Acute leukemias US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute leukemias. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute leukemias US Medical PG Question 1: A 15-year-old male presents to the emergency department with fever, malaise, and shortness of breath for 1 week. Further history reveals that the patient experiences swelling in his face in the morning that disappears as the day progresses. Physical exam reveals hepatosplenomegaly. A complete blood count shows WBC 84,000 cells/mL. Most of this patient's leukocytes are likely to express which of the following cell surface markers?
- A. CD20
- B. CD19 (Correct Answer)
- C. CD10
- D. CD16
- E. CD2
Acute leukemias Explanation: ***CD19***
- The clinical picture of a 15-year-old male with **fever**, **malaise**, **shortness of breath**, **facial swelling** (periorbital edema), and **hepatosplenomegaly** with a **WBC of 84,000 cells/mL** is highly suggestive of **acute lymphoblastic leukemia (ALL)**.
- **CD19** is a characteristic surface marker for **B-cell ALL**, which is the most common subtype of ALL in children and adolescents.
*CD20*
- **CD20** is also a B-cell marker, but its expression is usually seen in more mature B-cell lymphomas or leukemias, and less consistently or strongly in **precursor B-cell ALL** compared to CD19.
- While some B-ALL cases can express CD20, **CD19** is a more universal and defining marker for the lineage of the leukemic blasts in this context.
*CD10*
- **CD10** (common acute lymphoblastic leukemia antigen or CALLA) is a cell surface marker that can be expressed by **precursor B-cell ALL**, and its presence often correlates with a favorable prognosis.
- However, it is not expressed by all B-ALL cases and **CD19** is a more fundamental and consistently expressed pan-B-cell marker for these blasts.
*CD16*
- **CD16** (FcγRIII) is typically expressed on **natural killer (NK) cells**, neutrophils, macrophages, and some T-cells.
- It is not a characteristic marker for **leukemic blasts** in **acute lymphoblastic leukemia**.
*CD2*
- **CD2** is a surface glycoprotein found on most **T-lymphocytes** and **NK cells**.
- Its presence would indicate a **T-cell ALL**, which presents similarly but the most common form is B-cell ALL, for which CD19 is the definitive marker.
Acute leukemias US Medical PG Question 2: A 5-year-old boy presents to his pediatrician with weakness. His father observed that his son seemed less energetic at daycare and kindergarten classes. He was becoming easily fatigued from mild play. His temperature is 98°F (37°C), blood pressure is 90/60 mmHg, pulse is 100/min, and respirations are 20/min. Physical exam reveals pale conjunctiva, poor skin turgor and capillary refill, and cervical and axillary lymphadenopathy with assorted bruises throughout his body. A complete blood count reveals the following:
Leukocyte count: 3,000/mm^3
Segmented neutrophils: 30%
Bands: 5%
Eosinophils: 5%
Basophils: 10%
Lymphocytes: 40%
Monocytes: 10%
Hemoglobin: 7.1 g/dL
Hematocrit: 22%
Platelet count: 50,000/mm^3
The most specific diagnostic assessment would most likely show which of the following?
