Coagulation disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Coagulation disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Coagulation disorders US Medical PG Question 1: A 7-year-old boy is brought to the physician for a follow-up examination after the removal of a tooth. During the procedure, he had prolonged bleeding that did not resolve with pressure and gauze packing and eventually required suture placement. His older brother had a similar episode a year ago, but his parents and two sisters have never had problems with prolonged bleeding. Physical examination shows no abnormalities. Genetic analysis confirms an X-linked recessive disorder. Which of the following is most likely deficient in this patient?
- A. Protein C
- B. Factor VIII (Correct Answer)
- C. Von Willebrand factor
- D. Factor IX
- E. Factor XI
Coagulation disorders Explanation: ***Factor VIII***
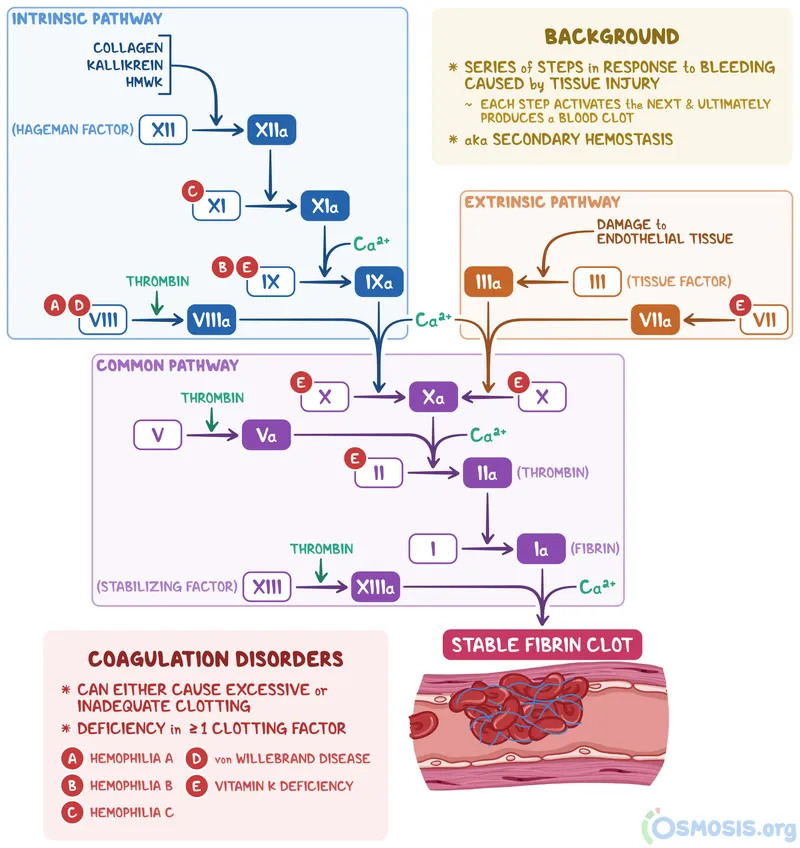
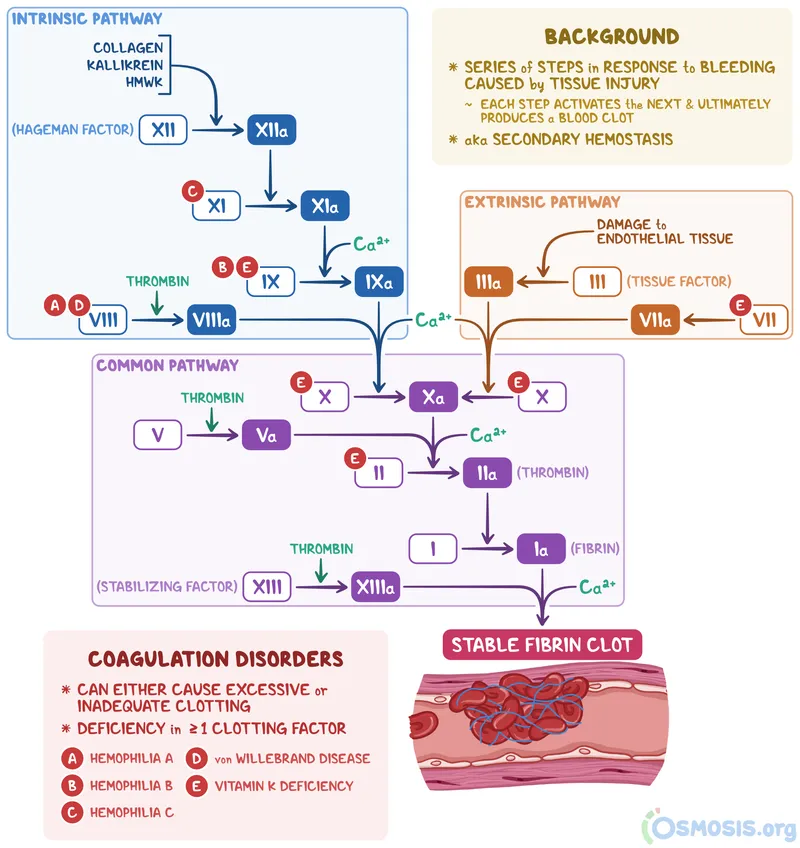
- The presentation of **prolonged bleeding** after a minor procedure like tooth extraction, an **X-linked recessive inheritance pattern**, and a male sibling with a similar history are classic features of **Hemophilia A**, which is caused by a deficiency of **Factor VIII**.
