Bone marrow failure syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bone marrow failure syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bone marrow failure syndromes US Medical PG Question 1: An 11-year-old boy presents to your clinic after 4 months of pain and swelling in his thigh. His mother states that at first she thought his condition was due to roughhousing, but it hasn’t gone away and now she’s concerned. You perform an X-ray that shows an ‘onion skin’ appearance on the diaphysis of the femur. You are concerned about a malignancy, so you perform a PET scan that reveals lung nodules. Which of the following is most associated with this disease?
- A. Defective mitochondrial DNA
- B. Nonsense mutation to DMD gene
- C. t(11;22) translocation (Correct Answer)
- D. t(9;22) translocation
- E. Rb loss of function mutation
Bone marrow failure syndromes Explanation: ***t(11;22) translocation***
- The clinical presentation, including the age of the patient (11-year-old boy), pain and swelling in the thigh, and the characteristic **"onion skin" appearance** on X-ray, are highly suggestive of **Ewing sarcoma**
- **Ewing sarcoma** is strongly associated with the **t(11;22) chromosomal translocation**, leading to the fusion of the **EWSR1 and FLI1 genes**
- This translocation is found in approximately **85-90% of Ewing sarcoma cases** and is the molecular hallmark of this aggressive pediatric bone malignancy
*Defective mitochondrial DNA*
- This is associated with mitochondrial disorders, which typically present with myopathies, encephalopathies, and other systemic issues, not bone tumors with an "onion skin" appearance
- While sometimes involved in cancer pathogenesis, defective mitochondrial DNA is not the primary genetic hallmark of Ewing sarcoma
*Nonsense mutation to DMD gene*
- A nonsense mutation in the **DMD gene** causes **Duchenne muscular dystrophy**, a genetic disorder characterized by progressive muscle weakness and degeneration
- This condition does not present with bone tumors, thigh pain from malignancy, or an "onion skin" periosteal reaction
*t(9;22) translocation*
- The **t(9;22) translocation**, also known as the **Philadelphia chromosome**, is characteristic of **chronic myeloid leukemia (CML)** and some cases of acute lymphoblastic leukemia (ALL)
- This genetic abnormality is associated with hematologic malignancies, not bone sarcomas like Ewing sarcoma
*Rb loss of function mutation*
- A loss-of-function mutation in the **Rb (retinoblastoma) gene** is associated with **retinoblastoma** and an increased risk of other cancers such as osteosarcoma and small cell lung cancer
- While osteosarcoma is a bone tumor, it typically presents with a "sunburst" or Codman's triangle appearance on X-ray, not the "onion skin" appearance seen in Ewing sarcoma
Bone marrow failure syndromes US Medical PG Question 2: A 3-year-old male child is found to have a disease involving DNA repair. Specifically, he is found to have a defect in the endonucleases involved in the nucleotide excision repair of pyrimidine dimers. Which of the following is a unique late-stage complication of this child's disease?
- A. Telangiectasia
- B. Colorectal cancer
- C. Malignant melanoma (Correct Answer)
- D. Lymphomas
- E. Endometrial cancer
Bone marrow failure syndromes Explanation: **Malignant melanoma**
- The described condition is **xeroderma pigmentosum**, an autosomal recessive disorder characterized by a defect in **nucleotide excision repair (NER)**, specifically the inability to remove **pyrimidine dimers** caused by **UV radiation**.
- This severely impaired DNA repair leads to an extreme predisposition to **UV-induced skin cancers**, including basal cell carcinomas, squamous cell carcinomas, and, most aggressively, **malignant melanoma**, which is a unique and life-threatening late-stage complication.
*Telangiectasia*
- **Telangiectasias** are dilated small blood vessels that appear on the skin or mucous membranes and can be associated with various conditions.
- While skin abnormalities are prevalent in xeroderma pigmentosum due to sun damage, **melanoma** is a more specific and severe late-stage complication directly resulting from the DNA repair defect.