- A. Bone marrow biopsy with ≥ 20% lymphoblasts (Correct Answer)
- B. Fluorescence in situ hybridization analysis with 9:22 translocation
- C. Peripheral blood smear with > 50% lymphoblasts
- D. Flow cytometry with positive terminal deoxynucleotidyl transferase staining
- E. Fluorescence in situ hybridization analysis with 12:21 translocation
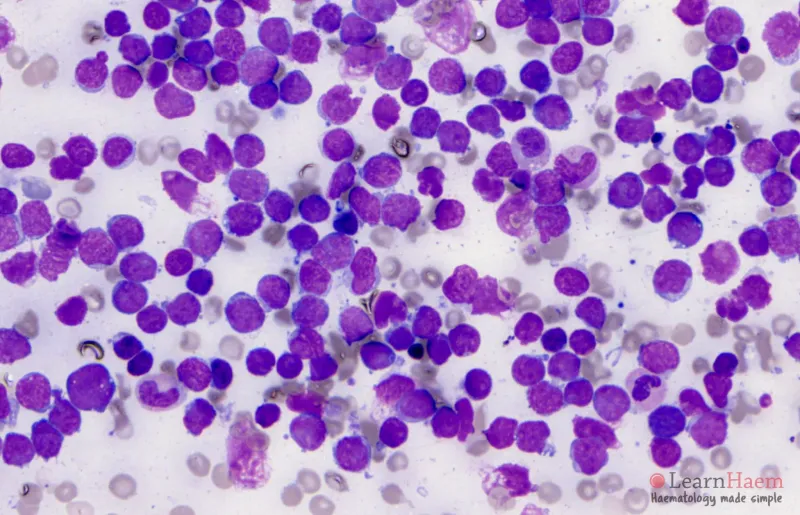
Acute leukemias Explanation: ***Bone marrow biopsy with ≥ 20% lymphoblasts***
- The patient's symptoms (weakness, fatigue, pallor, bruising, lymphadenopathy) and blood counts (anemia, thrombocytopenia, leukopenia with relative lymphocytosis) are highly suggestive of **Acute Lymphoblastic Leukemia (ALL)**.
- The most specific diagnostic assessment for ALL involves a **bone marrow biopsy** showing **≥20% lymphoblasts** per WHO 2016 classification, confirming the abnormal proliferation of immature lymphoid cells.
- This is the **gold standard** for diagnosing ALL and distinguishes it from other hematologic disorders.
*Fluorescence in situ hybridization analysis with 9:22 translocation*
- The **Philadelphia chromosome (t[9;22])** is characteristic of **Chronic Myeloid Leukemia (CML)**, which is rare in children and presents differently.
- While t(9;22) can occur in 3-5% of childhood ALL and indicates poor prognosis, it is a **prognostic marker**, not the primary diagnostic criterion for ALL itself.
*Peripheral blood smear with > 50% lymphoblasts*
- While lymphoblasts can be seen in the peripheral blood in ALL, a specific percentage threshold in peripheral blood is **not a diagnostic criterion** for ALL.
- The peripheral blood smear can be suggestive, but the **bone marrow blast percentage is the gold standard** for definitive diagnosis.
*Flow cytometry with positive terminal deoxynucleotidyl transferase staining*
- **Terminal deoxynucleotidyl transferase (TdT)** is a nuclear enzyme expressed in pre-B and pre-T lymphoblasts and is an important marker for ALL.
- Flow cytometry with positive TdT staining helps **characterize and classify the blasts** but does not quantify the blast percentage required for diagnosis, which is provided by the bone marrow biopsy.
*Fluorescence in situ hybridization analysis with 12:21 translocation*
- The **t(12;21) [ETV6-RUNX1] translocation** is the most common cytogenetic abnormality in childhood B-cell ALL (20-25% of cases) and is associated with favorable prognosis.
- While its presence is relevant for risk stratification and treatment planning, the primary diagnostic criterion for ALL is the **percentage of lymphoblasts in the bone marrow**.
Acute leukemias US Medical PG Question 3: A 47-year-old woman comes to the physician because of easy bruising and fatigue. She appears pale. Her temperature is 38°C (100.4°F). Examination shows a palm-sized hematoma on her left leg. Abdominal examination shows an enlarged liver and spleen. Her hemoglobin concentration is 9.5 g/dL, leukocyte count is 12,300/mm3, platelet count is 55,000/mm3, and fibrinogen concentration is 120 mg/dL (N = 150–400). Cytogenetic analysis of leukocytes shows a reciprocal translocation of chromosomes 15 and 17. Which of the following is the most appropriate treatment for this patient at this time?
