Chronic leukemias US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Chronic leukemias. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Chronic leukemias US Medical PG Question 1: A 64-year-old woman comes to the physician for her routine health maintenance examination. She feels well. She had cervical cancer and received radiotherapy 8 years ago. Her vital signs are within normal limits. On percussion, the spleen size is 15 cm. Otherwise, the physical examination shows no abnormalities. The laboratory test results are as follows:
Hemoglobin 10 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 65,000/mm3
Platelet count 500,000/mm3
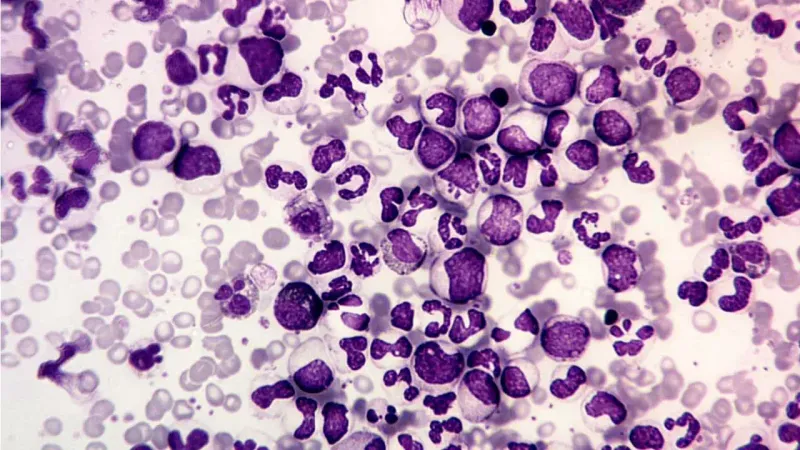
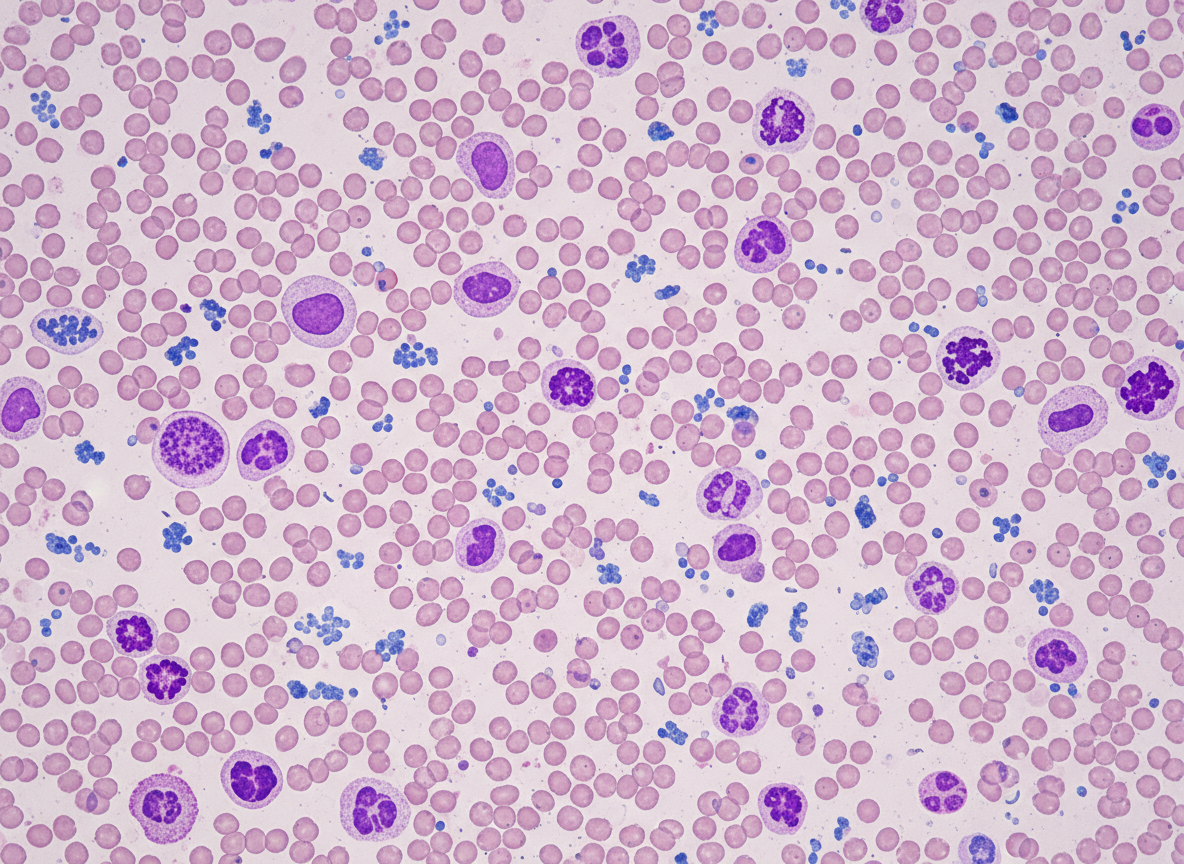
Two images of the peripheral blood smear are shown on the image. Which of the following is the most appropriate next step in management?
