Myelodysplastic syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Myelodysplastic syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Myelodysplastic syndromes US Medical PG Question 1: A 45-year-old woman comes to the physician because of a 1-week history of fatigue and bruises on her elbows. Examination shows a soft, nontender abdomen with no organomegaly. Laboratory studies show a hemoglobin concentration of 7 g/dL, a leukocyte count of 2,000/mm3, a platelet count of 40,000/mm3, and a reticulocyte count of 0.2%. Serum electrolyte concentrations are within normal limits. A bone marrow biopsy is most likely to show which of the following findings?
- A. Increased myeloblast count
- B. Sheets of abnormal plasma cells
- C. Wrinkled cells with a fibrillary cytoplasm
- D. Hypocellular bone marrow (Correct Answer)
- E. Dysplastic bone with ringed sideroblasts
Myelodysplastic syndromes Explanation: ***Hypocellular bone marrow***
- The patient presents with **pancytopenia** (low hemoglobin, leukocytes, and platelets) and a very low **reticulocyte count**, indicating severely impaired hematopoiesis [1].
- This constellation of findings, in the absence of organomegaly or other specific features, strongly suggests **aplastic anemia**, which is characterized by a **hypocellular bone marrow** with significant reduction in hematopoietic cells and replacement by fat [1][3].
*Increased myeloblast count*
- An increased **myeloblast count** in the bone marrow is characteristic of **acute myeloid leukemia (AML)**.
- While pancytopenia can occur in AML, the distinguishing feature would be a high percentage of blasts (typically >20%) in the bone marrow, which is not implied by the general presentation [1].
*Sheets of abnormal plasma cells*
- **Sheets of abnormal plasma cells** are the hallmark of **multiple myeloma** [2].
- This condition primarily presents with bone pain, hypercalemia, renal failure, and anemia, but not typically with severe pancytopenia and bruising as the primary presenting symptoms without other myeloma-defining events [2].
*Wrinkled cells with a fibrillary cytoplasm*
- **Wrinkled cells with a fibrillary cytoplasm** (Gaucher cells) are pathognomonic for **Gaucher disease**, a lysosomal storage disorder.
- Gaucher disease typically presents with hepatosplenomegaly, bone crises, and neurological symptoms, not primarily with aplastic anemia.
**References:**
[1] Kumar V, Abbas AK, et al.. Robbins and Cotran Pathologic Basis of Disease. 9th ed. Red Blood Cell and Bleeding Disorders, pp. 662-663.
[2] Cross SS. Underwood's Pathology: A Clinical Approach. 6th ed. Common Clinical Problems From Blood And Bone Marrow Disease, pp. 617-618.
[3] Cross SS. Underwood's Pathology: A Clinical Approach. 6th ed. Common Clinical Problems From Blood And Bone Marrow Disease, pp. 595-596.
Myelodysplastic syndromes US Medical PG Question 2: A 24-year-old woman complains of intermittent fever and joint pain. She says that these symptoms have been present for the past month. Before that, she had no signs or symptoms and was completely healthy. She has also lost her appetite and some weight. A complete blood count (CBC) showed severe pancytopenia. What is the next best step in evaluating this patient?
- A. Repeated CBCs for several weeks and reassess
- B. Treatment with corticosteroids
- C. Treatment with antibiotics
- D. Treatment for acute leukemia
- E. Bone marrow examination (Correct Answer)
Myelodysplastic syndromes Explanation: ***Bone marrow examination***
- The combination of **fever**, **joint pain**, **weight loss**, and **pancytopenia** in a previously healthy young woman raises suspicion for serious hematologic conditions like **aplastic anemia** or **acute leukemia**.
- A **bone marrow examination** is crucial for definitive diagnosis by evaluating the cellularity, morphology, and presence of abnormal cells.
*Repeated CBCs for several weeks and reassess*
- This approach is inappropriate given the **severe pancytopenia** and progressive symptoms, which indicate an urgent underlying pathology.
- Delaying diagnosis could worsen the patient's condition and compromise treatment outcomes due to the potential for severe infections or bleeding.