- A. Cyclophosphamide
- B. All-trans retinoic acid (Correct Answer)
- C. Imatinib
- D. Rituximab
- E. Platelet transfusion
Acute leukemias Explanation: ***All-trans retinoic acid***
- This patient's presentation with **easy bruising, fatigue, pallor, fever, hepatosplenomegaly, thrombocytopenia**, and a **t(15;17) translocation** is highly characteristic of **acute promyelocytic leukemia (APL)**.
- **All-trans retinoic acid (ATRA)** is the cornerstone of APL treatment, inducing differentiation of leukemic promyelocytes and reversing the coagulopathy often associated with this subtype.
*Cyclophosphamide*
- **Cyclophosphamide** is an alkylating agent used in various cancers and autoimmune diseases, but it is **not the primary or most appropriate initial therapy for APL**.
- Its mechanism of action involves DNA damage, which is different from the differentiation-inducing effect needed for APL.
*Imatinib*
- **Imatinib** is a tyrosine kinase inhibitor primarily used for **chronic myeloid leukemia (CML)** and some GISTs, targeting the **BCR-ABL fusion protein**.
- It is **ineffective in APL** as the underlying genetic abnormality (PML-RARA fusion) is different.
*Rituximab*
- **Rituximab** is a monoclonal antibody targeting the **CD20 antigen** found on B-lymphocytes, primarily used for **B-cell non-Hodgkin lymphoma** and some autoimmune conditions.
- It has **no role in the treatment of acute promyelocytic leukemia**, which is a myeloid malignancy.
*Platelet transfusion*
- While the patient has **thrombocytopenia (platelet count 55,000/mm3)** and **easy bruising/hematoma**, suggesting a need for platelet support, it is a **supportive measure**, not the definitive treatment for the underlying disease.
- **Platelet transfusion** alone does not address the fundamental pathophysiology of APL or the associated coagulopathy (fibrinogen 120 mg/dL), which requires ATRA.
Acute leukemias US Medical PG Question 4: A 35-year-old male presents to his physician with the complaint of fatigue and weakness for six months. His physician orders a CBC which demonstrates anemia and thrombocytopenia. During the subsequent work up, a bone marrow biopsy is performed which ultimately leads to the diagnosis of acute promyelocytic leukemia. Which of the following translocations and fusion genes would be present in this patient?
- A. t(15;17) - PML/RARalpha (Correct Answer)
- B. t(9;22) - PML/RARalpha
- C. t(9;22) - BCR/Abl1
- D. t(14;18) - PML/RARalpha
- E. t(8;14) - BCR/Abl1
Acute leukemias Explanation: ***t(15;17) - PML/RARalpha***
- **Acute Promyelocytic Leukemia (APL)** is uniquely characterized by the **t(15;17) translocation**, which fuses the **PML (promyelocytic leukemia)** gene on chromosome 15 with the **RARalpha (retinoic acid receptor alpha)** gene on chromosome 17.
- This specific genetic alteration is crucial for diagnosis and dictates treatment with **all-trans retinoic acid (ATRA)**, which targets the aberrant RARalpha fusion protein.
*t(9;22) - PML/RARalpha*
- The **t(9;22) translocation** is associated with **Chronic Myeloid Leukemia (CML)**, forming the **BCR-ABL1 fusion gene**, not PML/RARalpha.
- This option incorrectly pairs the translocation with a fusion gene specific to APL.
*t(9;22) - BCR/Abl1*
- While **t(9;22)** and the **BCR/Abl1 fusion gene** are correctly paired, this is the hallmark of **Chronic Myeloid Leukemia (CML)**, not acute promyelocytic leukemia.
- CML typically presents with a different clinical picture and bone marrow findings than APL, primarily **leukocytosis with a left shift** and **basophilia**.
*t(14;18) - PML/RARalpha*
- The **t(14;18) translocation** is characteristic of **follicular lymphoma**, not any form of acute leukemia.
- It results in the overexpression of the **BCL-2 gene**, promoting cell survival, and is not associated with the PML/RARalpha fusion.
*t(8;14) - BCR/Abl1*
- The **t(8;14) translocation** is associated with **Burkitt lymphoma**, leading to the translocation of the **MYC oncogene** close to immunoglobulin heavy chain enhancers.