*Colorectal cancer*
- **Colorectal cancer** is typically associated with other DNA repair defects, such as those in the **mismatch repair system**, as seen in conditions like **Lynch syndrome**.
- It is not a primary or most significant late-stage complication of xeroderma pigmentosum, which is primarily characterized by skin cancers.
*Lymphomas*
- **Lymphomas** are cancers of the lymphatic system, often linked to immune deficiencies or specific genetic translocations.
- While individuals with genetic syndromes can have increased cancer risks, **lymphoma** is not the hallmark late-stage complication of xeroderma pigmentosum; skin cancers are the predominant concern.
*Endometrial cancer*
- **Endometrial cancer** is a gynecological cancer often associated with hormonal factors or genetic predispositions like Lynch syndrome, which involves mismatch repair defects.
- This type of cancer is not a characteristic or unique late-stage complication of xeroderma pigmentosum, whose pathology is centered on **UV-induced DNA damage** and subsequent skin malignancies.
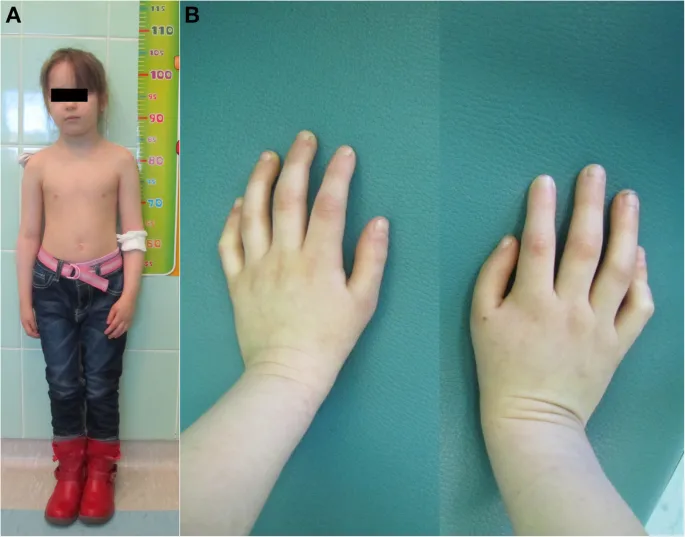
Bone marrow failure syndromes US Medical PG Question 3: A 7-year-old girl is brought to the physician by her mother because of a 5-day history of fever, fatigue, and red spots on her body. Her temperature is 38.3°C (101.1°F), pulse is 115/min, and blood pressure is 100/60 mm Hg. Physical examination shows pallor and petechiae over the trunk and lower extremities. Laboratory studies show a hemoglobin concentration of 7 g/dL, a leukocyte count of 2,000/mm3, a platelet count of 40,000/mm3, and a reticulocyte count of 0.2%. Peripheral blood smear shows normochromic, normocytic cells. A bone marrow aspirate shows hypocellularity. Which of the following is the most likely cause of this patient's findings?
- A. Idiopathic thrombocytopenic purpura
- B. Aplastic anemia (Correct Answer)
- C. Acute lymphoblastic leukemia
- D. Multiple myeloma
- E. Primary myelofibrosis
Bone marrow failure syndromes Explanation: ***Aplastic anemia***
- This diagnosis is strongly supported by the **pancytopenia** (anemia, leukopenia, thrombocytopenia), **fatigue**, and **petechiae**, coupled with a **hypocellular bone marrow** aspirate.
- The **low reticulocyte count** further indicates reduced erythropoiesis, a hallmark of bone marrow failure.
*Idiopathic thrombocytopenic purpura*
- This condition primarily causes isolated **thrombocytopenia**, while the patient also exhibits severe anemia and leukopenia.
- Bone marrow in ITP is typically normal or shows increased megakaryocytes, not hypocellularity.
*Acute lymphoblastic leukemia*
- While ALL can present with pancytopenia, fatigue, and petechiae, the bone marrow in ALL would show **hypercellularity** with an abundance of **blasts**, not hypocellularity.