*Treatment with corticosteroids*
- While corticosteroids might be used in some autoimmune conditions causing pancytopenia, initiating treatment without a definitive diagnosis is premature and could mask the underlying cause, especially in cases of malignancy.
- There is no specific indication for corticosteroid use in this scenario without further diagnostic information.
*Treatment with antibiotics*
- Although **fever** is present, there's no clear evidence of an infection (like localized symptoms or positive cultures), and **pancytopenia** is not primarily managed with antibiotics.
- Administering antibiotics empirically without a confirmed infection addresses a symptom rather than the underlying progressive hematological disorder.
*Treatment for acute leukemia*
- While **acute leukemia** is a strong possibility, definitive treatment should only commence after a confirmed diagnosis through **bone marrow examination**, as misdiagnosis can lead to inappropriate and harmful therapy.
- Other conditions like severe aplastic anemia also present with similar features but require different management strategies.
Myelodysplastic syndromes US Medical PG Question 3: A 76-year-old woman presents to the physician for a follow-up examination. She had a hemoglobin level of 10.5 g/dL last month. She complains of mild dyspnea with exercise. She reports exercising daily for the past 30 years. She is relatively healthy without any significant past medical history. She occasionally takes ibuprofen for knee pain. She denies a prior history of alcohol or tobacco use. Her temperature is 37.1°C (98.8°F), the pulse is 65/min, the respiratory rate is 13/min, and the blood pressure is 115/65 mm Hg. The examination shows no abnormalities. Laboratory studies show:
Laboratory test
Hemoglobin 10.5 g/dL
Mean corpuscular volume 75 μm3
Leukocyte count 6500/mm3 with a normal differential
Platelet 400,000/mm3
Serum
Iron 35
Total iron-binding capacity 450 μg/dL
Ferritin 8
Ca+ 9.0 mg/dL
Albumin 3.9 g/dL
Urea nitrogen 10 mg/dL
Creatinine 0.9 mg/dL
Serum protein electrophoresis and immunofixation show a monoclonal protein of 20 g/L (non-IgM). Marrow plasmacytosis is 5%. A skeletal survey shows no abnormalities. In addition to the workup of iron deficiency anemia, which of the following is the most appropriate next step in management?
- A. Referral for radiation therapy
- B. Check beta-2 microglobulin
- C. No further steps are required at this time
- D. Annual follow-up with laboratory tests (Correct Answer)
- E. Referral for induction therapy
Myelodysplastic syndromes Explanation: ***Annual follow-up with laboratory tests***
- This patient's presentation, with a **monoclonal protein (non-IgM) of 20 g/L** and **5% marrow plasmacytosis**, along with the absence of bone lesions and hypercalcemia, aligns with the diagnostic criteria for **Monoclonal Gammopathy of Undetermined Significance (MGUS)**.
- MGUS is a **pre-malignant condition** with a low annual risk of progression to multiple myeloma or related disorders, justifying annual monitoring rather than immediate aggressive intervention.
*Referral for radiation therapy*
- **Radiation therapy** is typically reserved for patients with localized complications of multiple myeloma, such as **painful bone lesions** or **spinal cord compression**, which are absent in this case.
- This patient's skeletal survey shows **no abnormalities**, ruling out the need for radiation therapy at this stage.
*Check beta-2 microglobulin*
- **Beta-2 microglobulin** is a marker used for staging **multiple myeloma**, indicating tumor burden and prognosis.
- While it's a helpful marker in confirmed myeloma, it is **not diagnostic for MGUS** and does not change the management of an asymptomatic patient with MGUS.
*No further steps are required at this time*
- While the patient does not need immediate aggressive treatment, **regular monitoring** is crucial due to the small but definite risk of progression of MGUS to multiple myeloma or related disorders.
- Doing nothing would be inappropriate, as missing the **progression of MGUS** could delay essential treatment.
*Referral for induction therapy*
- **Induction therapy** (e.g., chemotherapy, immunomodulatory drugs, proteasome inhibitors) is the primary treatment for **symptomatic multiple myeloma**.