- This option also incorrectly pairs the translocation with the **BCR/Abl1 fusion gene**, which is characteristic of CML, and is not relevant to APL.
Acute leukemias US Medical PG Question 5: A pathologist receives a patient sample for analysis. Cells in the sample are first labeled with fluorescent antibodies and then passed across a laser beam in a single file of particles. The light scatter and fluorescent intensity of the particles are plotted on a graph; this information is used to characterize the sample. This laboratory method would be most useful to establish the diagnosis of a patient with which of the following?
- A. Ventricular septal defect and facial dysmorphism with low T-lymphocyte count
- B. Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology
- C. Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria (Correct Answer)
- D. Multiple opportunistic infections with decreased CD4 counts
- E. Vesicular lesions with dermatomal distribution and dendritic corneal ulcers
Acute leukemias Explanation: ***Pancytopenia and deep vein thrombosis with intermittent hemoglobinuria***
- The described laboratory method is **flow cytometry**, which is the **gold standard for diagnosing paroxysmal nocturnal hemoglobinuria (PNH)** by detecting the absence of **CD55** and **CD59** on red blood cells due to impaired GPI anchor synthesis.
- PNH classically presents with **pancytopenia**, **hemolytic anemia** (leading to hemoglobinuria), and a high risk of **thrombosis** (e.g., deep vein thrombosis).
*Ventricular septal defect and facial dysmorphism with low T-lymphocyte count*
- This clinical picture suggests **DiGeorge syndrome**, which involves a developmental defect of the **third and fourth pharyngeal pouches**, leading to thymic hypoplasia and **T-cell deficiency**.
- While flow cytometry is used to quantify T-lymphocyte subsets (e.g., CD3, CD4, CD8), the primary method for diagnosing DiGeorge syndrome is **fluorescent in situ hybridization (FISH)** for a **22q11 deletion**, making it less ideal for flow cytometry diagnosis.
*Painless generalized lymphadenopathy with monomorphic cells and interspersed benign histiocytes on histology*
- This description with "**monomorphic cells**" is more consistent with certain **non-Hodgkin lymphomas** (e.g., Burkitt lymphoma) rather than Hodgkin lymphoma, which typically shows a **polymorphic** cellular infiltrate.
- While flow cytometry can be useful in characterizing lymphomas by identifying cell surface markers, the diagnosis is primarily established by **lymph node biopsy and histopathology** with **immunohistochemistry**, making flow cytometry a supplementary rather than primary diagnostic tool.
*Multiple opportunistic infections with decreased CD4 counts*
- This presentation is highly suggestive of **HIV infection leading to AIDS**. The "decreased CD4 counts" are a key diagnostic and prognostic marker.
- While flow cytometry is used to **monitor CD4 cell counts** in HIV patients, the initial diagnosis of HIV is established via **antibody/antigen combination tests** and confirmed by **Western blot** or **PCR for viral load**, not by flow cytometry.
*Vesicular lesions with dermatomal distribution and dendritic corneal ulcers*
- This clinical presentation points to **herpes zoster ophthalmicus** (shingles affecting the eye due to **varicella-zoster virus** reactivation).
- Diagnosis is primarily **clinical** based on the characteristic rash and eye findings, although **PCR** of vesicular fluid can confirm VZV infection. Flow cytometry has no role in this diagnosis.
Acute leukemias US Medical PG Question 6: A 70-year-old retired police officer is being evaluated for fatigue. A peripheral smear shows extremely elevated numbers of immature myeloid cells, which are positive for myeloperoxidase and a translocation t(15,17). Which of the following statements is true regarding his condition?
- A. Myelodysplastic syndromes may give rise to the condition.
- B. This condition is also developed early in life in patients with Down syndrome.
- C. Philadelphia chromosome may be seen and indicates a poor prognosis.
- D. Auer rods are responsible for gum hyperplasia and bleeding.