- X-linked recessive disorders primarily affect males, who inherit the single X chromosome from their mother, while females are typically carriers and do not show symptoms, consistent with the healthy parents and sisters.
*Protein C*
- Deficiency in **Protein C** is associated with a **hypercoagulable state**, leading to an increased risk of **thrombosis**, not bleeding.
- This condition is inherited in an **autosomal dominant** manner, which does not fit the X-linked recessive pattern described.
*Von Willebrand factor*
- **Von Willebrand disease** is the most common inherited bleeding disorder, often presenting with mucocutaneous bleeding (e.g., nosebleeds, menorrhagia), and while it can cause prolonged bleeding, it is typically inherited in an **autosomal dominant** pattern.
- Though some severe forms can be autosomal recessive, an X-linked recessive pattern with affected males and unaffected females in the described family structure is less characteristic of vWD than Hemophilia A.
*Factor IX*
- A deficiency in **Factor IX** causes **Hemophilia B**, which also presents with an X-linked recessive inheritance pattern and prolonged bleeding symptoms similar to Hemophilia A.
- However, Hemophilia A (Factor VIII deficiency) is about four to five times more common than Hemophilia B (Factor IX deficiency), making Factor VIII deficiency the more statistically likely diagnosis given similar clinical presentations.
*Factor XI*
- **Factor XI deficiency** (Hemophilia C) is a milder bleeding disorder, often characterized by **autosomal recessive** inheritance, though it can also be autosomal dominant or have variable penetrance.
- Symptoms are usually less severe than hemophilia A or B, and the inheritance pattern is not typically X-linked recessive.
Coagulation disorders US Medical PG Question 2: A 28-year-old man presents for severe abdominal pain and is diagnosed with appendicitis. He is taken for emergent appendectomy. During the procedure, the patient has massive and persistent bleeding requiring a blood transfusion. The preoperative laboratory studies showed a normal bleeding time, normal prothrombin time (PT), an INR of 1.0, and a normal platelet count. Postoperatively, when the patient is told about the complications during the surgery, he recalls that he forgot to mention that he has a family history of an unknown bleeding disorder. The postoperative laboratory tests reveal a prolonged partial thromboplastin time (PTT). Which of the following is the most likely diagnosis in this patient?
- A. von Willebrand disease
- B. Bernard-Soulier syndrome
- C. Thrombotic thrombocytopenic purpura
- D. Hemophilia A (Correct Answer)
- E. Glanzmann thrombasthenia
Coagulation disorders Explanation: ***Hemophilia A***
- The patient's presentation with **severe, persistent bleeding** during surgery despite normal preoperative coagulation studies (PT, INR, platelet count) and a subsequent **prolonged PTT** strongly indicates a **factor deficiency in the intrinsic pathway**.
- **Hemophilia A**, an X-linked recessive disorder, is caused by a deficiency of **Factor VIII**, leading to a prolonged PTT and deep tissue bleeding, which fits the clinical picture and family history.
*von Willebrand disease*
- This condition typically presents with **mucocutaneous bleeding** (e.g., nosebleeds, menorrhagia) and can have a prolonged bleeding time, but the primary defect is in **platelet adhesion**, not usually massive operative bleeding with normal platelet count.
- While **von Willebrand factor (vWF)** carries Factor VIII, a primary deficiency of vWF would affect factor VIII levels but the presentation and normal bleeding time here make it less likely than direct factor VIII deficiency.
*Bernard-Soulier syndrome*
- This is a **platelet disorder** characterized by defective **glycoprotein Ib/IX/V complex**, leading to impaired platelet adhesion and often **thrombocytopenia** with unusually large platelets.
- The patient had a **normal platelet count** and a subsequent prolonged PTT, which points away from a primary platelet adhesion defect.