- Since this patient has **MGUS** (asymptomatic monoclonal gammopathy without end-organ damage), induction therapy is **not indicated** and could expose her to unnecessary toxicity.
Myelodysplastic syndromes US Medical PG Question 4: A 20-year-old woman comes to the physician for the evaluation of fatigue and low energy levels for 2 months. She has not had fever or weight changes. She has no history of serious illness except for an episode of infectious mononucleosis 4 weeks ago. Menses occur at regular 28-day intervals and last 5 days with moderate flow. Her last menstrual period was 3 weeks ago. Her mother has Hashimoto's thyroiditis. Vital signs are within normal limits. Examination shows pale conjunctivae, inflammation of the corners of the mouth, and brittle nails. The remainder of the examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.3 g/dL
Mean corpuscular volume 74 μm3
Platelet count 280,000/mm3
Leukocyte count 6,000/mm3
Which of the following is the most appropriate initial step in management?
- A. Iron studies (Correct Answer)
- B. Vitamin B12 levels
- C. Peripheral blood smear
- D. Hemoglobin electrophoresis
- E. Direct Coombs test
Myelodysplastic syndromes Explanation: ***Iron studies***
- The patient presents with **microcytic anemia** (Hb 10.3 g/dL, MCV 74 μm3), along with symptoms like **fatigue**, pale conjunctivae, angular cheilitis, and brittle nails, all highly suggestive of **iron deficiency anemia**.
- **Iron studies** (serum iron, ferritin, total iron-binding capacity, transferrin saturation) are crucial to confirm the diagnosis and determine the severity of iron deficiency.
*Vitamin B12 levels*
- **Vitamin B12 deficiency** typically causes **macrocytic anemia** (elevated MCV), which is not consistent with the patient's **low MCV (74 μm3)**.
- While fatigue is a symptom, the other clinical signs and lab results point away from B12 deficiency.
*Peripheral blood smear*
- A **peripheral blood smear** may show microcytic, hypochromic red blood cells if iron deficiency is present, but it does not quantify **iron stores** or establish the cause definitively.
- While useful for morphological assessment, it is usually performed after initial labs suggest a specific type of anemia, and **iron studies** are more direct for diagnosing iron deficiency.
*Hemoglobin electrophoresis*
- **Hemoglobin electrophoresis** is used to diagnose hemoglobinopathies like **thalassemia** or **sickle cell disease**.
- While some thalassemias can cause microcytic anemia, the clinical picture with **angular cheilitis** and **brittle nails** strongly points towards iron deficiency, making iron studies a more appropriate initial step.
*Direct Coombs test*
- The **Direct Coombs test** is used to diagnose **autoimmune hemolytic anemia**, where antibodies are bound to the surface of red blood cells leading to their destruction.
- This patient's presentation does not suggest hemolysis (e.g., jaundice, splenomegaly, elevated LDH, low haptoglobin), and the dominant feature is **microcytic anemia from likely iron deficiency**.
Myelodysplastic syndromes US Medical PG Question 5: A 9-year-old boy is brought to the physician by his mother because of a 3-day history of fever and bleeding after brushing his teeth. His mother also reports that her son has asked to be picked up early from soccer practice the past few days because of fatigue. He appears pale and ill. His temperature is 38.3°C (101.1°F), pulse is 115/min, and blood pressure is 100/60 mm Hg. The lungs are clear to auscultation. Examination shows a soft, nontender abdomen with no organomegaly. There are several spots of subcutaneous bleeding on the abdomen and shins. Laboratory studies show a hemoglobin concentration of 7 g/dL, a leukocyte count of 2,000/mm3, a platelet count of 40,000/mm3, and a reticulocyte count of 0.2%. Serum electrolyte concentrations are within normal limits. A bone marrow biopsy is most likely to show which of the following findings?