- E. The patient can be treated with a vitamin A derivative. (Correct Answer)
Acute leukemias Explanation: ***The patient can be treated with a vitamin A derivative.***
- The presence of **immature myeloid cells** positive for **myeloperoxidase (MPO)** and a **t(15;17) translocation** strongly indicates **Acute Promyelocytic Leukemia (APL)**.
- APL is effectively treated with **all-trans retinoic acid (ATRA)**, which is a **vitamin A derivative**, as it induces differentiation of the promyelocytes.
*Myelodysplastic syndromes may give rise to the condition.*
- While myelodysplastic syndromes (MDS) can transform into other types of **acute myeloid leukemia (AML)**, they typically give rise to other subtypes of AML, not specifically APL, which has a distinct genetic translocation.
- MDS would usually show a **dysplastic morphology** in multiple cell lines, which is not described as the primary feature here.
*This condition is also developed early in life in patients with Down syndrome.*
- **Down syndrome** patients have an increased risk of specific leukemias, particularly **Acute Megakaryoblastic Leukemia (AML M7)** in early childhood, and **Acute Lymphoblastic Leukemia (ALL)**.
- APL, characterized by t(15;17), is not specifically associated with Down syndrome.
*Philadelphia chromosome may be seen and indicates a poor prognosis.*
- The **Philadelphia chromosome (t(9;22))** is characteristic of **Chronic Myeloid Leukemia (CML)** and some cases of **B-ALL**, not APL.
- The t(15;17) translocation is the defining feature of APL, and Philadelphia chromosome is not seen in this condition.
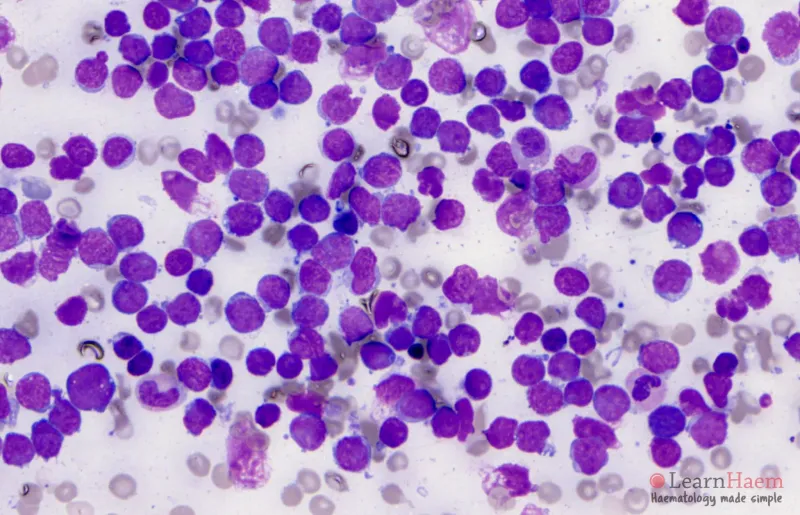
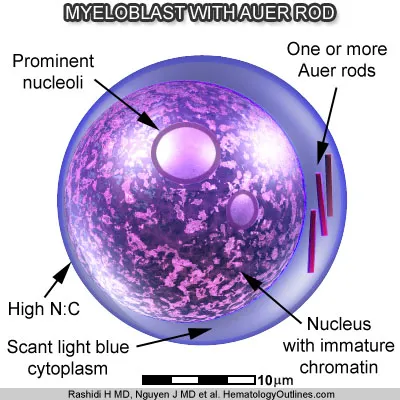
*Auer rods are responsible for gum hyperplasia and bleeding.*
- **Auer rods** are indeed characteristic of AML, including APL, and are formed by abnormal fusion of primary granules.
- However, **gum hyperplasia and bleeding** are more distinctly characteristic of **Acute Monocytic Leukemia (AML M5)** due to monocyte infiltration, rather than directly caused by Auer rods.