- A. Phlebotomy
- B. Rituximab
- C. Watchful waiting
- D. Allogeneic stem cell transplantation
- E. Dasatinib (Correct Answer)
Chronic leukemias Explanation: ***Dasatinib***
- The patient's presentation with **anemia**, **marked leukocytosis (65,000/mm³) with predominantly myeloid cells**, **thrombocytosis (500,000/mm³)**, and **splenomegaly (15 cm)** is highly suggestive of **Chronic Myeloid Leukemia (CML)**. The peripheral smear showing **myelocytes, metamyelocytes, and basophils** (indicated by arrows on the image) further supports this diagnosis.
- **Dasatinib** is a second-generation **tyrosine kinase inhibitor (TKI)** that targets the **BCR-ABL fusion protein**, which is the hallmark of CML. TKIs are the first-line treatment for CML.
*Phlebotomy*
- This is primarily used for **polycythemia vera** to reduce red blood cell mass and hematocrit.
- It is not indicated for CML, which is characterized by an overproduction of myeloid cells, not primarily red blood cells.
*Rituximab*
- **Rituximab** is a monoclonal antibody targeting the **CD20 antigen** on B-lymphocytes.
- It is used in the treatment of **B-cell non-Hodgkin lymphoma** and some autoimmune diseases, not CML.
*Watchful waiting*
- Given the patient's clear signs of **CML (leukocytosis, thrombocytosis, splenomegaly, and characteristic peripheral smear)**, active treatment is indicated, not watchful waiting.
- CML, if left untreated, progresses from the chronic phase to accelerated phase and then to **blast crisis**, which is rapidly fatal.
*Allogeneic stem cell transplantation*
- **Allogeneic stem cell transplantation** is a potentially curative treatment for CML.
- However, it is typically reserved for patients who have **failed TKI therapy** or have high-risk features, as **TKIs are the initial first-line treatment** due to their effectiveness and lower toxicity compared to transplantation.
Chronic leukemias US Medical PG Question 2: A 70-year-old man presents to his physician for evaluation of fullness and swelling of the left side of the abdomen over the last month. During this time, he has had night sweats and lost 2 kg (4.4 lb) unintentionally. He has no history of severe illness and takes no medications. The vital signs include: blood pressure 115/75 mm Hg, pulse 75/min, and temperature 36.8℃ (98.2℉). The abdomen has asymmetric distention. Percussion and palpation of the left upper quadrant reveal splenomegaly. No lymphadenopathy is detected. Heart and lung examination shows no abnormalities. The laboratory studies show the following:
Hemoglobin 9.5 g/dL
Mean corpuscular volume 95 μm3
Leukocyte count 8,000/mm3
Platelet count 240,000/mm3
Ultrasound shows a spleen size of 15 cm, mild hepatomegaly, and mild ascites. The peripheral blood smear shows teardrop-shaped and nucleated red blood cells (RBCs) and immature myeloid cells. Marrow is very difficult to aspirate but reveals hyperplasia of all 3 lineages. The tartrate-resistant acid phosphatase (TRAP) test is negative. The cytogenetic analysis is negative for translocation between chromosomes 9 and 22. Which of the following laboratory findings is most likely to be present in this patient?
