prognostic Score, and this patient's hemoglobin is 10 g/dL.
- This factor suggests a potentially **worse prognosis**, making it an incorrect answer for "good prognosis."
*Leukocyte count and differential*
- An **elevated leukocyte count** (above 15,000/mm³) and a **lymphopenia** (absolute lymphocyte count less than 600/mm³ or less than 8% of the white cell count) are adverse prognostic factors in Hodgkin lymphoma.
- This patient has a normal leukocyte count and differential (8000/mm³ with normal differential), which is **neutral to good** but less impactful than the disease stage.
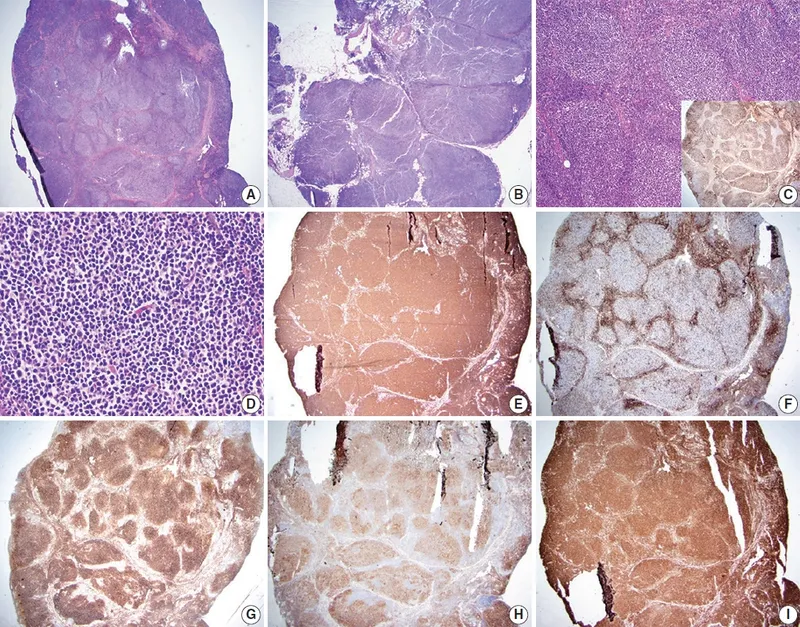
Non-Hodgkin lymphomas US Medical PG Question 8: A 70-year-old man is at his dermatologist’s office for the treatment of a severely pruritic erythroderma with scaling on his buttocks that has been slowly progressing over the past two weeks. The patient works as a truck driver and has a history of hypertension treated with enalapril. The patient reports having tried an over-the-counter cream on the rash without improvement. The vital signs are within normal range. On physical exam, he has multiple confluent and well-demarcated pink patches on his buttocks and legs with some scaling and enlarged inguinal lymph nodes. The dermatologist orders a skin biopsy that reveals Pautrier microabscesses. What is the most likely diagnosis?
- A. Atopic dermatitis
- B. Kaposi sarcoma
- C. Lichen planus
- D. Psoriasis
- E. Mycosis fungoides (Correct Answer)
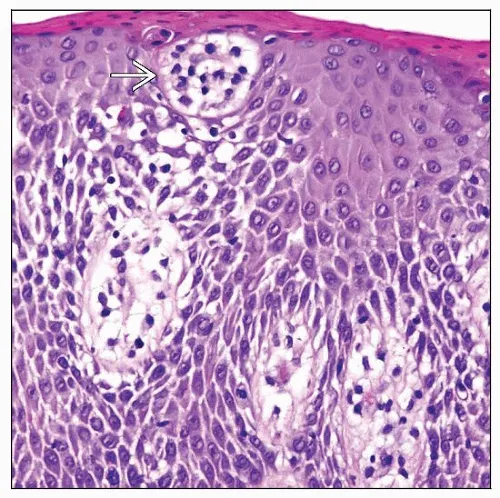
Non-Hodgkin lymphomas Explanation: ***Mycosis fungoides***
- The presence of **severely pruritic erythroderma** with **scaling**, progressing over weeks, and **enlarged regional lymph nodes** is highly suggestive of cutaneous T-cell lymphoma, specifically mycosis fungoides.