Acute leukemias US Medical PG Question 7: A 59-year-old man presents to his primary care physician for fatigue. In general, he has been in good health; however, he recently has experienced some weight loss, abdominal pain, and general fatigue. He has a past medical history of anxiety, diabetes, a fracture of his foot sustained when he tripped, and a recent cold that caused him to miss work for a week. His current medications include metformin, insulin, buspirone, vitamin D, calcium, and sodium docusate. His temperature is 99.5°F (37.5°C), blood pressure is 150/100 mmHg, pulse is 90/min, respirations are 18/min, and oxygen saturation is 98% on room air. Physical exam reveals a calm gentleman. A mild systolic murmur is heard in the left upper sternal region. The rest of the physical exam is within normal limits. Laboratory values are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 66,500/mm^3 with normal differential
Platelet count: 177,000/mm^3
Leukocyte alkaline phosphatase: elevated
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
BUN: 20 mg/dL
Glucose: 120 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 10.9 mEq/L
AST: 12 U/L
ALT: 10 U/L
Which of the following is the most likely diagnosis?
- A. Chronic myeloid leukemia
- B. Acute lymphoblastic leukemia
- C. Multiple myeloma
- D. Leukemoid reaction (Correct Answer)
- E. Chronic lymphocytic leukemia
Acute leukemias Explanation: ***Leukemoid reaction***
- The **highly elevated leukocyte count** (66,500/mm^3) with **normal differential** and **elevated leukocyte alkaline phosphatase (LAP)** are classic features of a leukemoid reaction.
- This condition is a reactive increase in white blood cells, often triggered by **severe infections, inflammation, or malignancy**, rather than a primary hematologic malignancy.
- The patient's **recent cold/infection** provides a clear trigger for this reactive process.
*Chronic myeloid leukemia*
- While CML also presents with marked leukocytosis, it is typically characterized by a **low or normal LAP score** and a left shift with immature myeloid forms (e.g., myelocytes, metamyelocytes).
- The patient's **normal differential** and **elevated LAP score** argue strongly against CML.
*Acute lymphoblastic leukemia*
- ALL is characterized by the presence of a large number of **lymphoblasts** (immature lymphocytes) in the blood and bone marrow, which is not suggested by the normal differential.
- It usually presents with symptoms of **bone marrow failure** (anemia, thrombocytopenia, infection) and often affects children, though it can occur in adults.
*Multiple myeloma*
- Multiple myeloma is a plasma cell malignancy characterized by **monoclonal gammopathy**, bone lesions, renal failure, and hypercalcemia; **marked leukocytosis is not a primary feature**.
- Although the patient has mildly elevated calcium, the absence of other myeloma features (renal dysfunction, anemia, bone pain) and the **very high WBC count with elevated LAP** make this diagnosis unlikely.
*Chronic lymphocytic leukemia*
- CLL is characterized by a **profound lymphocytosis** (elevated lymphocytes) with mature-appearing cells, which is not described by the "normal differential" of the leukocyte count.
- The elevated LAP would also be unusual in CLL, as CLL cells typically have low LAP activity.
Acute leukemias US Medical PG Question 8: A 3-year-old boy is brought to the physician by his mother because of a 2-week history of generalized fatigue, intermittent fever, and occasional bleeding from his nose. His temperature is 38.3°C (100.9°F). He appears pale. Physical examination shows cervical lymphadenopathy and multiple petechiae on his trunk. The spleen is palpated 3 cm below the left costal margin. His hemoglobin concentration is 9.3 g/dL, leukocyte count is 63,000/mm3, and platelet count is 30,000/mm3. A bone marrow aspirate predominantly shows immature leukocytes that stain positive for CD10, CD19, and terminal deoxynucleotidyl transferase (TdT), and negative for myeloperoxidase. Which of the following is the most likely diagnosis?