- A. Monoclonal elevation of IgG
- B. Hair-like cell-membrane projections
- C. JAK2 mutation (Correct Answer)
- D. Philadelphia chromosome
- E. Reed-Sternberg cells
Chronic leukemias Explanation: ***JAK2 mutation***
- The patient's presentation with **splenomegaly**, **night sweats**, **weight loss**, **teardrop cells**, **nucleated red blood cells**, and a "dry tap" (difficulty aspirating marrow) are highly suggestive of **primary myelofibrosis**.
- A **JAK2 mutation** (specifically JAK2 V617F) is found in approximately 50-60% of patients with primary myelofibrosis and is a crucial diagnostic marker, distinguishing it from other myeloproliferative neoplasms. Other driver mutations include CALR (~25-30%) and MPL (~5-10%).
*Monoclonal elevation of IgG*
- **Monoclonal elevation of IgG** is characteristic of **plasma cell disorders** such as **multiple myeloma** or **monoclonal gammopathy of undetermined significance (MGUS)**.
- This patient's symptoms and laboratory findings, particularly the peripheral blood smear with **teardrop cells** and a "dry tap," do not align with a plasma cell dyscrasia.
*Hair-like cell-membrane projections*
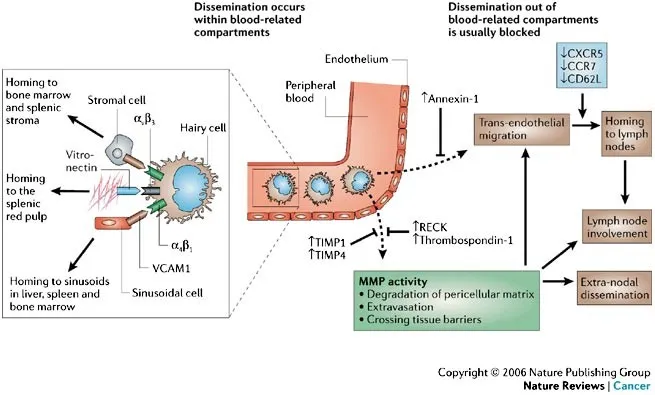
- **Hair-like cell-membrane projections** are the hallmark of **hairy cell leukemia**, a rare B-cell lymphoproliferative disorder.
- While hairy cell leukemia can cause **splenomegaly** and **pancytopenia**, the presence of **teardrop cells** and **immature myeloid cells** in the peripheral smear, along with a "dry tap," makes this diagnosis unlikely. The **negative TRAP test** also argues against hairy cell leukemia since TRAP positivity is characteristic of this condition.
*Philadelphia chromosome*
- The **Philadelphia chromosome (t(9;22))** encoding the **BCR-ABL1 fusion gene** is the defining characteristic of **chronic myeloid leukemia (CML)**.
- While CML can present with **splenomegaly** and **myeloid immature cells**, the absence of the Philadelphia chromosome on cytogenetic analysis (as stated in the stem) and the presence of **teardrop cells** and **dry tap** rule out CML in favor of myelofibrosis.
*Reed-Sternberg cells*
- **Reed-Sternberg cells** are large, multinucleated cells characteristic of **Hodgkin lymphoma**.
- Hodgkin lymphoma typically presents with **lymphadenopathy** and systemic symptoms, but the hematological findings and evidence of myelofibrosis in this patient do not support a diagnosis of lymphoma.
Chronic leukemias US Medical PG Question 3: A 72-year-old man with chronic lymphocytic leukemia (CLL) comes to the physician with a 2-day history of severe fatigue and dyspnea. He regularly visits his primary care physician and has not required any treatment for his underlying disease. His temperature is 36.7°C (98.1°F), pulse is 105/min, respiratory rate is 22/min, and blood pressure is 125/70 mm Hg. The conjunctivae are pale. Examination of the heart and lungs shows no abnormalities. The spleen is palpable 3 cm below the costal margin. No lymphadenopathy is palpated. Laboratory studies show:
Hemoglobin 7 g/dL
Mean corpuscular volume 105 μm3
Leukocyte count 80,000/mm3
Platelet count 350,000/mm3
Serum
Bilirubin Total // Direct 6 mg/dL / 0.8 mg/dL
Lactate dehydrogenase 650 U/L (Normal: 45–90 U/L)
Based on these findings, this patient’s recent condition is most likely attributable to which of the following?