- The absence of blasts on the peripheral smear and hypocellular marrow makes ALL unlikely.
*Multiple myeloma*
- This is a malignancy of **plasma cells** predominantly affecting older adults and is characterized by bone pain, hypercalcemia, renal failure, and monoclonal gammopathy.
- The patient's age and clinical presentation, especially the hypocellular bone marrow, are inconsistent with multiple myeloma.
*Primary myelofibrosis*
- Myelofibrosis typically presents with **extramedullary hematopoiesis**, splenomegaly, and a "dry tap" on bone marrow aspirate, which would show fibrosis.
- The patient's bone marrow is described as hypocellular, and no splenomegaly is mentioned, making myelofibrosis less likely.
Bone marrow failure syndromes US Medical PG Question 4: A 10-year-old girl with previously diagnosed sickle cell anemia presents to the emergency room with a low-grade fever, malaise, petechiae on her arms, and a rash on her face. She regularly takes hydroxyurea and receives blood transfusions to treat her condition. Her blood tests show a hemoglobin of 4.0 g/dL, MCV of 87 fl, and 2% reticulocyte count. An attempted bone marrow biopsy was a dry, empty tap. What is the most likely diagnosis?
- A. Reaction to the blood transfusions
- B. Gastrointestinal bleeding
- C. Anemia of chronic disease
- D. Aplastic crisis (Correct Answer)
- E. Sequestration crisis
Bone marrow failure syndromes Explanation: ***Aplastic crisis***
- The combination of **severe anemia** (hemoglobin 4.0 g/dL), **low reticulocyte count** (2%), and a **dry bone marrow tap** confirms a defect in red blood cell production.
- In a patient with **sickle cell anemia**, an aplastic crisis is often triggered by **Parvovirus B19 infection**, which targets erythroid precursors.
*Reaction to the blood transfusions*
- An acute transfusion reaction would typically present with fever, chills, urticaria, or dyspnea, which are not the predominant symptoms here.
- Hemoglobin would likely drop acutely or remain stable, but not necessarily with such a profound reticulocytopenia or bone marrow findings.
*Gastrointestinal bleeding*
- While GI bleeding can cause severe anemia, it would typically be associated with **microcytic anemia** (decreased MCV if chronic) and **elevated reticulocyte count** as the bone marrow tries to compensate, neither of which are observed.
- There is no mention of melena or hematochezia, and the dry bone marrow tap points to a production problem, not blood loss.
*Anemia of chronic disease*
- This condition typically results in **mild to moderate anemia** with a **normal or slightly reduced MCV** and a **low reticulocyte count**.
- However, the hemoglobin level of 4.0 g/dL is too severe for typical anemia of chronic disease, and the dry bone marrow tap is not a characteristic finding.
*Sequestration crisis*
- A sequestration crisis involves the rapid pooling of blood in the spleen or liver, leading to **acute severe anemia** and often **splenomegaly**.
- However, it would be characterized by a **high reticulocyte count** as the bone marrow attempts to compensate for the sudden blood loss, which is contrary to the findings in this case.
Bone marrow failure syndromes US Medical PG Question 5: A 21-year-old woman comes to the physician for an annual health maintenance examination. She has no particular health concerns. Laboratory studies show:
Hemoglobin 11.2 g/dL
Mean corpuscular volume 74 μm3
Mean corpuscular hemoglobin concentration 30% Hb/cell
Red cell distribution width 14% (N=13–15)
Genetic analysis shows a point mutation in intron 1 of a gene on the short arm of chromosome 11. A process involving which of the following components is most likely affected in this patient?
- A. TATA-rich nucleotide sequence
- B. Transfer RNA
- C. Heat shock protein 60
- D. Small nuclear ribonucleoprotein (Correct Answer)
- E. MicroRNA
Bone marrow failure syndromes Explanation: ***Small nuclear ribonucleoprotein***
- The patient's lab results (low 11.2 g/dL **hemoglobin**, low 74 µm3 **MCV**, and low 30% **MCHC**) indicate **microcytic, hypochromic anemia**, consistent with **thalassemia**.