*Thrombotic thrombocytopenic purpura*
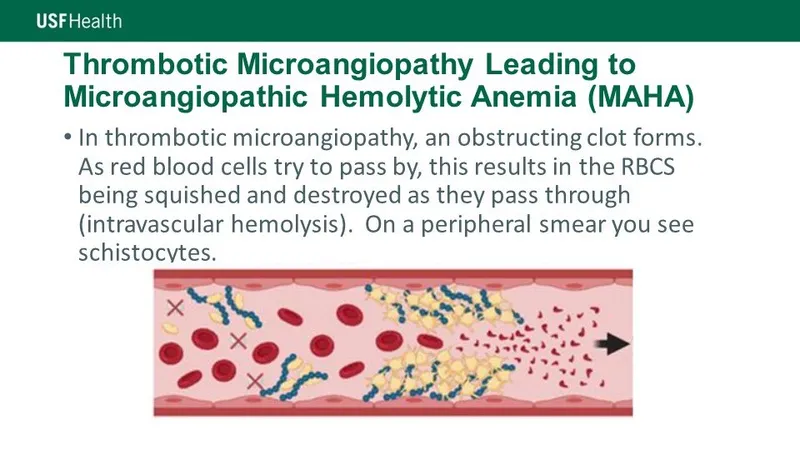
- This is a microangiopathic hemolytic anemia characterized by a **pentad of symptoms**: fever, neurologic symptoms, renal dysfunction, thrombocytopenia, and microangiopathic hemolytic anemia.
- It involves widespread **thrombosis** and **low platelet count**, which does not align with the patient's presentation of massive bleeding with normal platelet counts.
*Glanzmann thrombasthenia*
- This is a rare **platelet aggregation disorder** caused by a defect in **glycoprotein IIb/IIIa**, leading to impaired fibrinogen binding and platelet aggregation.
- While it causes severe bleeding, it would be associated with a **prolonged bleeding time** and normal PTT, which contradicts the patient's normal bleeding time and prolonged PTT.
Coagulation disorders US Medical PG Question 3: A 30-year-old woman presents to the emergency department in a state of confusion and disorientation that started this morning. She is accompanied by her husband who says that she has been unwell for about one week. She has been complaining of fatigue. Her husband says that this morning, she also complained that her urine was dark red in color and that there were some red spots over her legs. He did notice some changes in her level of consciousness that worsened over time and he decided to bring her in today. She does not have a significant medical history. Physical examination shows petechiae over her arms and legs. She is conscious but drowsy and disoriented and unable to answer the physician’s questions appropriately. Her temperature is 38.3°C (100.9°F), blood pressure is 160/100 mm Hg, pulse rate is 90/min, and respiratory rate is 20/min.
Laboratory studies show:
Hemoglobin 10 g/dL
Leukocyte count 9,000/mm3
Platelet count 30,000/mm3
Bleeding time 10 min
Prothrombin time 12 s
Activated partial thromboplastin time 30 s
D-dimer 0.4 mg/L (normal < 0.5 mg/L)
Serum fibrinogen 350 mg/dL (normal 200–400 mg/dL)
Serum bilirubin (indirect) 2.2 mg/dL
Serum creatinine 1.5 mg/dL
Serum LDH 1,010 U/L
Based on her history, and her physical and laboratory findings, which of the following is the most likely pathophysiology for her presentation?
- A. GPIIb/IIIa deficiency and failure of platelet aggregation
- B. Systemic activation of blood coagulation
- C. E. coli-mediated endothelial damage and formation of microthrombi
- D. Antiplatelet antibodies
- E. Decreased ADAMTS13 causing platelet adhesion and formation of microthrombi (Correct Answer)
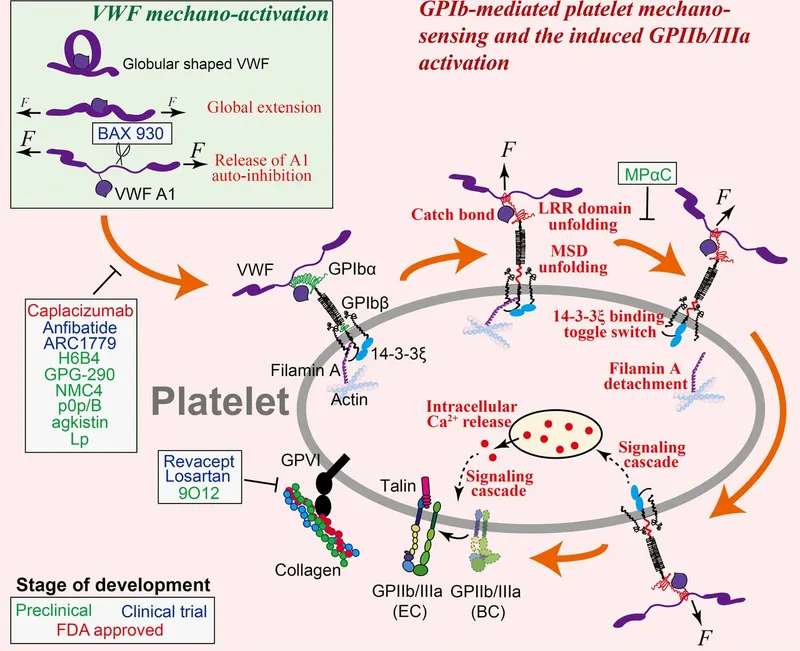
Coagulation disorders Explanation: ***Decreased ADAMTS13 causing platelet adhesion and formation of microthrombi***
* The constellation of **fever, neurologic symptoms (confusion, disorientation), renal dysfunction (creatinine 1.5 mg/dL), microangiopathic hemolytic anemia (indirect bilirubin 2.2 mg/dL, high LDH, dark red urine), and thrombocytopenia (platelet count 30,000/mm3, petechiae)** is characteristic of **Thrombotic Thrombocytopenic Purpura (TTP)**.