- A. Bone marrow involvement
- B. Splenomegaly
- C. Evan’s syndrome
- D. Autoimmune hemolytic anemia (Correct Answer)
- E. Diffuse large B cell lymphoma
Chronic leukemias Explanation: ***Autoimmune hemolytic anemia***
- The patient's **anemia (Hb 7 g/dL)**, elevated **lactate dehydrogenase (LDH)**, relatively high **indirect bilirubin** (total bilirubin 6 mg/dL, direct 0.8 mg/dL, indicating mostly indirect), and **splenomegaly** are classic signs of **hemolysis**.
- Given his underlying **CLL**, autoimmune hemolytic anemia (AIHA) is a common paraneoplastic complication, where increased lymphocyte production leads to **autoantibody formation** against red blood cells.
*Bone marrow involvement*
- While CLL can infiltrate the bone marrow, causing **marrow failure** and anemia, this typically presents with **pancytopenia** (low white blood cells, red blood cells, and platelets).
- This patient has a **high leukocyte count** and **normal platelet count**, making marrow failure less likely to be the primary cause of his acute symptoms.
*Splenomegaly*
- **Splenomegaly** can contribute to anemia through **splenic sequestration** and **hypersplenism**, leading to shortened red blood cell survival.
- However, the markedly elevated **LDH** and **indirect bilirubin** point specifically to an active hemolytic process, which is often *caused* by the autoimmune activity rather than being the sole mechanism of anemia.
*Evan’s syndrome*
- **Evan's syndrome** is a rare condition characterized by the coexistence of **autoimmune hemolytic anemia** and **immune thrombocytopenia**.
- The patient's **platelet count is normal (350,000/mm3)**, ruling out Evan's syndrome as the specific diagnosis, although he does have one component (AIHA).
*Diffuse large B cell lymphoma*
- Transformation of CLL to **Diffuse Large B-cell Lymphoma (DLBCL)**, known as **Richter's transformation**, can cause rapidly worsening symptoms, including anemia.
- However, the characteristic features of **hemolysis** (elevated LDH, indirect bilirubin) are not direct indicators of Richter's transformation; instead, Richter's would typically present with rapidly enlarging lymph nodes, worsening systemic symptoms, and a mass.
Chronic leukemias US Medical PG Question 4: A 71-year-old man comes to the physician for a routine health maintenance examination. He has occasional fatigue but otherwise feels well. He has a history of hypertension and type 2 diabetes mellitus. He is a retired chemist. His only medication is ramipril. His temperature is 37.8°C (100°F), pulse is 72/min, respirations are 18/min, and blood pressure is 130/70 mm Hg. Physical examination shows nontender cervical and axillary lymphadenopathy. The spleen is palpated 7 cm below the costal margin. Laboratory studies show a leukocyte count of 12,000/mm3 and a platelet count of 210,000/mm3. Further evaluation is most likely to show which of the following?
- A. Smudge cells (Correct Answer)
- B. Ringed sideroblasts
- C. Rouleaux formation
- D. Teardrop cells
- E. Polycythemia
Chronic leukemias Explanation: ***Smudge cells***
- The patient's presentation with **fatigue**, **lymphadenopathy**, **splenomegaly**, and a **leukocytosis** (12,000/mm³) is classic for **chronic lymphocytic leukemia (CLL)**.
- **Smudge cells** (also known as Gumprecht shadows) are characteristic findings on a peripheral blood smear in CLL, resulting from the fragile lymphocytes being crushed during slide preparation.
*Ringed sideroblasts*
- **Ringed sideroblasts** are immature red blood cells with iron granules accumulated in a ring around the nucleus, seen in **myelodysplastic syndromes** and **sideroblastic anemia**.
- This patient's symptoms and labs, particularly the significant lymphocytosis, do not support these conditions.
*Rouleaux formation*
- **Rouleaux formation** refers to red blood cells stacking up like coins, commonly seen in conditions with increased plasma proteins such as **multiple myeloma** or **macroglobulinemia**.
- The clinical picture here, with prominent lymphadenopathy and splenomegaly, is not typical for these disorders.