- A point mutation in **intron 1** of a gene suggests a problem with **RNA splicing**, which is mediated by **small nuclear ribonucleoproteins (snRNPs)** as part of the spliceosome.
*TATA-rich nucleotide sequence*
- The **TATA box** is located in the **promoter region** of genes and is involved in the initiation of **transcription**, not splicing.
- A mutation in the TATA box would affect the **rate of transcription** or gene expression, not the processing of mRNA after transcription.
*Transfer RNA*
- **tRNA** molecules are essential for **protein translation** by carrying specific amino acids to the ribosome.
- A problem with tRNA would affect the **synthesis of proteins**, not the processing of pre-mRNA.
*Heat shock protein 60*
- **Heat shock proteins** are molecular **chaperones** involved in the proper **folding of proteins** and preventing protein aggregation.
- A defect in HSP60 would lead to misfolded proteins, not impaired mRNA splicing.
*MicroRNA*
- **MicroRNAs (miRNAs)** are small non-coding RNA molecules that regulate gene expression by **silencing mRNA** or inhibiting **translation**.
- While miRNAs regulate gene expression, they are not directly involved in the **splicing of introns** from pre-mRNA.
Bone marrow failure syndromes US Medical PG Question 6: A 30-year-old man presents to the emergency department with complaints of red, pinkish urine in the morning. He adds that he has been feeling some abdominal pain. The patient is not taking any medication, and his laboratory test results are as follows:
Hb 11.0 g/dL
RBC 3.7 x 1012/L
WBC 4,000/mm3
PLT 100,000/mm3
Reticulocytes 17% of red cells
Coombs test Negative
Blood smear Polychromasia
Which statement is true about this patient’s condition?
- A. CD25 deficiency is expected to be seen
- B. Rituximab therapy is effective
- C. Patient is at great risk for bleeding
- D. Urinary hemosiderin testing will be negative
- E. Eculizumab can be used to treat this condition (Correct Answer)
Bone marrow failure syndromes Explanation: ***Eculizumab can be used to treat this condition***
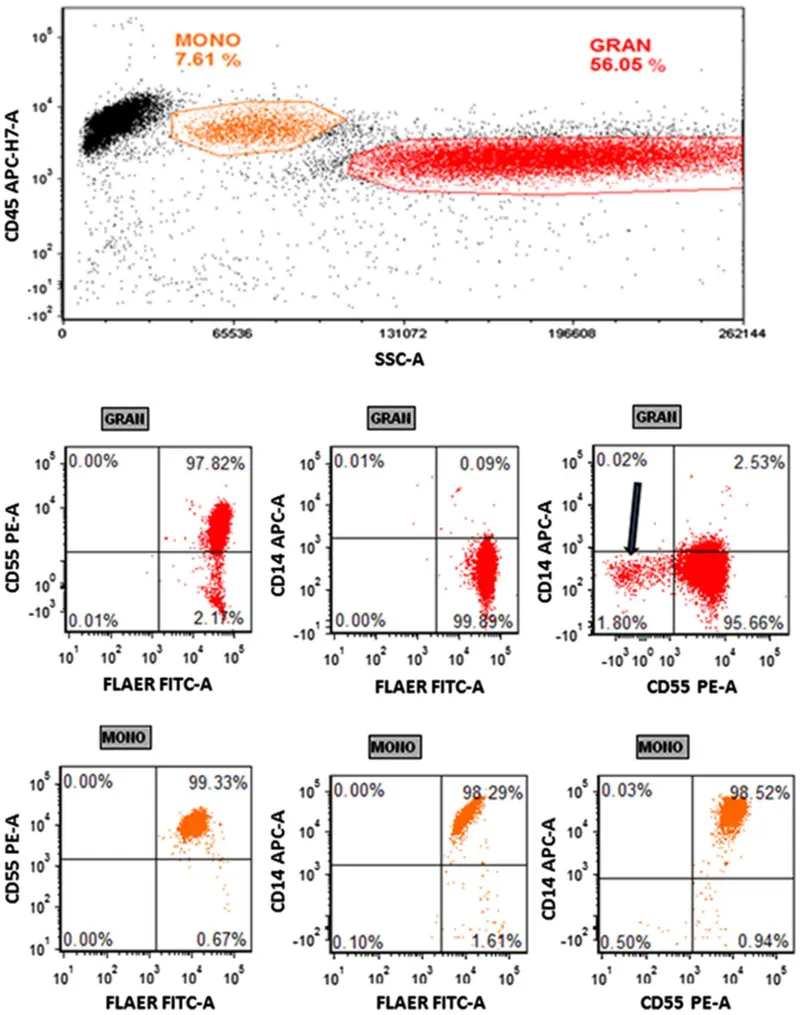
- The patient's symptoms (red, pinkish urine in the morning, abdominal pain), laboratory findings (anemia, thrombocytopenia, reticulocytosis, negative Coombs test, polychromasia), and clinical presentation are highly suggestive of **Paroxysmal Nocturnal Hemoglobinuria (PNH)**.
- **Eculizumab** is a monoclonal antibody that inhibits C5 complement protein, preventing the formation of the membrane attack complex and thus reducing hemolysis in PNH.