- The definitive diagnostic finding is **Pautrier microabscesses** on skin biopsy, which are collections of atypical T lymphocytes in the epidermis, pathognomonic for mycosis fungoides.
*Atopic dermatitis*
- While it can cause **pruritic and scaly erythematous patches**, it typically presents earlier in life, often with a history of allergies or asthma, which are not mentioned.
- **Pautrier microabscesses** are not a feature of atopic dermatitis; histology would show spongiosis and inflammation.
*Kaposi sarcoma*
- This condition presents as **violaceous plaques, patches, or nodules**, often in immunocompromised individuals, and is caused by HHV-8.
- Histologically, it shows **spindle cells** and **vascular proliferation**, not Pautrier microabscesses.
*Lichen planus*
- Characterized by **pruritic, polygonal, planar, purple papules and plaques** (the 6 Ps), often with Wickham's striae.
- Biopsy would reveal a **band-like lymphocytic infiltrate** at the dermoepidermal junction, not Pautrier microabscesses.
*Psoriasis*
- Typically presents as **well-demarcated erythematous plaques with silvery scales**, often on extensor surfaces.
- While it can cause erythroderma, **Pautrier microabscesses** are not characteristic; histology shows **acanthosis**, **parakeratosis**, and **Munro microabscesses** (neutrophils in the stratum corneum).
Non-Hodgkin lymphomas US Medical PG Question 9: A 67-year-old woman comes to the physician because of a 3-week history of fatigue and worsening back and abdominal pain. During this period, she has also had excessive night sweats and a 4.6-kg (10-lb) weight loss. She has had swelling of the neck for 3 days. She does not smoke or drink alcohol. Vital signs are within normal limits. Physical examination shows a 4-cm, supraclavicular, nontender, enlarged and fixed lymph node. The spleen is palpated 2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10.4 g/dL
Mean corpuscular volume 87 μm3
Leukocyte count 5,200/mm3
Platelet count 190,000/mm3
Serum
Lactate dehydrogenase 310 U/L
A CT scan of the thorax and abdomen shows massively enlarged paraaortic, axillary, mediastinal, and cervical lymph nodes. Histopathologic examination of an excised cervical lymph node shows lymphocytes with a high proliferative index that stain positive for CD20. Which of the following is the most likely diagnosis?
- A. Hairy cell leukemia
- B. Adult T-cell lymphoma
- C. Diffuse large B-cell lymphoma (Correct Answer)
- D. Marginal zone lymphoma
- E. Follicular lymphoma
Non-Hodgkin lymphomas Explanation: ***Diffuse large B-cell lymphoma***
- The patient presents with **B symptoms** (fever, night sweats, weight loss), rapid progression, generalized **lymphadenopathy** (cervical, supraclavicular, paraaortic, axillary, mediastinal), **splenomegaly**, and elevated **LDH**.
- **Histopathologic examination** showing lymphocytes with a **high proliferative index** and positive **CD20 staining** confirms a B-cell lymphoma with aggressive features, highly characteristic of DLBCL.
*Hairy cell leukemia*
- This condition typically presents with **splenomegaly** and **pancytopenia**, but **lymphadenopathy** is rare and often absent.
- The characteristic "hairy cells" are identified by specific markers (CD103, CD123, CD25), and a **high proliferative index** is not a feature.
*Adult T-cell lymphoma*
- This lymphoma is associated with **HTLV-1 infection** and often presents with hypercalcemia, skin lesions, and generalized lymphadenopathy, but it is a **T-cell lymphoma**.
- The **CD20 positivity** in the histology rules out a T-cell lineage lymphoma.
*Marginal zone lymphoma*
- This is an **indolent B-cell lymphoma** that typically progresses slowly and is often associated with chronic inflammation or autoimmune diseases.