*Teardrop cells*
- **Teardrop cells** (dacryocytes) are red blood cells with a characteristic teardrop shape, often associated with **myelofibrosis** due to their deformation as they squeeze through fibrotic marrow.
- The patient's presentation lacks other key features of myelofibrosis, such as significant anemia, extremely high leukocyte counts, or symptoms of marrow failure.
*Polycythemia*
- **Polycythemia** refers to an abnormally high concentration of red blood cells (or hemoglobin) in the blood, often associated with conditions like **polycythemia vera**.
- While fatigue can be a symptom, the patient's leukocyte count is elevated, not the erythrocyte count, and the presence of lymphadenopathy and splenomegaly points away from isolated polycythemia.
Chronic leukemias US Medical PG Question 5: A 71-year-old man presents to the primary care clinic with non-specific complaints of fatigue and malaise. His past medical history is significant for diabetes mellitus type II, hypertension, non-seminomatous testicular cancer, and hypercholesterolemia. He currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and he currently denies any illicit drug use. His vital signs include: temperature, 36.7°C (98.0°F); blood pressure, 126/74 mm Hg; heart rate, 87/min; and respiratory rate, 17/min. On examination, his physician notices cervical and inguinal lymphadenopathy bilaterally, as well as splenomegaly. The patient comments that he has lost 18.1 kg (40 lb) over the past 6 months without a change in diet or exercise, which he was initially not concerned about. The physician orders a complete blood count and adds on flow cytometry. Based on his age and overall epidemiology, which of the following is the most likely diagnosis?
- A. Hairy cell leukemia
- B. Acute myelogenous leukemia
- C. Chronic myelogenous leukemia
- D. Acute lymphocytic leukemia
- E. Chronic lymphocytic leukemia (Correct Answer)
Chronic leukemias Explanation: ***Chronic lymphocytic leukemia***
- The patient's age (71 years), non-specific symptoms like **fatigue and malaise**, unexplained **weight loss**, and findings of **lymphadenopathy** and **splenomegaly** are highly suggestive of **chronic lymphocytic leukemia (CLL)**.
- CLL is the most common leukemia in adults in Western countries, typically affecting older individuals, and is characterized by the accumulation of **monoclonal B lymphocytes** which can lead to lymphadenopathy and splenomegaly.
*Hairy cell leukemia*
- This condition is characterized by **pancytopenia**, **splenomegaly**, and the presence of **"hairy" cells** on peripheral smear and bone marrow.
- Lymphadenopathy is typically **less prominent or absent** in hairy cell leukemia compared to CLL.
*Acute myelogenous leukemia*
- AML typically presents with a **rapid onset of symptoms** due to bone marrow failure, such as severe anemia, thrombocytopenia (bleeding), and granulocytopenia (infections).
- While it can cause fatigue, the **lymphadenopathy and splenomegaly** are less characteristic as the primary presenting features compared to CLL, and the leukemia is defined by the proliferation of **myeloblasts**.
*Chronic myelogenous leukemia*
- CML is often associated with the **Philadelphia chromosome (BCR-ABL fusion gene)** while this patient's case is not specified.
- It usually presents with marked **leukocytosis with a left shift** (including myelocytes, metamyelocytes, and band forms), prominent splenomegaly, but often **less pronounced lymphadenopathy** than seen in CLL.
*Acute lymphocytic leukemia*
- ALL is primarily a disease of **childhood**, though it can occur in adults, but it is much less common in this age group than CLL.
- It usually presents with **abrupt onset** symptoms related to bone marrow failure, like fever, pallor, petechiae, and can have more prominent lymphadenopathy and hepatosplenomegaly but the age and chronic nature of symptoms point away from ALL.
Chronic leukemias US Medical PG Question 6: A 6-year-old boy is brought to the emergency department due to a severe infection. Laboratory work shows leukocytosis of 60 × 109/L with marked left shift, but no blast cells. The patient is febrile and dehydrated. The physician believes that this is a severe reaction to the infection and orders a leukocyte alkaline phosphatase (LAP) stain on a peripheral smear. The LAP score is elevated. Which of the following statements best describes an additional characteristic of the condition this child is suffering from?
- A. Chemotherapy is the treatment of choice.
- B. Myeloblasts and promyelocytes are expected to be found.
- C. This condition can lead to chronic myelocytic leukemia.