*CD25 deficiency is expected to be seen*
- **CD25** is a component of the IL-2 receptor, and its deficiency is not characteristic of PNH.
- PNH is characterized by a deficiency of **GPI-anchored proteins** like CD55 and CD59 on the surface of red blood cells, which protect against complement-mediated lysis.
*Rituximab therapy is effective*
- **Rituximab** is an anti-CD20 monoclonal antibody used primarily for B-cell lymphomas and autoimmune conditions, not PNH.
- Its mechanism of action is unrelated to the pathophysiology of PNH, which involves complement dysregulation.
*Patient is at great risk for bleeding*
- The patient has **thrombocytopenia** (PLT 100,000/mm3), which does put them at an increased risk of bleeding.
- However, in PNH, patients are at a higher risk of **thrombosis** (blood clots), which can be life-threatening, in addition to hemolysis and bone marrow failure.
*Urinary hemosiderin testing will be negative*
- The patient experiences **hemoglobinuria** ("red, pinkish urine in the morning"), which is indicative of chronic intravascular hemolysis.
- With ongoing hemolysis and hemoglobinuria, **urinary hemosiderin** (iron stored in renal tubular cells as a result of chronic hemoglobin reabsorption) would be expected to be positive, not negative.
Bone marrow failure syndromes US Medical PG Question 7: A 67-year-old man comes to the physician because of a 2-month history of generalized fatigue. On examination, he appears pale. He also has multiple pinpoint, red, nonblanching spots on his extremities. His spleen is significantly enlarged. Laboratory studies show a hemoglobin concentration of 8.3 g/dL, a leukocyte count of 81,000/mm3, and a platelet count of 35,600/mm3. A peripheral blood smear shows immature cells with large, prominent nucleoli and pink, elongated, needle-shaped cytoplasmic inclusions. Which of the following is the most likely diagnosis?
- A. Acute lymphoblastic leukemia
- B. Myelodysplastic syndrome
- C. Hairy cell leukemia
- D. Acute myelogenous leukemia (Correct Answer)
- E. Chronic myelogenous leukemia
Bone marrow failure syndromes Explanation: ***Acute myelogenous leukemia***
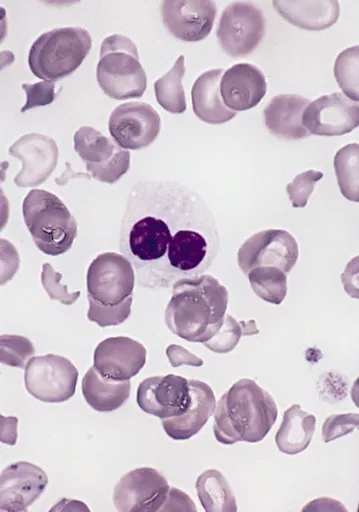
- The presence of immature cells with **large, prominent nucleoli** and **pink, elongated, needle-shaped cytoplasmic inclusions** (**Auer rods**) on peripheral blood smear is pathognomonic for **acute myeloid leukemia (AML)**.