- A. Acute megakaryoblastic leukemia
- B. Acute myelomonocytic leukemia
- C. Hairy cell leukemia
- D. Pre-B-cell acute lymphoblastic leukemia (Correct Answer)
- E. T-cell chronic lymphocytic leukemia
Acute leukemias Explanation: ***Pre-B-cell acute lymphoblastic leukemia***
- The patient's age (3 years old), **pancytopenia** (anemia, thrombocytopenia, and elevated WBC count with immature forms), **splenomegaly**, and **lymphadenopathy** are classic signs of ALL.
- The presence of immature leukocytes positive for **CD10, CD19, and TdT**, and negative for **myeloperoxidase (MPO)**, is specific for B-cell acute lymphoblastic leukemia.
*Acute megakaryoblastic leukemia*
- This leukemia is characterized by proliferation of **megakaryoblasts**.
- While it can manifest with pancytopenia, it would typically show immunophenotype markers like **CD41 and CD61**, not CD10 and TdT.
*Acute myelomonocytic leukemia*
- This is a type of **acute myeloid leukemia (AML)** and would show immature cells with **myeloid differentiation**.
- Cells would typically be positive for **myeloperoxidase (MPO)** and lack lymphoid markers like CD10 and TdT.
*Hairy cell leukemia*
- This is a **rare, chronic B-cell leukemia** typically seen in older adults, not children, and characterized by cells with "hairy" projections.
- While it involves B-cells, the immunophenotype and age of presentation do not match the case.
*T-cell chronic lymphocytic leukemia*
- This is a **chronic leukemia** primarily affecting older adults, not young children, and involves mature T-lymphocytes.
- The cell morphology and immunophenotype (immature cells positive for CD10, CD19, TdT) are inconsistent with this diagnosis.
Acute leukemias US Medical PG Question 9: A 7-year-old boy presents to his primary care physician for a general checkup. The patient has been feeling poorly for the past several weeks and has been losing weight. He states that he often feels weak and too tired to play with his friends. He is no longer interested in many recreational activities he used to be interested in. The patient's parents state that a few of their child's friends have been sick lately. His temperature is 102°F (38.9°C), blood pressure is 77/48 mmHg, pulse is 110/min, respirations are 24/min, and oxygen saturation is 98% on room air. On exam, you note a fatigued appearing child who has lost 10 pounds since his last appointment. Left upper quadrant tenderness and a mass is noted on abdominal exam. Which of the following best describes the most likely diagnosis?
- A. Smudge cells on peripheral smear
- B. TdT positive cells (Correct Answer)
- C. Infection sensitive to oseltamivir
- D. Auer rods on peripheral smear
- E. Parental mistreatment of the child
Acute leukemias Explanation: ***TdT positive cells***
- This patient's symptoms, including **fever**, **weight loss**, **fatigue**, and **splenomegaly** (left upper quadrant tenderness and mass), are highly suggestive of **Acute Lymphoblastic Leukemia (ALL)**.
- **Terminal deoxynucleotidyl transferase (TdT)** is a DNA polymerase found in immature lymphocytes (blasts) and is a key marker for diagnosing ALL.
- ALL is the **most common childhood malignancy**, particularly prevalent in children aged 2-10 years.
*Smudge cells on peripheral smear*
- **Smudge cells** are characteristic of **Chronic Lymphocytic Leukemia (CLL)**, which predominantly affects older adults and is rare in children.
- The clinical picture of rapid decline and significant systemic symptoms in a child is inconsistent with CLL.
*Infection sensitive to oseltamivir*
- Oseltamivir is an **antiviral medication for influenza**, and while the child has a fever, the profound **weight loss**, **fatigue**, and **abdominal mass** point towards a hematologic malignancy, not a typical viral infection.
- Viral infections rarely present with such a significant abdominal mass or sustained constitutional symptoms for several weeks.
*Auer rods on peripheral smear*
- **Auer rods** are cytoplasmic inclusions pathognomonic for **Acute Myeloid Leukemia (AML)**.
- While AML can occur in children, **ALL is far more common in this age group** (85% of childhood leukemias), and the presentation is highly classic for ALL, making TdT positivity the best diagnostic marker.