- D. A blood count will contain band forms, metamyelocytes, and myelocytes. (Correct Answer)
- E. The patient may develop anemia secondary to infection.
Chronic leukemias Explanation: ***A blood count will contain band forms, metamyelocytes, and myelocytes.***
- Leukocytosis with a **marked left shift** and **elevated LAP score** in the setting of severe infection is characteristic of a **leukemoid reaction**.
- A leukemoid reaction involves the premature release of immature myeloid forms such as **band forms, metamyelocytes, and myelocytes** into the peripheral blood, mimicking leukemia.
*Chemotherapy is the treatment of choice.*
- **Chemotherapy** is typically used to treat malignancies like leukemia, not a **leukemoid reaction**, which is a reactive process to severe infection.
- The primary treatment for a leukemoid reaction is to address the **underlying infection**.
*Myeloblasts and promyelocytes are expected to be found.*
- While there is a left shift, the question explicitly states "no blast cells," which differentiates a **leukemoid reaction** from acute leukemia.
- **Myeloblasts** and **promyelocytes** are more characteristic of acute myeloid leukemia, where they constitute a significant percentage of cells.
*This condition can lead to chronic myelocytic leukemia.*
- A **leukemoid reaction** is a reactive process to infection and does not transform into **chronic myelocytic leukemia (CML)**.
- CML is a myeloproliferative neoplasm characterized by the **BCR-ABL1 fusion gene** and a typically low LAP score, unlike the elevated LAP score seen here.
*The patient may develop anemia secondary to infection.*
- While **anemia of chronic disease** can occur with severe or prolonged infections, it is not the **additional characteristic** that best describes the leukemoid reaction itself, which primarily refers to the white blood cell changes.
- The prominent feature described is the specific reactive pattern of **leukocytosis** and **left shift**.
Chronic leukemias US Medical PG Question 7: A 64-year-old woman comes to the physician because of a 7-month history of abdominal discomfort, fatigue, and a 6.8-kg (15-lb) weight loss. Physical examination shows generalized pallor and splenomegaly. Laboratory studies show anemia with pronounced leukocytosis and thrombocytosis. Cytogenetic analysis shows a BCR-ABL fusion gene. A drug with which of the following mechanisms of action is most appropriate for this patient?
- A. Ribonucleotide reductase inhibitor
- B. Monoclonal anti-HER-2 antibody
- C. Topoisomerase II inhibitor
- D. Monoclonal anti-CD20 antibody
- E. Tyrosine kinase inhibitor (Correct Answer)
Chronic leukemias Explanation: ***Tyrosine kinase inhibitor***
- The patient's symptoms (abdominal discomfort, fatigue, weight loss, pallor, splenomegaly), laboratory findings (**anemia with pronounced leukocytosis and thrombocytosis**), and the presence of a **BCR-ABL fusion gene** are highly characteristic of **Chronic Myeloid Leukemia (CML)**.
- The **BCR-ABL fusion gene** encodes a constitutively active **tyrosine kinase**, which is the hallmark of CML and the primary therapeutic target for **tyrosine kinase inhibitors (TKIs)** like imatinib.
*Ribonucleotide reductase inhibitor*
- **Ribonucleotide reductase inhibitors** (e.g., hydroxyurea) block DNA synthesis and are used in myeloproliferative disorders to reduce cell counts, but they are not specific to the **BCR-ABL fusion gene** and are not the most appropriate first-line targeted therapy for CML.
- While they can control symptoms, they do not target the underlying molecular defect in CML as effectively as TKIs.
*Monoclonal anti-HER-2 antibody*
- **Monoclonal anti-HER-2 antibodies** (e.g., trastuzumab) are used to treat **HER-2 positive breast cancer** and some gastric cancers.
- They are not relevant to the treatment of CML, which is characterized by the **BCR-ABL fusion gene**.
*Topoisomerase II inhibitor*
- **Topoisomerase II inhibitors** (e.g., etoposide, doxorubicin) prevent DNA unwinding and replication, leading to cell death, and are used in various hematologic malignancies and solid tumors.
- These drugs are broad-spectrum chemotherapeutic agents not specifically targeted to the **BCR-ABL fusion protein** in CML and are not first-line therapy for this condition.