- The pancytopenia (anemia, thrombocytopenia) and extreme leukocytosis, along with generalized fatigue and pale appearance, are consistent with the presentation of AML.
*Acute lymphoblastic leukemia*
- Characterized by the proliferation of **lymphoblasts** (immature lymphocytes) in the bone marrow and peripheral blood, which typically lack Auer rods.
- While it can present with fatigue, pallor, and cytopenias, the specific morphologic features of the blast cells are different.
*Myelodysplastic syndrome*
- Involves ineffective hematopoiesis leading to **cytopenias** and dysplastic features in mature blood cells, but typically features less aggressive proliferation of immature cells than acute leukemias and **lacks Auer rods**.
- While it can progress to AML, the current description points to actively proliferating immature cells.
*Hairy cell leukemia*
- Characterized by **B lymphocytes with cytoplasmic projections** ("hairy cells") and is typically associated with **massive splenomegaly** and **pancytopenia**, but the characteristic Auer rods are absent.
- The cell morphology described (large nucleoli, needle-shaped inclusions) is inconsistent with hairy cells.
*Chronic myelogenous leukemia*
- Characterized by the **Philadelphia chromosome (BCR-ABL1 fusion gene)** and a marked increase in mature and immature myeloid cells, including granulocytes at various stages of maturation, but typically **lacks Auer rods** and usually has a higher proportion of mature rather than acutely immature cells.
- While it presents with leukocytosis and splenomegaly, the prominent immature cells with nucleoli and Auer rods are not features of CML.
Bone marrow failure syndromes US Medical PG Question 8: A 36-year-old man presents to his primary care physician with increasing fatigue. He says that the fatigue started after he returned from vacation in South America 4 weeks ago and thinks that it may be related to an infection he got while abroad. He does not know the name of the infection but says that he went to a local clinic for treatment and was given an antibiotic. Since then, he has noticed that he is no longer able to perform his job as a contractor who renovates old homes because he feels short of breath after just a few minutes of work. Furthermore, he says that he has been experiencing prolonged nosebleeds that never occurred prior to this episode. He denies any neurologic symptoms. His past medical history is significant for alcoholic hepatitis secondary to alcohol abuse 3 years prior. Physical exam reveals conjunctival pallor as well as petechiae. Which of the following findings is associated with the most likely cause of this patient's symptoms?
- A. Hypersegmented neutrophils
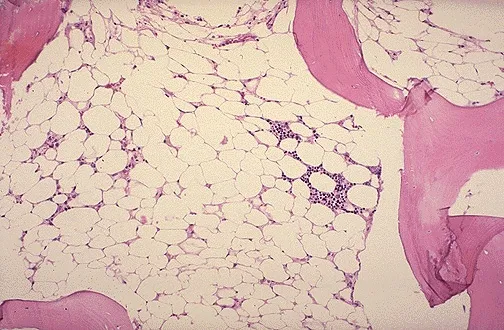
- B. Hypocellular bone marrow with fatty infiltration (Correct Answer)
- C. Schistocytes on peripheral blood smear
- D. Low circulating levels of erythropoietin
- E. Dense lines in the metaphysis of long bones
Bone marrow failure syndromes Explanation: ***Hypocellular bone marrow with fatty infiltration***
- The patient's history of **fatigue**, **shortness of breath**, **prolonged nosebleeds**, **conjunctival pallor**, and **petechiae** suggests **pancytopenia**, a hallmark of **aplastic anemia**.