- A. Infiltration of the marrow with collagen and fibrous tissue
- B. Normocellular bone marrow
- C. Hypercellular, dysplastic bone marrow with ringed sideroblasts
- D. Sheets of abnormal plasma cells
- E. Hypocellular fat-filled marrow with RBCs of normal morphology (Correct Answer)
Myelodysplastic syndromes Explanation: ***Hypocellular fat-filled marrow with RBCs of normal morphology***
- The patient presents with **pancytopenia** (anemia, leukopenia, thrombocytopenia) and a very low **reticulocyte count**, indicating severe bone marrow failure.
- A **hypocellular, fat-filled marrow** with normal RBC morphology is characteristic of **aplastic anemia**, which fits the clinical picture of fatigue, bleeding, and pallor due to suppressed hematopoiesis.
*Infiltration of the marrow with collagen and fibrous tissue*
- This finding is typical of **myelofibrosis**, which usually presents with **splenomegaly** due to extramedullary hematopoiesis and often **leukoerythroblastosis** in the peripheral blood.
- The patient's abdomen is soft with **no organomegaly**, and the blood counts do not suggest myelofibrosis.
*Normocellular bone marrow*
- A **normocellular marrow** would not explain the severe pancytopenia seen in this patient; it suggests adequate cell production, which is clearly lacking here.
- While other conditions can cause pancytopenia due to peripheral destruction, the **low reticulocyte count** points to a production problem in the bone marrow.
*Hypercellular, dysplastic bone marrow with ringed sideroblasts*
- This describes features of **myelodysplastic syndrome (MDS)**, which can cause pancytopenia and often presents with **dysplastic changes** in blood cells.
- While MDS can occur in children, the sudden onset and severe pancytopenia, coupled with the absence of specific dysplastic features mentioned, make aplastic anemia more likely.
*Sheets of abnormal plasma cells*
- **Sheets of abnormal plasma cells** are seen in **multiple myeloma**, a malignancy typically affecting older adults and associated with **bone pain**, hypercalcemia, renal failure, and **monoclonal gammopathy**.
- This diagnosis is highly unlikely in a 9-year-old boy with these symptoms.
Myelodysplastic syndromes US Medical PG Question 6: An otherwise healthy 42-year-old man undergoes routine investigations prior to blood donation. His complete blood count is shown:
Hemoglobin 9.3 g/dL
Mean corpuscular volume (MCV) 71 μm3
Mean corpuscular hemoglobin (MCH) 21 pg/cell
White blood cell count 8,200/mm3
Platelet count 317,000/mm3
Iron studies are shown:
Serum iron 210 μg/dL
Serum ferritin 310 ng/mL
Total iron binding capacity (TIBC) 290 μg/dL
Transferrin saturation 78%
He occasionally drinks alcohol and denies smoking or use of illicit drugs. There is a family history of anemia including his brother and maternal uncle. Examination shows conjunctival pallor, but is otherwise unremarkable. Which of the following is the most likely diagnosis?
- A. Hemochromatosis
- B. Anemia of chronic disease
- C. Acute myeloid leukemia
- D. Sideroblastic anemia (Correct Answer)
- E. Myelodysplastic syndrome
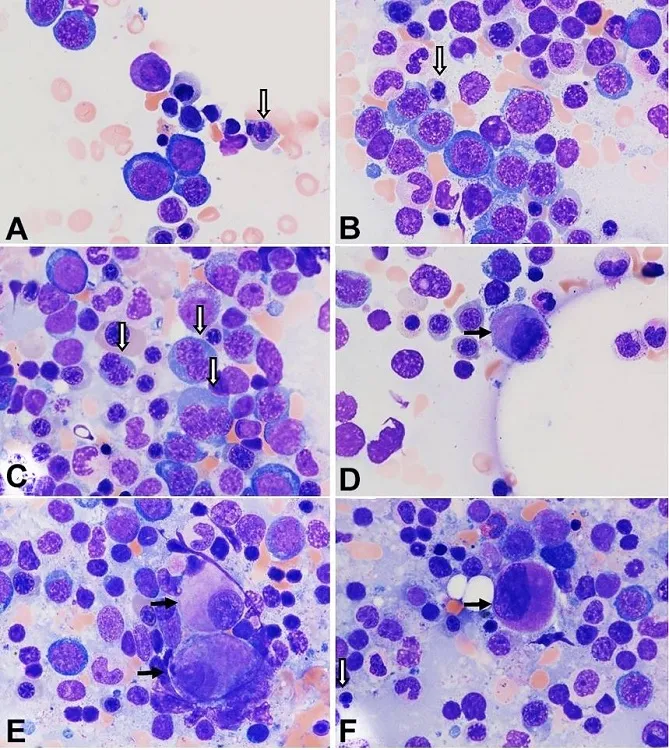
Myelodysplastic syndromes Explanation: ***Sideroblastic anemia***
- The patient presents with **microcytic anemia** (Hb 9.3 g/dL, MCV 71, MCH 21) and evidence of **iron overload** (serum iron 210, ferritin 310, transferrin saturation 78%). These findings, along with a **family history of anemia affecting males** (brother and maternal uncle), are classic for **hereditary sideroblastic anemia**, typically X-linked.