* **TTP** is caused by a deficiency in the **ADAMTS13 enzyme**, which normally cleaves **large Von Willebrand Factor (vWF) multimers**. A deficiency leads to accumulation of these large vWF multimers, causing **uncontrolled platelet adhesion and aggregation**, forming **microthrombi** in small blood vessels. This results in **hemolytic anemia** (due to fragmentation of red blood cells passing through the partially occluded vessels), **thrombocytopenia** (due to platelet consumption), and **end-organ damage** (kidney, brain).
*GPIIb/IIIa deficiency and failure of platelet aggregation*
* **GPIIb/IIIa deficiency (Glanzmann thrombasthenia)** is a disorder of **platelet aggregation**, leading to severe bleeding.
* Patients typically present with **mucocutaneous bleeding** and **normal platelet counts**. This patient has severe thrombocytopenia and evidence of microangiopathic hemolysis.
*Systemic activation of blood coagulation*
* This describes **Disseminated Intravascular Coagulation (DIC)**. While DIC involves microthrombi and thrombocytopenia, it is also characterized by **prolonged PT and aPTT**, **decreased fibrinogen**, and **elevated D-dimer** due to widespread activation of the coagulation cascade and subsequent fibrinolysis.
* This patient's **PT, aPTT, D-dimer, and fibrinogen levels are normal**, ruling out DIC as the primary etiology.
*E. coli-mediated endothelial damage and formation of microthrombi*
* This description is suggestive of **Hemolytic Uremic Syndrome (HUS)**, often caused by **Shiga-toxin-producing E. coli (STEC)**. HUS shares features with TTP but typically presents with a prodrome of **bloody diarrhea** and more prominent **renal failure** without significant neurological involvement as seen in TTP.
* The patient in this scenario does not report preceding diarrheal illness, making TTP a more likely diagnosis given the prominent neurological symptoms and mild renal dysfunction.
*Antiplatelet antibodies*
* This mechanism is characteristic of **Immune Thrombocytopenic Purpura (ITP)**, where antibodies destroy platelets, leading to thrombocytopenia and bruising/bleeding.
* **ITP** usually presents with isolated **thrombocytopenia** and normal hemoglobin and renal function, without evidence of microangiopathic hemolytic anemia or neurologic symptoms.
Coagulation disorders US Medical PG Question 4: A 14-year-old boy presents with his mother complaining of a swollen, red, painful left knee. His physician aspirates the joint and discovers frank blood. The patient denies a recent history of trauma to the knee. Upon further discussion, the mother describes that her son has had multiple swollen painful joints before, often without evidence of trauma. She also mentions a history of frequent nosebleeds and gum bleeding following visits to the dentist. Which of the following is the most likely underlying diagnosis?
- A. Factor VII deficiency
- B. Hemophilia C
- C. Child abuse
- D. Hemophilia B
- E. Hemophilia A (Correct Answer)
Coagulation disorders Explanation: ***Hemophilia A***
- The presentation of recurrent **hemarthroses** (swollen, red, painful joints with frank blood on aspiration) without trauma, along with a history of spontaneous bleeding (nosebleeds, gum bleeding), is highly characteristic of hemophilia.
- **Hemophilia A**, caused by a deficiency in factor VIII, is the most common type of severe hemophilia and often presents in childhood with these bleeding manifestations, particularly in joints.
*Factor VII deficiency*
- Factor VII deficiency primarily affects the **extrinsic pathway** of coagulation and typically presents with a prolonged **prothrombin time (PT)**, while the activated partial thromboplastin time (aPTT) would be normal.