- Aplastic anemia is characterized by a **hypocellular bone marrow** with significant **fatty infiltration**, replacing hematopoietic tissue.
- The history of antibiotic treatment abroad (possibly chloramphenicol) combined with the patient's symptoms points to **drug-induced aplastic anemia**.
*Hypersegmented neutrophils*
- **Hypersegmented neutrophils** are characteristic of **megaloblastic anemias**, such as those caused by **vitamin B12 deficiency** or **folate deficiency**.
- This patient's symptoms are more indicative of bone marrow failure rather than a maturation defect in myeloid cells.
*Schistocytes on peripheral blood smear*
- **Schistocytes** are fragmented red blood cells seen in **microangiopathic hemolytic anemias** (e.g., TTP, HUS, DIC) or mechanical hemolysis.
- While hemolysis can cause anemia, it does not explain the concurrent **thrombocytopenia** (leading to nosebleeds and petechiae) seen in this patient.
*Low circulating levels of erythropoietin*
- **Low erythropoietin** levels are typically seen in **anemia of chronic kidney disease**, where the kidneys fail to produce adequate erythropoietin to stimulate red blood cell production.
- This patient's presentation with significant bleeding issues and pancytopenia points away from kidney-related anemia.
*Dense lines in the metaphysis of long bones*
- **Dense lines in the metaphysis of long bones** are characteristic of **lead poisoning**, which can cause **anemia** and **fatigue**.
- However, lead poisoning does not typically cause the prominent bleeding symptoms (nosebleeds, petechiae) or pancytopenia seen in this patient.
- While the patient's occupation renovating old homes suggests potential lead exposure, the clinical picture is more consistent with aplastic anemia.
Bone marrow failure syndromes US Medical PG Question 9: A 67-year-old man presents to the emergency department with increased fatigue. He states that he has been feeling very tired lately but today lost consciousness while walking up the stairs. He reports mild abdominal distension/discomfort, weight loss, a persistent cough, and multiple episodes of waking up drenched in sweat in the middle of the night. The patient does not see a primary care physician but admits to smoking 2 to 3 packs of cigarettes per day and drinking 1 to 3 alcoholic beverages per day. He recently traveled to Taiwan and Nicaragua. His temperature is 99.5°F (37.5°C), blood pressure is 177/98 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 98% on room air. On physical exam, you note a fatigued appearing elderly man who is well-groomed. Cardiopulmonary exam reveals mild expiratory wheezes. Abdominal exam is notable for a non-pulsatile mass in the left upper quadrant. Laboratory values are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 105,500/mm^3
Platelet count: 197,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 92 mg/dL
Creatinine: 1.4 mg/dL
Ca2+: 10.2 mg/dL
Leukocyte alkaline phosphatase score: 25 (range 20 - 100)
AST: 12 U/L
ALT: 17 U/L
Which of the following is the most likely diagnosis?
- A. Tuberculosis
- B. Leukemoid reaction
- C. Acute myelogenous leukemia
- D. Acute lymphoblastic leukemia
- E. Chronic myeloid leukemia (Correct Answer)
Bone marrow failure syndromes Explanation: ***Chronic myeloid leukemia***
- The patient presents with **fatigue, weight loss, night sweats, and a persistent cough**, which are common symptoms of CML. The **extreme leukocytosis (105,500/mm^3)**, **non-pulsatile LUQ mass (splenomegaly)**, and a **low-normal leukocyte alkaline phosphatase (LAP) score of 25** are highly indicative of CML.
- CML characteristically shows a **low LAP score (typically <20)**, which distinguishes it from a leukemoid reaction. This patient's LAP of 25, while technically within the normal range (20-100), is at the lower end and consistent with CML.
- CML is a myeloproliferative disorder characterized by the **Philadelphia chromosome (BCR-ABL fusion gene)**, leading to uncontrolled proliferation of myeloid cells.