*Monoclonal anti-CD20 antibody*
- **Monoclonal anti-CD20 antibodies** (e.g., rituximab) target the CD20 protein on B lymphocytes and are primarily used to treat **B-cell non-Hodgkin lymphoma** and some autoimmune diseases.
- They have no role in the direct treatment of CML, which is a myeloid malignancy.
Chronic leukemias US Medical PG Question 8: A 67-year-old man comes to the physician because of a 2-month history of generalized fatigue. On examination, he appears pale. He also has multiple pinpoint, red, nonblanching spots on his extremities. His spleen is significantly enlarged. Laboratory studies show a hemoglobin concentration of 8.3 g/dL, a leukocyte count of 81,000/mm3, and a platelet count of 35,600/mm3. A peripheral blood smear shows immature cells with large, prominent nucleoli and pink, elongated, needle-shaped cytoplasmic inclusions. Which of the following is the most likely diagnosis?
- A. Acute lymphoblastic leukemia
- B. Myelodysplastic syndrome
- C. Hairy cell leukemia
- D. Acute myelogenous leukemia (Correct Answer)
- E. Chronic myelogenous leukemia
Chronic leukemias Explanation: ***Acute myelogenous leukemia***
- The presence of immature cells with **large, prominent nucleoli** and **pink, elongated, needle-shaped cytoplasmic inclusions** (**Auer rods**) on peripheral blood smear is pathognomonic for **acute myeloid leukemia (AML)**.
- The pancytopenia (anemia, thrombocytopenia) and extreme leukocytosis, along with generalized fatigue and pale appearance, are consistent with the presentation of AML.
*Acute lymphoblastic leukemia*
- Characterized by the proliferation of **lymphoblasts** (immature lymphocytes) in the bone marrow and peripheral blood, which typically lack Auer rods.
- While it can present with fatigue, pallor, and cytopenias, the specific morphologic features of the blast cells are different.
*Myelodysplastic syndrome*
- Involves ineffective hematopoiesis leading to **cytopenias** and dysplastic features in mature blood cells, but typically features less aggressive proliferation of immature cells than acute leukemias and **lacks Auer rods**.
- While it can progress to AML, the current description points to actively proliferating immature cells.
*Hairy cell leukemia*
- Characterized by **B lymphocytes with cytoplasmic projections** ("hairy cells") and is typically associated with **massive splenomegaly** and **pancytopenia**, but the characteristic Auer rods are absent.
- The cell morphology described (large nucleoli, needle-shaped inclusions) is inconsistent with hairy cells.
*Chronic myelogenous leukemia*
- Characterized by the **Philadelphia chromosome (BCR-ABL1 fusion gene)** and a marked increase in mature and immature myeloid cells, including granulocytes at various stages of maturation, but typically **lacks Auer rods** and usually has a higher proportion of mature rather than acutely immature cells.
- While it presents with leukocytosis and splenomegaly, the prominent immature cells with nucleoli and Auer rods are not features of CML.
Chronic leukemias US Medical PG Question 9: A 55-year-old male presents with complaints of intermittent facial flushing. He also reports feeling itchy after showering. On review of systems, the patient says he has been having new onset headaches recently. On physical exam, his vital signs, including O2 saturation, are normal. He has an abnormal abdominal mass palpable in the left upper quadrant. A complete blood count reveals: WBCs 6500/microliter; Hgb 18.2 g/dL; Platelets 385,000/microliter. Which of the following is most likely responsible for his presentation?
- A. BCR-ABL fusion
- B. Chronic hypoxemia
- C. Tyrosine kinase mutation (Correct Answer)
- D. Fibrosis of bone marrow
- E. Elevated serum erythropoietin levels
Chronic leukemias Explanation: ***Tyrosine kinase mutation***
- The patient's symptoms (facial flushing, post-showering pruritus, headaches) along with **elevated hemoglobin** (18.2 g/dL) and **splenomegaly** (abdominal mass in LUQ) strongly suggest **Polycythemia Vera (PV)**.
- PV is a **myeloproliferative neoplasm** typically caused by a **JAK2 V617F mutation**, which is a type of **tyrosine kinase mutation**, leading to constitutive activation of the JAK-STAT pathway and uncontrolled erythropoiesis.