*Parental mistreatment of the child*
- While some symptoms (weight loss, fatigue) could potentially be seen in neglect, the presence of **fever**, **splenomegaly** (abdominal mass), and **hypotension** points strongly to a severe underlying medical condition.
- Objective signs of systemic illness necessitate a thorough medical workup rather than suspicion of abuse.
Acute leukemias US Medical PG Question 10: A 6-year-old boy is brought to the emergency department with a mild fever for the past week. He has also had generalized weakness and fatigue for the past month. He has been complaining of diffuse pain in his legs and arms. He has a history of Down syndrome with surgical repair of a congenital atrial septal defect as an infant. His temperature is 38.0° C (100.4° F), pulse is 85/min, respirations are 16/min, and blood pressure is 90/60 mm Hg. He has enlarged cervical lymph nodes bilaterally that are nontender to palpation. He is uncooperative for the rest of the examination. Laboratory studies show:
Hemoglobin 10.2 g/dL
Hematocrit 30.0%
Leukocyte count 50,000/mm3
Platelet count 20,000/mm3
Serum
Sodium 136 mEq/L
Potassium 4.7 mEq/L
Chloride 102 mEq/L
Bicarbonate 25 mEq/L
Urea nitrogen 18 mg/dL
Creatinine 1.1 mg/dL
Total bilirubin 0.9 mg/dL
AST 30 U/L
ALT 46 U/L
Which of the following is most likely to confirm the diagnosis?
- A. Bone marrow biopsy (Correct Answer)
- B. Serum protein electrophoresis
- C. Blood culture
- D. Echocardiography
- E. Monospot test
Acute leukemias Explanation: ***Bone marrow biopsy***
- The patient's symptoms (fever, fatigue, diffuse bone pain, lymphadenopathy) combined with **marked leukocytosis (WBC 50,000/mm³), anemia, and severe thrombocytopenia** are highly suggestive of **acute leukemia**.
- Children with **Down syndrome have a 10-20 times increased risk** of developing acute leukemia, particularly acute lymphoblastic leukemia (ALL) and acute megakaryoblastic leukemia (AMKL).
- A **bone marrow biopsy** is the definitive diagnostic test for leukemia, as it allows for morphological, immunophenotypic, and cytogenetic analysis of bone marrow cells to confirm the diagnosis and classify the specific type of leukemia.
*Serum protein electrophoresis*
- This test is primarily used for diagnosing **plasma cell disorders** like multiple myeloma or monoclonal gammopathy, which are not suggested by the patient's presentation or laboratory findings.
- While leukemias can rarely present with abnormal protein production, it is not the initial or most appropriate diagnostic step for suspected leukemia.
*Blood culture*
- A blood culture is used to identify **bacterial or fungal infections** in the bloodstream. While the patient has a mild fever and could have an infection, the persistent symptoms (weeks to a month), generalized bone pain, and particularly the marked leukocytosis with severe thrombocytopenia and anemia are characteristic of hematologic malignancy rather than simple infection.
- Although ruling out infection may be important (especially in the context of potential neutropenia if blasts predominate), it would not confirm the underlying hematologic malignancy indicated by the lab results.
*Echocardiography*
- **Echocardiography** evaluates the structure and function of the heart. The patient has a history of repaired atrial septal defect, but there are no current cardiac symptoms or signs (e.g., murmurs, signs of heart failure) that necessitate an echocardiogram for the presenting complaints.
- This test would not help in diagnosing the suspected hematologic condition.
*Monospot test*
- The **Monospot test** is used to diagnose infectious mononucleosis, typically caused by the Epstein-Barr virus (EBV). While some symptoms (fever, fatigue, lymphadenopathy) can overlap, the marked leukocytosis (likely with circulating blasts), severe thrombocytopenia, and diffuse bone pain are not characteristic of mononucleosis.
- Infectious mononucleosis typically presents with **atypical lymphocytosis**, not the marked leukocytosis with severe thrombocytopenia seen in this case.
More Acute leukemias US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.