- **Sideroblastic anemia** is characterized by the bone marrow producing ring sideroblasts (erythroblasts with iron-laden mitochondria), leading to ineffective erythropoiesis and iron accumulation.
- The hereditary form presents in younger patients with isolated anemia and strong family history, distinguishing it from acquired forms.
*Hemochromatosis*
- While **hemochromatosis** also presents with iron overload (high serum iron, ferritin, and transferrin saturation), it typically does **not cause microcytic anemia** or any significant anemia.
- The primary defect in hemochromatosis is increased iron absorption leading to tissue iron deposition (liver, heart, pancreas), without the erythropoietic dysfunction seen in sideroblastic anemia.
*Anemia of chronic disease*
- **Anemia of chronic disease (ACD)** typically presents with normal or slightly reduced MCV and MCH, and is characterized by **low serum iron** and **low TIBC**, with normal or elevated ferritin.
- In this case, the patient has **elevated serum iron** and **high transferrin saturation (78%)**, making ACD unlikely.
*Acute myeloid leukemia*
- **Acute myeloid leukemia (AML)** involves the proliferation of immature myeloid cells and usually presents with pancytopenia or symptoms related to bone marrow failure (e.g., fatigue, bleeding, infections).
- The blood counts here show **isolated anemia with normal WBC and platelet counts**, and the iron studies are not typical for AML.
*Myelodysplastic syndrome*
- **Myelodysplastic syndromes (MDS)** are clonal disorders of hematopoietic stem cells, often presenting with cytopenias and dysplastic features in the bone marrow.
- While **acquired sideroblastic anemia** is a subtype of MDS (refractory anemia with ring sideroblasts), it typically occurs in **older adults (>60 years)** without a family history.
- This patient's **young age (42 years)** and **strong family history** (brother and maternal uncle) point to **hereditary sideroblastic anemia** rather than MDS-associated acquired sideroblastic anemia.
Myelodysplastic syndromes US Medical PG Question 7: A 7-month old boy, born to immigrant parents from Greece, presents to the hospital with pallor and abdominal distention. His parents note that they recently moved into an old apartment building and have been concerned about their son's exposure to chipped paint from the walls. On physical exam, the patient is found to have hepatosplenomegaly and frontal skull bossing. Hemoglobin electrophoresis reveals markedly increased HbF and HbA2 levels. What would be the most likely findings on a peripheral blood smear?
- A. Microcytosis and hypochromasia of erythrocytes (Correct Answer)
- B. Sickling of erythrocytes
- C. Basophilic stippling of erythrocytes
- D. Macrocytosis of erythrocytes with hypersegmented neutrophils
- E. Schistocytes and normocytic erythrocytes
Myelodysplastic syndromes Explanation: ### ***Microcytosis and hypochromasia of erythrocytes***
- This patient presents with **β-thalassemia major**, as evidenced by **Greek ancestry** (Mediterranean population at high risk), **markedly elevated HbF and HbA2 levels** on hemoglobin electrophoresis, **frontal skull bossing** from bone marrow expansion, and **hepatosplenomegaly** from extramedullary hematopoiesis.