- Clinical manifestations are usually milder than hemophilia A, but can include epistaxis, menorrhagia, and occasionally hemarthroses, but not with the classic severity and frequency seen here.
*Hemophilia C*
- Hemophilia C, caused by **factor XI deficiency**, is a milder bleeding disorder, often presenting with bleeding after trauma or surgery rather than spontaneous joint bleeding.
- It mainly affects Ashkenazi Jews and typically causes a prolonged **aPTT**, but usually less severe symptoms than hemophilia A or B.
*Child abuse*
- While child abuse should always be considered in cases of unexplained trauma, the detailed history of **recurrent, spontaneous bleeding events** (hemarthroses, nosebleeds, gum bleeding post-dental work) without a clear traumatic cause is more indicative of a systemic bleeding disorder.
- The pattern of bleeding is consistent with a coagulation defect rather than isolated traumatic injuries.
*Hemophilia B*
- Hemophilia B, or Christmas disease, is caused by **factor IX deficiency** and presents with symptoms clinically indistinguishable from hemophilia A (i.e., spontaneous joint and deep tissue bleeding).
- However, Hemophilia A is significantly more common than Hemophilia B (affecting about 1 in 5,000 to 10,000 live male births, compared to 1 in 25,000 to 30,000 for Hemophilia B). Therefore, Hemophilia A is the most likely diagnosis.
Coagulation disorders US Medical PG Question 5: A 4-year-old male is evaluated for frequent epistaxis and mucous membrane bleeding. Physical examination shows diffuse petechiae on the patient’s distal extremities. Peripheral blood smear shows an absence of platelet clumping. An ELISA binding assay reveals that platelet surfaces are deficient in GIIb/IIIa receptors. Serum platelet count is normal. Which of the following is the most likely diagnosis?
- A. Idiopathic thrombocytopenic purpura
- B. Thrombotic thrombocytopenic purpura
- C. Bernard-Soulier disease
- D. Hemophilia A
- E. Glanzmann’s thrombasthenia (Correct Answer)
Coagulation disorders Explanation: ***Glanzmann’s thrombasthenia***
- This condition is characterized by a **deficiency of GIIb/IIIa receptors** on platelets, leading to impaired platelet aggregation despite a normal platelet count.
- The patient's symptoms of **epistaxis**, **mucous membrane bleeding**, and **diffuse petechiae** are consistent with a primary hemostasis disorder.
*Idiopathic thrombocytopenic purpura*
- This autoimmune disorder causes **isolated thrombocytopenia** (low platelet count) due to antibody-mediated destruction of platelets.
- The patient's **normal platelet count** makes ITP an unlikely diagnosis.
*Thrombotic thrombocytopenic purpura*
- TTP is characterized by the **pentad of symptoms**: thrombocytopenia, microangiopathic hemolytic anemia, renal failure, neurological symptoms, and fever.
- The patient does not present with **anemia** or the other systemic features typical of TTP, and their platelet count is normal.
*Bernard-Soulier disease*
- This is a rare inherited disorder involving a **deficiency of GPIb-IX-V receptor** complex on platelets, which affects platelet adhesion to von Willebrand factor.
- While it causes bleeding symptoms and often **giant platelets** on smear, the specific defect mentioned (GIIb/IIIa deficiency) is not consistent with Bernard-Soulier.
*Hemophilia A*
- Hemophilia A is an **X-linked recessive bleeding disorder** caused by a deficiency of factor VIII.
- It primarily affects **secondary hemostasis**, leading to deep tissue bleeding (e.g., hemarthroses, hematomas) rather than petechiae and mucous membrane bleeding, and platelet function is normal.
Coagulation disorders US Medical PG Question 6: A 38-year-old male is brought to the emergency department by ambulance after a motor vehicle collision. He is found to have a broken femur and multiple soft tissue injuries and is admitted to the hospital. During the hospital course, he is found to have lower extremity swelling, redness, and pain, so he is given an infusion of a medication. The intravenous medication is discontinued in favor of an oral medication in preparation for discharge; however, the patient leaves against medical advice prior to receiving the full set of instructions. The next day, the patient is found to have black lesions on his trunk and his leg. The protein involved in this patient's underlying abnormality most likely affects the function of which of the following factors?
- A. Factor II only
- B. Factors II, VII, IX, and X
- C. Factors II and X
- D. Factors V and VIII (Correct Answer)
- E. Factor V only
Coagulation disorders Explanation: ***Factors V and VIII***
- The patient's initial presentation of **lower extremity swelling, redness, and pain** after trauma and immobilization is highly suggestive of **deep vein thrombosis (DVT)**, for which he received IV anticoagulation. The subsequent development of **black lesions on his trunk and leg** after switching to an oral anticoagulant and leaving against medical advice points to **warfarin-induced skin necrosis (WISN)**.