*Tuberculosis*
- While **fatigue, weight loss, night sweats, and cough** can be present in tuberculosis, the **dramatically elevated leukocyte count** and **splenomegaly** are not characteristic findings of TB.
- Tuberculosis would typically show a more prominent respiratory symptomology (e.g., hemoptysis) and imaging findings consistent with lung involvement, and its diagnosis would be confirmed by microbiologic studies.
*Leukemoid reaction*
- A leukemoid reaction is a **reactive leukocytosis (>50,000/mm^3)** often triggered by severe infection or inflammation, but it would present with an **elevated leukocyte alkaline phosphatase (LAP) score (typically >100)**, which contradicts the patient's low-normal LAP score of 25.
- Unlike CML, a leukemoid reaction does not typically cause **splenomegaly** to the extent that it forms a palpable mass.
*Acute myelogenous leukemia*
- AML typically presents with **malignant myeloid blasts** in the peripheral blood (often >20%) and bone marrow, and patients are usually more acutely ill with symptoms related to **pancytopenia** (e.g., severe anemia, thrombocytopenia with bleeding), which are not present in this case.
- While AML can cause leukocytosis, it is characterized by a **predominance of immature blast cells** rather than the mature granulocytes seen in CML.
*Acute lymphoblastic leukemia*
- ALL is primarily a disease of **lymphoid progenitor cells** and is more common in children, though it can occur in adults. It is characterized by the presence of **lymphoblasts** in the blood and bone marrow.
- While it can cause fatigue and weight loss, the **extremely high leukocyte count composed primarily of mature myeloid cells** and **prominent splenomegaly** are inconsistent with ALL.
Bone marrow failure syndromes US Medical PG Question 10: A 38-year-old woman was brought to the emergency department after she experienced dizziness and shortness of breath while walking with her friend. She recently immigrated to the United States and is unable to report her previous medical history. Physical exam reveals pallor underneath her eyelids. Labs are obtained with the following results:
Hemoglobin: 8.4 g/dL
Platelet count: 62,000/mm^3
Mean corpuscular volume: 89 µm^3
Reticulocyte count: 0.1%
Lactate dehydrogenase: 175 U/L
Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Living in an old house
- B. Recent infection with a toxin producing gram-negative rod
- C. Vegan diet
- D. Chronic alcohol abuse
- E. Administration of a 50S ribosomal inhibitor (Correct Answer)
Bone marrow failure syndromes Explanation: ***Administration of a 50S ribosomal inhibitor***
- The patient's symptoms (dizziness, shortness of breath, pallor) and lab results (anemia, thrombocytopenia, normal MCV, very low reticulocyte count) are highly suggestive of **aplastic anemia**.
- Aplastic anemia is often caused by exposure to toxins or medications; **chloramphenicol**, a 50S ribosomal inhibitor, is a classic cause of dose-independent, idiosyncratic aplastic anemia.
*Living in an old house*
- Living in an old house is associated with **lead poisoning**, which typically causes a **microcytic anemia** with **basophilic stippling**, not normocytic anemia with thrombocytopenia and low reticulocytes.
- Lead poisoning does not typically cause severe thrombocytopenia as seen in this patient.
*Recent infection with a toxin producing gram-negative rod*
- This scenario would suggest **hemolytic uremic syndrome (HUS)**, which presents with microangiopathic hemolytic anemia, thrombocytopenia, and acute kidney injury.
- The patient's **normal LDH** and **low reticulocyte count** argue against hemolysis as the primary cause of anemia.
*Vegan diet*
- A vegan diet can lead to **vitamin B12 deficiency**, which causes **macrocytic anemia**, often with pancytopenia.
- This patient has a **normal MCV (89 µm^3)**, ruling out macrocytic anemia.
*Chronic alcohol abuse*
- Chronic alcohol abuse can cause **folate deficiency** leading to **macrocytic anemia** and **thrombocytopenia**.
- The patient's **normal MCV** makes macrocytic anemia due to folate deficiency unlikely.
More Bone marrow failure syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.