- The peripheral blood smear in β-thalassemia major characteristically shows **severe microcytic, hypochromic anemia** with target cells, nucleated RBCs, and marked anisocytosis and poikilocytosis.
- The inadequate β-globin chain production leads to ineffective erythropoiesis and severe hemolysis, resulting in the microcytic, hypochromic pattern.
### *Basophilic stippling of erythrocytes*
- While **basophilic stippling** can be seen in β-thalassemia, it is not the **most characteristic** finding and is more commonly associated with **lead poisoning**.
- The chipped paint exposure in this case is a distractor; **lead poisoning does NOT cause elevated HbF/HbA2, frontal bossing, or this degree of organomegaly** in a 7-month-old.
- The hemoglobin electrophoresis findings definitively point to thalassemia, not lead toxicity.
### *Sickling of erythrocytes*
- **Sickling** is pathognomonic for **sickle cell disease**, which presents with elevated HbS (not HbF and HbA2) on electrophoresis.
- While both are hemoglobinopathies affecting Mediterranean populations, the electrophoresis pattern and clinical features clearly indicate thalassemia, not sickle cell disease.
### *Schistocytes and normocytic erythrocytes*
- **Schistocytes** indicate **microangiopathic hemolytic anemia** (e.g., TTP, HUS, DIC), which involves mechanical RBC fragmentation in damaged microvasculature.
- The patient's chronic presentation, organomegaly, skeletal changes, and hemoglobin electrophoresis findings are inconsistent with microangiopathic hemolysis.
### *Macrocytosis of erythrocytes with hypersegmented neutrophils*
- **Macrocytic anemia with hypersegmented neutrophils** is characteristic of **megaloblastic anemia** from vitamin B12 or folate deficiency.
- β-thalassemia causes **microcytic** anemia due to deficient hemoglobin synthesis, not macrocytic anemia from impaired DNA synthesis.
Myelodysplastic syndromes US Medical PG Question 8: A 71-year-old man comes to the physician for a routine health maintenance examination. He has occasional fatigue but otherwise feels well. He has a history of hypertension and type 2 diabetes mellitus. He is a retired chemist. His only medication is ramipril. His temperature is 37.8°C (100°F), pulse is 72/min, respirations are 18/min, and blood pressure is 130/70 mm Hg. Physical examination shows nontender cervical and axillary lymphadenopathy. The spleen is palpated 7 cm below the costal margin. Laboratory studies show a leukocyte count of 12,000/mm3 and a platelet count of 210,000/mm3. Further evaluation is most likely to show which of the following?
- A. Smudge cells (Correct Answer)
- B. Ringed sideroblasts
- C. Rouleaux formation
- D. Teardrop cells
- E. Polycythemia
Myelodysplastic syndromes Explanation: ***Smudge cells***
- The patient's presentation with **fatigue**, **lymphadenopathy**, **splenomegaly**, and a **leukocytosis** (12,000/mm³) is classic for **chronic lymphocytic leukemia (CLL)**.
- **Smudge cells** (also known as Gumprecht shadows) are characteristic findings on a peripheral blood smear in CLL, resulting from the fragile lymphocytes being crushed during slide preparation.
*Ringed sideroblasts*
- **Ringed sideroblasts** are immature red blood cells with iron granules accumulated in a ring around the nucleus, seen in **myelodysplastic syndromes** and **sideroblastic anemia**.
- This patient's symptoms and labs, particularly the significant lymphocytosis, do not support these conditions.
*Rouleaux formation*
- **Rouleaux formation** refers to red blood cells stacking up like coins, commonly seen in conditions with increased plasma proteins such as **multiple myeloma** or **macroglobulinemia**.
- The clinical picture here, with prominent lymphadenopathy and splenomegaly, is not typical for these disorders.
*Teardrop cells*
- **Teardrop cells** (dacryocytes) are red blood cells with a characteristic teardrop shape, often associated with **myelofibrosis** due to their deformation as they squeeze through fibrotic marrow.
- The patient's presentation lacks other key features of myelofibrosis, such as significant anemia, extremely high leukocyte counts, or symptoms of marrow failure.