- **Warfarin-induced skin necrosis** develops in patients with a congenital deficiency of **protein C** or, less commonly, **protein S**. Protein C, in its activated form (APC), functions to inactivate **Factor V (Va)** and **Factor VIII (VIIIa)**, which are crucial cofactors in the coagulation cascade. A deficiency means these factors remain active, leading to a **procoagulant state**.
*Factor II only*
- **Factor II (prothrombin)** is inactivated by protein C, but a deficiency in protein C primarily affects the inactivation of **Factors V and VIII**, which are the specific targets of activated protein C.
- While factor II is part of the coagulation cascade, its regulation is not the primary mechanism by which protein C deficiency leads to the hypercoagulable state seen in WISN.
*Factors II, VII, IX, and X*
- These factors are **vitamin K-dependent coagulation factors**, which are inhibited by warfarin. While a deficiency in protein C can lead to an initial hypercoagulable state when warfarin is started (due to the faster drop in protein C levels compared to these factors), the primary function of protein C is to inactivate **Factors V and VIII**.
- The problem described is a **protein C deficiency**, which specifically impacts the inactivation of factors V and VIII, not directly these other vitamin K-dependent factors.
*Factors II and X*
- Similar to Factor II only, these are **vitamin K-dependent factors** inhibited by warfarin. The core issue in warfarin-induced skin necrosis is a deficiency in protein C, which normally inactivates **Factors V and VIII**, leading to a transient prothrombotic state.
- While Factor X is affected by warfarin, the direct regulatory role of protein C is predominantly on factors V and VIII.
*Factor V only*
- While **Factor V** is indeed a target of activated protein C inactivation, **Factor VIII** is also a critical target. Inactivating both **Factor V** and **Factor VIII** is essential for effective anticoagulation by protein C.
- A deficiency in protein C affects both of these crucial cofactors, making the combined option more accurate.
Coagulation disorders US Medical PG Question 7: A 2-year-old boy had increased bleeding during a circumcision. His birth and delivery were uncomplicated, and his mother had no issues with prolonged bleeding during labor. Of note, his maternal grandfather has a history of bleeding complications. The boy's vital signs are stable and physical examination is notable for scattered bruises on his lower extremities. The lab results are as follows:
Hemoglobin 12.8 gm %
Hematocrit 35.4%
WBC 8400/mm3
Platelets 215 x 109/L
PT 14 s
PTT 78 s
What is the most likely diagnosis?
- A. Glanzmann thrombasthenia
- B. Hemophilia A (Correct Answer)
- C. Von Willebrand disease
- D. Scurvy
- E. Bernard-Soulier syndrome
Coagulation disorders Explanation: ***Hemophilia A***
- The patient's presentation with increased bleeding during circumcision, scattered bruises, and a **prolonged PTT** with normal PT and platelet count is highly suggestive of **Hemophilia A**.
- The familial history of bleeding complications in the maternal grandfather points towards an **X-linked recessive inheritance pattern**, characteristic of Hemophilia A.
- Hemophilia A results from **Factor VIII deficiency**, affecting the intrinsic coagulation pathway.
*Glanzmann thrombasthenia*
- This condition involves a defect in **platelet aggregation** due to deficiency of **GPIIb/IIIa**, which would typically manifest with a **normal platelet count** but abnormal platelet function tests.
- While it causes bruising and bleeding, it would not affect the PTT, as coagulation factors are normal in this platelet function disorder.
*Von Willebrand disease*
- This is the **most common inherited bleeding disorder** and typically presents with mucocutaneous bleeding and menorrhagia in females.
- While it can cause a **mildly prolonged PTT** due to low Factor VIII levels (vWF stabilizes Factor VIII), the PTT is typically only **mildly elevated**, not as significantly prolonged as seen here (78s vs normal ~25-35s).
- The **X-linked family history** (affected maternal grandfather, not parents) strongly favors hemophilia over the **autosomal dominant** inheritance of most vWD cases.
*Scurvy*
- Scurvy results from **vitamin C deficiency** leading to impaired collagen synthesis.
- While it can cause bleeding issues like petechiae and gingival bleeding, it would not cause a **prolonged PTT** or present with significant bleeding during a circumcision.
- Coagulation tests remain normal in scurvy.
*Bernard-Soulier syndrome*
- This is a rare, inherited platelet disorder characterized by **giant platelets** and **thrombocytopenia**, resulting from a defect in the **glycoprotein Ib/IX/V complex**.
- It would present with mucocutaneous bleeding and bruising, but the patient's **platelet count is normal** (215 × 10⁹/L) and the PTT would not be prolonged in this platelet function disorder.