*BCR-ABL fusion*
- A **BCR-ABL fusion gene** is characteristic of **Chronic Myeloid Leukemia (CML)**, which typically presents with markedly elevated WBCs and splenomegaly.
- While splenomegaly is present here, the patient's symptoms and hematologic findings (elevated Hgb, normal WBCs) are not consistent with CML.
*Chronic hypoxemia*
- **Chronic hypoxemia** can cause **secondary erythrocytosis** due to increased erythropoietin production in response to low oxygen levels.
- However, the patient's **O2 saturation is normal**, ruling out chronic hypoxemia as the cause of his elevated hemoglobin.
*Fibrosis of bone marrow*
- **Bone marrow fibrosis** is a hallmark of **Primary Myelofibrosis**, another myeloproliferative neoplasm, which typically presents with anemia, marked splenomegaly, and teardrop cells on peripheral smear.
- While it can manifest with constitutional symptoms, the patient's **high hemoglobin** and absent anemia make primary myelofibrosis less likely.
*Elevated serum erythropoietin levels*
- **Elevated serum erythropoietin (EPO) levels** are characteristic of **secondary erythrocytosis**, where EPO production increases due to conditions like hypoxemia, renal tumors, or exogenous EPO use.
- In **Polycythemia Vera**, EPO levels are typically **low or undetectable** due to feedback inhibition from the high red blood cell mass.
Chronic leukemias US Medical PG Question 10: A previously healthy 61-year-old man comes to the physician because of a 3-month history of intermittent fever, easy fatiguability, and a 4.4-kg (9.7-lb) weight loss. Physical examination shows conjunctival pallor. The spleen is palpated 5 cm below the left costal margin. Laboratory studies show a leukocyte count of 75,300/mm3 with increased basophils, a platelet count of 455,000/mm3, and a decreased leukocyte alkaline phosphatase score. A peripheral blood smear shows increased numbers of promyelocytes, myelocytes, and metamyelocytes. Which of the following is the most likely diagnosis?
- A. Chronic myeloid leukemia (Correct Answer)
- B. Acute promyelocytic leukemia
- C. Essential thrombocythemia
- D. Chronic lymphocytic leukemia
- E. Leukemoid reaction
Chronic leukemias Explanation: ***Chronic myeloid leukemia***
- The combination of **leukocytosis (75,300/mm3)**, **splenomegaly**, **increased basophils**, and a **low leukocyte alkaline phosphatase (LAP) score** is highly characteristic of CML
- The presence of immature myeloid forms (promyelocytes, myelocytes, metamyelocytes) on peripheral smear, referred to as a **"left shift"**, further supports this diagnosis
- CML is typically associated with the **Philadelphia chromosome [t(9;22)]** resulting in the BCR-ABL fusion gene
*Acute promyelocytic leukemia*
- This acute leukemia is characterized by a high number of **abnormal promyelocytes** with prominent Auer rods and is associated with the **t(15;17)** chromosomal translocation
- It typically presents with severe **cytopenias** (not leukocytosis) and a high risk of **disseminated intravascular coagulation (DIC)**, which are not described here
- The chronic course and marked leukocytosis make this diagnosis unlikely
*Essential thrombocythemia*
- This myeloproliferative neoplasm primarily involves **excessive platelet production**, leading to consistently high platelet counts (typically >450,000/mm3)
- While this patient has mild thrombocytosis, the prominently elevated **white blood cell count** (75,300/mm3) with myeloid left shift and **splenomegaly** point to a different myeloproliferative disorder
*Chronic lymphocytic leukemia*
- CLL is characterized by a proliferation of mature **B lymphocytes**, resulting in **lymphocytosis** with small, mature lymphocytes on peripheral smear
- The peripheral smear in this case shows increased **immature myeloid forms** (not lymphocytes), making CLL incompatible with this presentation
- CLL typically has a normal or elevated LAP score
*Leukemoid reaction*
- A leukemoid reaction is a reactive (non-malignant) process causing marked leukocytosis, usually in response to severe infection, inflammation, or malignancy
- It is characterized by a **normal or elevated LAP score**, which is the key distinguishing feature from CML
- The **decreased LAP score** in this patient makes a leukemoid reaction unlikely and strongly supports a diagnosis of CML
More Chronic leukemias US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.