*Polycythemia*
- **Polycythemia** refers to an abnormally high concentration of red blood cells (or hemoglobin) in the blood, often associated with conditions like **polycythemia vera**.
- While fatigue can be a symptom, the patient's leukocyte count is elevated, not the erythrocyte count, and the presence of lymphadenopathy and splenomegaly points away from isolated polycythemia.
Myelodysplastic syndromes US Medical PG Question 9: A 13-year-old girl is brought to the pediatrician due to a 4-month history of heavy vaginal bleeding during menstrual periods. She endorses episodes of bleeding gums after brushing her teeth and experienced prolonged bleeding after tonsillectomy 6 years ago. Her mother states that she bled significantly during childbirth and that the girl’s older brother has similar symptoms including easy bruising. Vitals were stable and physical exam was not revealing. Laboratory studies show:
Platelet count: 72,000/mm^3
Bleeding time: 14 min
Prothrombin time: 12 secs (INR = 1)
Partial thromboplastin time: 40 secs
Blood smear demonstrates increased megakaryocytes and enlarged platelets. Platelets do not aggregate to ristocetin. Which of the following is the most likely diagnosis?
- A. Glanzmann thrombasthenia
- B. Idiopathic thrombocytopenic purpura (ITP)
- C. Bernard-Soulier syndrome (Correct Answer)
- D. Aspirin or NSAID use
- E. von Willebrand disease (vWD)
Myelodysplastic syndromes Explanation: ***Bernard-Soulier syndrome***
- The patient presents with **thrombocytopenia** (platelet count 72,000/mm^3), **prolonged bleeding time** (14 min), and **enlarged platelets** and **megakaryocytes** on blood smear.
- The key diagnostic feature is the **failure of platelets to aggregate to ristocetin**, indicating a defect in the GPIb-IX-V receptor complex which mediates platelet adhesion to von Willebrand factor. This clinical picture in a patient with a family history of bleeding is classic for Bernard-Soulier syndrome.
*Glanzmann thrombasthenia*
- This condition is characterized by a defect in the **GPIIb/IIIa receptor**, which is crucial for platelet aggregation; however, patients with Glanzmann thrombasthenia typically have a **normal platelet count** and **normal platelet morphology**.
- Platelets in Glanzmann thrombasthenia would fail to aggregate to ADP, collagen, and epinephrine, but aggregation to **ristocetin** would generally be normal (unless very high concentrations are used), making it less likely given the specific finding of failed ristocetin aggregation and thrombocytopenia.
*Idiopathic thrombocytopenic purpura (ITP)*
- ITP causes isolated **thrombocytopenia** (low platelet count) and **increased megakaryocytes** in the bone marrow, but platelets are typically of **normal size** or may be **larger than normal** but not giant platelets.
- While ITP would cause a prolonged bleeding time, it would not typically show **enlarged platelets** on blood smear, nor would the platelets specifically fail to aggregate to ristocetin due to a receptor defect.
*Aspirin or NSAID use*
- Aspirin and NSAIDs inhibit **cyclooxygenase**, leading to impaired platelet aggregation and a **prolonged bleeding time**, but they do not cause **thrombocytopenia** or changes in **platelet morphology** like enlarged platelets or increased megakaryocytes.
- Platelet aggregation to ristocetin would be normal in the context of aspirin or NSAID use, as the GP Ib-IX-V and GP IIb/IIIa complexes are unaffected.
*von Willebrand disease (vWD)*
- vWD involves a deficiency or defect in **von Willebrand factor**, leading to impaired platelet adhesion and sometimes reduced factor VIII levels, which causes a **prolonged bleeding time**; however, platelet count and morphology are typically **normal**.
- While vWD can show decreased ristocetin-induced platelet aggregation, it does **not present with thrombocytopenia** or **enlarged platelets/megakaryocytes** as seen in this patient.