Coagulation disorders US Medical PG Question 8: An 8-year-old boy is brought to the pediatric emergency department by his parents with a complaint of abdominal pain and diarrhea for the past week. He states that for the past two days, he has noticed blood in his stool. His parents note that they attended a neighbor’s barbecue last weekend, but otherwise have not eaten any new foods or changed their usual diet. The patient is admitted to the hospital unit for further work-up. The provider team finds that the patient’s blood is positive for Shiga-like toxin and notes the following lab values: creatinine of 4.2 mg/dL, platelet count of 50,000/mm^3, and hemoglobin of 6.0 g/dL. Which of the following additional lab findings would be consistent with the diagnosis?
- A. Microthrombi within glomerular vessels on kidney biopsy (Correct Answer)
- B. Blunting of villi on ileal biopsy
- C. Crypt abscesses and ulcers on colonic biopsy
- D. Foamy macrophages in intestinal lamina propria on duodenal biopsy
- E. Sickling of red blood cells on peripheral blood smear
Coagulation disorders Explanation: ***Microthrombi within glomerular vessels on kidney biopsy***
- The clinical presentation (bloody diarrhea, elevated **creatinine**, low **platelets**, and low **hemoglobin**), a history of recent barbecue exposure, and presence of **Shiga-like toxin** are classic for **hemolytic uremic syndrome (HUS)**, typically caused by *E. coli* O157:H7.
- **HUS** is characterized by a **microangiopathic hemolytic anemia**, **thrombocytopenia**, and **acute kidney injury**, which pathology often reveals **microthrombi** in the glomerular capillaries.
*Blunting of villi on ileal biopsy*
- **Villus blunting** is characteristic of **celiac disease** or other malabsorptive syndromes but is not directly associated with the acute presentation of bloody diarrhea, kidney injury, and thrombocytopenia seen in HUS.
- **Celiac disease** typically presents with chronic diarrhea and malabsorption, not acute onset bloody diarrhea and hemolytic markers.
*Crypt abscesses and ulcers on colonic biopsy*
- These findings are typical of **inflammatory bowel disease (IBD)**, particularly **ulcerative colitis**, or severe infectious colitis like that caused by *Clostridium difficile*.
- While there is bloody diarrhea, the presence of **Shiga-like toxin**, **thrombocytopenia**, and **acute kidney injury** points away from IBD as the primary diagnosis.
*Foamy macrophages in intestinal lamina propria on duodenal biopsy*
- The presence of **foamy macrophages** in the lamina propria is characteristic of **Whipple's disease**, a rare systemic bacterial infection.
- This disease typically presents with chronic malabsorption, arthralgias, and neurological symptoms, which are distinct from the acute presentation of HUS.
*Sickling of red blood cells on peripheral blood smear*
- **Sickling of red blood cells** is diagnostic of **sickle cell anemia** or **sickle cell disease**, a genetic disorder.
- While it can cause hemolytic anemia and kidney complications, the presence of **Shiga-like toxin** and the specific clinical picture strongly point to HUS, not sickle cell crisis.
Coagulation disorders US Medical PG Question 9: A previously healthy 4-year-old boy is brought to the emergency department because of a 1-day history of pain and swelling of his left knee joint. He has not had any trauma to the knee. His family history is unremarkable except for a bleeding disorder in his maternal uncle. His temperature is 36.9°C (98.4°F). The left knee is erythematous, swollen, and tender; range of motion is limited. No other joints are affected. An x-ray of the knee shows an effusion but no structural abnormalities of the joint. Arthrocentesis is conducted. The synovial fluid is bloody. Further evaluation of this patient is most likely to show which of the following findings?
- A. Prolonged prothrombin time
- B. Synovial fluid leukocytosis
- C. Elevated antinuclear antibody levels
- D. Prolonged partial thromboplastin time (Correct Answer)
- E. Decreased platelet count
Coagulation disorders Explanation: ***Prolonged partial thromboplastin time***
- The clinical presentation of a young boy with **spontaneous hemarthrosis** (bloody synovial fluid in the knee) and a family history of a **bleeding disorder in a maternal uncle** is highly suggestive of **hemophilia A or B**.
- Both hemophilia A (factor VIII deficiency) and hemophilia B (factor IX deficiency) present with a **prolonged PTT** due to impaired intrinsic coagulation pathway, while PT and platelet count typically remain normal.
*Prolonged prothrombin time*
- A prolonged **prothrombin time (PT)** primarily indicates a deficiency in the **extrinsic coagulation pathway**, involving factor VII, or severe deficiencies in common pathway factors (II, V, X, fibrinogen).