- The patient's aggressive symptoms, rapid progression, significant **B symptoms**, and **high proliferative index** are not consistent with indolent lymphoma.
*Follicular lymphoma*
- This is also an **indolent B-cell lymphoma** characterized by a follicular growth pattern and usually presents with painless lymphadenopathy.
- The rapid onset of symptoms, significant **B symptoms**, and elevated **LDH** indicate an aggressive lymphoma, which is not typical of follicular lymphoma.
Non-Hodgkin lymphomas US Medical PG Question 10: A 72-year-old man goes to his primary care provider for a checkup after some blood work showed lymphocytosis 3 months ago. He says he has been feeling a bit more tired lately but doesn’t complain of any other symptoms. Past medical history is significant for hypertension and hyperlipidemia. He takes lisinopril, hydrochlorothiazide, and atorvastatin. Additionally, his right hip was replaced three years ago due to osteoarthritis. Family history is noncontributory. He drinks socially and does not smoke. Today, he has a heart rate of 95/min, respiratory rate of 17/min, blood pressure of 135/85 mm Hg, and temperature of 36.8°C (98.2°F). On physical exam, he looks well. His heartbeat has a regular rate and rhythm and lungs that are clear to auscultation bilaterally. Additionally, he has mild lymphadenopathy of his cervical lymph nodes. A complete blood count with differential shows the following:
Leukocyte count 5,000/mm3
Red blood cell count 3.1 million/mm3
Hemoglobin 11.0 g/dL
MCV 95 um3
MCH 29 pg/cell
Platelet count 150,000/mm3
Neutrophils 40%
Lymphocytes 40%
Monocytes 5%
A specimen is sent for flow cytometry that shows a population that is CD 5, 19, 20, 23 positive. Which of the following is the most likely diagnosis?
- A. Chronic lymphocytic leukemia (Correct Answer)
- B. Immune thrombocytopenic purpura
- C. Aplastic anemia
- D. Acute lymphoblastic leukemia
- E. Tuberculosis
Non-Hodgkin lymphomas Explanation: ***Chronic lymphocytic leukemia***
- The patient presents with mild **lymphadenopathy**, a **history of lymphocytosis**, and a **flow cytometry** showing cells positive for **CD5, CD19, CD20, and CD23**, which is pathognomonic for **CLL**.
- While the total leukocyte count is within normal limits due to the absolute neutrophil decrease, the persistent lymphocytosis and characteristic immunophenotype are highly indicative of CLL.
*Immune thrombocytopenic purpura*
- This condition is characterized by **isolated thrombocytopenia** caused by autoantibody-mediated platelet destruction, which is not supported by the patient's normal platelet count (150,000/mm3).
- While it can cause fatigue, it doesn't explain the lymphocytosis or the specific **CD marker profile**.
*Aplastic anemia*
- Aplastic anemia involves **pancytopenia** (decreased red blood cells, white blood cells, and platelets) due to bone marrow failure, which is not consistent with the patient's normal-range leukocyte and platelet counts.
- The patient's presentation with lymphocytosis and lymphadenopathy further makes this diagnosis unlikely.
*Acute lymphoblastic leukemia*
- **ALL** typically presents with symptoms related to **bone marrow failure** (anemia, thrombocytopenia, infections) and often very **high blast counts** in the peripheral blood and bone marrow.
- While it involves lymphocytes, the specific **CD5/19/20/23 co-expression** is characteristic of CLL, and ALL usually involves more aggressive symptoms and a different immunophenotype.
*Tuberculosis*
- **Tuberculosis** is an infectious disease that can cause **lymphadenopathy** and systemic symptoms like fatigue, but it is typically associated with a **caseating granulomatous inflammation** and is diagnosed via cultures or PCR rather than flow cytometry.
- It would not explain the specific **B-cell lymphocytosis** with the described immunophenotype.
More Non-Hodgkin lymphomas US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.