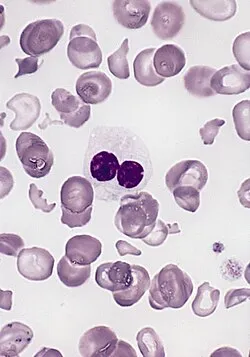
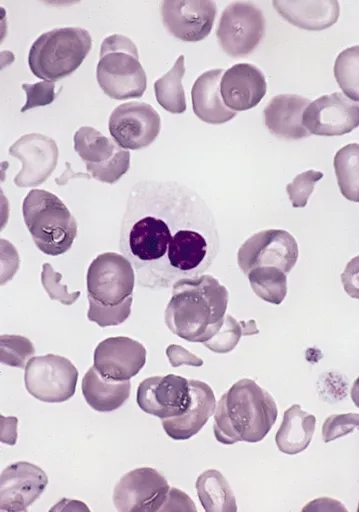
Myelodysplastic syndromes US Medical PG Question 10: A 60-year-old woman comes to the physician because of lower back pain, generalized weakness, and weight loss that has occurred over the past 6 weeks. She also says that her urine has appeared foamy recently. Physical examination shows focal midline tenderness of the lumbar spine and conjunctival pallor. Her temperature is 100.5°F (38°C). A photomicrograph of a bone marrow biopsy specimen is shown. Further evaluation of this patient is most likely to show which of the following findings?
- A. Myeloblasts with needle-shaped cytoplasmic inclusions
- B. Erythrocytes with cytoplasmic hemoglobin inclusions
- C. Neutrophils with hypersegmented nuclear lobes
- D. Grouped erythrocytes with stacked-coin appearance (Correct Answer)
- E. B-lymphocytes with radial cytoplasmic projections
Myelodysplastic syndromes Explanation: ***Grouped erythrocytes with stacked-coin appearance***
- The patient's presentation of **lower back pain** (lytic bone lesions), **foamy urine** (proteinuria from Bence Jones proteins), **weight loss**, and **fever** strongly suggests **multiple myeloma**.
- Bone marrow biopsy would show **increased plasma cells**, and further evaluation with **peripheral blood smear** would reveal **rouleaux formation** (stacked-coin appearance of RBCs).
- Rouleaux formation occurs due to **increased serum proteins** (M-protein/paraprotein) that decrease the negative charge between erythrocytes, causing them to stack.
- This finding, combined with **anemia** (conjunctival pallor) and **hypercalcemia** symptoms, is characteristic of multiple myeloma.
*Myeloblasts with needle-shaped cytoplasmic inclusions*
- This describes **Auer rods**, which are pathognomonic for **acute myeloid leukemia (AML)**.
- AML typically presents with **bleeding**, **infections**, and **pancytopenia**, rather than bone pain and foamy urine.
- The patient's clinical picture points to a **plasma cell dyscrasia**, not myeloid leukemia.
*Erythrocytes with cytoplasmic hemoglobin inclusions*
- This finding (Howell-Jolly bodies, Heinz bodies, or other inclusions) suggests **hemolytic anemia**, **thalassemia**, or **asplenia**.
- These conditions do not explain the **bone pain**, **proteinuria**, or **plasma cell proliferation** seen in this case.
- The patient's symptoms are better explained by **multiple myeloma**, not hemoglobinopathy.
*Neutrophils with hypersegmented nuclear lobes*
- Hypersegmented neutrophils (≥5 lobes) are characteristic of **megaloblastic anemia** due to **vitamin B12** or **folate deficiency**.
- While this could cause weakness and anemia, it does not explain the **bone pain**, **fever**, **foamy urine**, or **lumbar spine tenderness**.
- The complete clinical picture is consistent with **multiple myeloma**, not nutritional deficiency.
*B-lymphocytes with radial cytoplasmic projections*
- This describes **hairy cell leukemia**, a rare B-cell neoplasm with characteristic "hairy" projections.
- Hairy cell leukemia presents with **splenomegaly** and **pancytopenia**, not the bone lesions and proteinuria seen here.
- The patient's presentation aligns with **plasma cell myeloma**, not B-cell lymphoproliferative disorder.
More Myelodysplastic syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.