- This is not characteristic of hemophilia A or B, which are deficiencies in the **intrinsic pathway**.
*Synovial fluid leukocytosis*
- **Synovial fluid leukocytosis** (increased white blood cells) is typically seen in **inflammatory or infectious arthritis**, such as septic arthritis or juvenile idiopathic arthritis.
- While the knee is swollen and tender, the **bloody synovial fluid without trauma** points away from infection and towards a bleeding disorder.
*Elevated antinuclear antibody levels*
- **Elevated antinuclear antibody (ANA) levels** are a hallmark of **systemic autoimmune diseases** like systemic lupus erythematosus (SLE) or certain forms of juvenile idiopathic arthritis.
- These conditions do not typically present with spontaneous gross hemarthrosis as the primary symptom, nor would they explain the family history of a bleeding disorder.
*Decreased platelet count*
- A **decreased platelet count (thrombocytopenia)** would lead to a bleeding disorder characterized by mucocutaneous bleeding (e.g., petechiae, purpura, epistaxis) rather than deep joint bleeds.
- Platelet dysfunction or thrombocytopenia would cause a **prolonged bleeding time**, not typically a prolonged PTT, and the overall clinical picture does not align with a primary platelet disorder.
Coagulation disorders US Medical PG Question 10: A 13-year-old girl is brought to the pediatrician due to a 4-month history of heavy vaginal bleeding during menstrual periods. She endorses episodes of bleeding gums after brushing her teeth and experienced prolonged bleeding after tonsillectomy 6 years ago. Her mother states that she bled significantly during childbirth and that the girl’s older brother has similar symptoms including easy bruising. Vitals were stable and physical exam was not revealing. Laboratory studies show:
Platelet count: 72,000/mm^3
Bleeding time: 14 min
Prothrombin time: 12 secs (INR = 1)
Partial thromboplastin time: 40 secs
Blood smear demonstrates increased megakaryocytes and enlarged platelets. Platelets do not aggregate to ristocetin. Which of the following is the most likely diagnosis?
- A. Glanzmann thrombasthenia
- B. Idiopathic thrombocytopenic purpura (ITP)
- C. Bernard-Soulier syndrome (Correct Answer)
- D. Aspirin or NSAID use
- E. von Willebrand disease (vWD)
Coagulation disorders Explanation: ***Bernard-Soulier syndrome***
- The patient presents with **thrombocytopenia** (platelet count 72,000/mm^3), **prolonged bleeding time** (14 min), and **enlarged platelets** and **megakaryocytes** on blood smear.
- The key diagnostic feature is the **failure of platelets to aggregate to ristocetin**, indicating a defect in the GPIb-IX-V receptor complex which mediates platelet adhesion to von Willebrand factor. This clinical picture in a patient with a family history of bleeding is classic for Bernard-Soulier syndrome.
*Glanzmann thrombasthenia*
- This condition is characterized by a defect in the **GPIIb/IIIa receptor**, which is crucial for platelet aggregation; however, patients with Glanzmann thrombasthenia typically have a **normal platelet count** and **normal platelet morphology**.
- Platelets in Glanzmann thrombasthenia would fail to aggregate to ADP, collagen, and epinephrine, but aggregation to **ristocetin** would generally be normal (unless very high concentrations are used), making it less likely given the specific finding of failed ristocetin aggregation and thrombocytopenia.
*Idiopathic thrombocytopenic purpura (ITP)*
- ITP causes isolated **thrombocytopenia** (low platelet count) and **increased megakaryocytes** in the bone marrow, but platelets are typically of **normal size** or may be **larger than normal** but not giant platelets.
- While ITP would cause a prolonged bleeding time, it would not typically show **enlarged platelets** on blood smear, nor would the platelets specifically fail to aggregate to ristocetin due to a receptor defect.
*Aspirin or NSAID use*
- Aspirin and NSAIDs inhibit **cyclooxygenase**, leading to impaired platelet aggregation and a **prolonged bleeding time**, but they do not cause **thrombocytopenia** or changes in **platelet morphology** like enlarged platelets or increased megakaryocytes.
- Platelet aggregation to ristocetin would be normal in the context of aspirin or NSAID use, as the GP Ib-IX-V and GP IIb/IIIa complexes are unaffected.
*von Willebrand disease (vWD)*
- vWD involves a deficiency or defect in **von Willebrand factor**, leading to impaired platelet adhesion and sometimes reduced factor VIII levels, which causes a **prolonged bleeding time**; however, platelet count and morphology are typically **normal**.
- While vWD can show decreased ristocetin-induced platelet aggregation, it does **not present with thrombocytopenia** or **enlarged platelets/megakaryocytes** as seen in this patient.
More Coagulation disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.